Abstract
Intrathecal drug delivery systems (IDDS) is a crucial for treating refractory cancer pain, but their effectiveness in patients with pain across multiple spinal segments is limited by the localized spread of pain relief medication. Our team innovatively implanted double-catheter IDDS to manage pain related to neck and abdominal cancer. While this may represent a new solution, the efficacy, safety, and cost-effectiveness remain unclear. A multi-center retrospective cohort study. Pain management and medical oncology departments of six hospitals in various regions of China. 62 patients with neck or abdominal cancer pain were enrolled from November 2019 to June 2024. Patients were divided into two groups: the double-catheter IDDS group (n = 26) and the single-catheter IDDS groups (n = 36). Propensity score matching was employed to create a balanced cohort of 48 patients. The primary outcome was pain control, assessed using Numeric Rating Scale [NRS]), breakthrough pain (BTP), and opioid consumption, including intrathecal morphine dose [IDMED] and oral daily morphine dose [ODMED]. No significant differences were observed in the NRS score and IDMED between the double-catheter and single-catheter groups prior to surgery, one day post-surgery, and at hospital discharge (p > 0.05). However, one-month post-surgery, the NRS score was significantly lower in the double-catheter group compared to the single-catheter group, while the IDMED was significantly higher compared to the single-catheter group (p < 0.05). A significantly higher number of BTP episodes and ODMED was observed in the single-catheter group compared to the two-catheter group at one day post-surgery, at hospital discharge, and one-month post-surgery (p < 0.05). The duration of hospitalization and the incidence of adverse events did not differ significantly between the two groups (p > 0.05). However, the cumulative hospitalization expenses, IDDS opioid costs per month, and refill costs calculated for a month were significantly higher in the double-catheter group compared to the single-catheter group. Conversely, the monthly oral opioid costs and total costs of analgesic were significantly lower in comparison to the single-catheter group (p < 0.05). The preliminary findings of this study, both single- and double-catheter IDDS effectively manage cancer pain in neck and abdominal cancer patients without increasing adverse events. Despite higher initial costs, double-catheter IDDS demonstrates superior long-term pain control, a reduced incidence of BTP, and lower overall monthly analgesic costs. However, due to the limitations of the study’s sample size and patient survival time, further research is needed to assess the long-term benefits.
Similar content being viewed by others
Introduction
Refractory cancer pain, which is resistant to standard opioid and/or co-analgesic therapies, is a condition affecting approximately 10–20% of patients1. Several factors have been identified as risk factors for a poor pain prognosis, including younger age, elevated opioid tolerance, neuropathic pain conditions, incident pain, psychological distress, a history of nonmedical opioid use, and cognitive impairments. Managing the care of patients with intractable pain remains a significant challenge2.
Invasive modalities such as intrathecal drug delivery systems (IDDS) are often considered for patients whose pain remains refractory to conventional treatments. These interventional approaches have the potential to provide substantial analgesia for individuals who show limited responsiveness to standard medical management3. Research has indicated that the implementation of IDDS can significantly reduce systemic opioid utilization by more than 50%, thereby attenuating the associated adverse effects4. Nevertheless, challenges remain in applying IDDS for refractory cancer pain. A primary limitation is the restricted diffusion of intrathecal drug delivery, which is confined to an approximate 5–10 cm radius above and below the catheter5. This diffusion is further impeded by physiological factors such as respiratory and vascular pulsations. To address these challenges, optimize drug dosage, and enhance analgesic efficacy, the Polyanalgesic Consensus Conference recommends precise catheter tip placement at the spinal cord level corresponding to the predominant pain site6. A case report demonstrating the successful management of head and face cancer pain through catheter implantation in the anterior pontine cistern emphasizes the critical role of accurate catheter positioning7. However, the widespread nature of pain in numerous patients with refractory cancer pain complicates the identification of a single optimal catheter tip location, typically determined by the region of most intense pain8. While oral opioid therapy can effectively manage the pain of most patients, challenges remain for individuals who experience difficulties with or intolerance to oral medications9. Spiegel, Matthew et al. also pointed out that the clinical value of IDDS for many cancer pain patients is its ability to reduce the dose of oral morphine. However, more research should focus on future studies should focus on the efficacy of IDDS in isolation, devoid of or controlled for adjuvant analgesic medications10. This approach would also provide greater assistance to patients who are unable to take oral strong opioids in sustained-release or controlled-release formulations.
