Abstract
Assessing non-suicidal self-injury (NSSI) in adolescents and young adults is a critical yet challenging aspect of psychiatric evaluations for hospitalized patients. This study aimed to develop a detective model for probability of NSSI in adolescents and young adults utilizing a retrospective cross-sectional analysis. Data from 658 hospitalized adolescents and young adults, including demographic characteristics, hormone levels, and violence risk factors, were collected. Age, history of suicide attempts, gender, and psychiatric diagnosis were identified as key detectors through Boruta and LASSO machine learning algorithms, leading to the construction of a nomogram. Model performance was evaluated based on discrimination, calibration, and decision curve analysis (DCA). The model achieved the area under the receiver operating characteristic curve (AUC) values of 0.803 (training set; 95% CI 0.763–0.843) and 0.745 (validation set; 95% CI 0.676–0.814). Calibration plots demonstrated strong alignment between predicted and actual outcomes. The Hosmer-Lemeshow test indicated good model fit, while DCA revealed clinically relevant threshold ranges for the training and validation sets, highlighting the model’s potential to inform clinical decision-making. This detective model can support the rational allocation of medical resources and facilitate the early detection and intervention of NSSI behaviors in hospitalized adolescents and young adults.
Similar content being viewed by others
Introduction
Non-suicidal self-injury (NSSI) involves deliberate and repeated harm to one’s body without suicidal intent and includes behaviors such as cutting, needle pricking, scratching, hitting, and burning1. Typically emerging during adolescence, NSSI is closely associated with suicidal ideation, and potentially serves as a precursor to suicide2. Additionally, NSSI frequently co-occurs with violent behaviors and has been linked to violent crimes alongside self-harm3. Studies have indicated that the prevalence of NSSI among adolescents and young adults is estimated to range from 18 to 38%4,5,6. NSSI significantly impacts the physical appearance and psychological well-being of adolescents and young adults. Early and accurate identification probability of NSSI is essential for prevention. For individuals at risk or those who have already engaged in NSSI, timely pharmacological and psychological interventions can prevent the continuation of these behaviors into adulthood7. Currently, antidepressants may be prescribed to regulate mood, while psychological interventions often involve intensive community care, cognitive behavioral therapy (CBT), and dialectical behavioral therapy (DBT), the latter demonstrating significant efficacy in addressing self-harm behaviors8. Detecting probability of NSSI in hospitalized adolescents and young adults with mental disorders (AYAMD) and implementing tiered prevention strategies based on probability levels of NSSI hold significant clinical and societal implications.
Accurately detecting probability of NSSI in hospitalized AYAMD poses a challenge for healthcare professionals. Adolescence is characterized by profound biological, psychological, and social changes, and represents a critical period for behavioral, cognitive, emotional, and physical development. This phase of life is marked by heightened vulnerability9. Despite extensive research, the mechanisms underlying NSSI remain unclear. Studies suggest that NSSI is associated with various factors, including psychosocial stressors, unhealthy emotional regulation, abnormal brain function, altered neurochemical metabolism, hypothalamic-pituitary-adrenal axis dysfunction, and altered pain perception10. Additionally, research has revealed correlations between NSSI and various serum hormones, including thyroid hormones and cortisol11,12. Research indicates that the most commonly reported factors for NSSI include female gender, a history of NSSI, and psychiatric diagnoses, alongside adverse childhood experiences, bullying, behavioral disorders, and somatic symptoms13,14. Poor mental health is closely associated with NSSI, irrespective of age or gender15. Incorporating these predictive factors into clinical models could significantly enhance the detection probability of NSSI in AYAMD.
Existing clinical tools for assessing probability of NSSI have notable limitations. A systematic review published in 2021 highlighted insufficient evidence for the reliability and validity of current tools in clinical settings, underscoring the need for higher-quality assessment tools16. While tools such as the Ottawa Self-Injury Inventory17 and Self-Injurious Thoughts and Behaviors Interview18 are widely utilized as a result of their comprehensive assessment capabilities19, their reliability may be compromised. For instance, patients can become disengaged during lengthy assessments, and parents may be reluctant to report their children’s past NSSI behaviors, affecting the reliability of the assessment results20. Moreover, single-item assessments and procedural evaluations may overlook individuals exhibiting atypical behaviors or those unwilling to self-identify as engaging in NSSI. Clinical interviews are also subject to recall and expectation biases as a result of the patients’ cognitive limitations or fear of punitive consequences21. Currently, few predictive models for NSSI in AYAMD exist, and no models specifically designed for use by healthcare professionals have been published. Therefore, there is a pressing need for a reliable detective model to identify probability of NSSI in hospitalized adolescents and support the development of effective intervention strategies.
