Abstract
The aim of this study was to evaluate dental treatment outcomes and safety in the Intensive Care Unit (ICU). Data collected included the frequency of dental interventions, the incidence of ventilator-associated pneumonia (VAP), patient demographics, length of ICU stay, and mortality. In the statistical analysis, logistic regression models were utilized to explore associations between dental care and patient outcomes, calculating odds ratios for mortality outcomes, with adjustments for potential confounders. More than three interventions were associated with a lower risk of mortality in both crude (p < 0.0001) and adjusted analyses (p < 0.0001), suggesting a protective effect. Patients who received more frequent dental care demonstrated improved survival outcomes. VAP did not significantly increase mortality risk in this cohort (p = 0.3511). Dental procedures were not conclusively linked to a reduction in mortality; however, they were not associated with any important adverse effects, indicating that they are safe for ICU patients. The findings indicate that regular dental treatment in the ICU may be beneficial to patient survival and does not pose additional safety risks. While VAP did not independently predict mortality, receipt of comprehensive dental care was a protective factor.
Similar content being viewed by others
Introduction
Medicine has made significant advances in recent decades, yet despite technological progress, mortality rates in Intensive Care Units (ICUs) remain high, with variations between 13 and 16% incidence following admission1. In this context, one of the primary reasons for admission to these units is the need for mechanical ventilation due to a patient’s inability to breathe independently, which may be compromised by trauma, a medical condition, or recent surgery. These critically ill patients also rely on hospital staff to meet their basic needs, including nutrition and overall hygiene as well as oral hygiene required to be delivered2.
Patients in ICUs often lack adequate dental hygiene, which directly influences oral health issues that contribute to increased morbidity and mortality3. Poor oral health can lead spread of local infections and may increase risk of excess oral microbes being aspirated, potentially causing respiratory tract infections like ventilator-associated pneumonia (VAP), higher ICU hospitalization costs, and an increased need for medications such as antibiotics. This can result in bacterial resistance and opportunistic infections4,5,6,7,8. Oral health issues can have systemic impacts, evidenced by a bidirectional relationship between periodontal disease and renal disease9, and links between periodontal disease and acute myocardial infarction10, as well as between oral microbiota and various cardiovascular diseases, including infective endocarditis, rheumatic heart disease, heart failure, coronary artery disease, peripheral artery disease, and stroke11. Despite the significance of oral health, dental care, especially for major oral diseases like caries and periodontal disease, is often managed outside of the ICU by dentists who are not typically part of the ICU’s multidisciplinary team and who have limited evidence to guide safe practice within this context. Previously, in long-term care homes, professional oral health care (including dental hygienists) provided clinically onsite oral health services, reducing oral infections and associated cases of pneumonia and aspiration pneumonia12. In addition, preventive dental treatment within the 12 months prior to hospitalization or periodontal therapy within the 6 months prior was associated with a reduced risk of nonventilator hospital-acquired pneumonia13.
Several studies have investigated the role of dental care in Intensive Care Units (ICUs), primarily focusing on its potential to reduce mortality rates14,15,16,17,18. However, many of these studies are small in scale and may not provide a comprehensive understanding of the benefits and logistical considerations involved in integrating dental care into ICU management. Furthermore, there is significant variability in outcome measures across studies, as well as a lack of consensus on what constitutes optimal dental care for critically ill patients, including the recommended frequency of care and most effective interventions. Despite recent advances, these inconsistencies highlight the ongoing need for further investigation. The absence of standardized guidelines for oral care in ICUs also contributes to inconsistencies in patient care, underscoring the necessity of developing a solid evidence base to establish safe, standardized practices. Given these challenges and gaps, the rationale for the present study is to assess the outcomes and safety of dental involvement in ICUs through a six-year retrospective analysis, focusing on objective metrics such as mortality rates, length of hospital stay, and the frequency of dental interventions to assess the impact of dental care on ICU patient outcomes.