To optimize pain management for patients experiencing widespread cancer-related pain, our research team implemented double-catheter IDDS in patients with both neck and abdominal cancer pain11. This intervention resulted in significant pain relief and high patient satisfaction. However, the comparative risks and benefits of double-catheter IDDS in managing refractory cancer pain affecting the neck, abdomen, and other body regions remain unclear. Consequently, this study was undertaken as a multicenter retrospective analysis to evaluate the efficacy and safety of double-catheter IDDS for generalized refractory cancer pain.
Materials and methods
Patient selection
This multicenter, retrospective case-control study was approved by the Ethics Committee of Sichuan Cancer Hospital (Ethical approval number: SCCHEC-03-2024-071). All procedures involving human participants adhered to the ethical principles outlined in the Declaration of Helsinki. Between January 2019 and June 2024, a retrospective review was conducted of patients diagnosed with refractory cancer pain who underwent either single-catheter or double-catheter IDDS treatment at six participating centers. Experienced pain specialists at each center performed the surgical procedures. Following a comprehensive explanation of the potential benefits and risks associated with both minimally invasive surgical options, patients provided informed consent for their chosen treatment plan.
Inclusion criteria included patients with a confirmed diagnosis of refractory cancer pain12, experiencing both neck and abdominal pain, as indicated by a Numeric Rating Scale (NRS) score of ≥ 4 and breakthrough pain (BTP) occurring at least three times daily13, as well as those with adequate mental and cognitive capacity to undergo surgery (New York Heart Association heart function classification I-II). Exclusion criteria included patients who developed post-surgical spinal cord tumors that resulted in cerebrospinal fluid circulation disturbances, those requiring sedation due to inadequate pain control despite IDDS therapy with or without oral analgesics, individuals who underwent additional interventional pain management procedures following IDDS, and patients whose post-discharge follow-up data could not be obtained.
Intrathecal drug delivery systems
The Intrathecal Drug Delivery Systems was a thermoplastic polyurethane catheter (ZS2-I-Q-1.2/0.6–850, Suzhou Linhua Medical Device Co., Ltd., China). The IDDS catheter possesses a total length of 100 cm, with an outer diameter measuring 1.1 ± 0.1 mm and an inner diameter of 0.6 ± 0.1 mm. Five spiral-shaped drug delivery outlets were uniformly distributed along the tip of the catheter, connected to the infusion port through a disposable implanted drug delivery device with a dedicated needle. The other end of the dedicated needle was connected externally to an electronic pump (REHN-11, RenXian, China). The total volume of analgesic drugs for both patient controlled analgesia (PCA) pumps was 200 mL, with the lowest continuous infusion rate of 0.1 mL per hour.
Opioid analgesics
For intrathecal analgesia, a 10 mg:1 ml morphine injection was used (H21022436, Northeast Pharmaceutical Group Co., Ltd., China). Oral analgesics included morphine hydrochloride sustained-release tablets (H10930078, Southwest China Pharmaceutical Co., Ltd., China) and oxycodone hydrochloride sustained-release tablets (J20110014, Bard Pharmaceuticals Limited, UK). The dose conversion ratio for oxycodone to morphine tablets is 2:1.
Surgical procedures
Single-catheter IDDS
The patient presented with both malignant and chronic treatment-induced pain in the neck and abdomen14. In accordance with established guidelines and consensus recommendations for patients with extensive cancer pain, catheter implantation at the spinal cord level corresponding to the most severe pain was indicated6. Intraoperative management included electrocardiogram monitoring, oxygen therapy, venous access, ultrasound-guided abdominal transverse plane nerve block for right abdominal wall anesthesia, and local infiltration anesthesia at the L3/4 intervertebral space puncture site. Alternative puncture sites (L2/3 or L4/5) were considered if contraindications (infection, tumor, or tuberculosis) precluded access to L3/4. A 14-gauge Tuohy needle was used to perform a paramedian lumbar puncture at the L3/4 intervertebral space, confirmed by cerebrospinal fluid egress. A catheter was then inserted into the predetermined spinal cord level, and its position was verified using digital subtraction angiography (DSA). Following catheter advancement through a subcutaneous tunnel to a pre-incised abdominal pocket, connection to the port was established, and device integrity was confirmed (Fig. 1).
