Abstract
Prolonged therapy using nucleos(t)ide analogs (NUC) is inevitable in patients with chronic hepatitis B (CHB) infection, but its long-term impact on Parkinson’s disease (PD) risk remains unclear. This study evaluated the association between NUC therapy and PD incidence in a nationwide CHB cohort. The study population comprised the National Health Insurance Service claims database from January 1, 2013, to December 31, 2013, only included treatment naïve CHB patients and those without previously diagnosed with PD. Participants were followed until PD diagnosis or study completion. The primary outcome was PD incidence, comparing patients who initiated NUC therapy at cohort entry with those who did not. Over the 7.9-year study period, the incidence rate of PD in NUC-treated patients was 1.48 per 1000 persons, compared to 1.95 per 1000 persons in the untreated group. In an adjusted competing risk model, the 3-year follow-up showed a statistically significant reduction in risk (hazard ratio [HR]: 0.61; 95% confidence interval [CI] 0.39–0.97). In the propensity score-matched cohort of 18,365 pairs, the cumulative incidence during 2–4 years of follow-up was significantly lower in the NUC-treated group compared to the untreated group. However, no statistically significant difference in cumulative PD incidence was observed between the groups at the early or late stages of the follow-up period. NUC therapy initially reduced PD incidence, but this protective effect diminished over time, indicating a time-varying effect. Regular PD screening may be needed for long-term NUC users.
Similar content being viewed by others
Introduction
Chronic hepatitis B virus (CHB) infection has been a leading cause of cirrhosis and liver cancer1,2. To suppress the chronic inflammation caused by viral replication and to prevent the progression of liver disease, nucleos(t)ide analogs (NUC) have become the standard of care and now used worldwide3,4,5. Despite the effectiveness and utility of NUC therapy, unfortunately, current NUC therapy is not intended as a short-term cure, but rather to suppress viral proliferation for the duration of use, the prolonged duration of NUC therapy is inevitable3,6,7,8. As a result, most patients with CHB maintaining NUC therapy even decades of years after initiation3,6.
Toxicities such as myopathy, neuropathy, and nephropathy have been reported with NUC users in CHB, which mechanistically share mechanisms related to mitochondrial damage caused by NUC therapy9,10,11,12,13. In general, neurodegenerative disease (ND) is a representative disease associated with the accumulation of mitochondrial damage over time14,15. However, the impact of NUC therapy on development of ND in patients with CHB has not been studied.
Parkinson disease (PD) is one of the most common ND and has been associated with viral-induced chronic hepatitis16,17. In a previous study, it was reported that viral eradication in chronic hepatitis C reduced the incidence of PD in the long term. One of the possible mechanisms of this phenomenon may be a reduction in inflammatory cytokines and associated neuroinflammation due to chronic hepatitis18. In CHB, the use and maintenance of NUC may protect against PD development by suppressing the inflammatory process, while long-term NUC use may lead to mitochondrial damage and can be triggered earlier onset of PD.
In this context, we compared the incidence of PD over time in patients with CHB, with and without NUC therapy, using a national wide claims data from a CHB endemic area, to gain insight into whether NUC use is a risk factor or protective factor for PD in terms of therapeutic duration.
Materials and methods
Data source
This was a nationwide, population-level, historical cohort study using the National Health Insurance Service (NHIS) of the Republic of Korea. Approximately 97% of Korean residents are currently covered by health insurance based on employment or residential areas. NHIS has a comprehensive health database for diagnoses, treatments, procedures, and prescriptions19,20. Information on patient demographic characteristics, medical treatment records, and detailed diagnoses coded with the Korean Standard Classification of Disease Version 5 (modification of the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision [ICD-10]) were collected from all individuals.