Methods
Study design, data source and variables
An observational, longitudinal, and retrospective study was conducted in the adult ICU of the Regional Hospital of Ceilândia, a public hospital located in the Federal District, Brazil. The study received approval from the Research Ethics Committee of the Fundação de Ensino e Pesquisa em Ciências da Saúde (FEPECS) - Foundation for Education and Research in Health Sciences, under the number CAAE 86864618.4.0000.5553. All the procedures were performed in accordance with the ethical standards on human experimentation and with the Helsinki Declaration of 1975 and its later amendments. Informed consent was obtained from all participants and/or their legal guardians.
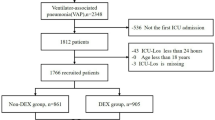
Data were obtained from the electronic medical records provided by the Trakcare – Intersystems database (Cambridge, MA, USA). The sample was convenience-based, involving all patients admitted during the study period. Records of admission and discharge from the adult ICU at Hospital Regional de Ceilândia (HRC) were used to identify patients. This study included all patients over 18 years old who were admitted to the ICU and were either already under mechanical ventilation or began ventilatory support after admission, with more than 48 consecutive hours of mechanical ventilation (MV). Exclusion criteria comprised patients who did not receive mechanical ventilation, developed pneumonia within the first 48 h of ventilation, were admitted with a diagnosis of ventilator-associated pneumonia (VAP) or another pulmonary infection, or stayed in the ICU for less than 48 h. There were no missing data during the study. Patients with readmissions, regardless of the timeframe, were counted as the same patient if they met the inclusion criteria. Patients were enrolled in the study regardless of their dental condition upon admission.
For the diagnosis of VAP, a clinical approach with a highly sensitive strategy was used: VAP was diagnosed only when there was no suspicion of other infection sites that could explain the observed clinical and radiographic findings. The presence of new or progressive radiographic infiltrate, along with at least one clinical finding suggestive of infection (including new onset fever, purulent sputum, leukocytosis, and declining oxygenation), was required19. The diagnosis was made independently by the ICU’s intensive care physician team.
The electronic medical records provided information about various patient variables, including gender, age, date of admission, date of ICU discharge, duration of mechanical ventilation, time until ICU discharge, presence or absence of VAP, outcome (discharge or death), and reasons for each patient’s hospitalization. To calculate the incidence of VAP, the incidence rate per 1,000 ventilator days was used. This method eliminated two potential biases: the days when the patient was not under MV and the differences between patients who spent a few days and those who spent many days on MV, with the latter having a higher likelihood of developing an infection.
Dental care
Dental care was administered from 2012 to 2017 by the same professional. Initially, dental services were offered for a limited number of hours each week; this availability was gradually increased over the years. The study grouped the patient population by each year to analyze trends.
All patients were treated in the ICU bed by the same dentist, who performed at each intervention: diagnostic evaluation, prophylactic removal of visible biofilm, and aspiration of oral and oropharyngeal secretions. The prophylactic removal of biofilm was performed using gauze soaked in chlorhexidine, pinched with metal instruments with a ratchet mechanism, similar to needle holders, and oral suction with a dental aspirator and oropharyngeal suction with a tracheal suction catheter. Additionally, when necessary, the dentist performed specific dental procedures to control potential infection foci, such as restorations or cavity sealing, extractions, and scaling, for example. All dental interventions (including procedures) were performed at the bedside, in the ICU environment itself. The protocol followed by the nursing team involved maintaining oral hygiene at least once a day using gauze soaked in 0.12% chlorhexidine, secured with adhesive tape to a wooden tongue depressor, and oral and oropharyngeal suction with a tracheal suction catheter (though adherence was not monitored). Here, chlorhexidine was used, although studies published after the start of this study have raised concerns about its effectiveness and the possibility that it may increase mortality in patients where it is used20.
Variables related to dental care, such as procedures performed and intervention dates, were also obtained from the electronic medical records. The average interval between interventions was calculated by dividing the number of hospitalization days by the number of interventions. Since dental extractions are more invasive and a secondary objective was to assess the safety of performing them, we chose to analyze their mortality risk separately from the other procedures.