Against this backdrop, the primary objective of this study is to analyze potential correlates of NSSI. Additionally, this study aims to develop a clinical detection model for assessing probability of NSSI in hospitalized AYAMD, providing a valuable tool for healthcare professionals.
Methods
Study design and participants
This retrospective study was conducted at a 4,500-bed university-affiliated medical centre in China. The methodology adhered to the updated version of Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis statement22. Eligible participants met the following inclusion criteria: (1) diagnosis of a mental disorder according to the International Classification of Diseases, 10th Edition, including depressive and anxiety disorders, affective disorders, schizophrenia, and childhood emotional disorders; (2) age between 15 and 29 years; and (3) hospitalization for treatment. Exclusion criteria included: (1) neurological diseases; (2) prolactinomas, pituitary tumours, or other endocrine system diseases; (3) organic mental disorders; and (4) incomplete clinical data with missing values for two or more intended variables. The sample size was determined utilizing the events-per-variable principle23, which is commonly utilized in the development of clinical prediction models and suggests that the ratio of patients experiencing clinical outcome events to the number of candidate predictor parameters should be at least five. Based on the formula N = EPV × X/P23, where N is the sample size, X is the number of predictor variables (24 in this study), and P is the prevalence rate of NSSI, we estimated a minimum sample size of 480 cases. This calculation assumed a 50% prevalence rate of NSSI, based on prior studies exhibiting a higher prevalence in clinical settings compared to community samples24. The EPV was set at 20 to ensure robust model development. Meanwhile, considering the large sample size required for machine learning.
NSSI assessment
NSSI was assessed following the criteria in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition1. Patients or their primary caregivers were interviewed about self-harming behaviours that may have occurred within the past 12 months, including (but are not limited to) cutting, needle pricking, scratching, hitting, and burning. Any occurrence of these behaviours during the specified period was classified as NSSI.
Brøset violence checklist
Given the potential correlation between aggression and NSSI, aggressive behavior was assessed utilizing the Brøset Violence Checklist (BVC), which assesses the risk of violence over a 24-hour period25. The BVC comprises six items—confusion, irritability, noise-making, physical threat, verbal threat, and object aggression—scored as 0 (none) or 1 (present). Total scores range from 0 to 6, with higher scores indicating greater risk. The BVC captures aggression toward oneself, others, and objects, providing a comprehensive tool for evaluating the risk of violence throughout the inpatient treatment process26.
Data access and collection
Data were extracted from the hospital information system. Collected variables included demographic and clinical characteristics such as age, gender, body mass index, marital status, education level, employment status, disease duration, hormone levels, hospitalization history, family history of mental illness, prior NSSI, suicide attempts, and psychotropic medication utilization. For patients with multiple admissions, data from the most recent admission were analyzed. Laboratory data primarily comprised prolactin, adrenocorticotropic hormone, plasma total cortisol, and thyroxine levels, measured from fasting blood samples taken between 7:00 and 8:00 AM on the morning following admission. Predictors included in the model, such as the number of previous suicide attempts, and other variables, were classified as categorical variables or continuous variables depending on their data types and clinical significance. In this study, the BVC and other assessments were administered by registered psychiatric professionals.
Quality control
The following series of measures to ensure the quality of the research wee utilized. First, the principal investigator conducted uniform training for all research personnel to ensure they understood the purpose of the study and their respective tasks. Second, pre-designed, standardized, and normalized data extraction forms that encompassed all required data items were utilized. Third, data collection was independently carried out by two designated researchers to ensure consistency, accuracy, and completeness in the collection methods. Discrepancies were resolved through consensus with the research leader.
Data analysis
Data analysis was performed utilizing SPSS (Version 26.0) and R (Version 4.1.3) software. For cases with missing data in ≤ 2 variables, the Multivariate Imputation by Chained Equations (MICE) method was applied utilizing the “mice” package in R, developed by Stef van Buuren. This approach handled missing values utilizing multiple imputation to enhance the completeness and reliability of the dataset for subsequent analysis. The “mice” package operates under the assumption of Missing at Random, where the likelihood of missing data is unrelated to the unobserved data but may depend on the observed data. The MICE iteratively impute missing values by modeling each incomplete variable as a function of the other variables, including the imputed values from prior iterations, until the imputed values stabilize across multiple iterations. Two-tailed p-values < 0.05 were considered statistically significant. Continuous data were statistically described utilizing mean ± standard deviation, while discrete data were statistically described utilizing percentages. Comparisons between training and validation datasets were conducted utilizing chi-square tests.