Double-catheter IDDS
The technical details of this surgical procedure have been previously documented and published by our team11. The distal ends of the double-catheter IDDS were positioned at the spinal cord segments associated with abdominal and cervical pain, respectively. To enhance the clarity of the surgical procedure, we provide an illustrative example involving implantation at the C1 and T5/6 spinal levels. Lumbar puncture was performed at the L2/3 and L3/4 intervertebral spaces using a 14-gauge Tuohy needle (Fig. 2A). Cerebrospinal fluid (CSF) aspiration confirmed successful subarachnoid space access. Subsequently, catheters were tunneled subcutaneously to an abdominal incision site, where they were connected to a port (Fig. 2B). The port was secured to the external oblique muscle fascia. Following wound closure, a non-invasive butterfly needle was used to connect the catheters to the port within the pocket (Fig. 2C). The needle’s distal end was attached to a PCA device (Fig. 2D). Simultaneously, using X-ray imaging and under the guidance of DSA, two catheters were introduced into the spinal canal via the Tuohy needle pathway (Fig. 3A). The correct placement of the catheters at the T5/6 and C1 spinal cord levels was subsequently confirmed (Fig. 3B-C).
Data collection
Data collection was conducted independently by two researchers. Four distinct data categories were compiled: (1) patient demographics, including age, gender, body mass index (BMI), preoperative NRS score, preoperative BTP score, preoperative oral daily morphine equivalent dose (ODMED), estimated survival time, and rationale for intrathecal drug delivery system (IDDS) implantation (inadequate pain relief, drug-related toxicity intolerance, or both); (2) tumor and cancer pain treatment details, encompassing analgesic drug side effects, surgical interventions, chemotherapy, radiation therapy, immunotherapy, targeted therapy, and interventional therapy; (3) IDDS analgesic efficacy indicators, such as NRS scores at multiple time points, daily BTP count, ODMED, and intrathecal morphine dose (IDMED); (4) perioperative complications (paraplegia, spinal cord nerve dysfunction, hypotension, respiratory depression, catheter obstruction, urinary retention, pain sensitization, numbness, intracranial hypotension syndrome) and associated hospitalization costs in Renminbi (Chinese Yuan, CNY), including IDDS implantation, maintenance, and first-month intrathecal opioid medication expenses based on discharge prescriptions. The primary outcome is IDDS analgesic efficacy indicators. The secondary outcome is perioperative complications and costs.
Statistical analysis
All measurement data were presented as mean ± standard deviation (SD) when the data were determined to be normally distributed (p > 0.1 in the normality test). Otherwise, data were presented as median (25th, 75th quartiles) or count (%). For normally distributed data with homogeneous variances, An independent samples t-test was employed to compare two groups. For continuous variables not meeting these assumptions, Mann-Whitney U tests and Wilcoxon matched-pairs signed-rank tests were conducted. Categorical variables were analyzed using chi-square or Fisher’s exact tests. Statistical analyses were performed using SPSS version 22.0 (IBM Corp.) with a significance level of p < 0.05.
Results
General data of patients
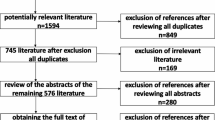
A total of 369 patients were administered IDDS analgesia for cancer-related pain. Of these, 117 presented with both neck and abdominal pain. Exclusion criteria included spinal cord metastases (n = 15), altered consciousness due to intracranial metastases (n = 22), bone radiofrequency ablation within one-month of IDDS (n = 4), and inability to complete one-month postoperative follow-up (n = 14). Ultimately, 62 patients met inclusion criteria, with 36 receiving single-catheter IDDS and 26 receiving double-catheter IDDS. To mitigate potential bias, propensity score matching (PSM) was employed to create balanced groups. A 1:1 matching ratio with a caliper of 0.2 was used, resulting in two groups of 24 patients each for comparative analysis (Fig. 4).
Prior to PSM, patient demographics and preoperative characteristics are summarized in Table 1. These include age, gender, BMI, baseline NRS and BTP scores, baseline ODMED, estimated survival time, and the indication for IDDS implantation. No significant differences were observed between groups at baseline. Following PSM, a matched cohort of 24 patients per group was generated, resulting in well-balanced demographic characteristics between the comparison groups.