Statistical analysis
For the analysis, variables including Sepsis/septic shock, External causes (such as gunshot wounds, blunt trauma, accidents, poisonings), Renal failure (both acute and exacerbated chronic), Postoperative complications (involving abdomen, thorax, gynecological areas, orthopedic issues), Cardiac alterations (including shock, cardiac arrest, tachyarrhythmia, cardiomyopathy, heart failure, hypertensive emergencies), Pulmonary alterations (such as pulmonary embolism, chronic obstructive pulmonary disease, acute respiratory distress syndrome), Liver cirrhosis, Hypovolemic shock, Pancreatitis/Pancreatic abscess, Neurological alterations (encompassing loss of consciousness, ischemic stroke, hemorrhagic stroke, traumatic brain injury (TBI), anoxic encephalopathy, neurosarcoidosis), and Other conditions (deep vein thrombosis, Leptospirosis, Meningitis) were analyzed year by year from 2012 to 2016. The data were presented in tabular form, where only absolute numbers and relative frequencies were analyzed. No statistical test was applied.
In addition, for statistical analysis, contingency tables were established between the analyzed variables and mortality. This was followed by the estimation of simple logistic regression models to calculate the crude odds ratios and their respective 95% confidence intervals. Subsequent analysis involved estimating multilevel multiple logistic regression models that accounted for variables at the individual level (first level) and the contextual level (the year as the second level), with the year treated as a contextual variable due to its association with specific patient cohorts. In the multivariable analysis, all variables with a p-value of ≤ 0.20 from the simple analyses were included, with those maintaining a p-value of ≤ 0.05 being retained in the final models. The adjusted odds ratios and their 95% confidence intervals were then derived from these multiple models. All analyses were conducted using the R software (R Core Team, 2018. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria), with a significance level set at 5%.
Results
It was observed that the study involved a population related to a generalist unit, with various reasons for hospitalization. A total population of 212 patients was included in the research, with a relative balance between the sexes and an average age of 52 years. Table 1 provides a summary of reasons for hospitalization in the ICU distributed over the years from 2012 to 2017. Post-operative care was the most common reason for hospitalization, followed by sepsis.
In Table 2, the procedures performed during the period are presented. It was observed that dental extractions were the most frequently performed procedure, accounting for 62.85% of all procedures. The remaining 37.14% included other procedures, in order to undergo separate statistical analysis.
Table 3 displays crude and adjusted analyses related to the mortality outcome. In the unadjusted analyses, significant correlations with mortality were observed for age, tooth extractions, and other dental procedures (including treatment for potential oral infections, suture removal, adjustments to removable dentures, cavity sealants, hemorrhage treatments, both supragingival and subgingival scaling, bruxism management, and salivary dysfunction treatments). Other significant factors were the length of ICU stay, the number of dental interventions, and the year of hospitalization (all with p < 0.05). A longer stay (> 14.5 days) was significantly associated with an increased risk of mortality in the crude analysis (OR: 2.98, p < 0.0001), indicating that patients with prolonged stays have a higher risk of dying. More than three dental interventions were significantly linked to reduced mortality. Patients hospitalized in 2012 were 3.83 times more likely to die than those in 2017 (95% CI: 1.20-12.27, p < 0.05).
Specifically, patients over 52 have a significantly higher risk of mortality after adjustment (adjusted OR: 2.63, p = 0.0024), but not in the crude analysis, suggesting other factors may confound the raw association.
Neither the duration of mechanical ventilation nor the presence of VAP were significantly associated with mortality (p > 0.3511). Overall, 12.3% of patients developed VAP, and 45.3% of these died. There was no significant relationship between the development of VAP and mortality (p > 0.05). The risk of death was lower in 2017 compared to 2012, 2014, and 2015 (p < 0.05). Age was a risk factor, with older patients having a higher mortality risk (p = 0.0024). From 2014 onward, the frequency of dental interventions increased, and the intervals between them significantly decreased (p < 0.05).
Discussion
This study suggests that more frequent dental care in the ICU is linked to several benefits, including the potential for reduced mortality rates when the number of dental interventions increases. To date, no studies in the existing literature have examined the number of dental interventions or the intervals between them, making this investigation a pioneer in the field. Additionally, it appears that the presence of VAP does not considerably influence patient outcomes. The research also confirmed the safety of conducting dental procedures on critically ill patients within a general hospital unit, regardless of their varying admission reasons, which may contribute to improved mortality rates. The results suggest that certain individual factors like age and frequency of dental interventions are considerable predictors of mortality in the ICU. The decrease in mortality risk associated with a longer length of stay was notable but was only observed in the crude analysis, suggesting that when other variables are accounted for, the length of stay alone may not be as strong a predictor of mortality. The year of admission was an important contextual factor, indicating improvements in ICU care or changes in practices over time.