When designing predictive factor selection for the model, this study concurrently employed the machine learning Boruta algorithm and Logistic Least Absolute Shrinkage and Selection Operator (LASSO) regression analysis for data analysis. The Boruta algorithm, implemented utilizing the “boruta” package in R, is a feature selection method based on the random forest classifier. It injects randomness into the dataset by creating shadow features, which are shuffled versions of the original features. The algorithm iteratively compares the importance of each original feature with these shadow features to determine whether the original feature holds more significance. Features deemed less important than the shadow features are pruned, resulting in a minimal and optimal subset of features with greater stability than those selected by a single random forest model27. Initially, the Boruta algorithm was utilized to confirm important predictive factors28. Subsequently, the LASSO regression algorithm was applied to select clinically predictive factors from the risk characteristics of AYAMD patients. LASSO regression, conducted utilizing the “glmnet” package in R, is a regularization technique that assists with automatically eliminating non-influential variables from a potentially large and multicollinear set of predictors. This method applies a penalty (L1- norm or lambda, λ) to shrink some coefficients to zero, effectively removing irrelevant predictors, which assists with preventing overfitting, producing a more interpretable set of predictors29. The optimal λ was selected utilizing a 5-fold cross-validation30.
To integrate these outcomes into a single metric, we took the intersection of the features identified by both methods. For each intersecting feature, we selected the most significant variables based on their rankings in both methods. Finally, an integrated feature importance metric was created based on the feature importance ranking from the Boruta algorithm and the magnitude of coefficients from LASSO. Based on this metric, a nomogram prediction model was constructed. Developing a nomogram involves running a logistic regression model and then converting the results into a visual nomogram. In the R packages utilized, the nomogram and calibration curve were created utilizing the “rms” package. Decision Curve Analysis (DCA) was performed with the “dca.R” package. Additionally, the receiver operating characteristic curve (ROC curve) was plotted utilizing the “pROC” package. The “reportROC” package calculated the optimal cutoff for binary classification of NSSI probability.
Model performance evaluation included discrimination, calibration, and DCA. Discrimination was assessed utilizing the area under the receiver operating characteristic curve (AUC). Typically, AUC values of < 0.6, 0.6 to 0.8, and > 0.8 indicate poor, moderate, and good discrimination, respectively31. The ROC and AUC are commonly utilized to assess a model’s ability to differentiate between patients who experience an event and those who do not. While these metrics measure discrimination, they do not evaluate whether the model provides clinical benefit. Calibration, which assesses the consistency between detected probabilities and observed outcomes, complements discrimination by measuring the accuracy of absolute probability predictions. DCA was applied to evaluate the clinical utility of the model. Compared with traditional discrimination and calibration metrics, the advantage of DCA lies in its ability to provide guidance for the decision-making process regarding the use of prediction models in clinical practice32. DCA thresholds were predefined as 25 − 50% to align with clinical resource constraints.
Ethical considerations
The study was approved by the Institutional Review Board of West China Hospital of Sichuan University (approval number: 2023-517). Data confidentiality was maintained throughout, and the study adhered to the principles of the Declaration of Helsinki. The requirement for informed consent was waived by the Medical Ethics Committee as a result of the retrospective nature of the research.
Results
Participant characteristics
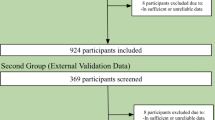
From October 2022 to March 2024, 658 patients who met the inclusion and exclusion criteria were enrolled. These patients were randomly assigned to either the training set (N = 461) or the validation set (N = 197) in a 7:3 ratio. Patients were further categorized into two groups based on their history of NSSI: those with a history of NSSI and those without. The overall NSSI prevalence was 50.9%, with rates of 51.8% in the training set and 48.7% in the validation set. The study flow and general patient characteristics are depicted in Fig. 1; Table 1.
Identification of predictive factors
The Boruta algorithm was employed to identify predictive variables, resulting in the selection of 10 significant predictors ranked by feature importance: history of suicide attempts, age, gender, psychiatric diagnosis, employment status, cortisol levels, education level, history of psychotropic medication use, history of antipsychotic medication use, and marital status (Fig. 2). Subsequently, LASSO regression analysis was performed to filter potential predictors, identifying four variables with non-zero coefficients: psychiatric diagnosis, history of suicide attempts, gender, and age (Fig. 3).
