Abstract
Cataract surgery, a common procedure for vision restoration, exhibits variable outcomes based on patient demographics. This study aimed to elucidate the effects of age and sex on risk factors, intraoperative complications, and postoperative outcomes of cataract surgery. A single-center retrospective cohort study analyzed 691 eyes from 589 individuals who underwent surgery at a tertiary referral center, using electronic medical records to assess preoperative risk factors, intraoperative complications, and best corrected visual acuity (BCVA) pre- and post-operatively, alongside demographic data. The study found that males aged 65–75 years had significantly higher rates of functional postoperative BCVA (91% for males vs. 79% for females, p = 0.007), a disparity not attributable to differences in surgical complications or risk factor prevalence. Age-specific thresholds were identified where BCVA improvements significantly declined beyond 65 years for females and 75 years for males. The likelihood of worsened BCVA post-surgery increased with age for both sexes, with a notable decline in BCVA improvement between the 55–65 years and 65–75 years age groups. These findings underscore the critical influence of sex and age on cataract surgery outcomes, advocating for the integration of these factors into preoperative evaluations to better tailor the timing and planning of cataract surgery and optimize clinical outcomes.
Similar content being viewed by others
Introduction
Cataract affects roughly 95 million people worldwide and is the predominant cause of blindness in developing nations1 The surgery, prevalent in advanced countries, substantially improves patients’ quality of life and safety2,3,4.
Despite advancements, cataract surgery poses risks, influenced by patient profiles, surgeon expertise, and cataract type, potentially impacting outcomes. Identifying these factors is vital to enhance surgery success and safety.
The Cataract National Dataset (CND) reveals how factors such as age, sex, comorbidities, and surgeon skill correlate with complication risks like posterior capsule rupture5. It supports a risk assessment system predicting individual outcomes, considering factors including age, sex, diabetes, and UV exposure6,7. While males and females undergo cataract surgery at similar rates8, females report poorer visual function outcomes and postoperative care9,10,11,12. It’s uncertain if this gender disparity persists across age groups or if specific risk factors and intraoperative complications contribute to these results.
Increasing age correlates with worse refractive results and satisfaction after cataract surgery, with those over 75 less likely to see improvement8,9,13. It remains uncertain if these age-related declines affect males and females equally or at what age the decline is most pronounced14.
In cataract surgery, the surgeon’s expertise and the level of supervision significantly affect complications and visual results. A large-scale study with 48,377 cases found that residents had higher complication rates than experienced surgeons but achieved comparable visual outcomes, due to varied case types and close supervision. Risk factors for poor visual results included age over 65 and specific complications like dropped nuclei or post-surgical retina, cornea, and lens issues15.
Puri et al. explored how supervisory experience affects phacoemulsification outcomes when performed by residents. They found that residents supervised by less experienced surgeons encountered more issues, like vitreous loss and anterior capsule tear, indicating a learning curve in surgical skill development16. However, the research didn’t consider sex-based differences, suggesting an area for further study on sex’s influence on surgical outcomes.
Given the projected rise in cataracts from an aging population, personalized medical and public health strategies addressing patient-specific demographics and risks are crucial for better surgical outcomes6.
This study examines how patient demographics, especially age and sex, and resident surgeon expertise affect cataract surgery outcomes. It focuses on the role of these demographics and other risk factors in surgery efficacy and complications under resident supervision. A key goal is to discern sex-based disparities in outcomes among different age groups, and whether sex impacts surgery success consistently or varies with age, thus offering insights into the interplay of demographic factors and surgical experience on cataract surgery success.
Methods
Study population
This study used retrospective data from January 2018 to February 2022, from Hadassah Medical Center’s ophthalmology department, considering patients with cataract surgeries by residents. Exclusions were for missing preoperative assessments or incomplete data.
In Israel, ophthalmology residents start a five-year program, engaging in surgeries from late in the first year. Complex or high-risk surgeries are allotted to seasoned residents or attendings.
The study received ethical approval from the institutional Helsinki Committee (HMO-0459-18), aligning with the Declaration of Helsinki and ensuring patient confidentiality.
