Abstract
The aim of this study was to assess the potential association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and type 2 diabetes mellitus (T2DM) in a middle-aged and elderly Chinese population using data from the China Health and Retirement Longitudinal Study (CHARLS) from 2011 to 2015. Methods We used data from CHARLS 2011 as baseline data and follow-up data from 2015. NHHR was used as a continuous and categorical variable, and multivariate logistic regression modeling was used to explore its relationship with T2DM. Three models were developed to adjust for the possible effects of 14 factors on the outcomes. Restricted cubic spline was used to check for possible nonlinear associations, and subgroup and interaction analyses were used to assess differences between groups. Results A total of 7847 subjects were enrolled in the study, of whom 948 (12.1%) were diagnosed with T2DM. The last NHHR quartile group (Q4) presented the highest risk of T2DM (OR, 1.115, 95% CI, 1.088–1.141) after accounting for all covariates. Restricted cubic spline regression modeling revealed a nonlinear relationship between NHHR and T2DM (p for nonlinear = 0.001). The results of the subgroup analyses were consistent across the categories, indicating a significant positive correlation. Interaction analyses revealed significant interactions between NHHR and age, gender and marital status. Conclusion In the middle-aged and elderly population in China, there is a strong correlation between elevated NHHR and increased risk of T2DM onset. The relationship between NHHR and T2DM can be further investigated in the future to provide reference for the development of more accurate prediction models.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus (T2DM) is a chronic metabolic disease characterized by persistent elevations in blood glucose that is associated with genetic, environmental, obesity, and other lifestyle factors1. The main features of T2DM include insufficient insulin secretion and insulin resistance. Prolonged illness and improper management can lead to a series of serious complications, such as cardiovascular disease, nephropathy, retinopathy and neuropathy, which seriously affect human health2,3,4. It is estimated that 537 million adults aged 20–79 years will have T2DM in 2021, and the incidence of T2DM is gradually increasing with the aging of the population, improvement of living standards, and changes in diet and lifestyle habits5. China has the largest number of diabetic patients in the world, and the annual cost of treating diabetes imposes a huge economic burden on society6. Therefore, by identifying high-risk groups and providing early screening and customized interventions, the incidence of T2DM can be reduced and population health improved.
Previous studies have shown that dyslipidemia is a risk factor for T2DM7. Lipid parameters, including total cholesterol (TC), triglycerides (TG), low-density lipoproteins (LDL-C), and high-density lipoproteins (HDL-C), have been used individually in previous studies to assess the risk and outcome of T2DM8,9, but the predictive value of these parameters is limited. In recent years, the non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) has gained increasing attention as an innovative and comprehensive metric for assessing the lipid composition of atherosclerosis and providing broad insights into anti-atherogenic and atherogenic lipid particles10. In addition to assessing the severity of atherosclerosis, the NHHR has relevance and predictive value for a wide range of diseases (cardiovascular, neurologic, hepatic and renal, etc.)11,12,13. Kim et al.14 demonstrated that the diagnostic efficacy of NHHR in assessing insulin resistance (IR) and identifying metabolic syndrome surpasses that of traditional lipid markers, demonstrating greater accuracy and clinical value. These studies demonstrate the potential strength of NHHR to predict metabolism-related diseases. Therefore, studying the association between NHHR and T2DM has significant scientific and clinical value. By understanding the association between NHHR and T2DM, the harm of T2DM to individuals and society can be reduced through early screening and intervention in specific populations.
It is worth mentioning that there have been previous studies exploring the correlation between NHHR and T2DM in rural areas of China and cross-sectional studies based on the NHANES database15,16. However, the data in this study were obtained from the China Health and Retirement Longitudinal Study (CHARLS) database.CHARLS covers 450 urban and rural communities in 28 provinces in China, which is a much broader and more representative sample. The aim of our study was to conduct a longitudinal prospective analysis of NHHR as a continuous and categorical variable to predict the risk of developing type 2 diabetes mellitus in the Chinese population. By utilizing the rich data resources of CHARLS, we expect to more accurately assess the relationship between NHHR and the risk of type 2 diabetes.