Development of the nomogram
Based on the results of the Boruta and LASSO algorithms, four predictive factors were selected for the final model: age, history of suicide attempts, gender, and psychiatric diagnosis. The logistic regression analysis for predictors is detailed in Table 2. These variables formed a visual model of nomogram for detecting probability of NSSI in AYAMD (Fig. 4). The optimal cutoff value of 0.404 was calculated using Youden’s index, converting continuous NSSI probability into binary high/low probability labels for clinical use.
The nomogram of predictors. ICD-10: International classification of diseases, 10th revision. F20–F29: Schizophrenia, schizotypal and delusional disorders; F30–F39: Mood [affective] disorders; F40–F48: Neurotic, stress-related and somatoform disorders; F50–F59: Behavioral syndromes associated with physiological disturbances and physical factors; F90–F98: Behavioral and emotional disorders with onset usually occurring in childhood and adolescence. To interpret the nomogram, first locate the value of each predictor on the corresponding scale and draw a vertical line upward to the “Points” bar to obtain the assigned points for that predictor. Next, sum the points for all predictors. Finally, draw a vertical line downward from the “Total Points” line to the “Probability of NSSI” scale to determine the detected probability of NSSI.
Validation of the nomogram
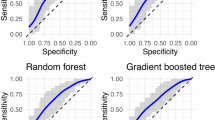
The AUC values for the training and validation sets were 0.803 (95% CI: 0.763–0.843) and 0.745 (95% CI: 0.676–0.814), respectively, indicating a moderate level of discrimination (Fig. 5). The Hosmer-Lemeshow goodness-of-fit test exhibited no statistically significant differences between the model’s predicted rate and observed NSSI rates, confirming good model fit (χ2 = 14.626, P = 0.067 for the training set; χ2 = 14.984, P = 0.061 for the validation set). Calibration curves further demonstrated high concordance between the predicted and actual NSSI probabilities (Fig. 6), underscoring the model’s accuracy. DCA curves for the training and validation sets indicated that within the pre-specified threshold range of 25 − 50%, the model generated significant net benefit, outperforming both the “All” and “None” strategies (Fig. 7).
Decision curve analysis of the detection model in the training (A) and validation (B) sets. The x-axis represents the threshold probability, and the y-axis represents the net benefit of detecting NSSI. The gray curve represents the net benefit assuming all patients are treated, while the black line assumes none are treated. The red and blue lines show the net benefit of using the nomogram in the validation and training sets, respectively. The embedded table lists the corresponding net benefit values across selected threshold probabilities in the validation set.
Discussion
This study introduced a visual detective model for evaluating the probability of NSSI among AYAMD patients, incorporating clinical factors such as age, gender, history of suicide attempts, and psychiatric diagnosis. The model demonstrated a good overall fit, satisfactory discrimination and robust calibration. It provides clinicians and nurses with a practical tool to detect probability of NSSI among hospitalized AYAMD patients on an individual basis.
The selection of predictive factors is a critical step in developing any predictive model, as it directly impacts the model’s quality. Identifying the most suitable predictive factors not only prevents overfitting but also reduces data collection costs, simplifies model structure, and saves computational time. These features make the model more interpretable, practical and easier to disseminate and apply33. A key strength of this study lies in its integration of the clinical realities of AYAMD patients with prior research on NSSI to identify candidate predictive factors. Machine learning algorithms, specifically with the Boruta algorithm and LASSO regression, were employed to screen and select the most relevant predictive factors for NSSI.
Prior research has established that NSSI typically emerges during adolescence, with risk decreasing gradually into adulthood34. Studies also highlight a strong association between suicide attempt history and NSSI, with patients exhibiting multiple suicide attempts being at higher risk of engaging in NSSI5,35. This behavior often serves as a means of alleviating internal distress36. Repeated suicide attempts may further normalize or facilitate NSSI behaviors37. To retain valuable information and reduce the risk of Type I errors, this study treated age and the number of suicide attempts as continuous variables rather than binary categories38. This approach allowed for greater precision in assigning predictive scores enhancing the model’s utility.
