Abstract
Recent studies have revealed that oral, gut, and intratumoral microbial dysbiosis significantly affects tumor progression, therapy resistance, and prognosis in cholangiocarcinoma (CCA) and pancreatic ductal adenocarcinoma (PDAC) patients. However, the biliary microbiome, which directly interacts with malignant tissues, remains poorly understood. In this study, we analyzed the bile microbiota from 17 CCA, 15 PDAC, and 40 choledocholithiasis (CDL) patients using bacterial 16 S rRNA and fungal ITS sequencing. Principal coordinate analysis revealed significant differences in microbial communities between the cancer and CDL groups. The microbial community structure in each group demonstrated a specific pattern. Linear discriminant analysis revealed Streptococcus, Sphingomonas, and Bacillus enrichment in CCA patients, Neisseria, Sphingomonas, and Caulobacter in PDAC patients were more prevalent compared with CDL patients. Caulobacter was more prevalent, wheares Campylobacter was less in PDAC patients than in CCA patients. Fungal DNA was detected in ~ 50% of the samples, with CCA and PDAC patients. KEGG pathway analysis revealed altered metabolic pathways, including peptidoglycan, sphingolipid, and fatty acid metabolism and bile acid metabolism, in CCA and PDAC patients. These findings highlight the potential role of the biliary microbiome in CCA and PDAC pathogenesis, offering new insights into disease mechanisms and biomarkers.
Similar content being viewed by others
Introduction
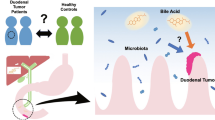
Study into the roles of microorganisms, particularly the gut microbiota, microbial communities, and localized microbiomes, in malignant diseases has emerged as a highly active area of research. Recent studies have elucidated the associations between the oral and intestinal microbiota and cholangiocarcinoma (CCA) and pancreatic duct adenocarcinoma (PDAC), which are highly lethal diseases1,2,3,4,5. A multinational study analyzing fecal and saliva samples from patients with PDAC using shotgun metagenomics revealed significant alterations in the gut and oral microbiota, suggesting the presence of a global gut microbiota signature in PDAC patients4. Microbial dysbiosis is thought to play a critical role in PDAC carcinogenesis, therapeutic resistance, and prognosis6,7. Similarly, in cholangiocarcinoma (CCA) patients, specific gut bacterial species have been identified and reported to be associated with distinct clinical features2,8. These findings underscore the importance of microbial dysbiosis in the pathophysiology of both PDAC and CCA.
Although this is still an emerging field of research, the literature describes several direct and indirect mechanisms modulating the increase and decrease in numbers of specific microorganisms associated with inflammatory responses, regulation of the immune system-microbiome-tumor axis, impacts on metabolism, and alterations to the tumor microenvironment leading to epithelial cell transformation and DNA damage, which have cancer-promoting effects9,10,11. However, since intestinal bacteria do not directly contact biliary and pancreatic tissues, the main mechanisms by which they exert influence remain an ongoing area of investigation. Furthermore, recent advances have revealed the presence of unique microbiomes within tumor tissues, which were previously considered sterile. Technological progress and a deeper understanding of tumor microenvironments have shown that the intratumoral microbiome plays a critical role in various aspects of PDAC and CCA, including tumor progression, diagnosis, treatment response, chemotherapeutic resistance, and immune modulation12,13,14,15,16. In parallel, recent studies have characterized fungal communities within various cancers, highlighting their distribution, interactions with immune cells, and prognostic potential17,18. For example, pathogenic fungi have been identified as predominant fungal genera infiltrating PDAC tumors in both mice and humans, emphasizing the importance of the mycobiome alongside the bacterial microbiome19.
These findings raise critical questions about the mechanisms by which bacteria establish themselves in CCA and PDAC tissues. While intratumoral bacteria have been hypothesized to originate from the gut microbiota, possible routes of translocation include the biliary and pancreatic ducts as well as hematogenous and lymphatic pathways1,12,20,21,22. Other reports demonstrated that pancreatic bacterial DNA profiles were similar to those in the duodenal tissues of the same patients, regardless of disease state, suggesting that bacteria may migrate from the gut into the pancreas15,23,22,24. Furthermore, pancreatic fluid frequently refluxes into the biliary tract (pancreatobiliary reflux); conversely, biliopancreatic reflux can occur in patients with pancreatobiliary maljunction25, suggesting that the bacterial flora in biliary and pancreatic fluids are closely related and are strongly influenced by the intestinal flora.