Each surgery was treated as a separate event due to the potential differences in complications and outcomes between eyes of the same patient, which is critical for evaluating the impact of age and sex on surgical risks and results.
Risk assessment in participants
Before surgery, a risk assessment based on a 0–22 scoring system evaluated patient factors like age, axial length, and cataract severity, alongside conditions such as Diabetic Retinopathy and prior ocular procedures. Higher scores suggested greater complication risk17.
Monitoring surgical complications
Surgical reports were meticulously reviewed for complications using predefined search terms. Thirteen types were recorded, including capsule tears, vitreous loss, and lens dislocation, among others, noting their occurrence and timing during surgery.
Evaluation of surgical outcomes
Surgical outcomes were assessed by comparing pre- and post-operative best corrected visual acuity (BCVA, LogMAR units). The improvement rate was calculated using the formula: (pre-operative BCVA—post-operative BCVA)/pre-operative BCVA. Cases meeting Israeli driving vision standards (BCVA under 0.3 LogMAR) were highlighted and defined as functional BCVA. Also noted were cases without BCVA improvement. The study focused on 656 patients with complete one-year visual data to assess short-term outcomes.
Statistical analysis
The D’Agostino-Pearson test checked for normality; the Mann–Whitney and Student’s T-tests analyzed non-normal and normal distributions, respectively. The Z proportion test compared categorical variables, and the Chi-Square Test determined sex differences across ages. Bonferroni’s correction controlled for multiple comparisons, with significance set at p < 0.05/number of comparisons. Cohort comparisons only included groups with n > 30 for robust analysis. Age stratification was by decade, and Scipy in Python was used for analysis18.
Results
Characteristics of patients
The study analyzed 691 eyes from 589 patients. Patients’ mean age was 71.5 ± 10.7 years, with a range of 24–97 years, and 49% were female. Cataract surgeries increased with age, peaking at 65–75 years and decreasing after 75, especially beyond 85 years. The age distribution of surgeries, depicted in Figure A.1 in the supplementary material, showed no significant sex differences (p = 0.47). Preoperative BCVA averaged 0.71 ± 0.71 LogMAR, improving to 0.24 ± 0.33 postoperatively—a 58.8 ± 36.4% mean increase.
Risk factors for surgical complications
Sex-based Prevalence of Risk Factors
Risk factor analysis, presented in Table 1, revealed no sex-based differences except for oral alpha-1 antagonists, significantly more common in males (23.9%) than females (1.2%; p < 0.001). Females averaged fewer risk factors (0.59 ± 0.79) than males (0.86 ± 1.0; p < 0.001) and had a lower preoperative cataract score (2.6 ± 2.5 vs. 3.1 ± 2.8; p = 0.03).
Age-related risk factor analysis
Patients with small pupils, using oral alpha-1 antagonists, or with phacodonesis and dense cataract were older on average (74.9 ± 9.7, 77.1 ± 9.1, and 78.2 ± 10.4 years, respectively) than those without these risk factors (70.7 ± 11.0, 70.5 ± 10.9, and 71.1 ± 10.8 years, respectively; p < 0.001). Conversely, patients with diabetic retinopathy were younger than those without it (66.7 vs. 71.7 years; p = 0.001). Table 2 lists mean ages for groups with and without certain risk factors; no significant age differences were noted for shallow anterior chamber or poor patient cooperation.
Stratified analysis showed age-related trends in risk factor prevalence, which are illustrated in Figure A.2 in the supplementary files. The prevalence of extreme axial length (< 21.5 or > 30 mm) decreased from the under-55 age group to the 55–65 age group (from 8.6 to 0.9%; p = 0.01), but this wasn’t significant after Bonferroni adjustment. The prevalence of oral Alpha-1 antagonist use rose from the 55–65 to the 65–75 age group (from 3.6 to 11.6%; p = 0.01), while diabetic retinopathy (DR) decreased (from 14.7 to 7.9%; p = 0.05), neither remaining significant post-adjustment.
A marked increase in risk factors like phacodonesis (from 3.8 to 15.5%; p = 0.001) and dense cataract (from 36.3 to 60.3%; p = 0.001) was noted between the 75–85 and the above- 85 age group. DR prevalence declined with age. For a comprehensive risk factor comparison stratified by age and sex, refer to Figure A.3 in the supplementary documents.