Few prior studies have developed predictive models based on clinical factors such as age, gender, history of suicide attempts, and psychiatric diagnosis, particularly in hospital settings. The majority of NSSI research has been conducted in community and school environments. There is a scarcity of predictive models developed specifically for clinical environments. Liang’s study39, developed a model for female patients with affective disorders (N = 396), utilizing marital status, age of onset, polarity of onset, first-episode psychotic symptoms, social dysfunction, and number of hospitalizations to build a model. Their model achieved a C-index of 0.73. Despite using only four predictors, our model achieved an AUC of 0.745 in the validation set and demonstrated significant clinical utility via DCA. By integrating clinical factors (e.g., intensive psychotherapy, pharmacotherapy, closed-ward care) and clinician preferences, the model evaluates net benefit across a 25–50% threshold range, dynamically balancing detection efficiency and risk of over-intervention. Threshold adjustment is recommended based on clinical context: 25% for high-risk screening and 50% for resource-constrained precision intervention, ensuring practicality and enabling rapid classification of patients into binary NSSI probability labels for clinical decision-making. For instance, at a 40% threshold probability (Fig. 7B), the model’s net benefit was 0.26, indicating that 26 true NSSI cases would be detected per 100 patients without increasing false positives. In contrast, the “All” strategy detected only 15 true positives, meaning the model provided 10 additional true positives compared to universal treatment, again without false positive increases40.
NSSI often occurs covertly, with many patients unwilling to disclose their behaviors voluntarily. In many cases, NSSI is discovered by parents or schools, prompting hospitalization41. Some patients may have already engaged in NSSI prior to admission42. Professional assessment of NSSI post admission can be cumbersome, potentially leading to adolescents developing adverse feelings towards the evaluation process, as well as introducing a time lag. The assessment results require analysis and correction by professionals, which is time-consuming and labor-intensive, leading to low diagnostic efficiency. Furthermore, patients at risk of NSSI are more likely to bring dangerous items—such as knives—into the ward, increasing the probability of secondary NSSI incidents in the hospital, requiring special attention from nursing staff43. This study advances assessment to the admission stage utilizing a simple and efficient method, providing medical staff with time and space to increase levels of protection and implement more targeted interventions for any patients identified as high probability of NSSI, thereby enhancing the clinical effectiveness of NSSI prevention. The observed rate of NSSI (approximately 50%) is indeed quite high, which poses certain challenges to any diagnostic algorithm. As highlighted by van Calster et al. (2018), when the baseline prevalence is very high, a model may face difficulty in reducing risk estimates to levels where patients would refuse treatment40. Integrating psychological scales could represent an innovative direction for future research to address model limitations in high-prevalence scenarios, especially applicable to mental disorders like NSSI that require personalized decisions.
The detective model can serve as a reference for clinical medical staff in decision-making and patient communication. Although Grimes44 pointed out that nomograms may be considered outdated in clinical practice as a result of the availability of simple computer programs, we believe they still hold value by providing readers with a clear and intuitive visualization of how the algorithm works. This is particularly beneficial compared to presenting only the formula with model estimates, such as intercepts and weights.
Additionally, prior studies have suggested a relationship between NSSI and dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis45. However, in our study, although serum hormones related to the HPA axis, such as plasma total cortisol, adrenocorticotropic hormone, thyroxine, and prolactin, were included in the analysis, they were not selected as detective factors. This finding suggests a limited correlation between these hormones and NSSI in our dataset. Research on the association between serum hormones and NSSI remains preliminary, with numerous potential mechanisms yet to be fully explored and elucidated. Future studies with broader methodologies and deeper analyses are needed to uncover the biological basis of NSSI and provide scientific evidence for developing effective interventions.
Despite its contributions, this study has certain limitations. Firstly, the data were derived from a single-center case sample, potentially limiting the model’s generalizability. Future studies should validate and refine the model’s detective ability utilizing multi-center data. Second, while the clinical detection model effectively predicts probability of NSSI, it cannot replace the experience and clinical judgment of healthcare professionals. It should serve as an auxiliary tool, combined with the judgment of professional medical staff, to guide clinical decision-making rather than a standalone decision. Third, national, sociocultural, and environmental factors were not included, potentially reducing the model’s accuracy across diverse populations. Future research should consider incorporating sociocultural variables to ensure the model’s relevance in various sociocultural contexts. Fourth, interactions between predictors could reveal valuable insights and potentially enhance predictive accuracy. For instance, factors such as age, gender, and history of suicide attempts may interact in complex ways to influence NSSI. Future research should investigate these interactions to uncover additional insights and improve predictive accuracy for clinical use. Fifth, the use of a single random split of the sample to conduct the DCA is a limitation of this study. Although this method is straightforward, it may produce unstable or biased estimates of model performance due to the inherent variability in data partitioning. Future research should consider employing more robust resampling techniques—such as k-fold cross-validation or bootstrapping—to improve the reliability and generalizability of model evaluation46. Finally, the model relies solely on clinical data and does not account for psychological or behavioral factors. Incorporating qualitative research findings could further refine the model.