We assume that analysis of the biliary microbiome is useful for estimating carcinogenetic and physiopathological status. In fact, previous studies have demonstrated that the biliary microbial communities differ significantly between patients with gallbladder polyps and gallstones, suggesting a possible association with underlying pathologies20,26,27. However, the biliary microbiomes in patients with malignant diseases, especially PDAC, have not been well characterized. Therefore, we investigated the biliary microbiomes and mycobiomes of patients with choledocholithiasis (CDL), CCA and PDAC to elucidate the impact of microorganisms related to these diseases. We found significant evidence that the biliary microbiome may influence pathophysiology in patients with these diseases.
Results
Clinical patient characteristics
Table 1 summarizes the clinical characteristics of the study subjects. The mean ages were 77.1 years for the CDL group, 77.5 years for the CCA group, and 77.7 years for the PDAC group, and no statistically significant differences were observed. Blood test results revealed no significant differences among the three groups for T-bilirubin (CDL: 5.4 mg/dL, CCA: 5.6 mg/dL, PDAC: 5.5 mg/dL), AST (CDL: 227.1 IU/L, CCA: 221.2 IU/L, PDAC: 220.2 IU/L), or ALT (CDL: 236.8 IU/L, CCA: 229.5 IU/L, PDAC: 226.8 IU/L) levels. Similarly, inflammatory markers, such as CRP levels (CDL: 8.35 mg/dL, CCA: 7.92 mg/dL) and WBC counts (CDL: 117.5 × 10²/µL, CCA: 110.3 × 10²/µL, PDAC: 107.5 × 10²/µL), did not differ significantly between the groups.
DNA was successfully extracted from 1 mL bile in all groups, with average yields of 2.4 ng/µL for the CDL group, 3.2 ng/µL for the CCA group, and 0.3 ng/µL for the PDAC group. Compared with the CDL and CCA groups, the PDAC group presented significantly lower DNA yields (p < 0.01).
Sequencing data and bacterial alpha and beta diversities
The 16 S ribosomal RNA genes of the bacterial communities were amplified via PCR, and next-generation sequencing was employed to perform a detailed analysis of the bacterial flora. The mean number of sequence reads was 53,265 (5,017–65,334) among all the samples. Alpha and beta diversity analyses were conducted using QIIME2. Regarding alpha diversity, the Chao1 index was utilized to assess the richness and diversity of bacterial communities in bile samples across the three groups. No statistically significant differences in the Chao1 values were observed among the groups (Fig. 1). Similarly, the Shannon and Simpson indices showed no significant variation, indicating comparable microbial abundance across the groups.
Beta diversity was examined using principal coordinate analysis (PCoA) to evaluate differences in microbial community composition between groups. Bray‒Curtis analysis revealed significant clustering differences between the CCA and CDL groups (distance:0.90, p < 0.01) and between the PDAC and CDL groups (distance:0.90, p < 0.05), indicating distinct microbial profiles (Fig. 2). While no statistically significant differences were observed between the CCA and PDAC groups, there was a trend toward differentiation (distance:0.96, p = 0.072). Similar findings were obtained via Jaccard distance metrics.
Analysis of microbial community structures
We analyzed the bacterial composition in the bile samples at the class and order levels across the groups (Fig. 3). At the class level, Gammaproteobacteria and Bacilli were predominant in all groups, collectively accounting for more than 60% of the microbial composition. At the order level, most Gammaproteobacteria were classified as Enterobacteriales, while the majority of Bacilli were identified as Lactobacillales.
Bacterial classes identified in bile samples from the CDL, CCA and PDAC groups. (a) Level and order (b) level classification. Each bar indicates the percentage contribution of the class-level and order-level profiles. Gates and classes represented in different colors are indicated at the bottom of the figure.
Comparative analysis of the bacterial flora revealed significant group-specific differences. Compared with the CDL group, the CCA group presented a lower abundance of Clostridia and a greater abundance of Bacilli (P < 0.05). Compared with those in the CDL group, Gammaproteobacteria and Clostridia were less abundant in the PDAC group, whereas Alphaproteobacteria were more abundant (P < 0.05). No statistically significant differences were observed at the class level between the CCA and PDAC groups.
At the order level, the CCA group presented reduced levels of Clostridiales and increased levels of Bacillales and Fusobacteriales compared with the CDL group (P < 0.05). In contrast, the PDAC group had lower levels of Clostridiales and higher levels of Caulobacterales and Bacteroidales than did the CDL group (P < 0.05). Additionally, the CCA group presented a lower abundance of Caulobacterales than did the PDAC group (P < 0.05).