Results
Baseline characteristics
Characteristics of the study population are shown in Table 1. A total of 7847 subjects were enrolled to participate, with a mean age of 58.0 years, 3657 (46.6%) males and 4187 (53.4%) females. 84.1% of the subjects were married, 90.7% had an education level of primary school or below, 93.6% lived in rural areas, 39.0% were smokers, and the vast majority (66.7%) did not consume alcohol. 948 cases (12.1%) developed T2DM in 2015 (Table 1).
Dose–response relationship between NHHR and T2DM
Table 2 shows the association of NHHR and quartiles of NHHR with the risk of T2DM. The risk of T2DM increased progressively with quartiles of NHHR (p indicates trend <0.001). Compared with the first NHHR group (Q1), the last NHHR quartile (Q4) had the highest risk of T2DM after adjusting for age, sex, education level, residence and marital status, smoking status, drinking status, sleep duration, systolic blood pressure, diastolic blood pressure, BMI, heart disease, stroke, and other chronic conditions (OR, 1.115, 95% CI, 1.088–1.141). Analyzed as a continuous variable, NHHR was significantly associated with T2DM (OR = 1.027; 95% CI: 1.013–1.042; p < 0.001). Figure 1 shows the dose-response relationship between NHHR and risk of T2DM. Restricted cubic spline regression showed a nonlinear relationship between NHHR and T2DM risk (p for nonlinear = 0.001).
Restricted cubic spline of the association between NHHR and the risk of T2DM. The model was adjusted for age, gender, education level, location and marital status, smoking status, drinking status, sleep time, SBP, DBP, BMI, stroke, heart disease, and other chronic conditions. The plot shows a non-linear relationship between NHHR and the risk of T2DM. To determine the optimal number of nodes, we initially tested different configurations of 3 to 7 nodes. By comparing the AIC and BIC values of the models and combining them with residual analysis, 4 nodes were finally selected as the optimal configuration.
Stratified analysis
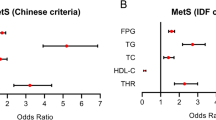
To see if there were differences in the effect of NHHR on the risk of developing T2DM between subgroups, we grouped participants by characteristics. The results showed that the effect of NHHR on the risk of T2FM was consistent across subgroups (Fig. 2). There was an interaction between NHHR and age, sex and marriage.
Discussion
Our results suggest that high NHHR is associated with T2DM risk. Subgroup analyses further validated the stability of this positive correlation result, which remained stable when the subgroups were stratified according to age, gender, marital status, education, place of residence, smoking, alcohol consumption sleep duration, and BMI. Based on dose-response relationship analysis, we found a nonlinear relationship between NHHR and T2DM risk.
Consistent with previous findings, our results suggest that dyslipidemia is strongly associated with T2DM risk7. Most of the previous studies have focused on conventional lipid parameters (TC, TG, HDL-C, LDL-C) for the treatment of dyslipidemia, while others have suggested that non-HDL-C (all plasma lipoproteins except HDL-C) is an important risk factor for cardiovascular disease17,18,19. The non-HDL-C to HDL-C ratio (NHHR) has been a hot topic in recent years compared to traditional conventional lipid parameters20. Numerous studies have shown that NHHR may be an important indicator of various diseases, including cardiovascular disease, neurologic disease, diabetes, and metabolic syndrome11,12,13. In atherosclerosis, NHHR is thought to play an important role in the balance between anti-atherogenic and atherogenic10. In the field of diabetes, it has been shown that NHHR has excellent predictive ability for diabetes and has better predictive accuracy compared to conventional lipid parameters15,16,21. Han et al.15. demonstrated the relevance of the non-HDL-C/HDL-C ratio to T2DM by following 11,487 nondiabetic participants ≥ 18 years of age in rural China. Talk et al.16 also demonstrated that an increase in NHHR may be associated with an increased likelihood of developing T2DM through a cross-sectional study using data from 10,420 U.S. adults from NHANES 2007–2018. Our findings are consistent with previous studies, further confirming the exact association between NHHR and T2DM and highlighting the status of NHHR as an important predictor. The present study covered 450 urban and rural communities in 28 provinces in China, which is a broader and more representative sample, and a longitudinal prospective analysis was conducted using the most recent data available.