It is important to note that NSSI is just one factor considered by clinicians when designing treatment plans. Cognitive function, emotional state, sleep quality, and psychiatric symptoms are also critical. Therefore, while this model offers valuable guidance, it should be perceived as part of a comprehensive clinical assessment to inform treatment decisions.
Conclusions
This study highlights that age, gender, history of suicide attempts, and psychiatric diagnosis are key factors for detecting the probability of NSSI. The visual model developed from these factors provides an effective tool for estimating probability of NSSI among AYAMD aged 15–29. By integrating these predictive factors into clinical practice, the model has the potential to enhance workflow efficiency, optimize resource allocation, and alleviate the healthcare burden associated with managing NSSI. Importantly, this model supports early detection and timely intervention for high probability of NSSI patients, contributing to more effective mental health care delivery and improved clinical outcomes, ultimately promoting patient well-being.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Zetterqvist, M. The DSM-5 diagnosis of nonsuicidal self-injury disorder: a review of the empirical literature. Child. Adolesc. Psychiatry Mental Health 9, 31. https://doi.org/10.1186/s13034-015-0062-7 (2015).
Kiekens, G. et al. The associations between non-suicidal self-injury and first onset suicidal thoughts and behaviors. J. Affect. Disord. 239, 171–179. https://doi.org/10.1016/j.jad.2018.06.033 (2018).
Richmond-Rakerd, L. S. et al. Adolescents who self-harm and commit violent crime: Testing early-life predictors of dual harm in a longitudinal cohort study. Am. J. Psychiatry. 176, 186–195. https://doi.org/10.1176/appi.ajp.2018.18060740 (2019).
Whitlock, J., Prussien, K. & Pietrusza, C. Predictors of self-injury cessation and subsequent psychological growth: Results of a probability sample survey of students in eight universities and colleges. Child. Adolesc. Psychiatry Mental Health 9, 19. https://doi.org/10.1186/s13034-015-0048-5 (2015).
Zhang, P. et al. A cross-sectional epidemiological study of non-suicidal self-injury prevalence in Chinese psychiatric patients. Nat. Mental Health 1, 266–272. https://doi.org/10.1038/s44220-023-00050-y (2023).
Muehlenkamp, J. J., Claes, L., Havertape, L. & Plener, P. L. International prevalence of adolescent non-suicidal self-injury and deliberate self-harm. Child. Adolesc. Psychiatry Mental Health 6, 10. https://doi.org/10.1186/1753-2000-6-10 (2012).
Reinhardt, M., Rice, K. G., Durán, B. S. & Kökönyei, G. A. Person-Centered approach to adolescent nonsuicidal self-injury: Predictors and correlates in a community sample. J. Youth Adolesc. 51, 1760–1773. https://doi.org/10.1007/s10964-022-01628-y (2022).
Steinhoff, A. et al. Self-injury from early adolescence to early adulthood: Age-related course, recurrence, and services use in males and females from the community. Eur. Child. Adolesc. Psychiatry 30, 937–951. https://doi.org/10.1007/s00787-020-01573-w (2021).
Sawyer, S. M., Azzopardi, P. S., Wickremarathne, D. & Patton, G. C. The age of adolescence. Lancet Child. Adolesc. Health 2, 223–228. https://doi.org/10.1016/s2352-4642(18)30022-1 (2018).
Wu, B. et al. Potential mechanisms of non-suicidal self-injury (NSSI) in major depressive disorder: A systematic review. Gen. Psychiatr. 36, e100946. https://doi.org/10.1136/gpsych-2022-100946 (2023).
Kindler, J. et al. Increased immunological markers in female adolescents with non-suicidal self-injury. J. Affect. Disord. 318, 191–195. https://doi.org/10.1016/j.jad.2022.08.125 (2022).
Flach, E. et al. Hypothalamic-pituitary-thyroid axis function in female adolescent nonsuicidal self-injury and its association with comorbid borderline personality disorder and depression. Prog. Neuropsychopharmacol. Biol. Psychiatry 111, 110345. https://doi.org/10.1016/j.pnpbp.2021.110345 (2021).
