Abstract
This study aimed to investigate common complications during the chronic phase of spinal cord injury (SCI) and to assess bladder management methods and their associated complications in patients with neurogenic lower urinary tract dysfunction (NLUTD). A retrospective analysis was performed using clinical data from chronic-phase SCI patients across multiple centers in China. The study population included individuals diagnosed with SCI and admitted between January 1, 2017, and December 31, 2022. Chi-square tests were used to evaluate differences in the distribution of complications, disease duration, bladder management methods, and urinary complications. Univariate and multivariate analyses were conducted to identify risk factors for urinary complications. A total of 849 SCI patients from 28 provinces in China were included, showing significant demographic and clinical differences between traumatic SCI (TSCI) and non-traumatic SCI (NTSCI). Urinary tract infection (59.95%) and bowel-related complications, such as constipation (62.17%), were the most frequently reported complications. Additionally, the incidences of osteoporosis (38.50%), neuropathic pain (29.99%), bowel incontinence (12.06%), and hydronephrosis (11.91%) were also high. NLUTD was present in 90.58% of SCI patients. Among these, intermittent catheterization was associated with significantly lower rates of urological complications compared to indwelling catheterization (p = 0.025). Multivariate analysis identified bladder management method as a significant risk factor for urinary complications, with indwelling catheterization associated with a higher risk of urinary stones (p < 0.001) compared to intermittent catheterization. The high prevalence of bowel- and urological-related complications among Chinese SCI patients highlights the need for increased societal attention. In terms of bladder management, intermittent catheterization may provide greater benefits compared to indwelling catheterization. Further research and education are necessary to promote intermittent catheterization as a standardized bladder management approach for SCI patients.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is a serious condition caused by damage to the spinal cord due to either traumatic or non-traumatic causes1,2. Over the past three decades, the global prevalence of SCI has increased from 236 to 1,298 cases per million population3,4. The estimated global incidence of SCI is 0.9 million new cases annually, with approximately 6.2 million years of life lived with disability5. The total lifetime cost per patient exceeds $3 million6. In China, the incidence of SCI is 16.47 per 100,000 people, with a prevalence of 358.30 per 100,0007. From 1990 to 2019, the number of SCI patients in China rose by 138.32%, from 2.14 to 5.10 million. During the same period, incidence and prevalence increased by 89.91% and 98.20%, respectively, which were significantly higher than the global average8.
In most cases, current treatment options only provide temporary relief and are unable to fully prevent the long-term negative effects of SCI. The initial injury may lead to further damage over time, causing progressive health deterioration6,9. This progression increases the risk of various complications, including bladder and bowel dysfunction, sleep disorders, spasticity, pressure ulcers, sexual dysfunction, obesity, and vascular and respiratory diseases10,11. Several studies have reported urinary complications in Chinese SCI patients12,13,14. Two single-center studies found that the proportion of urinary tract infections (UTIs) among SCI patients was 12.53% and 26.3%, respectively12,14. Moreover, the prevalence of UTIs in Chinese SCI patients was higher than in patients from medically developed countries13. However, these studies did not examine the different methods of urination or their associations with urinary complications.
This study investigated the incidence of common complications in the chronic phase of SCI in China, with a particular focus on bladder management methods related to neurogenic lower urinary tract dysfunction (NLUTD) and the associated urinary complications.
Methods
Definition
The chronic phase of SCI refers to the stable period following injury, generally beginning after more than 6 months, when initial inflammation and tissue damage have subsided3,15,16.
Study design and population
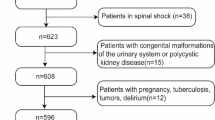
This multi-center retrospective study analyzed medical records from 11 healthcare institutions across China. Data were extracted from the electronic medical record and hospital information systems. The study followed the Declaration of Helsinki and was approved by the Ethics Committee of the China Rehabilitation Research Center (2023-014-02). Due to the retrospective, observational design and the anonymization of data, the requirement for informed consent was waived by the Ethics Committee of the China Rehabilitation Research Center (2023-014-01). Patients diagnosed with SCI and admitted between January 1, 2017, and December 31, 2022, were included. Patients with incomplete records or coexisting brain injuries were excluded. A flow chart of the study design is shown in Fig. 1. Data collection included demographic characteristics, causes of injury, physical examination findings, presence of complications, and lower urinary tract function. Each medical record was independently reviewed by two well-trained investigators. A double-entry verification process was implemented. All data were anonymized to maintain patient confidentiality.
