Abstract
Benign paroxysmal vertigo (BPV) is a common cause of dizziness, and some patients are comorbid with psychiatric disorders such as depression, requiring intervention with antidepressants. However, the causal association between BPV, depression and antidepressants has not been clearly established. We used two-sample bidirectional Mendelian randomization (MR) to analyze the causal association between BPV, depression, and antidepressants. From a Finnish database, 43,280 patients with depression and 329,192 controls, and 106,785 patients with antidepressants and 88,536 controls were selected. Independent single nucleotide polymorphisms (SNPs) for depression and antidepressants were used as instrumental variables (IVs) with genomic significance (p < 5 × 10–8). Similarly, genome-wide association study (GWAS) data for BPV were selected from a Finnish database consisting of 8280 cases and 359,094 controls. Afterwards, a two-sample MR study was performed using R’s Two Sample MR and MR-PRESSO software packages. The multiplicity and heterogeneity of the data, as well as the effect of individual SNPs on the results were investigated. The main statistical analyses were weighted median, weighted mode, MR-Egger and weighted inverse variance weighting (IVW) for random effects. Finally, we identified associations between BPV, antidepressants and depression. Four outliers (rs3773087, rs4619804, rs62099231, rs7192848) were found to be associated with depression. After removing the outliers, the statistics showed no heterogeneity (p > 0.05) and horizontal pleiotropy (p > 0.05). Antidepressants were also found to have a random effect IVW (β = 0.440; p = 9.692 × 10–6; OR = 1.553; 95% CI 1.278–1.887). The inverse MR random effects IVW results showed a causal association between BPV and antidepressants (β = 0.051; p = 0.045; OR = 1.052; 95% CI 1.001–1.1066). In conclusion, there was a significant causal association between antidepressants and BPV at the genetic level. Clinicians should pay attention to patients with BPV combined with depressive disorders and develop timely interventions.
Similar content being viewed by others
Introduction
Dizziness, as a common disabling symptom, its impact on an individual’s quality of life and socio-economic impact cannot be ignored. According to statistics, the prevalence of dizziness is about 20–30%1, and especially in patients with vertigo2, suffering from tremendous life stress. The most prevalent peripheral vestibular dysfunction injury among the vertigo types is benign paroxysmal vertigo (BPV), which is typified by sporadic episodes of vertigo, nausea, vomiting, and an unsteadiness sensation brought on by head movements3.
BPV is associated with abnormal movement of otolith particles, and otoliths and calcium carbonate particles exiting the elliptical capsule into one side of the semicircular canals are the main etiologic factor in BPV. BPV has a lifetime prevalence of 2.4% and can affect people at any stage in life4. The incidence and progression of BPV have been linked to a number of variables, including old age, head trauma, vitamin D inadequacy, osteoporosis, and psychosocial problems5. The complex interaction of these factors makes the prevention and treatment of BPV more complicated.
Vertigo caused by BPV can lead to anxiety and depression in patients and even affect their sleep, thus forming a vicious circle. Manual reduction is a non-invasive maneuver designed to reset displaced otoliths in the inner ear and is the most effective treatment for BPV6. After manual reduction treatment, some BPV patients still experience dizziness, which means they may have anxiety or depression and require medication. Residual symptoms such as dizziness and depression are more common in BPV patients treated with antidepressants7. There is still no consensus on the use of antidepressants for BPV with depression. The causal relationship between BPV and depressive disorders as well as between BPV and antidepressant treatment remains unclear.
However, the causal relationship between BPV and depressive disorders and whether depression after the onset of BPV is treated with depression medications remain unclear8. Mendelian randomization (MR) uses genetic mutations as instrumental variables (IVs)9. MR is helpful in reducing confusion and the likelihood of drawing false conclusions about reverse causality because the postnatal environment has no effect on these mutations10. MR studies usually use publicly available genome-wide association studies (GWAS) to obtain large samples and to be able to identify additional causal pathways11. As a result, MR has emerged as a useful technique for etiological research investigating causality.