The mechanism of the relationship between NHHR accumulation and T2DM risk is unclear, but this may be related to atherosclerosis. NHHR correlates with lipoprotein particle size, reflecting the balance between anti-atherosclerotic and pro-atherosclerotic particles15,21. Elevated NHHR suggests that a decrease in the size of LDL particles and an increase in the proportion of sdLDL promotes the development of atherosclerotic plaques. Second, NHHR levels reflect the risk of cholesterol deposition in peripheral tissues, resulting in increased free fatty acid concentrations and decreased insulin sensitivity22,23. Excessive lipid-induced oxidative stress disrupts insulin-related signaling pathways, decreases insulin activity, and increases the risk of T2DM development24. In addition, a rise in NHHR represents a decrease in HDL-C levels, which have very potent antidiabetic effects, such as enhancing insulin sensitivity, decreasing levels of oxidative stress and inflammation caused by non-HDL-C, and maintaining β-cell integrity25,26. Finally, long-term high NHHR is often accompanied by higher BMI and TC, and more habitual smoking and drinking, which is consistent with our results, and these are also common risk factors for the risk of developing T2DM27,28.
Our subgroup and interaction analyses showed differences in the relationship between NHHR and T2DM analysis by age, gender and marital status. With age, the body’s metabolic functions gradually diminish, including lipid metabolism, which leads to an imbalance in the metabolism of lipid components in the blood, which in turn affects the NHHR29. Older adults may be more prone to an elevated NHHR due to a reduced metabolic efficiency, increasing the risk of T2DM. In addition, aging is accompanied by a systemic low-grade inflammatory state and increased levels of oxidative stress, both of which are closely associated with elevated NHHR levels and the development of T2DM30,31. With respect to gender, although both men and women are more likely to develop T2DM with higher NHHR levels, women are more susceptible than men to the effects of NHHR, which influence the development of T2DM, similar to previous studies32. There are a number of possible explanations for this, firstly, estrogen benefits cardiovascular health, regulates insulin sensitivity as well as glucose metabolism, and reduces inflammation as well as levels of oxidative stress in tissues, however this protective effect diminishes with age, leading to an elevated NHHR and adverse outcomes16,33,34. Secondly, women are more likely to accumulate fat in the abdomen and hips, leading to increased systemic inflammation, which is also a risk factor for T2DM16,35. Finally, women have lower levels of basal fatty acid oxidation and are more likely to have metabolic disturbances compared to men36. It is worth mentioning that compared with married ones, single people (including unmarried, divorced, and widowed) are more likely to have elevated NHHR and increased risk of T2DM, which may be related to lifestyle, psychological factors, and behavioral habits.
Given the results of this study, the potential clinical significance is to emphasize the importance of incorporating NHHR into routine health assessments, especially for middle-aged and older populations who are at higher risk for T2DM. Early screening programs that include NHHR can help identify individuals who may benefit from lifestyle modifications or closer monitoring. In addition, healthcare providers should consider the significant interactions between NHHR and age, gender, and marital status when designing personalized prevention strategies. Additional research is needed to further substantiate these findings and develop more robust predictive models that combine NHHR with other relevant biomarkers and health indicators.
