Abstract
This study aimed to estimate the net monetary benefit (NMB) of trifocal intraocular lenses (IOL) versus monofocal IOL in South Korea according to patient age. A hybrid model with a short-term decision tree, followed by a lifetime Markov model, was developed. The study considered patients aged 45–75 years old. Probabilities of visual disturbances and wearing glass were obtained from a clinical trial of trifocal IOL (NCT03280108). The analysis considered medical and glass costs. Utility values for each age were adopted from previous studies. The incremental QALY was mapped to the patient’s willingness to pay (WTP) thresholds of gross domestic product per capita (GDP; $32,310), $23,000, and $15,000 per QALY gain to estimate the NMB. Trifocal IOL incurred higher costs but resulted in increased QALYs in all age groups. Under the WTP of $15,000, the NMB ranged from $694 at 75 to $6,880 at 45. The NMB with GDP was from $6,731 at 75 to $19,590 at 45. Using trifocal IOL can enhance the quality of life compared to no presbyopia correction with monofocal IOL in patients who want to correct presbyopia. Younger patients have greater economic benefits. Thus, trifocal IOLs are a worthy treatment option considering age and WTP.
Similar content being viewed by others
Introduction
The occurrence of cataracts increases every ten years of life, starting at 40 years of age, with a prevalence of over 90% in people aged over 65 years in South Korea1,2,3. Accordingly, intraocular lenses (IOLs) have undergone significant advancements4,5. Compared to conventional monofocal IOLs, presbyopia-correcting multifocal IOLs are designed to enhance visual acuity at intermediate and near distances, in addition to far distances1,6. They significantly reduce spectacle dependency following cataract surgery, thereby improving health-related and vision-related quality of life6,7,8.
In most countries, presbyopia-correcting IOLs are not commonly covered by the healthcare systems4,6,7,9,10. This lack of coverage often leads to persistent uncorrected presbyopia and subsequently reduced quality of life4,7. Thus, many patients undergoing cataract surgery wonder whether it is a good choice to pay out of pocket to receive presbyopia-correcting IOLs, even at high costs, instead of monofocal IOLs. Therefore, there is a need to provide information about the clinical and monetary benefits of IOLs to patients6.
The AcrySof IQ PanOptix (model TFNT00; Alcon) was the first trifocal IOL approved by the US Food and Drug Administration (FDA) in 20191,11 and is one of the most widely used presbyopia-correcting multifocal IOLs. Several studies have demonstrated the higher clinical effectiveness of the AcrySof IQ PanOptix IOL, showing better vision at all distances with a high level of patient satisfaction compared to the monofocal IOL1,10,11. However, few studies have compared the cost-effectiveness or cost-benefits of multifocal IOLs versus monofocal IOLs6,7,10,12,13. In particular, only one has compared the cost-benefits of PanOptix and monofocal IOL in the United States4.
This study aimed to provide a detailed cost-benefit analysis of trifocal IOL compared to monofocal IOLs in South Korea according to age.
Results
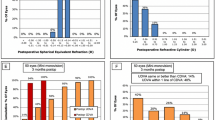
As a result of the cost-benefit analysis, the NMB with WTP of 1 GDP ($32,310), $23,000, and $15,000 for varying ages (45–75 years) were demonstrated in Fig. 1 and Table S2. As the starting age increases and WTP decreases, NMB decreases. The maximum and minimum NMB for patients willing to pay for trifocal IOL were $19,590, and $694, respectively. In all cases, from 45 to 75 years of age, trifocal IOL incurred higher costs but resulted in increased QALYs (Table S2). Furthermore, as the starting age decreased, the differences in costs per patient between the two groups decreased, and the differences in QALYs increased, indicating better outcomes in the younger age group (Tables 1 and 2).
The cost-benefit analysis model also revealed that IOL treatments, when implanted with trifocal IOL, increased costs by $4,274 from patients’ perspective compared to monofocal IOL (Table 3). Although using trifocal IOL incurs higher expenses for the IOL procedure and YAG laser capsulotomy, the costs of IOL explantation and glasses were lower. The main difference in costs between the two IOLs was attributed to the IOL procedure, which amounted to $4,842, followed by an additional $631 for glasses. The undiscounted life years were the same for both IOLs, while QALYs increased by 0.60 with the trifocal IOL.