Surgery complications
Sex-based prevalence of complications
A sex-based comparison of post-surgery complication rates revealed no significant differences between male and female patients. Detailed analyses by age and sex, are presented in Table A.1 and Figure A.4 in the supplementary materials.
Influence of patient’s age on surgery complications
Stratification by age showed varying complication rates; Posterior Chamber (PC) tear and vitreous loss differed across ages. Iris complication prevalence rose in patients over 85 compared to those 75–85 years (6.9% vs. 1%; p = 0.006), though this trend was not statistically significant after Bonferroni correction. For visual data, please see Figure A.5 in the supplementary materials.
Surgery outcomes
Effect of patient age on surgical outcomes
An age-stratified analysis assessed the impact on Best Corrected Visual Acuity (BCVA) improvement (Fig. 1). All ages saw gains, but the increase diminished significantly from 72% in those aged 55–65 to 61% in the 65–75 bracket, and down to 51% in the 75–85 years range (p = 0.002 and p = 0.0004, respectively). Post-operative BCVA was significantly better in younger patients. The 75–85 age group had a worse average BCVA than the 65–75 group (p = 0.01), and those over 85 had even higher (poorer) BCVA than the 75–85 age group (p = 0.03). Post-Bonferroni correction, these differences were not statistically significant.
Comparative Analysis of Pre- and post-operative Best Corrected Visual Acuity (BCVA) and Percentage of Improvement Across Age Groups. The dual-axis graph presents Best Corrected Visual Acuity (BCVA) measured in LogMAR before (blue bars) and after (orange bars) cataract surgery, alongside the percentage of visual acuity improvement (red line), across five distinct age groups. The left vertical axis corresponds to the BCVA values, with lower scores indicating better visual acuity. The right vertical axis denotes the percentage of BCVA improvement, with higher values representing greater visual recovery. Error bars indicate the standard deviation (SD) within each age group, providing a measure of variability around the mean BCVA scores. Statistical significance between consecutive age groups, following Bonferroni correction for multiple comparison, is marked by the respective p-value, illustrating the differential impact of surgery on visual outcomes by age.
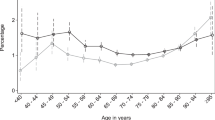
Further analysis, with sex stratification shown in Fig. 2, indicated significant age-related differences in visual acuity improvement post-surgery. Females over 65 years showed a significant reduction in improvement, from 0.76 ± 0.2 in the 55–65 age group to 0.58 ± 0.2 in the 65–75 group (p = 0.003). For males, a significant decrease in improvement was observed after age 75, from 0.64 ± 0.3 in the 65–75 group to 0.52 ± 0.3 in the 75–85 group (p = 0.002). Overall, males had a higher improvement percentage in most age groups, except for the 55–65 age group, where females had better outcomes.
Stratified Visual Acuity Outcomes by Age Group and Sex Before and After Surgery. Best Corrected Visual Acuity (BCVA) measured in LogMAR for males (blue and dark green bars for pre-operative and post-operative, respectively) and females (red and light green bars for pre-operative and post-operative, respectively) across different age groups. Additionally, the lines indicate the percentage of visual acuity improvement post-surgery for each sex (male in blue, female in red). The left vertical axis corresponds to BCVA values, with lower scores indicating better visual acuity, while the right vertical axis represents the improvement percentage. Error bars indicate the standard deviation (SD) within each age group, providing a measure of variability around the mean BCVA scores. Statistically significant differences, post Bonferroni correction for multiple comparisons, between consecutive age groups are noted with p-values, showing how surgical outcomes and recovery rates vary with age and between sexes. 'M' denotes males, 'F' denotes females, and ‘VA’ stands for Visual Acuity.