The American Spinal Injury Association (ASIA) Impairment Scale (AIS) was used to assess SCI severity, classifying injuries from grade A to E17. The causes of SCI were categorized according to the International Spinal Cord Injury Core Data Set (version 2.0)18. Specifically, traumatic SCI (TSCI) included sports and leisure injuries, assault, transport accidents, falls, birth injuries, and other traumatic causes. Non-traumatic SCI (NTSCI) included congenital or genetic causes, degenerative non-traumatic conditions, benign or malignant tumors, vascular causes (e.g., ischemia, hemorrhage, arteriovenous malformation), infections (e.g., bacterial, viral), and other non-traumatic spinal cord dysfunctions. A UTI was diagnosed based on typical symptoms and laboratory evidence, including elevated urinary white blood cell counts and positive results from urine bacteriological examination19.
Statistical analysis
Patients were categorized into TSCI and NTSCI groups. Continuous variables are reported as means ± standard deviations, and categorical variables as frequencies (percentages). The chi-square test was used to compare categorical variables between the TSCI and NTSCI groups, while the t-test was used to compare continuous variables. Univariate and multivariate regression analyses were performed to identify risk factors associated with urinary complications. A two-tailed p-value < 0.05 was considered statistically significant.
Results
Demographic and clinical characteristics
A total of 849 patients were included in the study, recruited from 28 provinces across China (Supplement Table 1). The demographic characteristics of the patients are presented in Table 1. Significant differences in gender distribution were observed between traumatic spinal cord injury (TSCI) (male 79%, female 21%) and non-traumatic spinal cord injury (NTSCI) (male 57.03%, female 42.97%) (p < 0.001). Patients with TSCI had a lower mean age (44.26 years) than those with NTSCI (p = 0.012), as well as a shorter median disease duration (1.18 [0.72, 3.92] years vs. 2.36 [1.14, 6.52] years). Furthermore, the age at injury onset was significantly younger in TSCI compared to NTSCI (p = 0.035). The distribution of onset times in 3-year intervals showed an increasing trend in both groups (Fig. 2). The leading causes of TSCI included falls (33%), traffic-related injuries (24%), sports-related injuries (18%), other traumas (17%), and assaults (1%), whereas NTSCI was mainly caused by vascular conditions (24%), benign tumors (19%), infections (16%), and degenerative diseases (15%) (Fig. 3). Cervical injuries were more common and lumbar injuries less frequent in TSCI compared to NTSCI. The American Spinal Injury Association Impairment Scale (AIS) classifications differed significantly, with NTSCI most frequently categorized as grade D (53.5%) and TSCI as grade A (39.9%) (Table 1).
As shown in Table 2, the proportion of patients admitted for rehabilitation decreased from 58.05% at 5 years to 14.81% at 15 years. However, 42.59% of patients with a disease duration of 15 years still required treatment for neurogenic lower urinary tract dysfunction (NLUTD), indicating a persistent need for care.
Patients with TSCI had a significantly longer median hospitalization duration (29.00 days [14.00, 68.25], p < 0.001) and higher median costs (31,319 Chinese Yuan [12,578, 83,719], p = 0.003) compared to NTSCI. Among TSCI patients, a higher proportion (50.8%) paid out-of-pocket, whereas patients with NTSCI predominantly used employee medical insurance (40.3%) and resident medical insurance (29.3%). Exploratory descriptive statistics on hospitalization costs related to different reasons and complications are provided in Supplementary Table 2.
Incidences of complications of SCI in China
The characteristics of complications among Chinese patients with spinal cord injury (SCI) are summarized in Table 3. Urological and bowel-related complications were the most common. Significant differences in urological complications were observed between TSCI and NTSCI (p = 0.006). Urinary tract infections (UTIs) were the most frequent urological complication, affecting 62.5% of TSCI and 53.8% of NTSCI patients. Details of bacterial species associated with UTIs are listed in Supplementary Table 3. The prevalence of urinary stones was significantly lower in NTSCI than in TSCI (p = 0.015), while hydronephrosis was less common in TSCI compared to NTSCI (p = 0.049). Apart from urological complications, significant differences were also observed in pulmonary embolism (p = 0.031), deep vein thrombosis (p = 0.016), and orthostatic hypotension (p = 0.017) between TSCI and NTSCI.