Wang, Y. J. et al. Risk factors for non-suicidal self-injury (NSSI) in adolescents: A meta-analysis. EClinicalMedicine 46, 101350. https://doi.org/10.1016/j.eclinm.2022.101350 (2022).
Mannekote Thippaiah, S. et al. Non-suicidal self-injury in developing countries: A review. Int. J. Soc. Psychiatry 67, 472–482. https://doi.org/10.1177/0020764020943627 (2021).
Wolff, J. C. et al. Emotion dysregulation and non-suicidal self-injury: A systematic review and meta-analysis. Eur. Psychiatry. 59, 25–36. https://doi.org/10.1016/j.eurpsy.2019.03.004 (2019).
Faura-Garcia, J., Orue, I. & Calvete, E. Clinical assessment of non-suicidal self-injury: A systematic review of instruments. Clin. Psychol. Psychother. 28, 739–765. https://doi.org/10.1002/cpp.2537 (2021).
Martin, J. et al. Psychometric properties of the functions and addictive features scales of the Ottawa self-injury inventory: A preliminary investigation using a university sample. Psychol. Assess. 25, 1013–1018. https://doi.org/10.1037/a0032575 (2013).
Fox, K. R. et al. Self-Injurious thoughts and behaviors interview-revised: Development, reliability, and validity. Psychol. Assess. 32, 677–689. https://doi.org/10.1037/pas0000819 (2020).
Nixon, M. K., Levesque, C., Preyde, M., Vanderkooy, J. & Cloutier, P. F. The Ottawa self-injury inventory: Evaluation of an assessment measure of nonsuicidal self-injury in an inpatient sample of adolescents. Child. Adolesc. Psychiatry Mental Health 9, 26. https://doi.org/10.1186/s13034-015-0056-5 (2015).
Gratch, I. et al. Self-Injurious thoughts and behaviors Interview-Revised (SITBI-R): Reliability, validity, and inter-informant agreement in an adolescent sample. J. Clin. Child. Adolesc. Psychol. 51, 484–494. https://doi.org/10.1080/15374416.2021.1901229 (2022).
Gopal, D. P., Chetty, U., O’Donnell, P., Gajria, C. & Blackadder-Weinstein, J. Implicit bias in healthcare: Clinical practice, research and decision making. Future Healthc. J. 8, 40–48. https://doi.org/10.7861/fhj.2020-0233 (2021).
Collins, G. S. et al. TRIPOD + AI statement: Updated guidance for reporting clinical prediction models that use regression or machine learning methods. Bmj 385, e078378. https://doi.org/10.1136/bmj-2023-078378 (2024).
van Smeden, M. et al. Sample size for binary logistic prediction models: Beyond events per variable criteria. Stat. Methods Med. Res. 28, 2455–2474. https://doi.org/10.1177/0962280218784726 (2019).
Asarnow, J. R. et al. Suicide attempts and nonsuicidal self-injury in the treatment of resistant depression in adolescents: Findings from the TORDIA study. J. Am. Acad. Child. Adolesc. Psychiatry 50, 772–781. https://doi.org/10.1016/j.jaac.2011.04.003 (2011).
Yao, X. et al. Acceptability and psychometric properties of Brøset violence checklist in psychiatric care settings in China. J. Psychiatr Mental Health Nurs. 21, 848–855. https://doi.org/10.1111/jpm.12132 (2014).
Almvik, R. & Woods, P. Short-term risk prediction: the Brøset violence checklist. J. Psychiatr Ment Health Nurs. 10, 236–238. https://doi.org/10.1046/j.1365-2850.2003.00563.x (2003).
Zhao, H. et al. The machine learning model for distinguishing pathological subtypes of non-small cell lung cancer. Front. Oncol. 12, 875761. https://doi.org/10.3389/fonc.2022.875761 (2022).
Kursa, M. B. & Rudnicki, W. R. Feature selection with the Boruta package. J. Stat. Softw. 36, 1–13. https://doi.org/10.18637/jss.v036.i11 (2010).
Tibshirani, R. Regression shrinkage and selection via the Lasso. J. Roy. Stat. Soc.: Ser. B (Methodol.) 58, 267–288. https://doi.org/10.1111/j.2517-6161.1996.tb02080.x (1996).
Bose, G. et al. Early predictors of clinical and MRI outcomes using least absolute shrinkage and selection operator (LASSO) in multiple sclerosis. Ann. Neurol. 92, 87–96. https://doi.org/10.1002/ana.26370 (2022).
de Hond, A. A. H., Steyerberg, E. W. & van Calster, B. Interpreting area under the receiver operating characteristic curve. Lancet Digit. Health 4, e853–e855. https://doi.org/10.1016/s2589-7500(22)00188-1 (2022).
