Abstract
The neutrophil-to-lymphocyte ratio (NLR) may predict outcomes in end-stage liver disease, but its value after transjugular intrahepatic portosystemic shunt (TIPS) is unclear. This study explored the link between NLR and long-term outcomes in decompensated cirrhosis patients post-TIPS. We retrospectively analyzed 184 patients treated between January 2016 and December 2021, noting demographic data, lab results, and follow-up outcomes, including liver transplantation or death. Cox regression, adjusted for various factors, showed that NLR is an independent predictor of post-TIPS progression (HR 1.665; 95% CI 1.149–2.414; P = 0.007). Patients were divided into tertiles based on NLR. The medium tertile had a 3.51-fold increased risk of progression compared to the lowest (HR 3.510; 95% CI 1.104–11.153, P = 0.033), and the highest tertile had a 5.112-fold increase (HR 5.112; 95% CI 1.653–15.806, P = 0.005). This suggests that NLR is a valuable prognostic marker for long-term progression in these patients, highlighting the role of systemic inflammation.
Similar content being viewed by others
Introduction
Approximately 5%~7% of compensated cirrhotic patients progress to decompensated cirrhosis annually1. During the decompensated stage, as the disease advances, portal pressure escalates, precipitating complications such as esophageal and gastric variceal bleeding, refractory ascites, hepatic encephalopathy, and hepatorenal syndrome. The median survival post-decompensation is a mere 2 years1,2,3,4. Transjugular intrahepatic portosystemic shunt (TIPS) serves as a minimally invasive interventional procedure for managing portal hypertension complications. Indications encompass refractory ascites, variceal bleeding, hepatorenal syndrome, and hepatic hydrothorax5,6. Despite its ability to alleviate portal vein pressure, TIPS does not sustain long-term liver function stability and is often viewed as a temporary solution before liver transplantation. Additionally, certain patient cohorts exhibit high mortality rates post-TIPS7,8. Thus, meticulous monitoring and screening of patients with potentially poor prognoses post-TIPS are imperative, as they might necessitate more aggressive interventions or even liver transplantation.
Presently, postoperative survival assessment for TIPS recipients typically relies on the Child-Turcotte-Pugh (CTP) and Model for End-Stage Liver Disease (MELD) scores9,10. Furthermore, several studies have explored post-TIPS survival assessment through models like the Albumin-Bilirubin (ALBI) grade, Bilirubin-Platelet Ratio, and Freiburg Index of Post-TIPS Survival (FIPS)11,12,13. However, these models primarily draw from Western cohorts, with etiological disparities in cirrhosis compared to Chinese patients. The applicability of these models to the Chinese population necessitates further validation. Moreover, these models predominantly focus on short-term postoperative prognosis, lacking evaluation of long-term survival. Hence, identifying novel, straightforward, and reliable biomarkers for assessing long-term outcomes post-TIPS insertion is paramount.
One such biomarker is the Neutrophil-to-Lymphocyte Ratio (NLR), reflecting host systemic inflammation and mirroring the imbalanced pro-inflammatory immune response during cirrhosis stages14. White blood cell count serves as a pivotal marker of systemic inflammatory response, with liver structure hemodynamic disturbance associated with underlying inflammation, as evidenced by elevated white blood cell counts, increased C-reactive protein (CRP), and pro-inflammatory cytokine release2,15. Additionally, studies have indicated NLR’s prognostic value in cardiovascular diseases, acute myocardial infarction, hepatocellular carcinoma, other tumor diseases, non-alcoholic fatty liver disease, and liver transplantation16,17,18,19. NLR emerges as a crucial independent prognostic indicator distinct from MELD and CTP scores20. Nonetheless, research on utilizing NLR to evaluate adverse outcomes in cirrhotic patients post-TIPS remains limited. Our objective is to investigate whether NLR can serve as a clinician-utilizable biomarker for systemic inflammation, aiding in predicting the long-term outcomes of decompensated cirrhotic patients post-TIPS.