In the analysis adjusted for individual factors, only age (p = 0.0024) and the number of dental interventions (p < 0.0001) were significantly associated with mortality. The study confirms that older patients are at an increased risk of mortality in the ICU, highlighting the need for customized care for this group, including specialized dental services. Supporting this, another study has linked older age with substantial functional decline and a higher prevalence of chronic conditions21. This earlier research suggests that serious infections in elderly patients are linked to poorer prognoses and increased complications. Due to factors such as malnutrition, age-related physiological and anatomical changes, a rise in severe chronic illnesses, and a decline in immune function, the elderly are more susceptible to infections. Likely because of these reasons, the present study found that patients over 52 years of age admitted to the ICU have a heightened risk of death, a factor that dental intervention alone cannot mitigate.
Concerning the finding that having more than three dental interventions was associated with lower mortality, this frequency of care emerged as a protective factor for patients. This observation introduces a fresh perspective on how consistent oral care may influence patient outcomes in the ICU. It is evident that patients with longer ICU stays tend to have more interventions. However, length of stay did not correlate significantly with mortality in the adjusted analysis, only in the unadjusted one (p = 0.0001). This suggests that the number of dental interventions is a more robust protective factor than the length of stay, as it was significant in both the crude (p < 0.0001) and adjusted analyses (p < 0.0001). As for the interval between interventions, no significant differences were noted (p = 0.6170), likely due to the absence of a control group—those without any interventions—which introduces bias into the study. A future study incorporating such a control group is warranted, but special attention must be paid to the ethical issues of withdrawing dental assistance where it is already routinely provided.
Various studies employing different methodologies have explored the impact of dental professionals in the ICU. One such study suggested that ICU patients who receive regular dental care, including oral hygiene and periodontal treatments, may see a reduced risk of mortality16. Conversely, other studies indicated that oral care provided by dental health teams does not substantially affect mortality rates in ICU patients15,18. However, it’s important to note that the last-mentioned study, a systematic review, included an analysis of a study where the dentist was not part of the multiprofessional team, which introduces a considerable bias to its conclusions.
Regarding mortality associated with VAP, its presence did not significantly impact outcomes (p = 0.3511), a finding that contrasts with parts of the existing literature. Some studies have reported that patients developing VAP may experience mortality rates exceeding 70%22, 60%23, or range from 0 to 60%, with an attributable mortality rate—deaths directly linked to the infection—of at least 13%24,25. It has been estimated that one-third to half of the deaths in patients who developed VAP are directly related to the infection and a previous study suggested an attributable mortality of 10%, with surgical patients and those of moderate disease severity showing an elevated risk22. Despite the cited data on all-cause mortality associated with VAP reaching up to 50%26, the contribution of VAP to ICU patient mortality remains a subject of debate. The comparable mortality rates observed in this study between patients with and without VAP may be attributable to the dental care interventions provided.
For patients receiving dental care, the controlled oral microbiota could result in a lower pathogenicity compared to those whose biofilm is not well-managed. The data suggest that mechanically ventilated patients who develop VAP, if treated by a dentist, may experience less severe infections, with reduced pathogenicity, more effective treatment responses, and more favorable prognoses. It is conceivable that the marked decline in mortality over the years is linked to a reduction in VAP incidence. A careful examination of the data allows us to propose that the dentist’s interventions may have contributed to the decreased mortality. However, this likely was not the sole contributing factor.
Improved oral hygiene has been suggested to reduce or remove respiratory pathogens, potentially preventing serious infections, especially in vulnerable patients4. In this sense, the dentist must develop, together with the multidisciplinary team, periodic training aimed at training to maintain low levels of biofilm16. Correspondingly, one study17 reported a reduction in mortality due to VAP from 10.33 to 0.73% following the implementation of a protocol involving a dentist’s participation in the ICU team. The association between dental procedures and lower mortality was observed in the crude analysis, implying that such interventions are safe and possibly beneficial in improving patient outcomes. The absence of a statistical difference in the adjusted analysis suggests that further research, with earlier interventions and a larger sample size, could provide more definitive evidence.