Linear discriminant analysis of the Microbiome
Given the observed variations in microbial proportions across taxonomic levels, linear discriminant analysis (LDA) was performed using the linear discriminant analysis effect size (LEfSe) approach, which can determine the taxonomic units most likely to explain differences between groups by coupling standards tests for statistical significance with additional tests encoding biological consistency and effect relevance. The LDA scores, represented on a logarithmic scale along the horizontal axis, indicate the magnitude of differences in the relative abundance of microbial features between groups (LDA score > 3.5, P < 0.05).
First, LDA was conducted for the CCA and CDL groups (Fig. 4). The analysis revealed that Streptococcus, Sphingomonas, and Bacillus had higher LDA scores in the CCA group than in the CDL group at the genus level, whereas Clostridium had a lower LDA score in the CCA group compared to the CDL group.
(a) LefSe comparison of bacterial classification between the CCA and CDL groups. Histograms of LDA scores for the significantly more abundant bacterial groups are shown, with the CCA group in red and the CDL in green. Each analysis was performed at the genus level, but when the genus was not determined, the next hierarchy was used. (b) Relative abundance of Streptococcus in each sample. (c) Relative abundance of Clostridiales in each sample.
Next, we compared the LDA scores of the PDAC and CDL groups (Fig. 5). In the PDAC group, Alphaproteobacteria displayed a higher LDA score at the class level, and Neisseria, Sphingomonas, and Caulobacter had higher LDA scores at the genus level compared to the CDL group. Conversely, Gammaproteobacteria presented a relatively low LDA score at the class level, and Klebsiella, Escherichia, and Clostridium presented relatively low LDA scores at the genus level.
(a) LefSe comparison of bacterial classification between the PDAC and CDL groups. Histograms of LDA scores for the significantly more abundant bacterial groups are shown, with the PDAC group in red and the CDL in green. Each analysis was performed at the genus level, but when the genus was not determined, the next hierarchy was used. (b) Relative abundance of Alphaproteobacteria in each sample. (c) Relative abundance of Clostridium in each sample.
Finally, LDA was performed to compare the PDAC and CCA groups (Fig. 6). In the PDAC group, Caulobacter had a higher LDA score than in the CCA group, whereas Campylobacter had a higher LDA score in the CCA group than in the PDAC group.
(a) LefSe comparison of bacterial classification between the CCA and PDAC groups. Histograms of LDA scores for the significantly more abundant bacterial groups are shown, with the CCA group in red and the PDAC group in green. Each analysis was performed at the genus level, but when the genus was not determined, the next hierarchy was used. (b) Relative abundance of Caulobacterales in each sample. (c) Relative abundance of Campylobacter in each sample.
Analysis of the fungal mycobiome
To further investigate microbial dynamics, we analyzed the composition of the fungal mycobiome across groups. Fungal DNA was detected in 33 of the 72 patients (45.8%), with the following distributions: 45% in the CDL group, 41.1% in the CCA group, and 53.3% in the PDAC group. For cases in which fungi were detected, the fungal compositions were analyzed. Figure 7a presents a stacked bar chart of fungal abundance at the class level, showing no statistically significant differences between the groups. Agaricomycetes emerged as the predominant fungal class across all the groups. Notably, the CCA and PDAC groups presented a trend toward lower proportions of Agaricomycetes and higher proportions of Saccharomycetes than did the CDL group. Additionally, Malasseziomycetes accounted for approximately 10% of the fungal composition in the CCA group, with the majority identified as Malassezia species.
Classes of fungi identified in bile samples from the CDL, CCA and PDAC groups. (a) Classification of levels. Each bar shows the percentage contribution of the gate-level and class-level profiles. The classes represented by different colors are indicated at the bottom of the figure. (b) The bacterial composition in the presence or absence of fungi in cancer cases is also shown.
Given these characteristic fungal variations, we explored the bacterial compositions in patients with and without detected fungi to assess potential symbiotic relationships between fungi and bacteria in cancer patients (Fig. 7b). However, no significant associations were detected between the presence or absence of fungi and the bacterial flora composition. Furthermore, we analyzed the correlations between bacterial and fungal species at various taxonomic levels; however, no significant results were obtained.