The results of the scenario analyses are presented in Table 4. The most significant difference in the NMB emerged from the scenario analysis with hours wearing glasses compared with the base-case analysis. When hours wearing glasses were reduced to 40% of the base case (reduction rate of 60%, 7 h), the NMB with a WTP of 15,000 was -$688, making it unaffordable for patients to pay more. Moreover, among all scenario analysis results, the NMB was the highest, with $16,610, $11,028, and $6,231 for WTP of one GDP, $23,000, and $15,000, respectively. These values corresponded to a 30% discount price for the trifocal IOL.
Figure 2 shows the results of the probabilistic simulation, illustrating that the QALYs for patients who underwent cataract surgery with monofocal IOLs were more sensitive to the input parameters than those with trifocal IOLs. The mean costs and QALYs of the trifocal IOL were $4,290 and 0.60, respectively, which were higher than those of the monofocal IOL, based on the results of 1,000 simulations (Table S3). This confirms the robustness of the findings from the CBA, as they demonstrate results similar to those of the base-case analysis in Table 3.
Discussion
This study conducted a cost-benefit analysis of bilateral cataract surgery involving the implantation of trifocal versus monofocal IOL in South Korea. A hybrid model that merges a decision tree of one year with a lifetime Markov model provides estimates of the costs and QALY related to two different IOLs. The analysis factors in both immediate post-operative results and long-term health states. Trifocal IOLs showed more QALY gains than monofocal IOLs, although they paid more from the patients’ perspectives. At a WTP of $15,000, NMB for ages 50, 60, and 70 were $6,138, $4,324, and $2,014, respectively. NMB decreases with age.
Our study conducted a cost-benefit analysis based on increasing age, as the quality of life after cataract surgery is dependent on age. This approach offers a comprehensive economic evaluation, emphasizing the value of trifocal IOL across a broad age range. This provides a detailed analysis of the cost-benefits of trifocal IOL in South Korea. Older individuals typically exhibit lower QALYs because of factors such as reduced life expectancy, increased chronic health conditions, cognitive decline, and social changes, all of which contribute to a diminished quality of life14,15. This study showed that as the starting age decreased, the NMB increased, particularly at higher WTP thresholds, as a result of lower QALYs at older age, which is supported by the results of previous studies. Hu et al. showed that the cost-effectiveness of multifocal IOLs decreased with patient age6. Similarly, a scenario analysis of a US study revealed higher NMB in younger patients4. This indicates that younger patients are likely to have greater economic and quality-of-life-related value from choosing a trifocal IOL instead of a monofocal IOL, although the initial costs are higher. This is an important insight, as it suggests that trifocal IOL can be advantageous for younger patients, providing them with better visual outcomes and potentially reducing the need for glasses. It also supports a broader, long-term perspective on IOL selection, emphasizing both clinical and economic value, and may help guide shared decision-making between patients and clinicians.
Moreover, we performed a scenario analysis and probabilistic simulation to validate the robustness of the findings. Scenario analysis was conducted to understand the effects of various input settings on the model results. We specifically considered the variations in the time spent wearing glasses that made the most significant difference in NMB compared with the base-case analysis. When people use glasses 60% less than the base case (or for 7 h), the NMB with a WTP of $15,000 becomes -$688, making it unaffordable for patients to cover any additional charges. Furthermore, in all the scenario analyses conducted, the highest NMB was $16,610, $11,028, and $6,231 according to the WTP thresholds when the price of the PanOptix IOL was cut by 30%. In other words, lowering the price means a lower amount of out-of-pocket money for patients; from patients’ perspective, it is a benefit.