Management of tumor and cancer-associated pain in the matched sample
As presented in Table 2, following PSM, a significantly higher proportion of patients in the Single-catheter IDDS group received preoperative immunotherapy compare to the Double-catheter IDDS group (p < 0.05). Conversely, no significant differences were observed between the two groups in terms of the incidence of preoperative analgesic drug side effects, the frequency of preoperative surgical procedures, or the administration rates of radiotherapy, chemotherapy, targeted drug therapy, and interventional therapy (p > 0.05).
Evaluation of analgesic effect
As presented in Table 3, primary analgesic efficacy for both modalities was assessed using NRS scores, the number of BTP per day, the supplementation with the ODMED, and the IDMED at preoperative, postoperative day 1, discharge, and one-month postoperative timepoints. Compared to preoperative values, NRS scores decreased significantly in both groups at all postoperative timepoints (p < 0.05). No significant differences in NRS scores were observed between groups at preoperative, postoperative day 1, or discharge (p > 0.05). However, at one-month postoperatively, the Double-catheter IDDS group exhibited significantly lower NRS scores compared to the Single-catheter IDDS group (t = 3.734, p = 0.001). Regarding BTP management, the Double-catheter IDDS group demonstrated significantly lower daily BTP incidence compared to the Single-catheter IDDS group at all evaluated timepoints (Z = 5.126, p < 0.001; Z = 1.994, p = 0.046; Z = 3.734, p = 0.001). Oral morphine supplementation was required in the Double-catheter IDDS group only on postoperative day 1, with subsequent tapering and discontinuation. Conversely, the Single-catheter IDDS group required continuous oral morphine supplementation postoperatively, with a significantly higher ODMED at postoperative day 1, discharge and one month postoperative timepoints compared to the Double-catheter IDDS group (Z = 2.718, p = 0.029; Z = 4.116, p < 0.001; Z = 3.943, p < 0.001). No significant differences in IDMED were observed between groups at postoperative day 1 or discharge, but a significant increase was noted in the Double-catheter IDDS group at one-month postoperatively (Z = 1.012, p = 0.311; Z = 1.540, p = 0.147; Z = 2.216, p = 0.033).
Adverse events
To mitigate the incidence of post-dural puncture headache (PDPH), prophylactic epidural blood patches (EBPs) were administered postoperatively to both groups of patients. All adverse events were managed with supportive care or intrathecal opioid dose adjustments. Despite the implantation of double catheters in the subarachnoid space for patients in the Double-catheter IDDS group, no cases of catheter-induced paraplegia were observed within one month postoperatively. Neither group experienced hypotension, respiratory depression, catheter obstruction, urinary retention, neurological dysfunction, or pain sensitization. As presented in Table 4, the Single-catheter IDDS group reported one case of sedation/drowsiness, seven cases of vomiting, and five cases of intracranial hypotension syndrome. In contrast, the Double-catheter IDDS group experienced four cases of sedation/drowsiness, two cases of vomiting, four cases of intracranial hypotension syndrome, one case of dry mouth, and one case of muscle spasm. Statistical analysis revealed no significant differences in adverse event incidence between the two groups (p > 0.05).
Hospital stays and associated expenses
As presented in Table 5, despite the increased procedural complexity of double-catheter IDDS, no significant difference in length of hospital stay was observed between the double-catheter and single-catheter IDDS groups (t = 0.35, p = 0.348). Hospitalization costs were significantly higher in the double-catheter IDDS group, primarily attributed to the increased number of implanted devices. Specifically, monthly IDDS opioid and refill costs were markedly elevated in the double-catheter group (t = 13.937, p < 0.001; t = 7.088, p < 0.001; t = 8.459, p < 0.001). Conversely, monthly oral opioid and total monthly analgesic costs were significantly lower in the double-catheter IDDS group compared to the single-catheter IDDS group (t = 3.943, p < 0.001; t = 3.011, p = 0.003).
Discussion
In this study, we compared the efficacy, safety, and cost-effectiveness of double-catheter versus single-catheter IDDS for managing pain in patients with neck and abdominal cancers. Our results indicate that, while both configurations are effective for pain control, the double-catheter IDDS offers distinct advantages in terms of long-term pain reduction and a decreased incidence of breakthrough pain (BTP). Specifically, at one-month post-surgery, patients in the double-catheter group reported significantly lower NRS pain scores and required less supplemental oral morphine than those in the single-catheter group. This suggests that the double-catheter system, presented here for the first time in its original research form, may offer more sustained pain relief, potentially enhancing patients’ quality of life.