Results
Study population features
Finally, 184 patients (average age: 51.04 ± 10.72 years) were enrolled in the study, including 44 (23.91%) females and 140 (76.09%) males as shown in Table 1. Of the enrolled patients, 72 (39.13%) showed cirrhosis aetiology due to viral hepatitis, 51 (27.72%) cirrhosis due to alcohol, 30 (16.30%) cirrhosis due to viral and alcohol and 31 (16.85%) were due to other causes (these include autoimmune liver disease, hemorrhagic cirrhosis, cryptogenic cirrhosis, etc.). The study participants were followed for an median of 28 (17, 42) months. During the follow-up period, 147 patients who survived were placed in the surviving group, whereas the 37 patients who passed away or had liver transplantation were placed in the progression group. The outcomes of our comparison of the demographic features of the patients in the surviving and progression groups revealed substantial age and aetiology disparities between the two groups. We also compared the laboratory parameters between the surviving and progression groups and found significant differences in neutrophils, blood ammonia, and NLR.
The prognostic significance of NLR
To further understand which indicators were predictive of patient prognosis, we performed ROC curve analysis on the baseline laboratory parameters that showed differences between the surviving and progression groups. Through the analysis of the area under the curve (AUC), we found that NLR has predictive value for long-term outcomes post-TIPS (Fig. 1). Additionally, using 12, 24, and 36 months post-TIPS as study endpoints, we found that the AUC for NLR was consistently higher than that for the neutrophils, MELD score and CTP score. Notably, the AUC for predicting adverse outcomes at 12 and 24 months post-TIPS was above 0.7, comparable to the plasma ammonia and FIPS model.
Association analysis between NLR and post-TIPS progression
A significant linear association was observed between NLR and post-TIPS progression as shown in Fig. 2 using the RCS method (P for non-linear = 0.611, P for overall = 0.006). On the premise of linear association, the Cox proportional hazards model analysis was performed. As shown in Fig. 3, the significantly positive association between NLR and post-TIPS progression remained consistent, regardless of whether NLR was included as a continuous or a categorical variable. Specifically, each additional SD increase of NLR was associated with a 1.794 times (HR, 1.794; 95% CI, 1.122–2.867), 1.837 times (HR, 1.837; 95% CI, 1.221–2.765), 1.726 times (HR, 1.726; 95% CI, 1.170–2.545), 1.665 times (HR, 1.665; 95% CI, 1.149–2.414) increased risk of post-TIPS progression at 12 months,24 months, 36 months and thoroughout the overall follow-up period, respectively. Subsequently, the study population were stratified into lowest, medium, and highest tertiles based on the NLR level. Using the lowest tertile as a reference, the progression risk inceased 3.510 times (HR, 3.510; 95% CI, 1.104–11.153) in the medium tertile and 5.112 times (HR, 5.112; 95% CI, 1.653–15.806) in the highest tertile, respectively.
Association between NLR level and the risk of post-TIPS progression. The RCS curve displays the linear association between NLR level and the risk of post-TIPS progression. The black solid vertical line indicates the median level of NLR, and the black solid horizontal line indicates the corresponding post-TIPS progression risk. The red solid line represents the estimated hazards ratio of different NLR level using the median NLR level as reference, with the shaded red area indicates the 95% confidence interval. The histgram presents the distribution of NLR. Note: the level of NLR was Yeo-Johnson transformed to correct the skewness of distribution.
Forest plot pooled the association between NLR and the risk of post-TIPS progression. The forest plot visually represents the statiscs, hazard ratios and corresponding 95% confidence intervals for each comparison using Cox regression model with age, sex, etiology and serum ammonia adjusted. The lowest tertile is used as reference when calculating the hazard ratios of medium tertile and highest tertile. The red dashed line at HR = 1 indicates no change in risk. Values to the right of this line indicate higher risk, while values to the left would indicate lower risk. Note: the level of NLR was Yeo-Johnson transformed to correct the skewness of distribution.
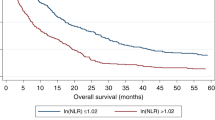
Figure 4 demonstrated the survival curves for aforementioned tertiles. The survival probability decreases progressively from the lowest tertile to the highest tertile. The log-rank test indicated a significant difference in survival among the tertiles (P-value < 0.001). Assuming we were interested in the progression status at 36 months, we could found the non-progression rate was extremely low for patients in the highest tertile, at 66.8%, while survival for those in the medium tertile and lowest tertile was 80.5 and 92.5%, respectively.
Survival probability stratified by NLR tertiles over time. The Kaplan-Meier survival curves display the survival probabilities of patients stratified into lowest (green), medium (orange), and highest (red) tertiles based on the level of NLR. The table below the graph shows the number of patients at risk (still being followed up) at corresponding time points for each tertile, with the percentage indicated in parentheses.