Predictive metagenomic analysis using PICRUSt2
To elucidate the functional gene profiles of the intestinal microbiota, we performed predictive metagenomic analysis using PICRUSt2. The EC database was utilized for functional annotation. Comparative analysis revealed 38 enzymes with significant differences (P < 0.05) in expression between the CCA and CDL groups, 48 differentially expressed enzymes between the PDAC and CDL groups (P < 0.05), and 14 differentially expressed enzymes between the PDAC and CCA groups (P < 0.05).
In the PDAC group, several enzymes, including those related to fucose metabolism, L-arginine pathways, cobalamin biosynthesis, gallate metabolism, and pyruvate fermentation, were notably less abundant than those in the CDL and CCA groups. Conversely, in comparisons between the PDAC and CCA groups, enzymes associated with hexuronide and glucuronide metabolism were expressed at significantly higher levels (Supplementary Figures S1, S2, S3).
Owing to the substantial number of enzyme-level changes detected, we mapped these expression variations to KEGG pathways and conducted pathway analysis. Relative pathway expression was compared across groups, as illustrated in Fig. 8. Compared with the CDL group, the PDAC group presented pronounced alterations in the activation of specific pathways, with fold changes observed in peptidoglycan biosynthesis (1.28), sphingolipid metabolism (3.06), N-glycan biosynthesis (4.29), fatty acid metabolism (1.54), and secondary bile acid biosynthesis (1.30). In contrast, the CCA group presented more modest pathway activation changes than did the PDAC group, with fold changes observed in peptidoglycan biosynthesis (1.24), sphingolipid metabolism (0.67), N-glycan biosynthesis (1.29), fatty acid metabolism (1.21), and secondary bile acid biosynthesis (1.21).
Schematic of the KEGG pathway, with fold change (FC) calculated for the CCA and PDAC groups, respectively, on the basis of the amount of enzyme in the CDL group. Light blue represents a slightly significant difference in the CCA group, blue represents a highly significant difference in the CCA group, and red represents a highly significant difference in the PDAC group, with larger circles indicating greater gene numbers.
Discussion
In the present study, we detected substantial amounts of bacterial DNA in bile samples from all patients, including patients who exhibited minimal signs of inflammation. This finding suggests the possibility of a consistent microbial community within the biliary tract. In support of this hypothesis, previous research utilizing 16 S rRNA sequencing identified a rich bacterial flora in the bile of healthy individuals and patients with gallbladder polyps22,26,28.
To further investigate this phenomenon, we compared the biliary microbiota among the DHL, CCA, and PDAC groups. Although no significant differences in alpha diversity were detected across these groups, beta diversity analysis revealed distinct bacterial community structures between the DHL and malignant groups, indicating disease-associated shifts in microbial colonization patterns. In terms of bacterial composition, Proteobacteria and Firmicutes were the predominant phyla across all bile samples, accounting for a majority of the detected bacteria. At the order level, Enterobacteriales and Lactobacillaleswere particularly abundant, similar to findings in prior studies29,30,31. Frequently reported genera in bile include Enterococcus, Streptococcus, Bacteroides, Klebsiella, Clostridium, Fusobacterium, and Pyramidobacter, with Proteobacteriaconsistently identified as the dominant phylum, aligning with our results29.
Focusing on disease-specific differences, our analysis revealed a greater prevalence of Bacilli and a lower abundance of Clostridia in CCA bile samples than in CDL bile samples. Multiple studies have presented the biliary microbiomes in patients with extrahepatic cholangiocarcinoma, revealing elevated abundances of genera such as Bacteroides, Geobacillus, Meiothermus, and Anoxybacilluscompared with those in patients with choledocholithiasis30,29,32,33. Additionally, prior research has highlighted reductions in Firmicutes abundance and increases in that of Bacteroidesin the biliary microbiota of CCA patients relative to controls29. Interestingly, in our study, the relative abundance of Bacteroides remained consistently low across all groups, suggesting potential variations driven by patient demographics, disease states, or methodological differences.
Our analysis revealed a greater prevalence of Bacilli and a lower abundance of Clostridia in the PDAC group than in both the CDL and CCA groups. Furthermore, the PDAC group presented a significantly greater presence of Alphaproteobacteria than did the PDAC and CCA groups. While studies focusing on the biliary microbiota of PDAC patients are limited, some prior investigations have provided valuable insight. For example, Li et al.. identified Pseudomonas, Chloroplast, and Acinetobacteras potential PDAC-associated taxa in bile samples32. Similarly, using gene sequencing, Maekawa et al.. revealed Enterobacter and Enterococcus (members of Lactobacillales) as predominant microorganisms in bile from PDAC patients, indicating findings that align closely with our results34.