Study population
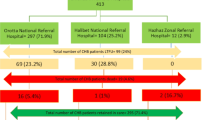
The study population comprised the NHIS claims database from January 1, 2013, to December 31, 2013, patients aged 30–70 years with CHB who have no experience with NUC therapy, not diagnosed with PD before cohort entry. (n = 273,503, Fig. 1) All patients had ICD-10 code B181 or B180, indicating a diagnosis of CHB. We defined PD diagnosed as individuals with primary or subsidiary diagnosis with an ICD-10 code for PD (G20), as used in previous study21,22. In NHIS registration system, all patients with a PD registration code are assured of being diagnosed by a neurologist with the definite criteria.
We excluded patients who were identified from before to 1 year after cohort entry; diagnosed with hepatitis C, HIV infection, or acute viral hepatitis; received an organ transplantation; diagnosed with hepatocellular carcinoma or other malignancy; and were diagnosed with stroke. In addition, patients who died within 1 year after cohort entry were excluded. The patients who were lost to follow-up within 6 months of the index date or developed PD within 6 months after the index date were also excluded. NUC use was defined as the newly initiated and continuous use of medications, with only those approved for first-line treatment at the time of cohort entry being included. The initiation of NUC therapy was based on established clinical guideline3. The patients who received NUC for less than 6 months were excluded in NUC treated group. The operational definitions used in this study are summarized in Supplementary Table 1.
After exclusion, a total of 238,219 patients were finally included in this study. Patients who were not prescribed NUC at all were classified as the untreated group. Patients who were prescribed NUC for CHB and adhered to the treatment regimen for more than 80% of the duration were categorized as the treated group. Patients who were treated with NUC and did not meet the adherence rate of 80% were excluded. (n = 7034) As a result, our cohort comprised 18,365 patients who received newly initiated NUC therapy (the treated group) and 212,820 patients who did not receive NUC therapy (the untreated group).
All baseline data, at the initial date of NUC therapy for the group receiving NUC; and at the first claim date for CHB during 2013 for the group without NUC, were obtained from the NHIS. We collected claims data encompassing age, sex, socioeconomic status, level of healthcare (primary, secondary, and tertiary care23), cirrhosis, and preexisting comorbidities such as diabetes mellitus, hypertension, dyslipidemia, chronic kidney disease, congestive heart failure, ischemic heart disease, and traumatic brain injury. Participants were followed from the index date until either the diagnosis of PD or the study’s conclusion on December 31, 2021. Individuals were censored at the date of death, as well as when NUC therapy was discontinued in the treatment group or newly initiated in the untreated group. This study was approved by the Institutional Review Board of Hanyang University Guri Hospital (IRB No. 2023-04-039), with all methods conducted in accordance with relevant guidelines and the Declaration of Helsinki. Written informed consent was waived due to the retrospective design.
Study outcome
The primary outcome of this study was the incidence of PD during the follow-up period, only those whose PD occurred more than 6 months after cohort entry were analyzed. We defined newly diagnosed cases of PD as individuals who were newly diagnosed with and if there were several claims with PD codes (G20), the first instance it occurred was considered the time of PD diagnosis. The secondary outcome was to identify the risk factors associated with PD in patients with CHB infection with or without NUC therapy.
Statistical analysis
All patients who met the eligibility criteria at baseline were included in the analyses. Categorical and continuous variables were compared using the Chi- square test and t- test respectively. The Cox proportional hazard model was used to compare the outcomes between the groups. We calculated the crude and adjusted hazard ratios (HRs) with 95% confidence intervals (CIs). The multivariable analysis included the following variables: age, sex, socioeconomic status, level of health care, and preexisting comorbidities such as diabetes mellitus, hypertension, dyslipidemia, chronic kidney disease, congestive heart failure, ischemic heart disease, traumatic brain injury, and cirrhosis. Since occurrence of death can lead to informative censoring in the assessment of the risk of PD, competing risk analysis was performed using Fine and Gray’s proportional sub- distribution hazard model24,25.