Supporting the safety of dental interventions, one study27 found no severe adverse events during dental treatments in ICU patients. This aligns with the findings of this study, where only mild adverse effects occurred, such as postoperative bleeding in some patients on anticoagulants, which were managed locally. This safety is contingent on the proper execution of the dental procedures, a conclusion also echoed by another recent study28.
Despite concerns about the safety of performing dental procedures in Intensive Care Units (ICUs), their execution is considered appropriate due to the advantageous conditions of the ICU setting. ICUs provide intensive monitoring, the availability of sedation, and reduce the need for costly patient transfers to surgical centers. Multidisciplinary support and round-the-clock patient monitoring in ICUs facilitate immediate postoperative care. Additionally, many ICU patients are at risk of developing long-term consequences or restrictions in accessing dental care, often necessitating in-hospital treatments. There are instances where dental treatment may be required before cardiac procedures, and in such cases, if ICU conditions are minimally adequate for procedure realization, it is recommended by ANVISA29 to perform these treatments promptly. Carrying out these procedures in the ICU can accelerate treatment, contribute to systemic health6, and reduce overall healthcare costs, also having broader public health implications by lowering expenses associated with treating severe cases.
In relation to mechanical ventilation duration, no significant statistical difference was found regarding mortality (p = 0.9041). Echoing this, other research highlights that quality improvement initiatives in observational studies have linked practices that reduce extubating times to decreased mortality. Similarly, some authors20 reported that spontaneous breathing trials are associated with shortened periods of mechanical ventilation and lower mortality.
The current study has some limitations. Firstly, it was retrospective, which may have led to data loss. Additionally, blinding was not feasible due to the nature of the dental interventions involved, and the groups were not matched for mortality risk at admission. This was also not a randomized clinical trial, which may limit the strength of the evidence. Future multicenter studies in countries with different economic statuses and larger sample sizes may provide more robust evidence of the effects observed in this study, contributing to a more conclusive assessment of the impact of dental care in ICUs.
The current study has multiple limitations. Firstly, as a retrospective analysis, there was a risk of data loss and incomplete records, which could limit the reliability of the findings. The study did not control for some potential confounding factors, such as variations in baseline oral health conditions, or differences in ICU staff training and protocols. These factors may influence patient outcomes and could have affected our results. For ethical reasons, it was not possible to establish a group without dental care, given that the service was already in place and it would not have been feasible to exclude patients from this treatment during the same period. To minimize this limitation, we chose to compare mortality among patients with varying levels of dental care (intervals greater or less than 3.5 days). However, future studies should standardize samples with a planned group without dental care for more accurate comparison. Additionally, blinding was not feasible due to the nature of the dental interventions, and groups were not matched based on mortality risk at admission, which may introduce bias. Since this was not a randomized clinical trial, the evidence level remains limited. Future multicenter studies with larger populations, in countries with different economic statuses, and consideration of these additional variables are recommended to validate and expand upon the findings of this study. Such studies could provide a more conclusive understanding of the impact of dental care on ICU patient outcomes.
Within the limits of the employed methodology, this study suggests that frequent dental interventions during hospitalization, addressing the removal of potential infection foci and removing visible biofilm and its retention sites, may be associated with reduced mortality rates. With this approach, the development of VAP did not appear to substantially increase the likelihood of death. Although it is not possible to categorically state that dental procedures were definitively related to the reduction in mortality, they were not associated with important adverse effects. These findings suggest that the involvement of dentists in ICU care may provide benefits to patients and is not associated with substantial safety concerns.
Data availability
Data used in this study is publicly available at Mendeley repository, https://data.mendeley.com/preview/x7rch5zxx4?a=17f4f515-ce83-4556-a20b-4a01d4031f1c.
References
Metaxa, V. et al. Palliative care interventions in intensive care unit patients. Intensive Care Med. 47, 1415–1425. https://doi.org/10.1007/s00134-021-06544-6 (2021).