Vickers, A. J., Van Claster, B., Wynants, L. & Steyerberg, E. W. Decision curve analysis: Confidence intervals and hypothesis testing for net benefit. Diagn. Progn Res. 7, 11. https://doi.org/10.1186/s41512-023-00148-y (2023).
Chowdhury, M. Z. I. & Turin, T. C. Variable selection strategies and its importance in clinical prediction modelling. Fam Med. Community Health. 8, e000262. https://doi.org/10.1136/fmch-2019-000262 (2020).
Muehlenkamp, J. J., Xhunga, N. & Brausch, A. M. Self-injury age of onset: A risk factor for NSSI severity and suicidal behavior. Arch. Suicide Res. 23, 551–563. https://doi.org/10.1080/13811118.2018.1486252 (2019).
Olfson, M. et al. Suicide following deliberate self-harm. Am. J. Psychiatry. 174, 765–774. https://doi.org/10.1176/appi.ajp.2017.16111288 (2017).
Arthur, J. L., Danielle, N. & Steven, M. Nonsuicidal self injury among young adults and adolescents: Historical, cultural and clinical Understandings. Soc. Work Mental Health https://doi.org/10.1080/15332985.2023.2264434 (2023).
Xu, H. et al. Suicide attempts and non-suicidal self-injury in Chinese adolescents: Predictive models using a neural network model. Asian J. Psychiatry 97, 104088. https://doi.org/10.1016/j.ajp.2024.104088 (2024).
Austin, P. C. & Brunner, L. J. Inflation of the type I error rate when a continuous confounding variable is categorized in logistic regression analyses. Stat. Med. 23, 1159–1178. https://doi.org/10.1002/sim.1687 (2004).
Liang, S. et al. Development and validation of a prediction nomogram for non-suicidal self-injury in female patients with mood disorder. Front. Psychiatry. 14, 1130335. https://doi.org/10.3389/fpsyt.2023.1130335 (2023).
Van Calster, B. et al. Reporting and interpreting decision curve analysis: A guide for investigators. Eur. Urol. 74, 796–804. https://doi.org/10.1016/j.eururo.2018.08.038 (2018).
Chen, X. et al. Mediating effect of self-concealment between non-suicidal self-injury and internet addiction in college students: A cross-sectional study. BMC Psychol. 11, 406. https://doi.org/10.1186/s40359-023-01393-y (2023).
Burke, T. A., Ammerman, B. A., Hamilton, J. L., Stange, J. P. & Piccirillo, M. Nonsuicidal self-injury scar concealment from the self and others. J. Psychiatr. Res. 130, 313–320. https://doi.org/10.1016/j.jpsychires.2020.07.040 (2020).
Dillon, C. B. et al. Staff awareness of suicide and self-harm risk in healthcare settings: A mixed-methods systematic review. J. Affect. Disord. 276, 898–906. https://doi.org/10.1016/j.jad.2020.07.113 (2020).
Grimes, D. A. The nomogram epidemic: Resurgence of a medical relic. Ann. Intern. Med. 149, 273–275. https://doi.org/10.7326/0003-4819-149-4-200808190-00010 (2008).
Klimes-Dougan, B. et al. Hypothalamic-pituitary-adrenal axis dysregulation in depressed adolescents with non-suicidal self-injury. Psychoneuroendocrinology 102, 216–224. https://doi.org/10.1016/j.psyneuen.2018.11.004 (2019).
Collins, G. S. et al. Evaluation of clinical prediction models (part 1): From development to external validation. Bmj 384, e074819. https://doi.org/10.1136/bmj-2023-074819 (2024).
Author information
Authors and Affiliations
Contributions
Q.L. : conception and design of the study, analysis and interpretation of data, drafting the article. Y.R. : acquisition of data, drafting the article, editing the article. Y.H. : manuscript preparation. R.X. : acquisition of data. Z.D. : analysis and interpretation of data. Y.L. : acquisition of data. X.Z. : conception and design of the study, editing the article. Q.L. and Y.R. contributed equally to this work.All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, Q., Ren, Y., Huang, Y. et al. Development and validation of a probability-assessment nomogram for non-suicidal self-injury in hospitalized adolescents and young adults with mental disorders. Sci Rep 15, 15142 (2025). https://doi.org/10.1038/s41598-025-00142-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-00142-y