Propensity score (PS)- matching analysis was performed to reduce the effect of selection bias and potential confounding factors between the treated and non-treated groups. Propensity scores were derived using the following variables: age, sex, socioeconomic status, level of health care, and preexisting comorbidities such as diabetes mellitus, hypertension, dyslipidemia, chronic kidney disease, congestive heart failure, ischemic heart disease, traumatic brain injury, and cirrhosis. For propensity score matching, an SAS matching macro, “%OneToManyMTCH,” was used for this caliper matching of nearest-neighbor approach for the first four to eight digits of propensity scores.
The cumulative incidence risk of PD at 1, 2, 3, 4, 5, 6, and 7 years following NUC therapy. In addition, time-dependent effects were evaluated based on Schoenfeld’s residuals, and cubic spline functions were introduced in the model26,27,28. Kaplan–Meier method and compared using the log-rank test between treated and untreated groups both before and after PS matching. All statistical analyses were performed SAS Enterprise Guide 7.1(SAS Institute Inc., Cary, NC) and R, version 4.3.1 (http://cran.r- project.org/). All reported p values are two- sided, and p values < 0.05 were considered statistically significant.
Results
Table 1 shows baseline characteristics. The overall follow-up duration for the study population was 7.89 years. Patients receiving NUC therapy (n = 18,365) tended to be younger (47.82 ± 9.53 vs. 49.45 ± 10.36) and more male (60.76% vs. 52.68%), with a lower prevalence of comorbidities but a higher prevalence of cirrhosis (30.42% vs. 7.17%) compared to patients without NUC therapy (n = 212,820). After propensity score matching, the baseline characteristics of the two groups did not significantly differ for the matching covariates, indicating good balance between the groups. (n = 18,365 in both groups) During the study period, a total of 1646 patients were diagnosed with PD. In the group NUC therapy, the incidence density was 0.19 per 100,000 PYs, while it was 0.25 per 100,000 PYs in the group not receiving NUC. In the propensity score-matched cohort, the incidence of PD was higher in the non-NUC group (1.72 per 1000 person-years) compared to the NUC-treated group (1.48 per 1000 person-years). When compared with the reported incidence in the general population aged < 50 years (1.1–1.8 per 1,000 person-years), the incidence in both groups appeared comparable22.
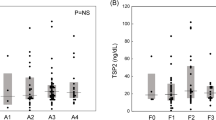
Table 2 shows the cumulative incidence and hazard ratios for PD at 1, 2, 3, 4, 5, 6, and 7 years of follow-up. When apply age-sex adjusted risk model, treated group had a significantly lower risk of developing PD at 3 and 4 years of follow-up (HR 0.57; 95% CI 0.37–0.89, HR 0.67; 95% CI 0.14–0.96, respectively). In the fully adjusted competing risk model, 3 years of follow-up (HR 0.61; 95% CI 0.39–0.97) showed statistical significance. In PS-matched cohort of 18,365 pairs, cumulative incidences of 2–4 years of follow-up groups showed statistically lower HR (0.50–0.58) in NUC treated group than untreated group. Figure 2 presents the HRs for the PS-matched cohort of 18,365 pairs in a forest plot. The risk of developing PD was initially lower in the treated group than its counterpart, but the risk of PD became comparable over time, losing statistical significance. In the Kaplan–Meier analysis, the log-rank test did not show statistical significance (Fig. 3A). However, the estimated hazard functions (Fig. 3B) indicate that the hazard ratio increased over time, initially favoring the treated group but approaching one by the end of the follow-up period.
In addition, we conducted a subgroup analysis using the matching variables selected for propensity score matching (Supplementary Table 2). While general trends indicated that the NUC-treated group had lower risk of PD than the untreated group across all subgroups, these differences did not reach statistical significance. Kaplan–Meier curves for representative subgroups (age, sex, and cirrhosis) showed similar duration-specific patterns to those observed in the entire cohort, except for patients aged ≥ 65 years. However, the log-rank test did not reveal any statistically significant differences (Supplementary Fig. 1).