In order to better understand the causal relationship among depression, antidepressants, and BPV and to offer a fresh viewpoint on the etiology of BPV, this study employed the MR approach to investigate the impact of depression and antidepressants on the etiology of BPV.
Materials and methods
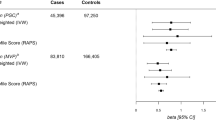
Depression and antidepressants: GWAS summary data
From the Finnish database, summary GWAS data for depression and antidepressants were retrieved (r9.finngen.fi)12. The depression study included 372,472 individuals from Europe, including 43,280 cases and 329,192 controls, with a total of 20,170,115 single nucleotide polymorphisms (SNPs). The antidepressants study comprised 195,321 European individuals, 106,785 of whom were in the medication group and 88,536 of whom were not on medication. Together, these individuals carried a total of 20,160,506 SNPs. The International Classification of Diseases, Tenth Revision (ICD-10) codes F32 and F33 were used to define depression.
Benign paroxysmal vertigo: GWAS summary data
The Finnish database’s greatest BPV GWAS summary data were chosen (r9.finngen.fi)12. A total of 367,374 individuals from Europe, including 8280 cases and 359,094 controls, were included in this GWAS database, with a total of 20,170,074 SNPs. The International Classification of Diseases, Tenth Revision, H81.8 code was used to define all cases (ICD-10).
Selection of genetic instrumental variants
Depression and antidepressants were the subjects of instrumental variables to research. The three MR analysis assumptions were satisfied by the instrumental variables used in this study: they had a significant correlation with exposure factors and had no relationship with confounding variables. Through exposure factors, instrumental variables have an impact on results. Using a genome-wide significance threshold of p < 5 × 10–8, we first identified SNPs linked to depression and antidepressants. Strong LD-induced linkage disequilibrium between SNPs was eliminated by clumping distance = 10,000 kb and r2 < 0.001. We then excluded SNPs associated with BPV (p < 1 × 10−5). Next, we determined that female sex, hypertension, hyperlipidemia, diabetes mellitus, osteoporosis, and vitamin D deficiency were confounding factors linked to BPV5,13,14,15. LDlink database was used to exclude confounding factors16. The deletion of palindromic SNPs with intermediate allele frequencies ensured the accuracy of the findings. Simultaneously, SNPs with F-statistics > 10 were chosen as instrumental variables in order to guarantee a higher correlation between instrumental variables and exposure17. F = β2/SE2 was the formula used to compute the F-statistic18.R2 using the formula R2 = (2 × EAF × (1 − EAF) × β2) /[ (2 × EAF × (1 − EAF) × β2) + (2 × EAF × (1 − EAF) × N × SE2)]19. Ultimately, we were able to identify 15 SNPs linked to antidepressants and 9 SNPs linked to depression (Supplementary Tables 1 and 3). Before identifying the SNPs linked to depression, we eliminated one palindrome SNP (rs11756123) and five confounding SNPs (rs3773087, rs4619804, rs62099231, rs7192848, rs9324959). No SNP was linked to BPV. IVs were derived from these nine SNPs (F-statistic > 10). Before we discovered SNPs linked to antidepressants, we eliminated three palindromic SNPs (rs117661209, rs2011374, and rs805826). There were no SNPs linked to BPV after seven confounding SNPs (rs115493740, rs2011374, rs328301, rs59956089, rs805826, rs9270366, rs9845443) were eliminated; these 15 SNPs were used as IV (F statistic > 10).
Reverse Mendelian randomization
To assess the likelihood of reverse causality, we performed a reverse MR analysis. In order to investigate the causal relationship between BPV and depression and antidepressants, BPV was employed as an instrumental variable. When selecting IVs with a p < 5e-8, we loosened the selection criteria for SNPs to a p < 1e-5 because there were only a limited number of SNPs available for reverse MR20. In order to confirm that the included SNPs still met the IVs requirements, we also calculated the F-statistics for each SNP in the reverse MR analysis, as was previously mentioned. The specific analysis methods employed were identical to those for the two-sample MR.