Further, the study found variations in BCVA before and after surgery. For females, pre-operative BCVA differed significantly between the 55–65 and 65–75 age groups (1.24 ± 0.99 vs. 0.73 ± 0.75, p = 0.009), and between the 75–85 and over 85 age groups (0.53 ± 0.44 vs. 0.84 ± 0.64, p = 0.006). For males, a significant difference in post-operative BCVA was noted between the 65–75 and 75–85 age groups (0.17 ± 0.18 vs. 0.24 ± 0.28, p = 0.005). In the under-55 group, pre-operative BCVA was notably lower in males than females (0.74 ± 0.68 vs. 1.19 ± 1.08, p = 0.01). Given the small size of the male cohort (n = 12), these results should be interpreted with caution.
In-depth analysis showed more males had functional (under 0.3 BCVA, LogMAR) post-operative BCVA across age groups, significantly so in those aged 65–75 (males 91% vs. females 79%, p = 0.007), as shown in Fig. 3.
Sex-Based Comparison of Functional Pre- and Post-Operative BCVA Across Age Groups. The left graph compares the percentages of functional pre-operative Best Corrected Visual Acuity (BCVA) (< 0.3 LogMAR) between females and males across various age groups. The right graph mirrors this comparison for post-operative BCVA, highlighting the significant sex differences in visual acuity outcomes. Point of statistical significance marked with the respective p-value.
Analyzing by sex alone, males had a significantly higher rate of functional post-operative BCVA than females (86% vs. 79%, p = 0.01), with both genders showing the same rate of functional pre-operative BCVA (34%), as shown in Table A.2 in supplementary. This aligns with greater BCVA improvement in males aged 65–75 years and above.
When examining changes in BCVA post-surgery by age, a clear pattern emerged: the likelihood of no improvement or worsening BCVA increased with patient age for both genders. Females had higher rates of these outcomes in every age category. A notable amount of females under 55 years showed no BCVA improvement post-surgery, as detailed in Figure A.6 in the supplementary materials.
Discussion
In this study we evaluated the association of age and sex with risk factors, intraoperative complications, and postoperative BCVA outcomes in cataract surgery.
Sex-specific findings showed equal surgery rates across genders, consistent with previous studies9. Post-surgery, males typically had better outcomes. Notably, feamles over 65 years old had higher functional preoperative BCVA, whereas males were more likely to achieve superior functional postoperative BCVA, especially noticeable in the 65–75 age group. Males also showed more significant visual acuity improvements across most age groups, except for those 55–65 years, where females, starting from a higher preoperative BCVA, improved more.
The findings correspond with earlier studies showing females often have less favorable surgical outcomes12,19. These disparities prompt further investigation into their consistency across age groups and possible links with pre-operative risks or intra-operative complications in females.
Our analysis didn’t find notable sex-based differences in surgical complications, which contrasts with findings from Geiger et al.20 and Morano et al.21, that observed more postoperative complications in males. Our data did show males have a higher use of oral alpha-1 antagonists, which increases with age and is linked to intraoperative floppy iris syndrome (IFIS)22,23,24,25,26,27. Given these drugs are also prescribed for conditions like COVID-19/SARS, Parkinson’s disease, PTSD28 and urinary symptoms in females29,30,31 vigilance for IFIS is necessary during cataract surgery for both sexes.
Despite more males under 55 years having risk factors like Oral-alpha and diabetic retinopathy, it didn’t lead to more postoperative complications, highlighting the complexity of factors influencing surgical outcomes. The observed postoperative discrepancies between sexes, therefore, could not be explained by risk factors or complications, pointing to the potential influence of subjective aspects like BCVA assessment.
Studies have shown that females report lower visual acuity than males, a discrepancy potentially related to their lesser engagement in post-surgery care such as laser capsulotomy and refractive error correction, according to VF14 questionnaire results pre- and 4 months post-surgery9,11. Subjective measures and psychosocial factors could also play a role in shaping these sex-specific perceived outcomes after surgery. Thus, while our findings align with previous reports of males achieving better postoperative outcomes, the reasons for this advantage are not yet clear since they don’t correspond to risk factors or complications. This emphasizes the need to factor in both physiological and psychological elements when assessing postoperative success across genders9.