Discussion
Currently, the NUC therapy in patients with CHB aims to achieve viral suppression, preventing liver disease progression. However, it requires continuous therapy for several years or even decades3,6,7 Effective viral suppression has been shown to protect against liver disease progression and reduce the occurrence of extrahepatic complications associated with chronic inflammation3. From the perspective of PD development, NUC therapy may offer a protective effect by suppressing viral activity17,29. However, prolonged NUC use carries potential risks, including an increased likelihood of neurodegenerative diseases due to underlying mechanisms such as accumulating mitochondrial damage9,10,14,15,30. Despite the widespread use of NUCs globally, there has been no research investigating the impact of NUCs on PD incidence.
In this study, we focused on NUC treatment-naïve patients at the time of cohort entry to compare the risk of PD development between those who initiated and maintained NUC therapy and those who did not. We aimed to explore the relationship between NUC use and PD incidence, as well as any hidden clinical phenotypes associated with the mechanism. Our study found that PD incidence decreased in the years following NUC initiation, but this protective effect diminished over time. These findings suggest that the duration of NUC therapy may have time-varying clinical impact on PD development in CHB patients, offering early protection but potential toxicity with long-term use.
In the subgroup analysis, designed to identify any groups where NUC treatment had a statistically significant advantage, showed a general trend of reduced PD incidence in the NUC-treated group, though no subgroup showed a clear statistical advantage. Additionally, based on existing literature, we performed Kaplan–Meier analysis on factors potentially related to PD (e.g., age, cirrhosis, and gender)16,22,31. Apart from patients over 65, the time-varying effect of NUC therapy was also observed in subgroups, suggesting that the changes in PD incidence over time may be related more to the effect of NUC treatment itself rather than specific subgroups. Whether the time-varying effects of NUC therapy on PD incidence are observed across different subgroups remains to be elucidated.
Previous studies on the relationship between CHB and PD incidence have yielded conflicting results17,32,33,34,35. A recent meta-analysis also confirmed inconsistent findings regarding PD incidence in CHB patients36. However, none of previous studies examined the effects of NUC use. Mechanistically, there have been reports linking hepatotropic virus infections, such as CHB, to PD development, suggesting an association with neuroinflammation due to chronic liver disease17,29,30. Studies on hepatitis C virus show that viral eradication can reduce PD risk18, indicating that viral suppression might similarly lower PD incidence in CHB. Unlike HCV, however, CHB treatment requires continuous NUC therapy, which may have positive effects on viral suppression but could also contribute to PD or other ND through mitochondrial damage. Non-human studies have shown that long-term exposure to NUCs can cause neuronal damage, raising concerns about the long-term toxicity of NUCs9,10,11,37. If the effects of NUCs on PD risk are time-varying, as suggested by our study, previous research may have failed to fully capture the relationship between CHB and PD incidence. Further research is needed to elucidate the underlying mechanisms behind the time-varying effects of NUC use on PD risk, as seen in our findings.