Berdahl et al. performed a cost-benefit analysis to compare multifocal and monofocal IOLs using Markov models and a decision tree model from the patient perspective in the United States4. They showed that bilateral PanOptix IOL provide an improved vision-related quality of life (QALY gain of 0.67) at an incremental cost $2,783 compared to monofocal IOL. However, in the base-case analysis of this study in South Korea, there was a difference in cost of $4,274 and a QALY gain of 0.60 for patients with PanOptix IOL compared to those with monofocal IOL. Although it was difficult to compare the differences in costs, which varied by country, the differences in the QALYs were similar. It is difficult to compare the results reported by Hu et al. with our results because they analyzed the bifocal IOL, while we studied a trifocal IOL6. Nevertheless, Hu et al. revealed that multifocal IOLs are a cost-effective strategy compared to monofocal IOLs, with an ICER of $4,805, which can be lower than WTP of $50,0006. This indicates that patients can have a better quality of life. This is consistent with the QALY gains observed in this study.
Our study had several limitations. First, we applied disutility to patients wearing glasses who experienced visual disturbances and underwent IOL explantation, drawing from the literature16,17,18. The application of disutility values for patients in the short-term period of 1-year still carries some uncertainty. Nonetheless, previous studies have also conducted cost-effectiveness and cost-benefit analyses of trifocal versus monofocal intraocular lenses and similarly adopted QALY loss in these patients4,6. Second, we assumed that spectacle-dependent patients wore glasses for 17.5 h a day, covering the entire daytime, except for the time spent sleeping. As the duration of wearing glasses can vary among individual patients, the assumption of 17.5 h may overestimate the time spent wearing glasses. Therefore, we presented scenario analyses for the hours of wearing glasses, considering reductions of 20%, 40%, and 60% from the base case. Third, while visual disturbances were considered for a lifetime in the models from previous studies4,6, the model in our study included visual disturbances in the short-term model, which was limited to one year. Although visual disturbances can occur after one year from the cataract surgery, we have confirmed that the symptoms occurring after this period will not have a significant impact on the patient’s quality of life based on clinical advisory. Fourth, the efficacy inputs used in the model were based on global patients, comprising only 5% Asians, and may exhibit some differences from Koreans19. We used efficacy data from global patients for base-case analysis because the efficacy results for Korean patients were based on a small sample size20. However, we included these results for the key efficacy parameters (overall spectacle dependence, probability of IOL explantation, and average YAG use per patient) in the scenario analyses. Additionally, our model did not take into account the potential variability in postoperative refractive outcomes, which could affect the accuracy of QALY and NMB estimates. In clinical practice, only 73.7% of eyes achieving a prediction error within ± 0.5 diopters21,22,23. This variation is largely attributed to measurement errors in axial length and anterior chamber depth, as well as to inaccuracies in estimating the effective lens position, which depends on the IOL power calculation formula. As these factors were not considered in our analysis, the projected benefits of trifocal IOLs may have been overestimated24,25.
We conducted a cost-benefit analysis comparing trifocal and monofocal IOLs in the context of bilateral cataract surgery in South Korea. Despite being more expensive, trifocal IOLs have been found to provide greater QALYs, particularly among younger patients, who showed higher NMB values compared to older patients. By correcting presbyopia, trifocal IOLs can offer improved visual outcomes and a higher quality of life than monofocal IOLs. As such, trifocal IOLs are a valuable treatment option for younger patients willing to bear the out-of-pocket expenses for cataract surgery. Given the increasing demand for visual performance and independence in modern life—especially among working-age individuals—our findings highlight the clinical relevance of trifocal IOLs in improving both functional vision and overall patient satisfaction. These insights can support personalized surgical planning and patient-centered decision-making.
Method
The population of interest comprised patients with cataracts who were willing to pay for multifocal IOLs to correct presbyopia. To elicit net monetary benefit (NMB), we modeled the costs and effectiveness of trifocal IOL (Acrysoft IQ Panoptix, TFNT00, Alcon) and monofocal IOL (AcrySof IQ monofocal, SN60AT, Alcon) based on a clinical trial (ClinicalTrials.gov Identifier: NCT03280108)1,26. The model was developed from the patient’s perspective. However, we included out-of-pocket costs and the medical costs of payers in the analysis. The mean age at baseline in this model was 59 years, which was analyzed using the Korean multifocal registry, constructed using data from 13 institutions in Korea. We estimated the cost and QALY by age groups in increments of 5 years from 45 to 75 years. The proportion of males, calculated as 39% from the Korean registry, was applied to the mortality rate of patients, which varied according to sex. A discount rate of 3.5% was applied to the costs and QALYs.