Precise catheter tip placement is paramount for optimal pain management in IDDS. Research has demonstrated a substantial decline in morphine concentrations with increasing distance from the catheter tip, with levels averaging only 24% ± 15% and 20% ± 12% of peak concentration at spinal cord segments 5 cm caudal and cephalad, respectively, to the discharge site. This phenomenon, even without considering cerebrospinal fluid circulation disturbances, adequately explains the pharmacokinetic failures observed in certain chronic intrathecal administrations15. Consequently, ensuring catheter tip placement within the spinal cord plane innervated by nociceptive pathways is crucial. Recognizing the critical influence of catheter tip positioning, Wang et al. achieved exceptional clinical outcomes in managing head and facial malignancy pain by meticulously placing the catheter tip near the anterior cistern of the cranial nerve pontine, thereby emphasizing the pivotal role of catheter location in IDDS efficacy16.
The efficacy of IDDS in managing refractory cancer pain has been extensively documented17, but there is also a substantial body of research emphasizing the importance of intrathecal catheter tip placement in effective pain management. For instance, current literature has substantiated the clinical efficacy of catheter implantation at the C1 vertebral level for managing head and neck tumor-related pain6, and at the T10 level for low back pain18. Current practice for generalized cancer pain involves catheter placement at the spinal cord level corresponding to the most intense pain, often supplemented with oral analgesics19. However, a substantial number of patients continue to require higher oral medication dosages due to factors such as catheter positioning and the limited diffusion capabilities of drugs like morphine, fentanyl, alfentanil, and sufentanil20. Conversely, as demonstrated in this study, some patients elect IDDS to mitigate the adverse effects of analgesic medications, including nausea, vomiting, drowsiness, and severe constipation21.
Given the paucity of research investigating optimal intrathecal catheter tip placement for systemic cancer pain management, our team initiated a novel approach involving the simultaneous implantation of two catheters in the neck and abdominal regions. Comprehensive technical details and drug administration protocols for this procedure have been extensively described in our previously published work11.
In the double catheter IDDS group, continuous administration of small morphine doses targeted the spinal cord regions associated with neck and abdominal cancer pain. In contrast, in the single catheter IDDS group, a pain specialist determined the most painful area based on the patient’s individual clinical presentation. This multicenter retrospective study evaluated the clinical efficacy and safety of single and double-catheter interventions for patients experiencing concurrent neck and abdominal cancer pain. To mitigate imbalances in demographic characteristics and preoperative treatments, PSM statistical methods were applied to the study cohort22. Notably, both IDDS strategies demonstrated efficacy in cancer pain management. However, one-month postoperative data revealed a marked reduction in BTP requiring daily management in the double catheter group compared to the single catheter group, where inadequate analgesia contributed to persistent BTP in some patients23.
Data analysis revealed no significant differences in IDMED between groups from postoperative day one to discharge. However, a significant increase in IDMED was observed in the double catheter IDDS group compared to the single catheter IDDS group at one-month postoperatively. This disparity can be attributed to exclusive reliance on IDDS analgesia by the double catheter IDDS group upon discharge, eliminating the need for adjuvant morphine. Conversely, the single catheter IDDS group employed IDDS for targeted pain management while supplementing with oral morphine for other pain sites. Consequently, the double catheter IDDS group demonstrated minimal to no OMED requirements from discharge to one-month postoperatively, whereas the single catheter IDDS group required continuous oral morphine supplementation. These findings emphasize the potential advantages of the double catheter approach in optimizing IDDS efficacy24.
The insertion of two catheters, each measuring 1.1 ± 0.1 mm in diameter, into the spinal canal necessitates careful consideration of potential complications, including secondary spinal cord compression and nerve damage resulting from the presence of th catheters, which could lead to severe paraplegia25, especially in spinal segments accommodating both catheters. Moreover, the infection risk and the spatial occupation of the catheters pose substantial threats to cerebrospinal fluid circulation26. Notably, no patients in this cohort experienced paraplegia. This outcome may be attributed to the spatial separation between the arachnoid membrane and spinal cord surface, estimated to be approximately 5–10 mm at the L1-L2 vertebral level27. This anatomical distance may explain the absence of reported spinal cord compression or paralysis despite the presence of two catheters in the thoracic and lumbar regions.