Statistical and MR analysis
Association of depression genetic IVs with BPV GWAS
We took nine distinct genetic IVs for depression out of the combined GWAS data set. Independent genetic IV association with BPV GWAS was shown. (Supplementary Table 1).
Association of BPV genetic IVs with depression GWAS
In all, 24 distinct genetic IVs were extracted from the pooled BPV GWAS data sets. An independent genetic IV association with depression (GWAS) was shown. (Supplementary Table 2).
Association of antidepressions genetic IVs with BPV GWAS
From the combined GWAS dataset for antidepressants, we isolated 15 distinct genetic IVs for each. An independent genetic IV association with BPV GWAS was shown. (Supplementary Table 3).
Association of BPV genetic IVs with antidepressions GWAS
The BPV GWAS pooled data set contained 27 distinct genetic IVs that we separately extracted. Showed an independent genetic IV association with the antidepressants GWAS. (Supplementary Table 4).
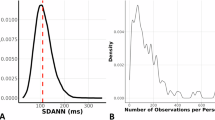
Pleiotropy and heterogeneity test
Using the Two Sample MR and MR-PRESSO packages in R, version 4.3.1, we conducted two-sample MR analyses for depression, antidepressants, and BPV21. Horizontal pleiotropy was found using the MR-PRESSO method and the MR-Egger’s intercept test22, p > 0.05 showed that the GWAS of depression and antidepressants gene instrumental variables for BPV did not exhibit horizontal pleiotropy. To find heterogeneity in the MR analysis, Cochran Q statistics (MR-IVW) and Rucker Q statistics (MR-Egger) were employed, and p > 0.05 indicated no heterogeneity23. Outliers, which typically affect the heterogeneity of the data, were found in our MR analysis using the MR-PRESSO analysis distortion test. After eliminating outliers, we must reanalyze the data24.
MR analysis
The causal relationship between depression, antidepressants, and BPV was examined using the MR-Egger, weighted median, IVW, simple model, and weighted model methods. The IVW results served as our primary foundation25. Auxiliary judgment was based on the MR-Egger, weighted median, simple pattern, and weighted pattern methods26. P < 0.05 was considered a statistically significant difference.
Single SNP effect analysis
We expressed each putative causal effect of depression, antidepressants, and BPV separately using “mr” and “mr_scatter_plot” in R27. To calculate the single SNP effect size of depression and antidepressants on BPV, “mr_forest_plot” was utilized28. To find out if a single SNP had an impact on the causal relationship between depression, antidepressants, and BPV, “mr_leaveoneout_plot” sensitivity analysis was employed29.
Results
Pleiotropy and heterogeneity of depression and antidepressants genetic IVs
In our study, we investigated the genetic interplay between depression, antidepression, and BPV using MR analysis. Initially, we identified four outliers (rs3773087, rs4619804, rs62099231, rs7192848) in the MR analysis between depression and BPV. However, no outliers were found in the analysis between antidepressants and BPV. When outliers were eliminated from the MR analysis of depression, antidepressants, and BPV, there was no longer any horizontal pleiotropy (p > 0.05) or heterogeneity (p > 0.05) (Tables 5–8 of Supplementary Material).
There was no correlation between BPV and depression
We found no correlation between BPV and depression. Further MR analysis, conducted after excluding the outliers, did not reveal any gene-level causal relationship between depression and BPV. The results of the depression and BPV analyses were as follows: IVW (β = − 0.025; p = 0.846; OR = 0.976; 95% CI 0.763–1.249), MR-Egger (β = − 0.461; p = 0.587; OR = 0.630; 95% CI 0.130–3.050), simple model (β = − 0.224; p = 0.443; OR = 0.799; 95% CI 0.475–1.346), weighted model (β = − 0.215; p = 0.413; OR = 0.806; 95%CI 0.488–1.332), weighted median (β = − 0.146; p = 0.356; OR = 0.864; 95% CI 0.632–1.180). These findings suggest that there is no evidence of a causal relationship between depression and genetic alterations in BPV.