Most cataract surgery patients were 65–75 years old, despite literature indicating increased cataract occurrence with age8. This may suggest a shift towards surgeries for visual enhancement, which could also be influenced by our institutional practices where residents are less likely to perform surgeries on the very elderly17. An important finding from our research is the impact of age on cataract surgery results, especially in BCVA enhancement. We identified gender-related age thresholds where BCVA gains decline—post-65 years for females and post-75 for males—which are critical considerations for surgical timing. While younger patients typically experience more significant enhancements in postoperative BCVA, a trend consistent with other studies32,33, it’s crucial to note that all age groups benefit from surgery. Patients over 85 years still achieve notable improvement, averaging 50% better BCVA, with 65% reaching functional vision post-surgery for both genders. These outcomes argue against delaying surgery for the elderly due to significant life quality impacts and increased fall risks34. Even those over 96 years have meaningful visual gains, although reduced compared to younger individuals, possibly due to more severe age-related maculopathy32,35.
Moreover, our research identified age-related risk factors for cataract surgery that affect both genders. These include oral alpha-1 antagonists use, small pupil size, phacodonesis, and dense cataracts, all of which increase with age. These conditions are often linked to pseudoexfoliation (PXF), the accumulation of fibrillar material in ocular tissues, complicating surgery36,37,38,39.
Contrary to other risk factors, patients with diabetic retinopathy (DR) were notably younger than those without, suggesting diabetes may hasten cataract development, requiring sooner surgery. This aligns with studies designating DR as an indicator for early cataract surgery40,41.
Addressing the limitations of our study, the limited number of patients with specific complications may have influenced the statistical significance of age-related differences. Additionally, the retrospective design and potential Electronic Medical Record (EMR) data limitations may have led to missing nuanced or unrecorded complications, such as intraoperative floppy iris syndrome. Despite these challenges, we implemented stringent data validation methods to enhance reliability. The focus on resident-performed surgeries and the single-center nature of the study could restrict the applicability of our findings to wider surgical practices and settings. Moreover, while our one-year follow-up conforms to common practices, it might not be sufficient to detect long-term complications or the persistence of visual acuity improvements. A more extended follow-up, inclusive of a wider array of surgeons across multiple institutions, could yield more comprehensive insights into the long-term effects of cataract surgery.
Conclusions
Our comprehensive analysis has underscored the critical roles of sex and age in determining the outcomes of cataract surgery. Notably, the distinct patterns observed in female’s postoperative results underscore the inadequacy of relying solely on traditional clinical metrics. These patterns affirm the importance of incorporating a broader range of physiological and psychological factors into preoperative assessments and postoperative care plans to optimize surgical outcomes.
Data availability
The datasets used or analyzed during the current study available from the corresponding author on reasonable request.
References
Liu, Y. C., Wilkins, M., Kim, T., Malyugin, B. & Mehta, J. S. Cataracts. Lancet 390, 600–612 (2017).
Cullen, K. A., Hall, M. J. & Golosinskiy, A. Ambulatory surgery in the United States, 2006. Natl. Health Stat. Rep. 28, 1–25 (2009).
Hatch, W. V., Campbell, E. D. L., Bell, C. M., El-Defrawy, S. R. & Campbell, R. J. Projecting the growth of cataract surgery during the next 25 years. Arch. Ophthalmol. 130, 1479–1481 (2012).
Lamoureux, E. L., Fenwick, E., Pesudovs, K. & Tan, D. The impact of cataract surgery on quality of life. Curr. Opin. Ophthalmol. 22, 19–27 (2011).
Narendran, N. et al. The cataract national dataset electronic multicentre audit of 55,567 operations: Risk stratification for posterior capsule rupture and vitreous loss. Eye (Lond) 23, 31–37 (2009).
McCarty, C. A., Mukesh, B. N., Fu, C. L. & Taylor, H. R. The epidemiology of cataract in Australia. Am. J. Ophthalmol. 128, 446–465 (1999).
Lewis, A. et al. Cataract surgery and subtype in a defined, older population: the SEECAT Project. Br. J. Ophthalmol. 88, 1512–1517 (2004).
Seah, S. K. L., Wong, T. Y., Foster, P. J., Ng, T. P. & Johnson, G. J. Prevalence of lens opacity in Chinese residents of Singapore: The Tanjong Pagar survey. Ophthalmology 109, 2058–2064 (2002).