Discussion
Although previous studies have established the prognostic value of NLR in patients with cirrhosis or hepatocellular carcinoma, research on its use as a biomarker to predict post-TIPS mortality in cirrhotic patients is limited. In this retrospective analysis, we investigated the prognostic impact of NLR on overall progression in patients with decompensated cirrhosis undergoing TIPS at 12-month, 24-month, 36-month. Futhermore, the Cox regression models revealed that higher NLR was associated with increased long-term progression post-TIPS, and this association remained significant after adjusting for potential confounders such as age, sex, etiology of cirrhosis and the level of plasma ammonia.
Our research results are consistent with earlier studies, demonstrating the prognostic value of NLR in various contexts of liver cirrhosis. Previous studies have shown that in patients with stable liver cirrhosis, NLR predicts all-cause mortality regardless of CTP and MELD scores20. Additionally, multicenter studies have established a correlation between NLR and mortality within a year of non-elective hospitalization, indicating a sustained risk of death due to acute immunological dysregulation long after the initial hospitalization21. These findings emphasize the role of systemic inflammation, as reflected by NLR, in the progression and prognosis of liver disease. NLR, as a readily available marker, may reflect the balance between pro-inflammatory and anti-inflammatory responses in cirrhotic patients22. Elevated NLR levels indicate an enhanced inflammatory state, which is associated with poor outcomes across various chronic conditions14,23.
While scientific data supports the use of NLR as a prognostic marker, the underlying mechanism by which leukocyte imbalance leads to increased mortality remains unclear. Kalra et al. hypothesize that an increased NLR may promote the circulation of low-density granulocytes, which exhibit pro-inflammatory properties24. Literature indicates that systemic inflammatory response syndrome contributes to worsening prognosis in cirrhosis patients. Systemic inflammation, in the setting of cirrhotic immune dysregulation and reduced production of immunologic proteins, leads to elevated levels of pro-inflammatory cytokines25,26. In decompensated states, patients are prone to continuous bacterial translocation and increased NLR, where chronic inflammation may result in hemodynamic disturbances and organ damage, impacting overall mortality27. In post-TIPS patients, portal hypertension and subsequent blood shunting may exacerbate systemic inflammation. Chronic inflammation in these patients could contribute to further hepatic decompensation, increased susceptibility to infections, and other complications such as hepatic encephalopathy, which are common causes of mortality post-TIPS28.
Although the MELD score has been widely used for candidate selection and risk stratification in TIPS patients, its predictive capability remains controversial29. Particularly, the predictive performance of the MELD score is unsatisfactory in patients with low MELD scores24. Our study contributes to the understanding of integrating NLR into clinical practice. By identifying patients with higher NLR levels, clinicians can potentially stratify patients based on their risk and optimize both their TIPS eligibility and the priority for transplantation. The current study evaluated only the NLR measured before TIPS admission. NLR levels may fluctuate during hospitalization, and subsequent research could investigate whether NLR patterns have additional prognostic significance.
However, it is important to acknowledge the limitations of our study. Being a retrospective analysis, there is an inherent risk of selection bias and confounding factors that might not be fully accounted for, despite adjustments. Additionally, the study population was from a single center, which may limit the generalizability of our findings. Future prospective studies with larger, multicenter cohorts are warranted to validate our results and further explore the mechanisms underlying the relationship between NLR and post-TIPS outcomes.
In conclusion, our study suggests that NLR is a valuable prognostic marker for long-term progression in patients with decompensated cirrhosis undergoing TIPS. Elevated NLR levels are associated with a higher risk of adverse outcomes, highlighting the importance of systemic inflammation in this patient population. Integrating NLR into the pre-procedural evaluation could enhance risk stratification and guide clinical decision-making to improve patient outcomes.