BPV was not associated with depression
By MR analysis, there was no genetic causal effect of BPV on depression. The following were the findings from the analyses of depression and BPV: IVW (β = 0.030; p = 0.230; OR = 1.030; 95% CI 0.981–1.082), MR-Egger (β = 0.004; p = 0.942; OR = 1.004; 95% CI 0.906–1.112), simple model (β = 0.086; p = 0.256; OR = 1.090; 95% CI 0.944–1.257), weighted model (β = 0.072; p = 0.295; OR = 1.075; 95% CI 0.943–1.226), weighted median (β = 0.044; p = 1.182; OR = 1.045; 95% CI 0.980–1.113). According to our analysis, there is no connection between depression and genetic variations in BPV.
Antidepressants was associated with BPV
On the other hand, our MR analysis demonstrated a genetic causal effect of antidepressants on BPV. Antidepressants and BPV analysis showed that IVW (β = 0.440; p = 9.692 × 10–6; OR = 1.553; 95% CI 1.278–1.887), MR-Egger (β = 1.233; p = 3.132 × 10–1; OR = 3.432; 95% CI 0.345–34.088), simple model (β = 0.216; p = 3.726 × 10–1; OR = 1.241; 95% CI 0.781–1.972), weighted model (β = 0.203; p = 4.345 × 10–1; OR = 1.225; 95% CI 0.754–1.990), weighted median (β = 0.271; p = 4.930 × 10–2; OR = 1.311; 95% CI 1.004–1.771). Our analysis concluded that genetic changes are causal between antidepressants and BPV.
BPV was associated with antidepressants
Furthermore, our MR analysis revealed a genetic causal effect of BPV on antidepressants. The results of BPV and antidepressants analysis were as follows: IVW (β = 0.051; p = 0.045; OR = 1.052; 95% CI 1.001–1.106), MR-Egger (β = − 0.007; p = 0.903; OR = 0.993; 95% CI 0.894–1.104), simple model (β = 0.042; p = 0.448; OR = 1.042; 95% CI 0.937–1.160), weighted model (β = 0.046; p = 0.457; OR = 1.047; 95% CI 0.932–1.176), weighted median (β = 0.042; p = 0.178; OR = 1.042; 95% CI 0.984–1.104). Our analysis concluded that there is a causal relationship between genetic changes in BPV and the use of antidepressants.
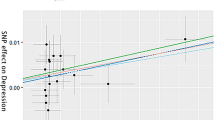
No significant bias in single depression and antidepressants SNP effect
Lastly, our MR analysis did not detect any significant bias in the SNP effects for depression and antidepressants. Analyses using weighted median, IVW, simple mode, weighted mode, and MR-Egger methods demonstrated that the impact of antidepressants on depression did not influence BPV for any SNP variation (Fig. 1). The analysis of the single SNP effect size further demonstrated this point (Fig. 2). Simultaneously, our MR leave-one-out sensitivity analysis demonstrated that altering any depression or antidepressant SNP by deleting a particular SNP did not alter the outcomes (Fig. 3).
Individual estimates about the putative causal effect of depression, antidepressants with BPV. (a) Depression and BPV. (b) BPV and depression. (c) Antidepressants and BPV. (d) BPV and antidepressants. IVW inverse variance weighted, MR Mendelian randomization, SNP single‐nucleotide polymorphism, BPV benign paroxysmal vertigo.
MR leave‐one‐out sensitivity analysis for the effect of depression and antidepressants SNPs with BPV. (a) Depression and BPV. (b) BPV and depression. (c) Antidepressants and BPV. (d) BPV and antidepressants. MR Mendelian randomization, SNP single‐nucleotide polymorphism, BPV benign paroxysmal vertigo.