McKee, M., Whatling, J. M., Wilson, J. L. & Vallance-Owen, A. Comparing outcomes of cataract surgery: Challenges and opportunities. J. Public Health (Bangkok) 27, 348–352 (2005).
Hughes, R., Aristodemou, P., Sparrow, J. M. & Kaye, S. Surgeon effects on cataract refractive outcomes are minimal compared with patient comorbidity and gender: An analysis of 490 987 cases. Br. J. Ophthalmol. 107, 488–494 (2023).
Hashemi, H. et al. The role of demographic characteristics in the outcomes of cataract surgery and gender roles in the uptake of postoperative eye care: A hospital-based study. Ophthalmic Epidemiol. 19, 242–248 (2012).
Quintana, J. M. et al. Relationship of sociodemographic variables with outcomes after cataract surgery. Eye 27, 698–708 (2013).
Schein, O. D. et al. Predictors of outcome in patients who underwent cataract surgery. Ophthalmology 102, 817–823 (1995).
Hashemi, H. et al. The role of demographic characteristics in the outcomes of cataract surgery and gender roles in the uptake of postoperative eye care: A hospital-based study. Ophthalmic. Epidemiologypidemiol. 19, 242–248 (2012).
Ti, S. E., Yang, Y. N., Lang, S. S. & Chee, S. P. A 5-year audit of cataract surgery outcomes after posterior capsule rupture and risk factors affecting visual acuity. Am. J. Ophthalmol. 157, 180 (2014).
Puri, S. et al. Comparing resident cataract surgery outcomes under novice versus experienced attending supervision. Clin. Ophthalmol. 9, 1675–1681 (2015).
Cnaany, Y. et al. Ophthalmology residents’ experience in cataract surgery: Preoperative risk factors, intraoperative complications, and surgical outcomes. Ophthalmol. Therapy 8, 1541. https://doi.org/10.21203/RS.3.RS-3991746/V1 (2024).
Virtanen, P. et al. SciPy 1.0: Fundamental algorithms for scientific computing in Python. Nat. Methods 17, 261. https://doi.org/10.1038/s41592-019-0686-2 (2020).
Hashemi, H. et al. The role of demographic characteristics in the outcomes of cataract surgery and gender roles in the uptake of postoperative eye care: A hospital-based study. Ophthalmic. Epidemiol. 19, 242–248 (2012).
Geiger, M. D. et al. Are there sex-based disparities in cataract surgery?. Int. J. Ophthalmol. 17, 137–143 (2024).
Morano, M. J. et al. Incidence and risk factors for retinal detachment and retinal tear after cataract surgery: IRIS® registry (intelligent research in sight) analysis. Ophthalmology science 3, 100314 (2023).
Christou, C. D., Esagian, S. M., Ziakas, N., Prousali, E. & Tzamalis, A. Factors predisposing to intraoperative floppy-iris syndrome: An up-to-date meta-analysis. J. Cataract. Refract. Surg. 48, 1335–1341 (2022).
Blouin, M. C., Blouin, J., Perreault, S., Lapointe, A. & Dragomir, A. Intraoperative floppy-iris syndrome associated with alpha1-adrenoreceptors: Comparison of Tamsulosin and Alfuzosin. J. Cataract. Refract. Surg. 33, 1227–1234 (2007).
Kaczmarek, I. A., Prost, M. E. & Wasyluk, J. Clinical risk factors associated with intraoperative floppy iris syndrome: A prospective study. Int. Ophthalmol. 39, 541–549 (2019).
Karaca, U. et al. Evaluation of static and dynamic Pupillometry changes in men using Silodosin for benign prostatic hypertrophy. BMC Ophthalmol. https://doi.org/10.1186/s12886-021-01894-7 (2021).
Maluskova, M., Vidlar, A., Maresova, K., Lounova, V. & Karhanova, M. Floppy iris syndrome associated with specific medication intake: A narrative review. Biomed. Pap. Med. Fac. Univ. Palacky Olomouc. Czech Repub. 167, 9–15 (2023).
Herranz Cabarcos, A., Pifarré Benítez, R. & Martínez Palmer, A. Impact of intraoperative floppy IRIS syndrome in cataract surgery by phacoemulsification: Analysis of 622 cases. Arch. Soc. Esp. Oftalmol. 98, 78–82 (2023).