Materials and methods
Patient population
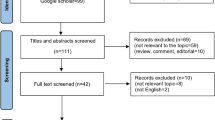
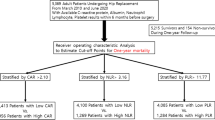
We conducted a retrospective analysis of patients with decompensated cirrhosis who underwent TIPS procedures for refractory ascites or significant gastroesophageal bleeding at Guizhou Provincial People’ s Hospital between January 2016 and December 2021. The study received approval from the Ethics Committee of Guizhou Provincial People’ s Hospital (2023-009). Individual consent was waived for this retrospective analysis. Demographic data and laboratory parameters of all cirrhotic patients were extracted from medical records. The study population comprised patients with radiological confirmation of decompensated cirrhosis who underwent the TIPS procedure. Exclusion criteria included patients diagnosed with non-cirrhotic portal hypertension, Budd-Chiari syndrome, pulmonary hypertension, right heart diastolic dysfunction (E/A < 0.75), and left ventricular ejection fraction less than 50%, as identified by echocardiography within 1 month prior to the procedure. Additionally, patients with hepatocellular carcinoma, those who had been infected within 1 month, and those lost to follow-up after TIPS placement were also excluded. Ultimately, 184 patients were included. An inclusion diagram is presented in Fig. 5.
Transjugular intrahepatic portosystemic shunt (TIPS) procedure
The indications for TIPS implantation were determined through meticulous preoperative evaluation and consultation by our hepatology and interventional specialist teams. Each patient underwent the TIPS procedure, which was performed by interventional radiologists. During this process, we utilized CT-guided right internal jugular vein puncture as the peripheral vascular access for TIPS. Venous pressure in the right hepatic vein was measured using a catheter, followed by needle insertion to establish a connection between the right hepatic vein and the intrahepatic portion of the portal vein. The stent was then guided through the pathway created by the needle and expanded using an expandable polytetrafluoroethylene-covered stent (10 mm; Viatorr TIPS endoscopy; Gore, Flagstaff, Arizona, USA) with the balloon expanded to 8 mm. The patency rate of TIPS in patients was monitored using Doppler ultrasound every 3–6 months.
Data collection
Baseline characteristics, including sex, age, BMI, as well as the etiology of cirrhosis for each patient were recorded. Laboratory indicators, including serum total bilirubin level, albumin level, alanine aminotransferase (ALT) level, sodium level, creatinine level, international normalized ratio (INR) level, platelet count, neutrophil count, lymphocyte count and plasma ammonia, were collected within 48 h before TIPS implantation. Prognostic scores, including MELD and CTP scores, were calculated using the most recent test results before TIPS implantation.
To confirm patient prognosis outcomes and the last clinical follow-up date, we relied on the final medical records of patients’ visits and telephone follow-up interviews. The primary outcome was adverse progression within 12, 24, and 36 months of TIPS implantation, including liver transplantation or death from complications such as gastrointestinal bleeding, liver failure, and hepatic encephalopathy (HE).
Statistical analysis
Data were processed with the R software (version 4.3.0, R Core Team, Vienna, Austria). Statistical differences were considered significant at p < 0.05 (two-sided). The overall population were divided into two groups based on their outcomes. Continuous variables were collected and presented as mean ± SD or median (lower quartile, upper quartile) in cases of non-normal distribution, and comparisons were made using Student’s t-test or Mann-Whitney U test as appropriate. Categorical data were expressed as frequency percentages and compared using the chi-square test. A receiver operating characteristic (ROC) curve was generated to compare the neutrophils, blood ammonia, NLR, MELD score, CTP score, and FIPS, using the respective area under the curve (AUC) values to assess predictive ability for 12-month, 24-month, and 36-month mortality. AUC values nearing 0.7 are generally considered indicative of acceptable predictability. Accounting for the skewness in the distribution of NLR, the level of NLR was Yeo-Johnson transformed in regression analysis. Initially, we used restricted cubic spline (RCS) to examine the linearity of association between NLR and post-TIPS analysis. Once the premise of linearity held, Cox regression analysis was employed to assess the association of NLR between post-TIPS adverse progression at 12 months, 24 months, 36 months and overall follow-up period. In Cox regression model, age, sex, the etiology of cirrhosis and the level of serum ammonia were adjusted. To verify the robustness of the result of continuous NLR, we further divided the patients into three tertiles according to their NLR level: lowest tertile, medium tertile, highest tertile. The hazards ratio of medium tertile and highest tertile were calculated using the lowest tertile as the reference with aforementioned covariates adjusted. Additionally, a Kaplan–Meier estimator plot was created to illustrate the association of NLR with survival probability. Log-rank test was used for the comparison among these tertiles.
Data availability
The [clinical] data used to support the findings of this study are available from the corresponding author at [wangrongpin@126.com] upon request.