Discussion
To our knowledge, this is the first two-sample MR analysis of the association between BPV and antidepressant risk using a large genetic dataset. The MR results support a causal relationship between BPV and antidepressants. It provides ideas for the clinical management of patients with BPV combined with depression.
We found no significant causal association between BPV and depression. However, there are different views on the relationship between depression and BPV. Many studies have found that depression levels are generally higher in BPV patients than in the general population30. Depressive disorders have been reported to produce somatic symptoms, including BPV31. In a population-based cohort study based on Taiwan, the risk of subsequent development of BPV was 1.55 times higher in patients with depressive disorder than in the general population32. A national cohort observational study from Korea showed that mood disorders increased the risk of BPV. In the subgroup analysis, the incidence of BPV in the emotional disorder group was significantly higher than that in the general population in all age groups and both genders33. This may be associated with proinflammatory cytokines playing an important role in mood disorders, altering serotonin levels and glutamate receptor activity34,35,36,37, and inducing oxidative stress in endothelial cells, mediating the recurrence of vasospasm, which can be displaced from the macular epithelium via otoliths, leading to BPV38. These studies suggest an epidemiological association between depression and BPV.
Studies have found higher rates of comorbid psychiatric disorders in BPV patients39. The risk of depressive disorder is significantly increased in BPV patients. However, a meta-analysis of BPV and depressive disorder found that the association between BPV and depressive disorder was not statistically significant40. Our results suggest that there is no significant causal relationship between BPV and depression at the genetic level. The differences in the results of studies on the relationship between BPV and depression may be related to a variety of factors, including study design, patient population, and interventions. In the future, larger and rigorous clinical studies may be needed to explore the relationship between BPV and depression.
Dizziness is a common side effect of many antidepressant treatments and may contribute to residual instability after BPV treatment41,42. The persistence of residual symptoms after manual reduction of BPV may be related to age, times of manual reduction, anxiety or depression, and other factors. Residual symptoms were more common in patients treated with antidepressants7. The unpredictability and uncontrollability of residual symptoms and vertigo attacks after BPV treatment may aggravate psychological distress and reduce the quality of life of patients. Some patients need antidepressant treatment to relieve the symptoms of depressive disorder after BPV7. However, there is no unified consensus on the use of antidepressants for BPV-comorbid depressive disorders. Our study found a significant causal association between antidepressants and BPV. Due to the high prevalence of comorbid psychiatric disorders in patients with BPV, this suggests that they may require antidepressants to help manage the mental health issues associated with vertigo. As a result, there is a potential increased demand for antidepressants. This may lead to a vicious circle between depressive disorder and vestibular dysfunction, which seriously affects the quality of life of patients. Therefore, in clinical work, we should pay more attention to the mental health of BPV patients, determine whether BPV patients are complicated with depression, and provide psychological counseling rather than direct use of antidepressant drugs.
We examined the causal relationship between depression, antidepressants, and BPV onset. At the same time, we also examined the reverse causality between depression, antidepressants, and BPV. This study is not without limitations, though. First, the results of our study are only applicable to individuals with European ancestry, and this limits the generalizability of the findings. Thus, further research utilizing larger ethnic data sets might be required to evaluate the generalizability of our findings to other ethnic groups. Second, there is no guarantee that the SNPs will be specific in identifying particular symptoms and the severity of BPV. Furthermore, a prospective randomized controlled trial was not carried out in our study to confirm the effectiveness of antidepressant-focused interventions for the treatment of BPV. As consequently, the possible benefit of reducing antidepressant use in treating BPV-comorbid depressive disorders could not be determined by our research. Our findings are drawn from a genetic standpoint and are meant to provide clinicians with insight into potential treatment options.