To reduce PDPH, both patient groups received prophylactic EBPs postoperatively28. This practice deviates from the International Multidisciplinary Consensus Practice Guidelines for PDPH, which do not endorse prophylactic EBP for PDPH prevention29. It is noteworthy that the patients in this study experienced cancer-related pain, which generally resulting in poorer nutritional status compared to non-cancer patients, thereby diminishing capacity for dural self-repair30. Moreover, the presence of pain often precluded extended bed rest, typically recommended for PDPH symptom alleviation. Despite using EBP following spinal puncture, no significant differences in postoperative adverse reactions were observed between groups. These adverse reactions primarily included postoperative sedation/drowsiness, vomiting, intracranial hypotension syndrome, xerostomia, muscle spasms, and other symptoms in a small subset of patients, aligning with the incidence reported in other IDDS clinical studies31.
The substantial implantation costs and minimal maintenance requirements associated with IDDS pose significant barriers to its widespread implementation32. Wangjun et al. reported a mean hospitalization duration of approximately 15 days for single-catheter IDDS patients in Beijing, China, aligning with the current study’s findings. However, the reported hospitalization costs of $7268 (52016 CNY) exceeded the present study’s figure of 12,606 CNY22. Given the earlier publication date of Wangjun et al.‘s research and the ongoing reduction in the costs of domestically produced IDDS materials in China, it is highly conceivable that implantation costs have decreased over time. While the initial investment in a double-catheter IDDS increased overall hospitalization expenses, its more complete analgesic efficacy significantly reduced monthly analgesic expenditures in later stages compared to single-catheter IDDS. The potential reduction or elimination of oral analgesic use highlights the long-term cost-effectiveness of double-catheter IDDS for managing cancer pain in advanced disease states.
Our study has several important limitations. (1) The sample size, the small sample size may reduce statistical power to detect subtle differences, although we collected data from six large medical centers to enhance the representativeness of the sample, the limited number of cancer pain patients undergoing IDDS, especially double-catheter IDDS, constrained the possibility of achieving a larger sample size. To address this limitation, future randomized controlled trial studies could increase sample size by incorporating more centers or extending the recruitment period, thereby improving statistical power and the generalizability of the results. (2) the short follow-up period. the short follow-up period limits a comprehensive evaluation of the long-term efficacy and safety of IDDS, Given the limited survival duration of patients with advanced cancer, the follow-up period in this study was established at one month. To address this limitation, future multicenter randomized controlled trials (RCTs) will amend the inclusion criteria to require participants to have an anticipated survival time exceeding three months.(3) the cost analysis, the cost analysis does not account for key economic factors, such as the costs of managing complications and long-term device maintenance, nor does it include costs-effectiveness assessments based on quality-adjusted life years, thus restricting the broader healthcare perspective. Future randomized controlled trials should incorporate larger sample sizes, extended follow-up periods, and more comprehensive cost-effectiveness analyses to strengthen the robustness and generalizability of these findings.
Conclusion
In summary, the double-catheter IDDS strategy, which entails the concurrent placement of two catheters to address pain at multiple locations, such as concurrent refractory cancer pain in the neck and abdomen, presents a new alternative for patients experiencing refractory cancer pain. However, it is essential to acknowledge that the retrospective design of this study, combined with a limited observation period and a small sample size, necessitates further investigation to clarify the potential benefits and risks associated with this novel surgical approach.
Data availability
The comprehensive data outlined in the paper is provided in the Methods and Results sections. For further information or additional data details, readers are encouraged to reach out to the corresponding author.
Abbreviations
- BMI:
-
body mass index
- BTP:
-
Breakthrough pain
- CNY:
-
Chinese Yuan
- CSF:
-
Cerebrospinal fluid
- DSA:
-
Digital subtraction angiography
- EBP:
-
Epidural blood patches
- IDDS:
-
Intrathecal drug delivery systems
- IDMED:
-
Intrathecal morphine dose
- NA:
-
Not available
- NRS:
-
Numeric rating scale
- ODMED:
-
Oral daily morphine dose
- PCA:
-
Patient-controlled analgesia
- PSM:
-
Propensity score matching
References
Mercadante, S. Refractory Cancer Pain and Intrathecal Therapy: critical review of a systematic review. Pain Ther. 12 (3), 645–654 (2023).