This study was performed at the Samsung Medical Center (SMC) and Sungkyunkwan University according to the tenets of the Declaration of Helsinki, and approved of by the institutional review board of SMC (SMC 2023-01-125). This study is a cost-benefit analysis based on publicly available data and did not involve any human participants or the use of human tissue. Therefore, ethical approval and informed consent were not required and were waived accordingly.
Model structure
We developed a hybrid model with a short-term decision tree of a 1-year time horizon, followed by a lifetime Markov model, to evaluate the cost-benefit of IOL treatments when implanted with a trifocal IOL versus a monofocal IOL in a South Korean setting (Fig. 3). To reflect the key influences on patients in the year following cataract surgery, a combined model of short- and long-term modules was constructed. The short-term module captures the costs and outcomes associated with the symptoms of patients who experience visual disturbances, demonstrating moderate to very extremely bothersome glare/haloes/starbursts after cataract surgery. During this period, patients with and without visual disturbances can be divided into different states based on whether they depend on spectacles, including reading, distancing, and bifocal or progressive glasses.
Survivors from the short-term module entered the lifetime model, which was based on plausible health states: well (patients with complete spectacle independence and absence of visual disturbances), spectacle-dependent (patients requiring reading, distance, bifocal, or progressive glasses), and death. Patients with and without glasses in the short-term module entered the glass and well states, respectively, in the lifetime model. In this model, death is considered an absorbing state of health. The rates of lens explantation and yttrium aluminum garnet (YAG) capsulotomy procedures were also included as post-surgery events in the model. In our model, while the rate of YAG procedures only affected costs, the rate of lens explantation affected costs and patients’ quality of life. Patients were analyzed for a lifetime horizon limited to 100 years of age or death, whichever occurred first.
Several key assumptions were required for the model. As visual disturbances are not considered in the lifetime module, it is assumed that all patients—both spectacle-independent and spectacle-dependent—resolved the glare/halos/starbursts after the first yearly cycle post-surgery. The mortality rate was assumed to be the same across all health states for the trifocal and monofocal IOL arms in the model. Patients who wore glasses were assumed to do so throughout their lifetime.
The input parameters used in the base-case analysis are listed in Table 1. In the short-term module, the proportion of patients experiencing moderate to very extremely bothersome visual disturbances was 12% and 7.2% in patients with trifocal and monofocal IOL, respectively26. The overall spectacle dependence rates for trifocal and monofocal IOLs were 19.5% and 91.8%, respectively1. The distribution of spectacle dependence type (reading, distance, bifocal, or progressive glasses) after trifocal and monofocal IOL implantation was derived from internal data (Table S1). The proportions of patients who underwent IOL explantation after trifocal and monofocal IOL implantation in one year were 0.78% and 0.88%, respectively1,27.
In the long-term module, patients in health states of the well or glasses remain in these states or transition to death. The probability of death was adopted based on the 2021 Complete Life Table from the Korean Statistical Information Service27 and applied to the proportion of surviving patients in each health state in each cycle.