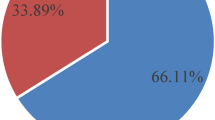
Bladder management characteristics and urinary complications in Chinese SCI patients with NLUTD
The study examined bladder management strategies used by Chinese SCI patients with NLUTD (Table 4), along with related complications and risk factors. Intermittent catheterization (42.6%) was the most frequently used method, followed by indwelling catheters (33.89%). Bladder management methods differed significantly between TSCI and NTSCI (p = 0.005), with TSCI patients mainly using intermittent catheterization (46.20%) and NTSCI patients more often using indwelling catheters (37.56%).
As shown in Table 5, patients paying out-of-pocket were more likely to choose intermittent catheterization, whereas those with health insurance, including employee and resident medical insurance, were more likely to use indwelling catheterization.
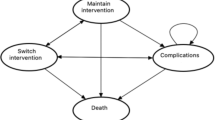
Table 6 presents the reasons for hospitalization according to bladder management in SCI patients with NLUTD. Patients using intermittent catheterization had significantly fewer urological-related hospitalizations (10/307) than those using indwelling catheters (18/239, p = 0.025). Urinary complications associated with different bladder management methods are summarized in Table 7. Intermittent catheterization was associated with a significantly lower overall risk of urinary complications compared to indwelling catheters (p = 0.025) (Fig. 4). Specific urinary complications were also analyzed by management method. Patients using indwelling catheters had a significantly higher prevalence of urinary stones compared to those using intermittent catheterization (p < 0.001). Similarly, the incidence of UTIs differed significantly across bladder management methods (p = 0.016); however, no statistically significant difference was observed between intermittent and indwelling catheterization (p = 0.083).
Risk factors associated with UTIs (Table 8) and urinary stones (Table 9) were further analyzed. Both indwelling and intermittent catheterization were identified as risk factors for UTIs when compared to normal voiding, with indwelling catheters posing a higher risk. For urinary stones, multivariate regression analysis showed no significant difference among indwelling catheterization, intermittent catheterization, or other bladder management methods compared to normal voiding. However, patients using indwelling catheters had a significantly higher risk of developing urinary stones compared to those using intermittent catheterization (p < 0.001). With regard to UTI, the severity of injury according to the AIS classification represents a risk factor in the univariate analysis, but no longer in the multivariate analysis.
Discussion
In recent years, there has been a growing global trend in the population of individuals with spinal cord injury (SCI)7,20,21. In this study, both traumatic SCI (TSCI) and non-traumatic SCI (NTSCI) showed increasing trends in onset time in recent years (Fig. 2). The demographic characteristics observed were consistent with findings from previous studies22,23,24,25. TSCI patients were predominantly male, while NTSCI showed a more balanced gender distribution. The average age at onset was younger in TSCI than in NTSCI. In terms of etiology, falls were the most common cause of TSCI in this cohort, followed by traffic accidents.
Several factors influence the distribution of age, gender, and etiology in TSCI. Prior research has shown that young men are more likely to experience injuries from traffic accidents and falls from height26. High falls account for a considerable proportion of SCI cases in China27. The rapid growth of the workforce in manufacturing and construction sectors over recent decades may be associated with a high incidence of fall-related injuries in younger individuals. This highlights the urgent need for improved workplace safety measures and personal protection to prevent such injuries. In addition, young men are more likely to engage in risky behaviors, which may contribute to this trend. The proportion of assault-related SCI in China was significantly lower than in other countries, likely due to strict national regulations on firearms and weapons28,29. In this study, traffic accidents were the second most frequent cause of TSCI. Given the widespread use of motor vehicles, traffic accidents continue to represent a major cause of TSCI globally.
Urological and bowel-related complications were the most frequently reported complications in this study. Among TSCI patients, urinary tract infection (UTI) was the most common, while constipation was most prevalent among NTSCI patients. Previous studies have also reported a high incidence of UTI and constipation following SCI30,31. Stillman et al. found that UTI (62%) was the most frequent complication within the first year after discharge from inpatient rehabilitation, with 33% of patients also reporting constipation31. Another single-center study reported a UTI incidence of 49.8%, with the duration of indwelling catheter use identified as a key risk factor30,31.