As a nationwide population-based prospective cohort study, this study has a wide coverage and a good sample representation. We used NHHR as a continuous variable to explore its dose-response relationship with stroke risk, and made the findings reliable and convincing by developing three models to adjust for the possible effects of 11 factors on the outcome. Subgroup analyses were conducted to explore differences in the correlation between NHHR and T2DM risk across multiple subgroups.
There are some limitations of this study. First, some potential confounders limited the interpretation of our findings, such as dietary, ethnic, and lifestyle differences. Second, we only included Chinese participants aged 45 years and older, and the applicability among younger age groups and different ethnic groups should be viewed with skepticism. Third, due to the data design of the CHARLS database, subjects in this study may have been affected by selection bias. Finally, this observational study could not determine a causal relationship between NHHR and T2DM risk, only an association between the two.
Methods
Data sources
The data for this study were obtained from CHARLS, a nationwide interdisciplinary survey, which collected comprehensive data on basic information, family structure, physical status, health insurance, work pension, income and expenditure, housing, and laboratory tests by using face-to-face interview methods and structured questionnaires with participants aged 45 years and older in 28 provinces and 450 communities. In addition, CHARLS subjects were fasted for more than 12 h, venous blood samples were collected from the participants, and whole blood specimens were stored at 4℃ and immediately sent for testing to detect the levels of TG, LDL-C, and HDL-C, among others, using enzyme colorimetric assay. Each assay result was merged with the data file by two China CDC staff to ensure accuracy37.
Study population
This study used data from CHARLS, and the CHARLS study protocol was approved by the Ethics Review Committee of Peking University, China, and written informed consent was obtained from all participants.
Our study used two waves of CHARLS data conducted in 2011 and 2015. Baseline participants were selected from the 2011 dataset (n = 17708). To determine the final study population, we applied the following exclusion criteria:1. excluding subjects who already had T2DM at baseline, 2. age < 45 years, 3. exclusion of subjects with abnormal BMI (Values more than 3 SDs), 4. excluded participants without complete NHHR data, 5. exclusion of subjects with missing T2DM information at the 2015 follow-up visit. The specific design and participant flow is shown in Fig. 3.
Variables
Non-HDL cholesterol to HDL cholesterol ratio (NHHR).
NHHR indicates the ratio of non-HDL-C to HDL-C, and the difference between serum TC level (mmol/L) minus HDL-C level (mmol/L) is non-HDL-C.
Diagnosis of type 2 diabetes mellitus
The outcome variable in this study was the occurrence of T2DM events during the follow-up period (2015).The diagnosis of T2DM was determined by one or more of the following criteria: (1) fasting blood glucose ≥ 126 mg/dl (7 mmol/L), (2) random blood glucose ≥ 200 mg/dl (11.1 mmol/L) (3) hemoglobin A1c ( HbA1c) ≥ 6.5%, (4) self-reported of “yes” (“Have you ever been diagnosed with diabetes or hyperglycemia?“).
Covariates
Covariate data were selected based on the results of previous studies6,38, incorporating the following factors as covariates: (1) Categorical variables: gender, education level, marital status, place of residence, smoking status, drinking status, self-reported heart disease, stroke, and other chronic diseases (cancer, chronic lung disease, memory-related disorders, renal disorders, liver disease, arthritis, digestive disorders, asthma, and psychiatric problems). (2) Continuous variables: age, sleep, systolic blood pressure (SBP), diastolic blood pressure (DBP), and BMI. education level was categorized as primary school or below, high school, and college or above. Never smokers were defined as “non-smokers” and smokers, including those who had quit, were defined as “smokers”. Alcohol consumption was categorized as “never”, “less than once a month” and “more than once a month”. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were the average of three measurements using an Omron HEM-7200 sphygmomanometer.