Strength and limitations
This study compares patient groups with and without NUC therapy, evaluating the potential clinical implications of the time-varying effects of NUCs. A major strength is the use of a large-scale national database, with a long median follow-up of approximately 8 years, allowing us to observe clinical phenotypes potentially related to the time-varying effects of NUCs. Additionally, the calculation of period-specific cumulative hazards and the examination of hazard functions effectively demonstrate the impact of NUC therapy for CHB on the incidence of PD27,28. While the retrospective observational design of this study introduces inherent limitations, we mitigated these by leveraging a nationally representative dataset from a CHB-endemic region. We employed stringent exclusion criteria to accurately evaluate the potential impact of NUC therapy on PD incidence in CHB patients. To further minimize confounding, we used propensity score matching and incorporated competing risk analysis to enhance the robustness of our findings. Another limitation is the inability to account for variables not included in the claims data, such as known PD risk factors or the effects of medications other than NUCs. The impact of unmeasured variables, including baseline and serial laboratory data related to viral status, chronic inflammation, and cirrhosis (e.g., viral DNA, ALT, Fib-4, and Child–Pugh score), on the association between NUC use and PD incidence remains uncertain. Additionally, it remains unclear how PD incidence might be influenced by NUC use or non-use outside of insurance coverage or due to individual clinical decisions. Furthermore, we were unable to fully elucidate the underlying mechanisms, and it remains unclear whether other neurodegenerative diseases that share mitochondrial damage as a common mechanism exhibit similar incidence patterns. Differences based on CHB subtypes, race, or the type of NUC used were also not explored. Although these factors may have had differential effects on PD incidence, they could not be separately analyzed in this study. Despite these limitations, our study is the first to investigate the various mechanisms of PD development, including neuroinflammation from chronic liver inflammation and mitochondrial damage caused by long-term NUC therapy.
Conclusion
In patients with CHB, initiating NUC therapy initially provided a protective effect against PD incidence; however, this effect diminished over time, suggesting a clinically relevant time-varying impact, possibly related to the long-term toxicity of NUCs. Given the necessity of long-term NUC therapy for CHB management, there may be a need for PD screening in long-term NUC users. Further studies are needed to replicate these findings and confirm their validity.
Data availability
Data used in this study are maintained by the Korea National Health Insurance Service (NHIS, https://nhiss.nhis.or.kr), and available from corresponding author upon submitting a proposal to be approved by the NHIS.
Abbreviations
- CHB:
-
Chronic hepatitis B virus
- CIs:
-
Confidence intervals
- HRs:
-
Hazard ratios
- NUCs:
-
Nucleos(t)ide analogs
- ND:
-
Neurodegenerative disease
- NHIS:
-
The National Health Insurance Service
- PD:
-
Parkinson disease
- PS:
-
Propensity score
References
Global, regional, and national burden of hepatitis B, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol. Hepatol. 7, 796–829. https://doi.org/10.1016/S2468-1253(22)00124-8 (2022).
Huang, D. Q. et al. Global epidemiology of cirrhosis: Aetiology, trends and predictions. Nat. Rev. Gastroenterol. Hepatol. 20, 388–398. https://doi.org/10.1038/s41575-023-00759-2 (2023).
Korean Association for the Study of the, L. KASL clinical practice guidelines for management of chronic hepatitis B. Clin. Mol. Hepatol. 28, 276–331. https://doi.org/10.3350/cmh.2022.0084 (2022).
Terrault, N. A. et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology 67, 1560–1599. https://doi.org/10.1002/hep.29800 (2018).
Lampertico, P. et al. EASL 2017 clinical practice guidelines on the management of hepatitis B virus infection. J. Hepatol. 67(2), 370–398. https://doi.org/10.1016/j.jhep.2017.03.021 (2017).
Hsu, Y. C., Tseng, C. H. & Kao, J. H. Safety considerations for withdrawal of nucleos(t)ide analogues in patients with chronic hepatitis B: First, do no harm. Clin. Mol. Hepatol. 29, 869–890. https://doi.org/10.3350/cmh.2022.0420 (2023).
Liem, K. S., Gehring, A. J., Feld, J. J. & Janssen, H. L. A. Challenges With stopping long-term nucleos(t)ide analogue therapy in patients with chronic hepatitis B. Gastroenterology 158, 1185–1190. https://doi.org/10.1053/j.gastro.2019.10.050 (2020).