To further investigate these microbial differences, we conducted LEfSe analysis. Compared with the CDL group, the CCA group presented significantly greater LDA values for Bacilli at the class level and Streptococcus at the genus level, whereas at the class level Clostridiapresented lower LDA scores in the CCA patients. Previous studies examining the biliary microbiota in CCA patients have identified a wide range of dominant bacterial genera, but no consistent conclusions have been reached30,31,32,33,35. Saab et al.. reported that Enterococcus, Streptococcus, Bacteroides, Klebsiella, and Pyramidobacterwere the most abundant genera in the biliary microbiota of CCA patients29. Additionally, Song et al.. demonstrated that the biliary microbial composition in gallbladder cancer (GBC) and CCC patients differed markedly, suggesting that species such as Peptostreptococcus stomatis and Enterococcus faeciummay play a role in GBC progression36. These findings, combined with our results, highlight the potential importance of the Bacilli class in the progression of biliary and pancreatic carcinomas. The variations in microbial communities between disease states suggest that specific bacterial taxa may contribute to the pathogenesis and progression of these malignancies.
Conversely, the PDAC group had significantly higher LDA scores for Alphaproteobacteria at the class level and Caulobacter at the genus level, whereas they had lower LDA scores for Gammaproteobacteria at the class level and Klebsiella and Escherichia at the genus level. A previous study of 187 pancreatic cancer (PC) patients demonstrated increased abundance of Proteobacteria in PC samples, with an increased abundance of Gammaproteobacteriaspecifically observed in PDAC tissues compared with those of the CDL group37. This subset of Proteobacteriahas been suggested to increase gemcitabine metabolism, potentially contributing to chemotherapeutic resistance15. Furthermore, the abundance of Proteobacteriahas been shown to be greater in PDAC patients than in those with other cancers, including those with breast cancer, glioblastoma, lung cancer, colorectal cancer and melanoma38. These findings highlight a potential role for Proteobacteria in carcinogenesis and prognosis via their influence as intratumoral microbes. Our study also revealed significant shifts in the proportions of Proteobacteria in the bile of PDAC patients, suggesting that these bacteria may influence the processes of carcinogenesis, disease progression and prognosis through modulation of the intratumoral microbiome. These findings highlight the need for further investigation into the interplay between the biliary microbiota and intratumoral bacterial populations.
In the comparison between PDCA and CCA patients, Caulobacter was more prevalent in PDCA patients, whereas Campylobacter showed particularly high LDA scores in CCA patients. Caulobacterhas previously been reported to be significantly associated with gallbladder cancer39. Additionally, Campylobacter jejuniis known to produce cytolethal distending toxin (CDT), with some studies suggesting an association with gastrointestinal cancers40,41. Although the mechanism underlying the observed differences in these bacterial populations within CCA and PDCA patient bile remains unclear, this finding presents an intriguing area for further investigation.
Conversely, research regarding fungal communities in bile remains rare. Recent studies have characterized fungi in patients with various cancers, with associations between the presence of Candida, Saccharomyces, and Malasseziaand specific cancers. These findings indicate that fungi may affect host immunity and cancer progression, highlighting the role of the mycobiome in cancer biology17,18. In particular, Malasseziaabundance has shown notable increases in both murine models and human pancreatic cancer patients, and antifungal drugs have been shown to protect against tumor progression in a mouse model of PDCA19. Additionally, solitary biliary candidiasis is a common comorbidity in patients with malignant biliary obstruction and is associated with poor prognosis in patients with advanced cholangiocarcinoma42. Our study revealed that fungi were present in approximately half of the samples, with no difference among the groups; however, Saccharomycetes tended to be more common in CCC and PDCA patients than in those with AC, and Malasseziomycetes was detected in CCC patients. Saccharomyceteshas been implicated in the progression of various cancers17. Notably, GFP-labeled Saccharomyces cerevisiaeadministered orally to mice migrated to the pancreas within 30 min, suggesting that the gut mycobiome may directly affect the pancreatic microenvironment19. Clinically, fungal and bacterial species have been shown to interact with and potentially modulate pathophysiological states43. However, in our study, no significant changes in the bacterial microbiota were observed in the presence or absence of fungi. This area warrants further investigation to better understand the implications of fungal–bacterial dynamics for disease modification.