Statistical analysis
Normally distributed continuous variables are expressed as mean and standard deviation (SD), and abnormally distributed continuous variables are expressed as median (interquartile spacing (IQR)). Categorical variables are expressed as frequencies and percentages. After grouping by NHHR quartiles (Q1, Q2, Q3, and Q4), baseline characteristics and incidence of T2DM were compared using one-way ANOVA, Kruskal-Wallis H test, or chi-square test. Three logistic models were used to estimate the ratio of ratios (OR) for T2DM using NHHR as a continuous variable (per IQR increment) or a categorical variable (per quartile) with a confidence interval (CI) of 95%. The three different models included (1) Model 1: without any covariates; (2) Model 2: adjusted for sociodemographic factors, including age, gender, education, marital status, and place of residence. (3) Model 3: This model adjusted for all factors, including age, gender, education, marital status, place of residence, smoking status, alcohol consumption status, sleep, systolic blood pressure (SBP), diastolic blood pressure (DBP), BMI, self-reported heart disease, stroke, and other chronic diseases. These results are expressed as OR as well as 95% Cl. Restricted cubic spline was used to test for possible non-linear associations and to visualize the dose-response association between NHHR and T2DM. We performed subgroup analyses based on age (< 65, ≥ 65 years), sex, marital status, education level, place of residence, smoking, alcohol consumption, sleep duration (< 7, ≥ 7 h), and BMI (< 25, ≥ 25 kg/m2). In addition, interaction analyses were performed using the product term [NHHR × (interaction term)] from the main analysis to identify changes in the influence of sociodemographic factors and health-related behaviors in the relationship between NHHR and T2DM. For missing values, we recalculated the data using Multiple Interpolation by Chained Equations (MICE). MICE allows different types of variables to be predicted from each other through a series of regression models to generate plausible filler values. To ensure the quality of the fill, we incorporated a range of auxiliary variables (age, sex, education level, residence, marital status, smoking status, drinking status, sleep duration, SBP, DBP, BMI, heart disease, stroke, and other chronic conditions). To assess the adequacy of the fills, we performed 50 independent fills (i.e., m = 50) and also calculated the proportion of missing information for each variable, as shown in Table 1.
All statistical analyses were performed in R 4.1. Statistical significance was established using a two-tailed test with a threshold of P < 0.05.
Conclusion
Higher NHHR levels are strongly associated with the risk of T2DM in Chinese middle-aged and elderly populations. Maintaining an appropriate NHHR range may help reduce the risk of T2DM in middle-aged and older adults, but further studies are needed to verify the causality of this association.
Data availability
The data for this study was obtained from CHARLS, the official website is http://charls.pku.edu.cn/. Researchers who want to use these data can register accounts via the website.
References
Dedoussis, G. V. Z., Kaliora, A. C. & Panagiotakos, D. B. Genes, diet and type 2 diabetes mellitus: a review.[J]. Rev. Diabet. Studies: RDS. 4 (1), 13–24 (2007).
Yun, J. & Ko, S. Current trends in epidemiology of cardiovascular disease and cardiovascular risk management in type 2 diabetes.[J]. Metab. Clin. Exp. 123, 154838 (2021).
Mamakou, V. et al. Schizophrenia and type 2 diabetes mellitus.[J]. Psychiatrike = Psychiatriki. 29 (1), 64–73 (2018).
Stumvoll, M., Goldstein, B. J. & van Haeften, T. W. Type 2 diabetes: principles of pathogenesis and therapy.[J]. Lancet (London England). 365 (9467), 1333–1346 (2005).
Sun, H. et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045.[J]. Diabetes Res. Clin. Pract. 183, 109119 (2022).
Pan, L. et al. Dose-response relationship between Chinese visceral adiposity index and type 2 diabetes mellitus among middle-aged and elderly Chinese.[J]. Front. Endocrinol. 13, 959860 (2022).
Filippatos, T. et al. Pathophysiology Diabet. Dyslipidaemia [J] Curr. Vascular Pharmacol., 15(6):566–575. (2017).
Martagon, A. J. et al. HDL abnormalities in type 2 diabetes: clinical implications.[J]. Atherosclerosis 394, 117213 (2024).