Neurogenic lower urinary tract dysfunction (NLUTD) is highly prevalent in individuals with SCI, with 70–84% experiencing upper or lower urinary tract complications32,33. The main goals of NLUTD management are to preserve upper urinary tract function by maintaining low intravesical pressure through effective bladder drainage and to ensure urinary continence34. Effective management of NLUTD is a critical component of SCI rehabilitation, as it significantly impacts overall morbidity35. Guidelines from the European Association of Urology Nurses (EAUN), European Association of Urology (EAU), and American Urological Association (AUA) recommend intermittent catheterization as the standard approach for patients unable to empty their bladder and strongly advise against the long-term use of indwelling catheters whenever possible36,37,38. Our study showed that 36.7% of patients use intermittent catheterization, there is still a gap compared to developed countries39. This discrepancy may be attributed to the relatively higher cost of intermittent catheterization and insufficient awareness among healthcare providers. Thus, intermittent catheterization still needs to be further popularized among SCI patients with NLUTD in China.
In this study, patients using intermittent catheterization had significantly lower rates of urological-related hospitalizations and complications compared to those using indwelling catheters. These findings were consistent with multivariate regression analysis results, which showed that intermittent catheterization was associated with a lower risk of UTIs and urinary stones compared to indwelling catheter use, aligning with international findings40,41,42,43. Crescenze et al. reported that patients using indwelling catheters had a higher rate of urological-related hospitalizations (26.3%) than those using intermittent catheterization (15.7%) over a one-year follow-up period40. Similarly, Weld et al. found that intermittent catheterization was linked to the lowest complication rates, including significantly reduced incidences of epididymitis, pyelonephritis, and bladder stones, compared to urethral indwelling catheters42. Krebs et al. showed that urethral indwelling catheters carried a higher risk of UTIs than intermittent catheterization, with long-term use being a key predictor of symptomatic UTIs in individuals with NLUTD. However, the incidence of UTI related to intermittent catheterization in China remains relatively high compared to previous studies. Another study from China also reported a high rate of UTIs in patients undergoing intermittent catheterization13. Possible contributing factors include catheter reuse, inadequate hand hygiene, and insufficient cleansing of the urethral meatus. Therefore, proper training and education are essential to ensure patients using intermittent catheterization adopt correct techniques and adhere to standardized procedures.
This study represents the first comprehensive, multicenter retrospective analysis in China examining bladder management and associated complications of NLUTD in both TSCI and NTSCI during the chronic phase. However, several limitations must be acknowledged. As a hospital-based study, the findings may not be generalizable to the broader population. The retrospective design may also introduce recall bias. Despite the heterogeneity of etiologies in NTSCI, subgroup analysis was not conducted due to limited data. Additionally, the sample size remains relatively small, highlighting the need for larger, population-based studies in the future.
Conclusion
The high prevalence of urological and bowel-related complications among Chinese SCI patients requires greater societal attention. In bladder management, intermittent catheterization may offer more benefits than indwelling catheterization. Further research and guidance are necessary to promote standardized intermittent catheterization as the primary bladder management strategy among SCI patients.
Data availability
The dataset used and analyzed during the current study is available from the corresponding author upon reasonable request.
References
New, P. W., Cripps, R. A. & Bonne Lee, B. Global maps of non-traumatic spinal cord injury epidemiology: towards a living data repository. Spinal Cord. 52 (2), 97–109 (2014).
Lee, B. B., Cripps, R. A., Fitzharris, M. & Wing, P. C. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord. 52 (2), 110–116 (2014).
Khorasanizadeh, M. et al. Neurological recovery following traumatic spinal cord injury: a systematic review and meta-analysis. J. Neurosurg. Spine. 30 (5), 683–699 (2019).
Anjum, A. et al. Spinal cord injury: pathophysiology, multimolecular interactions, and underlying recovery mechanisms. Int. J. Mol. Sci. 21 (20), 7533 (2020).
Safdarian, M. et al. Global, regional, and National burden of spinal cord injury, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. 22 (11), 1026–1047 (2023).