Afsharimani, B., Kindl, K., Good, P. & Hardy, J. Pharmacological options for the management of refractory cancer pain-what is the evidence? Support Care Cancer. 23 (5), 1473–1481 (2015).
Brozović, G., Lesar, N., Janev, D., Bošnjak, T. & Muhaxhiri, B. Cancer pain and therapy. Acta Clin. Croat. 61 (Suppl 2), 103–108 (2022).
Perruchoud, C., Dupoiron, D., Papi, B., Calabrese, A. & Brogan, S. E. Management of Cancer-Related Pain with Intrathecal Drug Delivery: a systematic review and Meta-analysis of Clinical studies. Neuromodulation 26 (6), 1142–1152 (2023).
Hindle, A. Intrathecal opioids in the management of acute postoperative pain. Continuing Educ. Anaesth. Crit. Care Pain. 8 (3), 81–85 (2008).
Deer, T. R. et al. The Polyanalgesic Consensus Conference (PACC): Recommendations for Trialing of Intrathecal Drug Delivery Infusion Therapy. Neuromodulation 20(2), 133–154 (2017).
Zhou, H. et al. Prepontine cisternal routine for intrathecal targeted drug delivery in craniofacial cancer pain treatment: technical note. Drug Deliv. 29 (1), 3213–3217 (2022).
Mastenbroek, T. C., Kramp-Hendriks, B. J., Kallewaard, J. W. & Vonk, J. M. Multimodal intrathecal analgesia in refractory cancer pain. Scand. J. Pain. 14, 39–43 (2017).
Jain, S., Malinowski, M., Chopra, P., Varshney, V. & Deer, T. R. Intrathecal drug delivery for pain management: recent advances and future developments. Expert Opin. Drug Deliv. 16 (8), 815–822 (2019).
Spiegel, M. A. et al. Evaluation of an Intrathecal Drug Delivery Protocol leads to Rapid reduction of systemic opioids in the Oncological Population. J. Palliat. Med. 24 (3), 418–422 (2021).
Zhang, A., Wang, H., Li, Q. & Chen, C. Double-catheter intrathecal targeted drug delivery systems for the treatment of neck and abdominal cancer pain. Asian J. Surg. (2024).
Newsome, S., Frawley, B. K. & Argoff, C. E. Intrathecal analgesia for refractory cancer pain. Curr. Pain Headache Rep. 12 (4), 249–256 (2008).
Portenoy, R. K. & Hagen, N. A. Breakthrough pain: definition, prevalence and characteristics. Pain 41 (3), 273–281 (1990).
Zhang, H. Cancer Pain Management-New therapies. Curr. Oncol. Rep. 24 (2), 223–226 (2022).
Flack, S. H., Anderson, C. M. & Bernards, C. Morphine distribution in the spinal cord after chronic infusion in pigs. Anesth. Analg. 112 (2), 460–464 (2011).
Zou, D., Zhang, W. & Wang, Y. Prepontine cistern intrathecal targeted drug delivery for cancer-related craniofacial pain. Pain Med. 22 (12), 3112–3114 (2021).
Zhou, L. & Guo, Z. Intrathecal analgesia via a percutaneous port with patient-controlled intrathecal analgesia for the management of movement-evoked breakthrough cancer pain of refractory lower extremity cancer pain: a retrospective review. Pain Phys. 26 (4), 375–382 (2023).
Belverud, S. A., Mogilner, A. Y. & Schulder, M. Intrathecal bupivacaine for head and neck pain. Local. Reg. Anesth. 3, 125–128 (2010).
Wang, W., Shi, Q., Cao, Y., Fan, B. & Yang, Y. Intrathecal drug delivery systems for cancer pain: a retrospective analysis at a single tertiary medical center in China. Heliyon 10 (14), e34522 (2024).
Ummenhofer, W. C., Arends, R. H., Shen, D. D. & Bernards, C. M. Comparative spinal distribution and clearance kinetics of intrathecally administered morphine, fentanyl, alfentanil, and sufentanil. Anesthesiology 92 (3), 739–753 (2000).