Khil, J. et al. Changes in total cholesterol level and cardiovascular disease risk among type 2 diabetes patients.[J]. Sci. Rep. 13 (1), 8342 (2023).
Zhu, L. et al. Lipoprotein ratios are better than conventional lipid parameters in predicting coronary heart disease in Chinese Han people.[J]. Kardiologia Polska. 73 (10), 931–938 (2015).
Qi, X. et al. The association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and risk of depression among US adults: a cross-sectional NHANES study.[J]. J. Affect. Disord. 344, 451–457 (2024).
You, J. et al. Association between the Non-high-density Lipoprotein Cholesterol to High-Density Lipoprotein Cholesterol Ratio and the risk of coronary artery disease.[J]. BioMed research international, 2020,2020:7146028.
Zelber-Sagi, S. et al. Non-high-density lipoprotein cholesterol independently predicts new onset of non-alcoholic fatty liver disease.[J]. Liver International: Official J. Int. Association Study Liver. 34 (6), e128–e135 (2014).
Kim, S. W. et al. Non-HDL-cholesterol/HDL-cholesterol is a better predictor of metabolic syndrome and insulin resistance than apolipoprotein B/apolipoprotein A1.[Z]. : 168, 2678–2683. (2013).
Han, M. et al. Association of non-HDL-C/HDL-C ratio and its dynamic changes with incident type 2 diabetes mellitus: the rural Chinese cohort study.[J]. J. Diabetes Complicat. 34(12), 107712 (2020).
Tan, M. et al. The association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio with type 2 diabetes mellitus: recent findings from NHANES 2007–2018.[J]. Lipids Health Dis. 23 (1), 151 (2024).
Hsu, S. H. et al. Positive Association between Small Dense Low-Density Lipoprotein Cholesterol Concentration and Biomarkers of Inflammation, thrombosis, and Prediabetes in non-diabetic adults.[J]. J. Atheroscler. Thromb. 26 (7), 624–635 (2019).
Navarese, E. P. et al. Association between Baseline LDL-C Level and Total and Cardiovascular Mortality after LDL-C lowering: a systematic review and Meta-analysis.[J]. JAMA 319 (15), 1566–1579 (2018).
Schulze, M. B. et al. Joint role of non-HDL cholesterol and glycated haemoglobin in predicting future coronary heart disease events among women with type 2 diabetes.[J]. Diabetologia 47 (12), 2129–2136 (2004).
Wang, A. et al. Non-HDL-C/HDL-C ratio is associated with carotid plaque stability in general population: a cross-sectional study.[J]. Front. Neurol. 13, 875134 (2022).
Sheng, G. et al. Evaluation of the value of conventional and unconventional lipid parameters for predicting the risk of diabetes in a non-diabetic population.[J]. J. Translational Med. 20 (1), 266 (2022).
Zhen, R. et al. The relationship between Non-HDL-C /HDL-C ratio (NHHR) and Vitamin D in type 2 diabetes Mellitus.[J]. Diabetes, metabolic syndrome and obesity: targets and therapy, 16:2661–2673. (2023).
Manell, H. et al. Hyperglucagonemia in youth is associated with high plasma free fatty acids, visceral adiposity, and impaired glucose tolerance.[J]. Pediatr. Diabetes. 20 (7), 880–891 (2019).
Darenskaya, M. A., Kolesnikova, L. I. & Kolesnikov, S. I. Oxidative stress: pathogenetic role in diabetes Mellitus and its complications and therapeutic approaches to correction.[J]. Bull. Exp. Biol. Med. 171 (2), 179–189 (2021).
Denimal, D. Antioxidant and anti-inflammatory functions of high-density lipoprotein in type 1 and type 2 diabetes.[J]. Antioxidants (Basel, Switzerland), 2023,13(1).