Vismara, I., Papa, S., Rossi, F., Forloni, G. & Veglianese, P. Current options for cell therapy in spinal cord injury. Trends Mol. Med. 23 (9), 831–849 (2017).
Liu, C. et al. Incidence, prevalence, and causes of spinal injuries in China, 1990–2019: findings from the global burden of disease study 2019. Chin. Med. J. (Engl). 137 (6), 704–710 (2024).
Guan, B., Anderson, D. B., Chen, L., Feng, S. & Zhou, H. Global, regional and National burden of traumatic brain injury and spinal cord injury, 1990–2019: a systematic analysis for the global burden of disease study 2019. BMJ Open. 13 (10), e075049 (2023).
He, W., Li, Z. Q., Gu, H. Y., Pan, Q. L. & Lin, F. X. Targeted therapy of spinal cord injury: Inhibition of apoptosis is a promising therapeutic strategy. Mol. Neurobiol. 61 (7), 4222–4239 (2024).
Ditunno John, F. and S. Formal Christopher, chronic spinal cord injury. N. Engl. J. Med. 330 (8), 550–556.
Cristante, A. F., Barros Filho, T. E., Marcon, R. M., Letaif, O. B. & Rocha, I. D. Therapeutic approaches for spinal cord injury. Clinics 67 (10), 1219–1224 (2012).
Wang, Z. M. et al. Epidemiological characteristics of spinal cord injury in Northwest China: a single hospital-based study. J. Orthop. Surg, Res. 15 (1), 214 (2020).
Liu, J., Luo, C., Xiao, W. & Xu, T. Urinary tract infections and intermittent catheterization among patients with spinal cord injury in Chinese community. Sci. Rep. 13 (1), 17683 (2023).
Yang, R. et al. Epidemiological characteristics of traumatic spinal cord injury in Guangdong, China. Spine 42 (9), E555–E561 (2017).
Ahuja, C. S. et al. Traumatic spinal cord injury-repair and regeneration. Neurosurgery 80 (3s), S9–S22 (2017).
Richard-Denis, A., Chatta, R., Thompson, C. & Mac-Thiong, J. M. Patterns and predictors of functional recovery from the subacute to the chronic phase following a traumatic spinal cord injury: a prospective study. Spinal Cord. 58 (1), 43–52 (2020).
Rupp, R. et al. International standards for neurological classification of spinal cord injury: revised 2019. Top. Spinal Cord Inj Rehabil. 27 (2), 1–22 (2021).
Biering-Sørensen, F. et al. International spinal cord injury core data set (version 2.0)-including standardization of reporting. Spinal Cord. 55 (8), 759–764 (2017).
Fitzpatrick, M. A. & Nwafo, N. Urinary tract infection diagnostic and management considerations in people with spinal cord injury and neurogenic bladder. Infect. Dis. Clin. N Am. 38 (2), 381–393 (2024).
Global & national burden of spinal cord injury. 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. 22 (11), 1026–1047 (2023).
Qin, H. et al. Analysis and comparison of the trends in burden of spinal cord injury in China and worldwide from 1990 to 2021: an analysis of the global burden of disease study 2021. Front. Public. Health. 12, 1517871 (2024).
Barbiellini Amidei, C., Salmaso, L., Bellio, S. & Saia, M. Epidemiology of traumatic spinal cord injury: a large population-based study. Spinal Cord. 60 (9), 812–819 (2022).
Shang, S. et al. Sex-related differences in epidemiology, treatment, and economic burden of traumatic spinal cord injury in China (2013–2018). Spine 48 (17), e288–e301 (2023).
Sun, J. et al. Traumatic spinal injury-related hospitalizations in the united States, 2016–2019: a retrospective study. Int. J. Surg. 109 (12), 3827–3835 (2023).
Gupta, A., Taly, A. B., Srivastava, A. & Murali, T. Non-traumatic spinal cord lesions: epidemiology, complications, neurological and functional outcome of rehabilitation. Spinal Cord. 47 (4), 307–311 (2009).
Wang, H. et al. Epidemiology of traumatic spinal fractures: experience from medical university-affiliated hospitals in Chongqing, China, 2001–2010. J. Neurosurg. Spine. 17 (5), 459–468 (2012).