Cost
The cost of cataract surgery with a monofocal IOL per unilateral eye was analyzed from the national health claims data of one million patients in 2020 by the Health Insurance Review & Assessment Service (HIRA). In 2020, 14,385 cataract surgeries were performed, with a mean cost of $838. Moreover, we estimated the cost of cataract surgery with trifocal IOL per unilateral eye with the costs of IOLs. The cost of trifocal and monofocal IOLs was based on the HIRA public announcement for non-reimbursed medical expenses in 202228 and the report for national healthcare reimbursed medical expenses from HIRA29, respectively. As the claims data we utilized for estimating the cost of cataract surgery pertained only to cases involving monofocal IOLs, which are reimbursed in Korea, we assessed the cost of cataract surgery with trifocal IOLs by deducting the cost of a monofocal IOL and then adding the cost of trifocal IOL to the baseline monofocal cataract surgery expense. In the case of exchanging IOL, patients undergo surgery once more and incur costs equivalent to those of the initial cataract surgery, as assumed. Furthermore, patients whose vision becomes cloudy again after cataract surgery may require a laser surgery known as YAG laser capsulotomy. The cost of YAG laser capsulotomy was estimated from HIRA healthcare big data by dividing the total cost ($87,103) by the number of patients (252,372) after cataract surgery in 20224. This was reflected in the average use of the YAG laser per patient after trifocal and monofocal IOL implantation, which was 24.81% and 6.14%, respectively. Based on the cost of glasses and the frequency of replacing glasses obtained from interviews with Korean opticians, the annual cost of glasses per type (reading, distance, bifocal, or progressive) was calculated (Table S1). The distribution of glasses normalized to 100% was applied to each type of glass19. All costs were converted based on an average currency of 2023 (1,308 KRW = 1 USD).
Utility
In this model, in the well-health state, patients do not have spectacle dependence or visual disturbances after cataract surgery. The utility value of a healthy state depends on the patient’s age group. The utilities for the 40–49, 50–59, 60–69, and over 70 years age groups were 0.975, 0.967, 0.938, and 0.890, respectively30. Therefore, the utility in the base case was 0.967, reflecting the mean age of the patients included in the model (59). Furthermore, baseline utility varied in the analyses depending on the starting age.
Disutility associated with adverse events of bothersome visual disturbances (glare/haloes/starbursts, -0.18), wearing glasses (-0.065), and undergoing a lens explantation procedure (-0.150) were previously reported by Brown et al.16, Dobrez and Calhoun18, and Busbee et al.17, respectively, and were used in this analysis. Patients were assumed to experience bothersome visual disturbances (glare/haloes/starbursts) for an estimated 4 h per day (60.9 days in a calendar year)31. To estimate the utility of patients wearing glasses, it was assumed that they use them for 17.5 h a day, subtracting the average sleeping time in Korea based on the Korean Statistical Information Service32.
Net monetary benefit
The NMB patients could expect from trifocal IOL implantation was calculated as the incremental QALY benefit multiplied by the patient’s willingness-to-pay (WTP) per QALY gain minus incremental costs. We considered multiple WTP thresholds, including the Gross domestic product (GDP) of South Korea, as there is no universally accepted WTP for cataract surgery in South Korea. According to the Korea Health Insurance Review and Assessment, a national agency for drug reimbursement decision-making in South Korea, the accepted incremental cost-effectiveness ratio for general medicines ranged from $4,144 to $22,118, with a median of $13,127 between 2014 and 2021. We considered 3 WTP, as assumed: GDP, $23,000 per capita, and $15,000 per capita. GDP per person in Korea was $32,310 in 2023. As the starting age affected the outcomes, we calculated the NMB using three WTP values for the age range of 45–75 years.
Sensitivity analysis
Scenario and probabilistic sensitivity analyses were conducted to understand the effect of uncertainty on the model input parameters. An analysis was performed with four scenarios for parameters that contain uncertainties. Efficacy, including overall spectacle dependence, probability of IOL explantation, and average YAG use per Korean patient, was included as a parameter for scenario analyses. Further, the discounted prices of trifocal IOL were considered, taking into account potential variations among institutions. Finally, under the strong assumption that the patients wore glasses for the entire day, except during sleep, analyses with reduced hours of wearing glasses were performed. The input values used in the scenario analyses are listed in Table 2.
A probabilistic sensitivity analysis with 1,000 simulations was performed to examine the effect of uncertainty around all model inputs simultaneously. The principal parameters included efficacy, utility, and cost, which were input parameters in the base-case analysis. Different values were drawn for each input parameter via random sampling based on different distributions to reflect the attributes of each parameter. Beta and Dirichlet distributions were used as efficacy inputs, log-normal distributions for cost inputs and duration of visual disturbance, and normal distributions for utility inputs.