Conclusions
Using Mendelian randomization techniques, we have demonstrated a significant genetic causal association between antidepressants and BPV. This has prompted us to strengthen our focus on mental health issues in patients with BPV in our clinical practice, to assess psychiatric disorders at an early stage, and to work with mental health professionals to provide a more comprehensive treatment program, if necessary. In addition, the biological basis of this association should be studied in greater depth in the future to elucidate the underlying mechanisms.
Data availability
You can find all the datasets created and/or examined in this study in the FinnGen repository (https://r9.finngen.fi). The website (https://mrcieu.github.io/TwoSampleMR/articles/index.html) has the R code that has been analyzed.
References
Pothier, D. D. et al. Association between catastrophizing and dizziness-related disability assessed with the Dizziness catastrophizing scale. JAMA Otolaryngol. Head Neck Surg. 144, 906–912. https://doi.org/10.1001/jamaoto.2018.1863 (2018).
Strupp, M. & Brandt, T. Diagnosis and treatment of vertigo and dizziness. Dtsch. Arztebl. Int. 105, 173–180. https://doi.org/10.3238/arztebl.2008.0173 (2008).
Yu, S., Liu, F., Cheng, Z. & Wang, Q. Association between osteoporosis and benign paroxysmal positional vertigo: a systematic review. BMC Neurol. 14, 110. https://doi.org/10.1186/1471-2377-14-110 (2014).
Bhattacharyya, N. et al. Clinical practice guideline: benign paroxysmal positional vertigo. Otolaryngol. Head Neck Surg. 139, S47-81. https://doi.org/10.1016/j.otohns.2008.08.022 (2008).
Chen, J., Zhang, S., Cui, K. & Liu, C. Risk factors for benign paroxysmal positional vertigo recurrence: a systematic review and meta-analysis. J. Neurol. 268, 4117–4127. https://doi.org/10.1007/s00415-020-10175-0 (2021).
Brandt, T. Benign paroxysmal positioning vertigo. Adv. Otorhinolaryngol. 55, 169–194. https://doi.org/10.1159/000059062 (1999).
Vaduva, C., Estéban-Sánchez, J., Sanz-Fernández, R. & Martín-Sanz, E. Prevalence and management of post-BPPV residual symptoms. Eur. Arch. Otorhinolaryngol. 275, 1429–1437. https://doi.org/10.1007/s00405-018-4980-x (2018).
Correia, F., Medeiros, A. B., Castelhano, L., Cavilhas, P. & Escada, P. Personality and psychopathology in Ménière’s disease. Acta Otorrinolaringol. Esp. (Engl. Ed.) 72, 344–351. https://doi.org/10.1016/j.otoeng.2020.06.010 (2021).
Saccaro, L. F., Gasparini, S. & Rutigliano, G. Applications of Mendelian randomization in psychiatry: a comprehensive systematic review. Psychiatr. Genet. 32, 199–213. https://doi.org/10.1097/YPG.0000000000000327 (2022).
Didelez, V. & Sheehan, N. Mendelian randomization as an instrumental variable approach to causal inference. Stat. Methods Med. Res. 16, 309–330. https://doi.org/10.1177/0962280206077743 (2007).
Shivakumar, S., Wilken, M. B., Tsao, V., Bitarello, B. D. & Thom, C. S. Genetically influenced tobacco and alcohol use behaviors impact erythroid trait variation. medRxiv https://doi.org/10.1101/2023.05.01.23289329 (2023).
Kurki, M. I. et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature 613, 508–518. https://doi.org/10.1038/s41586-022-05473-8 (2023).
Furman, J. M. & Cass, S. P. Benign paroxysmal positional vertigo. N. Engl. J. Med. 341, 1590–1596. https://doi.org/10.1056/NEJM199911183412107 (1999).
Kim, J. S. & Zee, D. S. Clinical practice. Benign paroxysmal positional vertigo. N. Engl. J. Med. 370, 1138–1147. https://doi.org/10.1056/NEJMcp1309481 (2014).