References
D’Amico, G. et al. Clinical states of cirrhosis and competing risks. J. Hepatol. 68, 563–576. https://doi.org/10.1016/j.jhep.2017.10.020 (2018).
Dirchwolf, M. & Ruf, A. E. Role of systemic inflammation in cirrhosis: From pathogenesis to prognosis. World J. Hepatol. 7, 1974–1981. https://doi.org/10.4254/wjh.v7.i16.1974 (2015).
Gines, P. et al. Liver cirrhosis. Lancet 398, 1359–1376. https://doi.org/10.1016/S0140-6736(21)01374-X (2021).
Poordad, F. F. Presentation and complications associated with cirrhosis of the liver. Curr. Med. Res. Opin. 31, 925–937. https://doi.org/10.1185/03007995.2015.1021905 (2015).
Salerno, F. et al. Refractory ascites: Pathogenesis, definition and therapy of a severe complication in patients with cirrhosis. Liver Int. 30, 937–947. https://doi.org/10.1111/j.1478-3231.2010.02272.x (2010).
Garcia-Pagan, J. C. et al. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl. J. Med. 362, 2370–2379. https://doi.org/10.1056/NEJMoa0910102 (2010).
Fagiuoli, S. et al. Consensus conference on TIPS management: Techniques, indications, contraindications. Dig. Liver Dis. 49, 121–137 (2017). https://doi.org/10.1016/j.dld.2016.10.011
Garcia-Pagan, J. C., Saffo, S., Mandorfer, M. & Garcia-Tsao, G. Where does TIPS fit in the management of patients with cirrhosis? JHEP Rep. 2, 100122. https://doi.org/10.1016/j.jhepr.2020.100122 (2020).
Malinchoc, M. et al. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 31, 864–871. https://doi.org/10.1053/he.2000.5852 (2000).
Kamath, P. S. et al. A model to predict survival in patients with end-stage liver disease. Hepatology 33, 464–470. https://doi.org/10.1053/jhep.2001.22172 (2001).
Gaba, R. C. et al. Prognostic capability of different liver disease scoring systems for prediction of early mortality after transjugular intrahepatic portosystemic shunt creation. J. Vasc Interv Radiol. 24, 411–420. https://doi.org/10.1016/j.jvir.2012.10.026 (2013). 420 e411-414; quiz 421.
Bureau, C. et al. Serum bilirubin and platelet count: A simple predictive model for survival in patients with refractory ascites treated by TIPS. J. Hepatol. 54, 901–907. https://doi.org/10.1016/j.jhep.2010.08.025 (2011).
Bettinger, D. et al. Refining prediction of survival after TIPS with the novel Freiburg index of post-TIPS survival. J. Hepatol. 74, 1362–1372. https://doi.org/10.1016/j.jhep.2021.01.023 (2021).
Thabut, D. et al. Model for end-stage liver disease score and systemic inflammatory response are major prognostic factors in patients with cirrhosis and acute functional renal failure. Hepatology 46, 1872–1882. https://doi.org/10.1002/hep.21920 (2007).
Mehta, G., Mookerjee, R. P., Sharma, V. & Jalan, R. Systemic inflammation is associated with increased intrahepatic resistance and mortality in alcohol-related acute-on-chronic liver failure. Liver Int. 35, 724–734. https://doi.org/10.1111/liv.12559 (2015).
Bhat, T. et al. Neutrophil to lymphocyte ratio and cardiovascular diseases: A review. Expert Rev. Cardiovasc. Ther. 11, 55–59. https://doi.org/10.1586/erc.12.159 (2013).
Absenger, G. et al. A derived neutrophil to lymphocyte ratio predicts clinical outcome in stage II and III colon cancer patients. Br. J. Cancer. 109, 395–400. https://doi.org/10.1038/bjc.2013.346 (2013).
Halazun, K. J. et al. Elevated preoperative neutrophil to lymphocyte ratio predicts survival following hepatic resection for colorectal liver metastases. Eur. J. Surg. Oncol. 34, 55–60. https://doi.org/10.1016/j.ejso.2007.02.014 (2008).
Oh, B. S. et al. Prognostic value of C-reactive protein and neutrophil-to-lymphocyte ratio in patients with hepatocellular carcinoma. BMC Cancer. 13, 78. https://doi.org/10.1186/1471-2407-13-78 (2013).