Data availability
All relevant data are within the paper and its supplementary files.
Abbreviations
- IOL:
-
Intraocular lens
- NMB:
-
Net monetary benefit
- WTP:
-
Willingness to pay
- GDP:
-
Gross domestic product
- YAG:
-
Yttrium aluminum garnet
- HIRA:
-
Health Insurance Review & Assessment Service
- SMC:
-
Samsung Medical Center
References
Modi, S. et al. Visual and patient-reported outcomes of a diffractive trifocal intraocular lens compared with those of a monofocal intraocular lens. Ophthalmology 128(2), 197–207 (2021).
Rim, T. H. T., Kim, M., Kim, W. C., Kim, T-I. & Kim, E. K. Cataract subtype risk factors identified from the Korea National health and nutrition examination survey 2008–2010. BMC Ophthalmol. 14(1), 1–15 (2014).
Korea disease control and prevention agency. The 5th Korea National Health and Nutrition Examination survey 2010–2012. (2013).
Berdahl, J., Bala, C., Dhariwal, M., Rathi, H. & Gupta, R. Cost-benefit analysis of a trifocal intraocular lens versus a monofocal intraocular lens from the patient’s perspective in the united States. Plos One 17(11), e0277093 (2022).
Davis, G. The evolution of cataract surgery. Mo. Med. 113(1), 58 (2016).
Hu, J. Q., Sarkar, R., Sella, R., Murphy, J. D. & Afshari, N. A. Cost-effectiveness analysis of multifocal intraocular lenses compared to monofocal intraocular lenses in cataract surgery. Am. J. Ophthalmol. 208, 305–312 (2019).
Maxwell, W. A., Waycaster, C. R., D’Souza, A. O., Meissner, B. L. & Hileman, K. A united States cost–benefit comparison of an apodized, diffractive, presbyopia-correcting, multifocal intraocular lens and a conventional monofocal lens. J. Cataract Refractive Surg. 34(11), 1855–1861 (2008).
Rampersad, N. & Zitha, A. J. Impact of cataract surgery on vision-related quality of life. Afr. Vis. Eye Health 79(1), 1–12 (2020).
Berdahl, J. et al. Patient and economic burden of presbyopia: a systematic literature review. Clin. Ophthalmol. :3439–3450. (2020).
Lan, Q. et al. Cost-effectiveness of presbyopia correction among seven strategies of bilateral cataract surgery based on a prospective single-blind two-center trial in China. Ophthalmol. Therapy. 11(6), 2067–2082 (2022).
Food, U. S. & Administration, D. ALI. AcrySof® IQ PanOptix® Trifocal Intraocu lar Lens (Model TFNT00) and AcrySof® IQ PanOptix® Toric Trifocal Intraocular Lens (2019). Models TFNT30, TFNT40, TFNT50, TFNT60).
Lin, J. C. & Yang, M. C. Cost-effectiveness comparison between monofocal and multifocal intraocular lens implantation for cataract patients in Taiwan. Clin. Ther. 36(10), 1422–1430 (2014).
Greenbaum, S. Cost–benefit analysis of multifocal IOLs versus monovision pseudophakia. J. Cataract Refractive Surg. 35(4), 614 (2019).
Kocot, E., Kotarba, P. & Dubas-Jakóbczyk, K. The application of the QALY measure in the assessment of the effects of health interventions on an older population: A systematic scoping review. Archives Public. Health 79, 1–12 (2021).
McPhail, S. M. Multimorbidity in chronic disease: impact on health care resources and costs. Risk management and healthcare policy. 143 – 56. (2016).
Brown, M. M., Brown, G. C., Brown, H. C., Peet, J. & Roth, Z. Value-based medicine, comparative effectiveness, and cost-effectiveness analysis of topical cyclosporine for the treatment of dry eye syndrome. Arch. Ophthalmol. 127(2), 146–152 (2009).
Busbee, B. G., Brown, M. M., Brown, G. C. & Sharma, S. Cost-utility analysis of cataract surgery in the second eye. Ophthalmology 110(12), 2310–2317 (2003).