Roade, L., Riveiro-Barciela, M., Esteban, R. & Buti, M. Long-term efficacy and safety of nucleos(t)ides analogues in patients with chronic hepatitis B. Ther. Adv. Infect. Dis. 8, 2049936120985954. https://doi.org/10.1177/2049936120985954 (2021).
de Fraga, R. S., Van Vaisberg, V., Mendes, L. C. A., Carrilho, F. J. & Ono, S. K. Adverse events of nucleos(t)ide analogues for chronic hepatitis B: A systematic review. J. Gastroenterol. 55, 496–514. https://doi.org/10.1007/s00535-020-01680-0 (2020).
Fontana, R. J. Side effects of long-term oral antiviral therapy for hepatitis B. Hepatology 49, S185-195. https://doi.org/10.1002/hep.22885 (2009).
Fleischer, R. D. & Lok, A. S. Myopathy and neuropathy associated with nucleos(t)ide analog therapy for hepatitis B. J. Hepatol. 51, 787–791. https://doi.org/10.1016/j.jhep.2009.06.011 (2009).
Madeddu, G. et al. Mitochondrial toxicity and body shape changes during nucleos(t)ide analogues administration in patients with chronic hepatitis B. Sci. Rep. 10, 2014. https://doi.org/10.1038/s41598-020-58837-3 (2020).
Feng, J. Y. Addressing the selectivity and toxicity of antiviral nucleosides. Antivir. Chem. Chemother. 26, 2040206618758524. https://doi.org/10.1177/2040206618758524 (2018).
Lin, M. T. & Beal, M. F. Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature 443, 787–795. https://doi.org/10.1038/nature05292 (2006).
Bose, A. & Beal, M. F. Mitochondrial dysfunction in Parkinson’s disease. J. Neurochem. 139(Suppl 1), 216–231. https://doi.org/10.1111/jnc.13731 (2016).
Ben-Shlomo, Y. et al. The epidemiology of Parkinson’s disease. Lancet 403, 283–292. https://doi.org/10.1016/S0140-6736(23)01419-8 (2024).
Pakpoor, J. et al. Viral hepatitis and Parkinson disease: A national record-linkage study. Neurology 88, 1630–1633 (2017).
Lin, W. Y. et al. Association of antiviral therapy with risk of Parkinson disease in patients with chronic hepatitis C virus Infection. JAMA Neurol. 76, 1019–1027. https://doi.org/10.1001/jamaneurol.2019.1368 (2019).
Kyoung, D. S. & Kim, H. S. Understanding and utilizing claim data from the Korean National Health Insurance Service (NHIS) and health insurance review & assessment (HIRA) database for research. J. Lipid Atheroscler. 11, 103–110. https://doi.org/10.12997/jla.2022.11.2.103 (2022).
Lim, J., Kim, Y. J., Kim, S. & Choi, J. Increased risk of osteoporotic fracture in patients with autoimmune hepatitis. Am. J. Gastroenterol. https://doi.org/10.14309/ajg.0000000000002354 (2023).
Jo, S. et al. Association of NO2 and other air pollution exposures with the risk of Parkinson disease. JAMA Neurol. 78, 800–808. https://doi.org/10.1001/jamaneurol.2021.1335 (2021).
Park, J. H. et al. Trends in the incidence and prevalence of Parkinson’s disease in Korea: A nationwide, population-based study. BMC Geriatr. 19, 320. https://doi.org/10.1186/s12877-019-1332-7 (2019).
Kim, J. A., Yoon, S., Kim, L. Y. & Kim, D. S. Towards actualizing the value potential of Korea health insurance review and assessment (hira) data as a resource for health research: Strengths, limitations, applications, and strategies for optimal use of HIRA data. J. Kor. Med. Sci. 32, 718–728. https://doi.org/10.3346/jkms.2017.32.5.718 (2017).
Fine, J. P. & Gray, R. J. A proportional hazards model for the subdistribution of a competing risk. J. Am. Stat. Assoc. 94, 496–509. https://doi.org/10.1080/01621459.1999.10474144 (1999).