Hua, F. et al. Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochrane Database Syst. Rev. 10, CD008367. https://doi.org/10.1002/14651858.CD008367.pub3 (2016).
Blum, D. F. C. et al. Influence of dentistry professionals and oral health assistance protocols on intensive care unit nursing staff. A survey study. Rev. Bras. Ter. Intensiva. 29, 391–393. https://doi.org/10.5935/0103-507X.20170049 (2017).
Scannapieco, F. A., Bush, R. B. & Paju, S. Associations between periodontal disease and risk for nosocomial bacterial pneumonia and chronic obstructive pulmonary disease. A systematic review. Ann. Periodontol. 8, 54–69. https://doi.org/10.1902/annals.2003.8.1.54 (2003).
Azarpazhooh, A. & Leake, J. L. Systematic review of the association between respiratory diseases and oral health. J. Periodontol. 77, 1465–1482. https://doi.org/10.1902/jop.2006.060010 (2006).
Morais, T. M. et al. Importance of dental work in patients under intensive care unit. Rev. Bras. Ter. Intensiva. 18, 412–417 (2006).
Gomes-Filho, I. S., Passos, J. S. & Seixas Da Cruz, S. Respiratory disease and the role of oral bacteria. J. Oral Microbiol. 2, 5811. https://doi.org/10.3402/jom.v2i0.5811 (2010).
Bansal, M., Khatri, M. & Taneja, V. Potential role of periodontal infection in respiratory diseases—A review. J. Med. Life 6, 244–248 (2013).
He, I. et al. Demystifying the connection between periodontal disease and chronic kidney disease—An umbrella review. J. Periodontal Res. 58, 874–892. https://doi.org/10.1111/jre.13161 (2023).
Nalliah, R. P., Basu, T. & Chang, C. H. Association between periodontal care and hospitalization with acute myocardial infarction. J. Am. Dent. Assoc. 153, 776–786e772. https://doi.org/10.1016/j.adaj.2022.02.003 (2022).
Tonelli, A., Lumngwena, E. N. & Ntusi, N. A. B. The oral microbiome in the pathophysiology of cardiovascular disease. Nat. Rev. Cardiol. 20, 386–403. https://doi.org/10.1038/s41569-022-00825-3 (2023).
Baker, D. et al. The association between accessing dental services and nonventilator hospital-acquired pneumonia among 2019 Medicaid beneficiaries. Infect. Control Hosp. Epidemiol. 44, 959–961 (2023).
Marusiak, M. J., Paulden, M. & Ohinmaa, A. Professional oral health care prevents mouth-lung infection in long-term care homes: A systematic review. Can. J. Dent. Hyg. 57, 180–190 (2023).
Honore, P. M., Afonso, E. D. P. & Blot, S. Dental care and hospital mortality in ICU patients. Am. J. Infect. Control 50, 714–715. https://doi.org/10.1016/j.ajic.2022.02.020 (2022).
Bellissimo-Rodrigues, W. T. et al. Effectiveness of a dental care intervention in the prevention of lower respiratory tract nosocomial infections among intensive care patients: A randomized clinical trial. Infect. Control Hosp. Epidemiol. 35, 1342–1348. https://doi.org/10.1086/678427 (2014).
Ribeiro, I. L. A. et al. Impact of a dental care intervention on the hospital mortality of critically ill patients admitted to intensive care units: A quasi-experimental study. Am. J. Infect. Control 50, 1156–1161. https://doi.org/10.1016/j.ajic.2022.01.022 (2022).
Sabino, B. C. et al. The impact of dental care intervention on ventilator-associate events: A quasi-experimental study. Am. J. Infect. Control. 50, 1055–1059. https://doi.org/10.1016/j.ajic.2021.11.026 (2022).
de Araújo, E. C. F., da Silva, R. O. & Raymundo, M. L. B. Does the presence of oral health teams influence the incidence of ventilator-associated pneumonia and mortality of patients in intensive care units? Systematic review. Spec. Care Dentist. 43, 452–463. https://doi.org/10.1111/scd.12785 (2023).
Society, A. T. & America, I. D. S. o. guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am. J. Respir Crit. Care Med. 171, 388–416. https://doi.org/10.1164/rccm.200405-644ST (2005).