Dobrez, D. G. & Calhoun, E. A. Testing subject comprehension of utility questionnaires. Qual. Life Res. 13, 369–376 (2004).
Alcon. Data on File. Clinical Study Report TDOC—0055352. (2018).
Kim, T., Chung, T-Y., Kim, M. J., Lee, K. & Hyon, J. Y. Visual outcomes and safety after bilateral implantation of a trifocal presbyopia correcting intraocular lens in a Korean population: A prospective single-arm study. BMC Ophthalmol. 20(1), 1–11 (2020).
Stopyra, W. Analysis of accuracy of twelve intraocular lens power calculation formulas for eyes with axial myopia. Taiwan. J. Ophthalmol. 13(2), 225–230 (2023).
Nemeth, G. & Modis, L. Jr. Accuracy of the hill radial basis function method and the Barrett universal II formula. Eur. J. Ophthalmol. 31, 566–571 (2021).
Stopyra, W., Voytsekhivskyy, O. & Grzybowski, A. Accuracy of 20 intraocular Lens power calculation formulas in medium-long eyes. Ophthalmol. Ther. 13(7), 1893–1907 (2024).
Stopyra, W., The exactness of intraocular lens power calculation formulas for short eyes & and correlation between method accuracy and eyeball axial length. Ceska a Slovenska oftalmologie: Casopis Ceske oftalmologicke Spolecnosti a Slovenske. Oftalmologicke Spolecnosti 78(5), 236–240 (2022).
Stopyra, W. Analysis of accuracy of twelve intraocular lens power calculation formulas for eyes with axial hyperopia. Saudi J. Ophthalmol. 37(2), 125–130 (2023).
Alcon Research Ltd. Directions for Use: AcrySof® IQ PanOptix® Trifocal IOL (Model TFNT00). (2019).
2021 Complete life table [Internet]. [cited 31 December 2023]. (2021). Available from: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B42
Service, H. I. R. A. Announcement for non-reimbursed medical expenses 2022 [Available from: https://www.hira.or.kr/npay/index.do#app%2Frb%2FnpayDamtInfoList
Service, H. I. R. A. National health insurance reimbursed medical expenses. (2023).
Korea national health statistics [Internet]. [cited 31 December 2023]. (2020). Available from: https://gsis.kwdi.re.kr/statHtml/statHtml.do?orgId=338&tblId=DT_LCD_F002
Jin, G. J., Crandall, A. S. & Jones, J. J. Changing indications for and improving outcomes of intraocular lens exchange. Am. J. Ophthalmol. 140(4), 688 (2005). e1-. e9.
Regional statistics [Internet]. 2017 [cited 31 December 2023]. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=800&tblId=DT_800003N_A039&conn_path=I
Acknowledgements
We thank Chulsoon Kim for support in conducting this study. We would like to thank Editage (www.editage.co.kr) for English language editing.
Funding
This study was funded by Alcon Korea Ltd., Seoul, South Korea, the wholesaler of AcrySof IQ PanOptix and AcrySof SN60AT IOLs. No authors received remuneration for writing this manuscript.
Author information
Authors and Affiliations
Contributions
S-H.K. and D.H.L. conceived the concept for this study. S.M. and Y.K.W. wrote the initial draft of the manuscript. S.M. and S-H.K. were involved in model development, data curation, methodology, and visualization. All authors were involved in interpretation of data for the work. All authors were involved in critical revision of the manuscript. S.M. and S-H.K. performed the statistical analysis. S-H.K. and D.H.L. supervised the study as corresponding author.
Corresponding authors
Ethics declarations
Competing interests
This study was sponsored by Alcon Korea Ltd., Seoul, South Korea. (https://www.alcon.com/). Chulsoon Kim is an employee of Alcon Korea Ltd. (the study sponsor). The authors report no other conflicts of interest related to this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Min, S., Won, Y.K., Kwon, SH. et al. Cost-benefit analysis of a trifocal intraocular lens versus a monofocal intraocular lens in South Korea. Sci Rep 15, 17330 (2025). https://doi.org/10.1038/s41598-025-00712-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-00712-0