Guo, Z., Huang, B., Gan, L., Liang, S. & Liu, Y. No genetic causality between obesity and benign paroxysmal vertigo: A two-sample Mendelian randomization study. Open Med. https://doi.org/10.1515/med-2024-0940 (2024).
Machiela, M. J. & Chanock, S. J. LDlink: a web-based application for exploring population-specific haplotype structure and linking correlated alleles of possible functional variants. Bioinformatics 31, 3555–3557. https://doi.org/10.1093/bioinformatics/btv402 (2015).
Burgess, S., Thompson, S. G. & Collaboration, C. C. G. Avoiding bias from weak instruments in Mendelian randomization studies. Int. J. Epidemiol. 40, 755–764. https://doi.org/10.1093/ije/dyr036 (2011).
Zhang, L. et al. Unlocking the medicinal mysteries: preventing lacunar stroke with drug repurposing. Biomedicines https://doi.org/10.3390/biomedicines12010017 (2023).
Sun, M. et al. Association between air pollution and primary liver cancer in European and east Asian populations: a Mendelian randomization study. Front. Public Health 11, 1212301. https://doi.org/10.3389/fpubh.2023.1212301 (2023).
Liang, X. & Fan, Y. Bidirectional two-sample Mendelian randomization analysis reveals a causal effect of interleukin-18 levels on postherpetic neuralgia risk. Front. Immunol. 14, 1183378. https://doi.org/10.3389/fimmu.2023.1183378 (2023).
Zhao, D. et al. Primary biliary cirrhosis and osteoporosis: a bidirectional two-sample Mendelian randomization study. Front. Immunol. 14, 1269069. https://doi.org/10.3389/fimmu.2023.1269069 (2023).
Li, H. et al. Diet-derived antioxidants and osteoporosis: A Mendelian randomization study. PLoS One 18, e0293145. https://doi.org/10.1371/journal.pone.0293145 (2023).
Yang, M. et al. Large-scale genetic correlation analysis between spondyloarthritis and human blood metabolites. J. Clin. Med. https://doi.org/10.3390/jcm12031201 (2023).
Reshi, Q. M., Ahmed, I., Al-Anazi, K. M. & Farah, M. A. Indexing hematological and serum biochemical reference intervals of Himalayan snow trout, Schizothorax esocinus to instrument in health assessment. Front. Physiol. 14, 989442. https://doi.org/10.3389/fphys.2023.989442 (2023).
Qiu, B. et al. Gut microbiota and common gastrointestinal diseases: a bidirectional two-sample Mendelian randomized study. Front. Microbiol. 14, 1273269. https://doi.org/10.3389/fmicb.2023.1273269 (2023).
Wu, L. et al. Causal relationship between systemic lupus erythematosus and primary liver cirrhosis based on two-sample bidirectional Mendelian randomization and transcriptome overlap analysis. Arthritis Res. Ther. 26, 10. https://doi.org/10.1186/s13075-023-03235-z (2024).
Lyu, L. et al. Causal relationships of general and abdominal adiposity on osteoarthritis: A two-sample Mendelian Randomization Study. J. Clin. Med. https://doi.org/10.3390/jcm12010320 (2022).
Zhu, G. et al. Mendelian randomization study on the causal effects of COVID-19 on childhood intelligence. J. Med. Virol. 94, 3233–3239. https://doi.org/10.1002/jmv.27736 (2022).
Yang, M. et al. No evidence of a genetic causal relationship between ankylosing spondylitis and gut microbiota: A two-sample Mendelian Randomization Study. Nutrients https://doi.org/10.3390/nu15041057 (2023).
van der Zaag-Loonen, H. J., van Leeuwen, R. B., Bruintjes, T. D. & van Munster, B. C. Prevalence of unrecognized benign paroxysmal positional vertigo in older patients. Eur. Arch. Otorhinolaryngol. 272, 1521–1524. https://doi.org/10.1007/s00405-014-3409-4 (2015).