Perez, D. M. α1-adrenergic receptors: insights into potential therapeutic opportunities for COVID-19, heart failure, and Alzheimer’s disease. Int. J. Mol. Sci. 24, 4188 (2023).
Mansbart, F., Kienberger, G., Sönnichsen, A. & Mann, E. Efficacy and safety of adrenergic alpha-1 receptor antagonists in older adults: A systematic review and meta-analysis supporting the development of recommendations to reduce potentially inappropriate prescribing. BMC Geriatr. 22, 1–29 (2022).
Kim, D. K. et al. Alpha-1 adrenergic receptor blockers for the treatment of lower urinary tract symptoms in women: A systematic review and meta-analysis. Int. Neurourol. J. 23, 56 (2019).
Pischedda, A., Farina, F. P., Madonia, M., Cimino, S. & Morgia, G. Use of alpha1-blockers in female functional bladder neck obstruction. Urol. Int. 74, 256–261 (2005).
Jaycock, P. et al. The Cataract National Dataset electronic multi-centre audit of 55 567 operations: Updating benchmark standards of care in the United Kingdom and internationally. Eye 23, 38–49 (2009).
Muhtaseb, M., Kalhoro, A. & Ionides, A. A system for preoperative stratification of cataract patients according to risk of intraoperative complications: A prospective analysis of 1441 cases. Br. J. Ophthalmol. 88, 1242–1246 (2004).
Hodge, W. et al. The consequences of waiting for cataract surgery: A systematic review. CMAJ: Can. Medical Associat. J. 176, 1285 (2007).
Syam, P. P. et al. Clinical outcome following cataract surgery in very elderly patients. Eye 18, 59–62 (2004).
Plateroti, P., Plateroti, A. M., Abdolrahimzadeh, S. & Scuderi, G. Pseudoexfoliation syndrome and pseudoexfoliation glaucoma: A review of the literature with updates on surgical management. J. Ophthalmol. 2015, 1–9 (2015).
Borkenstein, A. F. & Borkenstein, E. M. Surgical experience with a redesigned, fully preloaded, hydrophobic acrylic intraocular lens in challenging cases of pseudoexfoliation syndrome, phacodonesis, and small pupils. Clin. Ophthalmol. 13, 199 (2019).
Buhbut, O. et al. Risk factors for a phacodonesis surprise during cataract surgery in patients with pseudoexfoliation. Int. Ophthalmol. 43, 4739–4746 (2023).
Grzybowski, A., Kanclerz, P., Huerva, V., Ascaso, F. J. & Tuuminen, R. Diabetes and phacoemulsification cataract surgery: Difficulties, risks and potential complications. J. Clin. Med. 8, 716 (2019).
Tomić, M. et al. Hypertension and hypercholesterolemia are associated with cataract development in patients with type 2 diabetes. High Blood Press. Cardiovasc. Prevent. 28, 475–481 (2021).
Kiziltoprak, H., Tekin, K., Inanc, M. & Goker, Y. S. Cataract in diabetes mellitus. World J. Diabetes 10, 140–153 (2019).
Acknowledgements
The authors express their gratitude to Dr. Ron Kaufman and Dr. Ori Saban for their valuable insights that enhanced this article.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by A.G., H.B., Y.C., M.H. and I.C. The first draft of the manuscript was written by H.B., A.G., and Y.C. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved and performed in accordance with the institutional Helsinki Committee (study #: HMO-0459-18). Due to the retrospective nature of the study, the Institutional Helsinki committee waived the need of obtaining informed consent. Data was collected from the Ophthalmology Department database and anonymized before analysis. This study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments. The institutional Helsinki committee exempts retrospective research from informed consent by the participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ben-Eli, H., Cnaany, Y., Halpert, M. et al. Investigating the impact of age and sex on cataract surgery complications and outcomes. Sci Rep 15, 1242 (2025). https://doi.org/10.1038/s41598-024-84382-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-84382-4
Keywords
This article is cited by
-
Preoperative prediction of intraoperative complications in cataract surgery: a machine learning approach
International Ophthalmology (2025)