Klompas, M., Li, L., Kleinman, K., Szumita, P. M. & Massaro, A. F. Associations between ventilator bundle components and outcomes. JAMA Intern. Med. 176, 1277–1283. https://doi.org/10.1001/jamainternmed.2016.2427 (2016).
Blot, S. et al. Prevalence, risk factors, and mortality for ventilator-associated pneumonia in middle-aged, old, and very old critically ill patients. Crit. Care Med. 42, 601–609. https://doi.org/10.1097/01.ccm.0000435665.07446.50 (2014).
Torres, A. et al. International ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia: guidelines for the management of hospital-acquired pneumonia (HAP)/ventilator-associated pneumonia (VAP) of the European Respiratory Society (ERS), European Society of Intensive Care Medicine (ESICM), European Society of Clinical Microbiology and Infectious diseases (ESCMID) and Asociación Latinoamericana Del Tórax (ALAT). Eur. Respir J. 50. https://doi.org/10.1183/13993003.00582-2017 (2017).
Chan, E. Y., Ruest, A., Meade, M. O. & Cook, D. J. Oral decontamination for prevention of pneumonia in mechanically ventilated adults: Systematic review and meta-analysis. BMJ 334, 889. https://doi.org/10.1136/bmj.39136.528160.BE (2007).
Melsen, W. G. et al. Attributable mortality of ventilator-associated pneumonia: A meta-analysis of individual patient data from randomised prevention studies. Lancet Infect. Dis. 13, 665–671. https://doi.org/10.1016/S1473-3099(13)70081-1 (2013).
Lee, S. et al. Chlorhexidine-related mortality rate in critically ill subjects in Intensive Care units: A systematic review and meta-analysis. Respir Care. 64, 337–349. https://doi.org/10.4187/respcare.06434 (2019).
Papazian, L., Klompas, M. & Luyt, C. E. Ventilator-associated pneumonia in adults: A narrative review. Intensive Care Med. 46, 888–906. https://doi.org/10.1007/s00134-020-05980-0 (2020).
Bellissimo-Rodrigues, W. T. et al. Is it necessary to have a dentist within an intensive care unit team? Report of a randomised clinical trial. Int. Dent. J. 68, 420–427. https://doi.org/10.1111/idj.12397 (2018).
Pains, M. B. et al. Infection control: Dental extractions in ICU patients and their relation to the exams. Concilium 23, 51–66. https://doi.org/10.53660/CLM-2388-23S15 (2023).
Brasil Agência Nacional de Vigilância Sanitária. Medidas de Prevenção de Infecção Relacionada à Assistência à Saúde. Brasília: Anvisa (2017). https://www.gov.br/anvisa/pt-br/centraisdeconteudo/publicacoes/servicosdesaude/publicacoes/caderno-4-medidas-de-prevencao-de-infeccao-relacionada-a-assistencia-a-saude.pdf/view (accessed 03 October 2023).
Acknowledgements
To Dr. Risomar de Sousa Alves and Dr. Maria Luisa Santos de Oliveira, I would like to express my sincere gratitude for the support and leadership you have provided that enabled the successful development and completion of this research. We could not have accomplished this work without the opportunities you provided.
Funding
All the study was carried out with the authors’ own resources, not obtaining any type of external funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection was performed by M.B.P., analysis was performed by A.F.L. and N.S.M. The first draft of the manuscript was written by M.B.P. and C.R.M.M., and all authors commented on previous versions of the manuscript. The final revision and final version were written by P.T.S.F. All authors read and approved the final manuscript and to have approved the submitted version and to have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by Comitê de Ética em Pesquisa da Fundação de Ensino e Pesquisa em Ciências da Saúde (FEPECS) registration code: CAAE 86864618.4.0000.5553. All the procedures were performed in accordance with the ethical standards on human experimentation and with the Helsinki Declaration of 1975 and its later amendments. Informed consent was obtained from all participants and/or their legal guardians.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pains, M.B., de Melo, N.S., Leite, A.F. et al. Contribution of dental treatment to reducing mortality in the ICUs: a 6-year retrospective analysis. Sci Rep 15, 18188 (2025). https://doi.org/10.1038/s41598-024-84418-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-84418-9