Ferrari, S. et al. Vertigo “in the pink”: The impact of female gender on psychiatric-psychosomatic comorbidity in benign paroxysmal positional vertigo patients. Psychosomatics 55, 280–288. https://doi.org/10.1016/j.psym.2013.02.005 (2014).
Hsu, C. L. et al. Risk of benign paroxysmal positional vertigo in patients with depressive disorders: a nationwide population-based cohort study. BMJ Open 9, e026936. https://doi.org/10.1136/bmjopen-2018-026936 (2019).
Kim, S. K. et al. Mood disorders are associated with increased risk of BPPV: A national sample cohort. Laryngoscope 131, 380–385. https://doi.org/10.1002/lary.28638 (2021).
Graeff, F. G., Guimarães, F. S., De Andrade, T. G. & Deakin, J. F. Role of 5-HT in stress, anxiety, and depression. Pharmacol. Biochem Behav. 54, 129–141. https://doi.org/10.1016/0091-3057(95)02135-3 (1996).
Sanacora, G., Zarate, C. A., Krystal, J. H. & Manji, H. K. Targeting the glutamatergic system to develop novel, improved therapeutics for mood disorders. Nat. Rev. Drug Discov. 7, 426–437. https://doi.org/10.1038/nrd2462 (2008).
Dantzer, R. Cytokine, sickness behavior, and depression. Neurol. Clin. 24, 441–460. https://doi.org/10.1016/j.ncl.2006.03.003 (2006).
Lichtblau, N., Schmidt, F. M., Schumann, R., Kirkby, K. C. & Himmerich, H. Cytokines as biomarkers in depressive disorder: current standing and prospects. Int. Rev. Psychiatry 25, 592–603. https://doi.org/10.3109/09540261.2013.813442 (2013).
Ishiyama, A., Jacobson, K. M. & Baloh, R. W. Migraine and benign positional vertigo. Ann. Otol. Rhinol. Laryngol. 109, 377–380. https://doi.org/10.1177/000348940010900407 (2000).
Chen, Z. J. et al. Increased risk of benign paroxysmal positional vertigo in patients with anxiety disorders: a nationwide population-based retrospective cohort study. BMC Psychiatry 16, 238. https://doi.org/10.1186/s12888-016-0950-2 (2016).
Yeo, B. S. Y. et al. Association of benign paroxysmal positional vertigo with depression and anxiety-a systematic review and meta-analysis. Laryngoscope 134, 526–534. https://doi.org/10.1002/lary.30957 (2024).
Martellucci, S. et al. Features of residual dizziness after canalith repositioning procedures for benign paroxysmal positional vertigo. Otolaryngol. Head Neck Surg. 154, 693–701. https://doi.org/10.1177/0194599815627624 (2016).
Mendel, B., Bergenius, J. & Langius, A. Dizziness symptom severity and impact on daily living as perceived by patients suffering from peripheral vestibular disorder. Clin. Otolaryngol. Allied Sci. 24, 286–293. https://doi.org/10.1046/j.1365-2273.1999.00261.x (1999).
Acknowledgements
The authors would like to thank the participants and investigators of the FinnGen study.
Author information
Authors and Affiliations
Contributions
Liya Pan, Yayun Liao and Kejian Zhou designed the study; Yayun Liao and Kejian Zhou wrote the manuscript; Yayun Liao, Zhiyan Guo, Lu Qin, Shan Deng, Hong Yang and Baohui Weng performed the statistical analysis. Yayun Liao and Kejian Zhou are co-first authors. All authors agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liao, Y., Zhou, K., Guo, Z. et al. Mendelian randomization analysis reveals causal relationship between depression, antidepressants and benign paroxysmal vertigo. Sci Rep 15, 837 (2025). https://doi.org/10.1038/s41598-024-85047-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-85047-y