Burns, M. L. et al. Variation in intraoperative opioid administration by patient, clinician, and hospital contribution. JAMA Netw. Open. 7 (1), e2351689 (2024).
Qin, W. et al. Comparison of external system and implanted system in intrathecal therapy for refractory cancer pain in China: a retrospective study. Brain Behav. 13 (1), e2851 (2023).
Løhre, E. T., Thronæs, M. & Klepstad, P. Breakthrough cancer pain in 2020. Curr. Opin. Support Palliat. Care. 14 (2), 94–99 (2020).
Sindt, J. E., Odell, D. W., Dalley, A. P. & Brogan, S. E. Initiation of intrathecal drug delivery dramatically reduces systemic opioid use in patients with advanced cancer. Neuromodulation 23 (7), 978–983 (2020).
Abrecht, C. R., Greenberg, P., Song, E., Urman, R. D. & Rathmell, J. P. A contemporary medicolegal analysis of implanted devices for chronic pain management. Anesth. Analg. 124 (4), 1304–1310 (2017).
Huang, M., Dalm, B. & Simpson, R. K. Toxic myelitis and arachnoiditis after intrathecal delivery of bupivacaine via an implanted drug delivery system: case report and review of the literature. Cureus 10 (2), e2240 (2018).
Saifuddin, A., Burnett, S. J. & White, J. The variation of position of the conus medullaris in an adult population. A magnetic resonance imaging study. Spine (Phila Pa. 1976). 23 (13), 1452–1456 (1998).
Mohammed, H., Madipola, N., Chawda, S. & de Silva, R. N. Terson’s syndrome following epidural blood patch for spontaneous intracranial hypotension. Pract. Neurol. 23 (5), 434–435 (2023).
Uppal, V. et al. Evidence-based clinical practice guidelines on postdural puncture headache: a consensus report from a multisociety international working group. Reg. Anesth. Pain Med. 49 (7), 471–501 (2024).
Cotogni, P. et al. : The role of nutritional support for Cancer patients in Palliative Care. Nutrients 13(2). (2021).
Smith, T. J. et al. Randomized clinical trial of an implantable drug delivery system compared with comprehensive medical management for refractory cancer pain: impact on pain, drug-related toxicity, and survival. J. Clin. Oncol. 20 (19), 4040–4049 (2002).
Kleinmann, B. & Wolter, T. Intrathecal Opioid Therapy for Non-malignant Chronic Pain: a long-term perspective. Neuromodulation 20 (7), 719–726 (2017).
Acknowledgements
The authors would like to thank Dr Hongzhen Zhou from Department of pain, the Second Affiliated Hospital of Guangxi Medical University for Statistical Analysis and thank her for guiding our team to complete this article.
Funding
This research was supported by Natural Science Foundation of Guangxi (Grant No. 2020GXNSFAA297101; Grant No. 2020GXNSFBA238020) and medical research project in Sichuan Province (Grant No. S21052) and Natural Science Foundation of Sichuan (Grant No. 2022NSFSC1346) and Natural Science Foundation of Guangxi University of Chinese Medicine (Grant No.2019MS050) and the Bethune Charitable Foundation (NO. ezmr2023-031).
Author information
Authors and Affiliations
Contributions
Qin Li, Huaiming Wang and Aimin Zhang were involved in the conception and study design. Qin Li and Qiju Li were responsible for document retrieval. Qin Li, Bo Zhong and Aimin Zhang were involved in the writing and revision of the manuscript. Maoxia Xu,Xin Hu and Pengjiu Feng were responsible for the data analysis. Jiang Zou and Aimin Zhang were in charge of concept design, article proofreading and project guidance. All authors were responsible for critical revision of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All included patients gave their oral and written informed consent. The study was approved by the Ethics Committee (full name: the Ethics Committee of Sichuan Provincial Cancer Hospital) (reference number SCCHEC-03-2024-071) to the Department of Anesthesiology, Sichuan Cancer Hospital & Institute.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, Q., Wang, H., Li, Q. et al. Efficacy and safety of single and double catheter intrathecal drug delivery systems in patients with refractory neck and abdominal cancer pain. Sci Rep 14, 32072 (2024). https://doi.org/10.1038/s41598-024-83799-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-83799-1