Feng, H. Y., Ning, G. Z., Feng, S. Q., Yu, T. Q. & Zhou, H. X. Epidemiological profile of 239 traumatic spinal cord injury cases over a period of 12 years in Tianjin, China. J. Spinal Cord Med. 34 (4), 388–394 (2011).
Eli, I., Lerner, D. P. & Ghogawala, Z. Acute traumatic spinal cord injury. Neurol. Clin. 39 (2), 471–488 (2021).
Sherrod, B. A. et al. Epidemiology of gunshot-related spinal injuries and related risk factors for in-hospital mortality in the united States from 2015–2019: A National trauma data bank analysis. J. Neurotrauma. 41 (9–10), 1112–1121 (2024).
Liu, J., Hao, X., Shang, X., Chi, R. & Xu, T. Incidence and risk factors of urinary tract infection in hospitalized patients with spinal cord injury in a hospital of China. Sci. Rep. 14 (1), 3579 (2024).
Haisma, J. A. et al. Complications following spinal cord injury: occurrence and risk factors in a longitudinal study during and after inpatient rehabilitation. J. Rehabil Med. 39 (5), 393–398 (2007).
Dorsher, P. T. & McIntosh, P. M. Neurogenic bladder. Adv. Urol. 2012, 816274 (2012).
Manack, A. et al. Epidemiology and healthcare utilization of neurogenic bladder patients in a US claims database. Neurourol. Urodyn. 30 (3), 395–401 (2011).
Jeong, S. J., Cho, S. Y. & Oh, S. J. Spinal cord/brain injury and the neurogenic bladder. Urol. Clin. N Am. 37 (4), 537–546 (2010).
Ku, J. H. The management of neurogenic bladder and quality of life in spinal cord injury. BJU Int. 98 (4), 739–745 (2006).
Blok, B. et al. EAU Guidelines Neuro-urology 601 (European Association of Urology, 2024).
Blok, B. et al. Neuro-urology, Nononcology Guidelines. https://uroweb.org/guideline/neuro-urology (European Association of Urology, 2020).
Ginsberg, D. A. et al. The AUA/SUFU guideline on adult neurogenic lower urinary tract dysfunction: diagnosis and EVALUATION. J. Urol. 206 (5), 1097–1105 (2021).
Hagen, E. M. & Rekand, T. Management of bladder dysfunction and satisfaction of life after spinal cord injury in Norway. J. Spinal Cord Med. 37 (3), 310–316 (2014).
Crescenze, I. M. et al. Self-reported urological hospitalizations or emergency room visits in a contemporary spinal cord injury cohort. J. Urol. 205 (2), 477–482 (2021).
Dedeić-Ljubović, A. & Hukić, M. Catheter-related urinary tract infection in patients suffering from spinal cord injuries. Bosn J. Basic. Med. Sci. 9 (1), 2–9 (2009).
Weld, K. J. & Dmochowski, R. R. Effect of bladder management on urological complications in spinal cord injured patients. J. Urol. 163 (3), 768–772 (2000).
Krebs, J., Wöllner, J. & Pannek, J. Risk factors for symptomatic urinary tract infections in individuals with chronic neurogenic lower urinary tract dysfunction. Spinal Cord. 54 (9), 682–686 (2016).
Acknowledgements
This study was supported by National Key Research and Development Program of China (2023YFC3606003), the Cooperative Project of China Rehabilitation Research Center (2021HZ-08) and the Beijing Natural Science Foundation (7222235).
Author information
Authors and Affiliations
Contributions
X.L., L.L. and H.S. designed the protocol and prepared the main manuscript text. H.S., H.D., Y.L., Z.H. and G.L. prepared Tables 4, 5, 6 and 7 and supplement tables. S.H., D.H., Y.L., Z.H., G.L., Z.C., X.H. and G.C.prepared figures. S.H., D.H., Y.L., Z.H., G.L., Z.C., X.H., G.C., Y.L., H.H., J.T., L.P., T.L., D.L., M.Z. and H.C collected data and prepared Tables 1, 2 and 3. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The funding source Cooperative Project of China Rehabilitation Research Center (2021HZ-08) was funded by Coloplast. All authors declare that they have no other competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sun, H., Deng, H., Liu, Y. et al. Research on complications and bladder management of the chronic phase spinal cord injury in China. Sci Rep 15, 15718 (2025). https://doi.org/10.1038/s41598-025-00621-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-00621-2