Yang, T. et al. Correlation between the triglyceride-to-high-density lipoprotein cholesterol ratio and other unconventional lipid parameters with the risk of prediabetes and type 2 diabetes in patients with coronary heart disease: a RCSCD-TCM study in China.[J]. Cardiovasc. Diabetol. 21 (1), 93 (2022).
Morissette, A. & Mulvihill, E. E. Obesity management for the treatment of type 2 diabetes: emerging evidence and therapeutic approaches.[J]. Journal of pharmacy & pharmaceutical sciences: a publication of the Canadian Society for Pharmaceutical Sciences, Societe Canadienne des sciences pharmaceutiques, 27:13065. (2024).
Liu, G. et al. Smoking cessation and weight change in relation to cardiovascular disease incidence and mortality in people with type 2 diabetes: a population-based cohort study.[J]. The lancet. Diabetes Endocrinol. 8 (2), 125–133 (2020).
Zeng, Q. et al. Lipids and lipid metabolism in cellular senescence: emerging targets for age-related diseases.[J]. Ageing Res. Rev. 97, 102294 (2024).
Kong, L. et al. Mitophagy in Relation to Chronic inflammation/ROS in Aging.[J] (Molecular and cellular biochemistry, 2024).
Militello, R. et al. Physical Activity and Oxidative Stress in Aging.[J]. Antioxidants (Basel, Switzerland), 2024,13(5).
Yuge, H. et al. Triglycerides/HDL cholesterol ratio and type 2 diabetes incidence: Panasonic Cohort Study 10.[J]. Cardiovasc. Diabetol. 22 (1), 308 (2023).
Xiang, D. et al. Protective Effects of Estrogen on Cardiovascular Disease Mediated by Oxidative Stress.[J]2021:5523516 (Oxidative medicine and cellular longevity, 2021).
Varlamov, O., Bethea, C. L. & Roberts, C. T. J. Sex-specific differences in lipid and glucose metabolism.[J]. Front. Endocrinol. 5, 241 (2014).
Paniagua, J. A. Nutrition, insulin resistance and dysfunctional adipose tissue determine the different components of metabolic syndrome.[J]. World J. Diabetes. 7 (19), 483–514 (2016).
Blaak, E. Gender differences in fat metabolism.[J]. Current opinion in clinical nutrition and metabolic care, 4(6):499–502. (2001).
Zhao, Y. et al. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS).[J]. Int. J. Epidemiol. 43 (1), 61–68 (2014).
Qing, G. et al. The association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and suicidal ideation in adults: a population-based study in the United States.[J]. Lipids Health Dis. 23 (1), 17 (2024).
Funding
This research was funded by the National Natural Science Foundation of China (NSFC) (No. 82260248), the Doubel Thousand Talents Plan of Jiangxi (No. jxsq2023201024), natural science foundation of Jiangxi Province (No. 20212BAB206029).
Author information
Authors and Affiliations
Contributions
Jiacong Tan (first author): conceptualization, writing- original draft preparation, methodology, software, Writing- review & editing. Huaxin Zhu: data curation, Writing- review & editing.Yanyang Zeng and Jiawei Li : visualization, Writing- review & editing.Yeyu Zhao : supervision, Writing- review & editing.Xue Xiao : conceptualization, Writing- review & editing.Corresponding author: Meihua Li : Writing- review & editing.All authors contributed to the writing of the final manuscript, Writing- review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Ethical principles were strictly followed in this study. This study used data from the China Health and Aged Care Tracking Survey (CHARLS), which was provided by a legally authorized institution, and informed consent was obtained from the participants. No personally identifiable information was involved in the study. The study was reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Nanchang University to ensure that it complied with the ethical standards for medical research.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tan, J., Zhu, H., Zeng, Y. et al. Non high density lipoprotein to high density lipoprotein cholesterol ratio and type 2 diabetes in Middle aged and Elderly Chinese. Sci Rep 15, 8485 (2025). https://doi.org/10.1038/s41598-024-84686-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-84686-5