Biyik, M. et al. Blood neutrophil-to-lymphocyte ratio independently predicts survival in patients with liver cirrhosis. Eur. J. Gastroenterol. Hepatol. 25, 435–441. https://doi.org/10.1097/MEG.0b013e32835c2af3 (2013).
Rice, J. et al. Neutrophil-to-lymphocyte ratio associates independently with mortality in hospitalized patients with cirrhosis. Clin. Gastroenterol. Hepatol. 16, 1786–1791 e1781, (2018). https://doi.org/10.1016/j.cgh.2018.04.045
Peng, Y. et al. The role of neutrophil to lymphocyte ratio for the assessment of liver fibrosis and cirrhosis: A systematic review. Expert Rev. Gastroenterol. Hepatol. 12, 503–513. https://doi.org/10.1080/17474124.2018.1463158 (2018).
Di Martino, V. et al. Granulocyte colony stimulating factor in decompensated cirrhosis, acute alcoholic hepatitis, and acute-on-chronic liver failure: A comprehensive meta-analysis of randomized controlled trials. Clin. Res. Hepatol. Gastroenterol. 47, 102207. https://doi.org/10.1016/j.clinre.2023.102207 (2023).
Kalra, A. et al. Neutrophil-to-lymphocyte ratio correlates with proinflammatory neutrophils and predicts death in low model for end-stage liver disease patients with cirrhosis. Liver Transpl. 23, 155–165. https://doi.org/10.1002/lt.24702 (2017).
Cazzaniga, M. et al. The systemic inflammatory response syndrome in cirrhotic patients: Relationship with their in-hospital outcome. J. Hepatol. 51, 475–482. https://doi.org/10.1016/j.jhep.2009.04.017 (2009).
Albillos, A., Lario, M. & Alvarez-Mon, M. Cirrhosis-associated immune dysfunction: Distinctive features and clinical relevance. J. Hepatol. 61, 1385–1396. https://doi.org/10.1016/j.jhep.2014.08.010 (2014).
Arroyo, V. et al. The systemic inflammation hypothesis: Towards a new paradigm of acute decompensation and multiorgan failure in cirrhosis. J. Hepatol. 74, 670–685. https://doi.org/10.1016/j.jhep.2020.11.048 (2021).
Boike, J. R. et al. North American Practice-Based Recommendations for Transjugular Intrahepatic Portosystemic Shunts in Portal Hypertension. Clin. Gastroenterol. Hepatol. 20, 1636–1662 e1636, (2022). https://doi.org/10.1016/j.cgh.2021.07.018
Zhao, Y., Wang, Y. & Xu, J. Predictive accuracy comparison of prognostic scoring systems for survival in patients undergoing TIPS placement: A systematic review and meta-analysis. Acad. Radiol. https://doi.org/10.1016/j.acra.2023.10.050 (2023).
Acknowledgements
Not applicable.
Funding
This study supported by the Guizhou senior innovative talent project (Grant numbers [QKHPTRC-GCC [2022]041 − 1]) and the Guizhou Provincial People’ s Hospital Talent Fund (Zi Xu) under the Grant Hospital Talent Project [2022]-4.
Author information
Authors and Affiliations
Contributions
Zhu KS, Wang RP finished Study concept and design, Zhang Q, Long L finished acquisition of data, Zhang Q, Xu Z finished analysis and interpretation of data, Zhang Q, Xu Z finished drafting of the manuscript, Luo XH finished critical revision of the manuscript for important intellectual content, Zhang Q, Xu Z finished administrative, technical, or material support, and Zhu KS, Wang RP finished study supervision. All authors have made a significant contribution to this study and have approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was carried out in accordance with recommendations in the ethical guidelines of the latest version of the Declaration of Helsinki and those provide by the Guizhou Provincial People’ s Hospital. The protocol was approved by the Ethics Committee of the Guizhou Provincial People’ s Hospital (No. 2023-009).
Informed consent
Individual consent was waived for this retrospective analysis.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, Q., Xu, Z., Long, L. et al. Predictive value of neutrophil-to-lymphocyte ratio for long-term adverse outcomes in cirrhosis patients post-transjugular intrahepatic portosystemic shunt. Sci Rep 15, 797 (2025). https://doi.org/10.1038/s41598-024-84630-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-84630-7