Kim, G. A. et al. Association between non-alcoholic fatty liver disease and the risk of dementia: A nationwide cohort study. Liver Int. 42, 1027–1036. https://doi.org/10.1111/liv.15244 (2022).
Wileyto, E. P., Li, Y., Chen, J. & Heitjan, D. F. Assessing the fit of parametric cure models. Biostatistics 14, 340–350. https://doi.org/10.1093/biostatistics/kxs043 (2013).
Uno, H. et al. Moving beyond the hazard ratio in quantifying the between-group difference in survival analysis. J. Clin. Oncol. 32, 2380–2385. https://doi.org/10.1200/JCO.2014.55.2208 (2014).
Huang, Q. & Tian, C. Visualizing time-varying effect in survival analysis: 5 complementary plots to Kaplan–Meier curve. Oxid Med Cell Longev 2022, 3934901. https://doi.org/10.1155/2022/3934901 (2022).
Felipo, V., Montoliu, C. & Llansola, M. Neuroinflammation and neurological alterations in chronic liver diseases. Neuroimmunol. Neuroinflammation https://doi.org/10.4103/2347-8659.160845 (2015).
Morris, H. R., Spillantini, M. G., Sue, C. M. & Williams-Gray, C. H. The pathogenesis of Parkinson’s disease. Lancet 403, 293–304. https://doi.org/10.1016/S0140-6736(23)01478-2 (2024).
Apetauerova, D. et al. A prospective study of the prevalence of parkinsonism in patients with liver cirrhosis. Hepatol. Commun. 5, 323–333. https://doi.org/10.1002/hep4.1624 (2021).
Choi, H. Y., Mai, T. H., Kim, K. A., Cho, H. & Ki, M. Association between viral hepatitis infection and Parkinson’s disease: A population-based prospective study. J. Viral Hepat. 27, 1171–1178. https://doi.org/10.1111/jvh.13346 (2020).
Goldstein, L., Fogel-Grinvald, H. & Steiner, I. Hepatitis B and C virus infection as a risk factor for Parkinson’s disease in Israel-A nationwide cohort study. J. Neurol. Sci. 398, 138–141. https://doi.org/10.1016/j.jns.2019.01.012 (2019).
Golabi, P. et al. The prevalence of Parkinson disease among patients with hepatitis C infection. Ann. Hepatol. 16, 342–348. https://doi.org/10.5604/01.3001.0009.8588 (2017).
Wu, W. Y. et al. Hepatitis C virus infection: A risk factor for Parkinson’s disease. J. Viral Hepat. 22, 784–791. https://doi.org/10.1111/jvh.12392 (2015).
Yaow, C. Y. L. et al. Risk of Parkinson’s disease in hepatitis B and C populations: A systematic review and meta-analysis. J. Neural Transm. (Vienna) https://doi.org/10.1007/s00702-023-02705-7 (2023).
Zhang, Y. et al. Long-term exposure of mice to nucleoside analogues disrupts mitochondrial DNA maintenance in cortical neurons. PLoS ONE 9, e85637. https://doi.org/10.1371/journal.pone.0085637 (2014).
Funding
This study was supported by The Research Supporting Program of the Korean Association for the Study of the Liver (KASL2023-04), and by the Research fund of Hanyang University (HY-202500000001286).
Author information
Authors and Affiliations
Contributions
JL, HYL, HS, and HIK were involved in the study concept and design, data analysis, interpretation, drafting of the manuscript, and critical revision of the manuscript. HS, HIK, and SJJ were involved in data acquisition, data analysis, interpretation, and study supervision. All authors were responsible for the data acquisition and critical revision of the manuscript and approved the final version. JL, HYL, and HS contributed equally to this work and share first authorship.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lim, J., Lee, H.Y., Sang, H. et al. Association of nucleos(t)ide analogue therapy with Parkinson disease in chronic hepatitis B patients. Sci Rep 15, 15192 (2025). https://doi.org/10.1038/s41598-025-00110-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-00110-6