Finally, we performed metabolic function prediction of the microbiota using PICRUSt2 to clarify the functional enzyme spectrum in each group. We revealed the differential expression of several genes related to carcinomas, such as those involved in pyruvate fermentation44, gallate45, fucoses46, and glucuronide47, in each group. These results support the idea that biliary microbial dysbiosis is responsible for pathological conditions. To clarify the metabolic pathways associated with the predicted enriched genes, we subsequently conducted KEGG pathway analysis. This revealed an enrichment of genes associated with bile acid- and glycan-related pathways in the bile of pancreatic cancer patients. Bile acids are known to directly activate signaling pathways involved in carcinogenesis, such as the FXR pathway, and have significant associations with cancer initiation and progression through direct mechanisms48. In fact, previous studies have documented associations between bile acid levels and pathological states in both pancreatic and biliary tract cancers49,50,51. Additionally, N-glycans are significantly altered in cancerous tissue types, and glycan moieties have been shown to participate in essential oncogenic processes, including cell signaling, proliferation, cell death, invasion, angiogenesis, and metastasis52,53. Such differences in KEGG pathways are thought to potentially influence the processes underlying disease pathogenesis.
This study has several limitations. First, owing to ethical and technical concerns, we could not examine the characteristics of the biliary microbiomes of healthy individuals. To circumvent contamination of the intestinal environment during ERCP collection, we could not rule out the presence of duodenal-derived bacteria in the collection fluid. In addition, since we did not stratify the patients according to the degree of inflammation, we could not exclude the influence of the underlying conditions. Furthermore, we were unable to verify whether the bile duct lumen bacteria were similar to those adhered to tumor tissue. Finally, we were unable to determine whether the biliary microbiota is a cause or a consequence of carcinogenesis. Future research exploring the relationships between bacteria in bile and those within tumors will be critically important.
In conclusion, increasing evidence suggests that microorganisms may influence the incidence, onset, and progression of diseases such as CCA and PDAC. However, the specific underlying pathogenesis, persistent inflammation, regulation of the immune‒microbe‒tumor axis, metabolic impact, and alterations in the tumor microenvironment and intratumor microbiome remain insufficiently understood, highlighting the need for a closer examination of the role of the biliary microbiome. Further research into the biliary and tumor microbiomes is increasingly essential to elucidate these complex interactions and establish preventive and therapeutic strategies for CCA and PDAC patients.
Methods
Human subjects
We focused on the associations between bacteria and fungi in bile and pancreatic cancer tissues and examined the differences in bacterial and fungal flora in the bile of cholangitis, cholangiocarcinoma, and pancreatic carcinoma patients. There were 17 cholangiocarcinoma (CCA) patients, 15 pancreatic carcinoma (PDAC) patients, and 72 controls (40 of which has choledocholithiasis [CDL]), who underwent endoscopic retrograde cholangiopancreatography (ERCP) for obstructive jaundice at the Mie Prefectural General Medical Center, Yokkaichi, Japan. This study was conducted according to the guidelines of the Helsinki Declaration and approved by the Ethics Committee of the Mie Prefectural General Medical Center, Yokkaichi, Japan. Informed consent was obtained from all participants or their legal guardians.
DNA extraction and illumina library generation
Bile was obtained from patients with obstructive jaundice through endoscopic retrograde cholangiopancreatography, which was performed by experienced doctors in a dedicated operating room. Bile was collected using a new sterile catheter into a sterile bottle during the sampling process and stored at −20 °C until analysis. DNA extraction from the samples was conducted via a MORA-EXTRACT Kit (Kyokuto Pharmaceutical Industrial Co., Ltd., Japan) according to the manufacturer’s instructions.
Next-generation sequencing (NGS) analysis of the microbial community structures in the feces was performed using a MiSeq (Illumina, San Diego, CA). PCR amplification was performed with the primers 1ST-341 F (5′- ACACTCTTTCCCTACACGACGCTCTTCCGATCT-NNNNN-CCTACGGGNGGCWGCAG-3′) and 1ST-805R (5′- GTGACTGGAGTTCAGACGTGTGCTCTTCCGATCT-NNNNN-GACTACHVGGGTATCTAATCC-3′), followed by the primers 2ndF (5’- AATGATACGGCGACCACCGAGATCTACAC-Index2-ACACTCTTTCCCTACACGACGC-3’) and 2ndR (5’- CAAGCAGAAGACGGCATACGAGAT-Index1-GTGACTGGAGTTCAGACGTGTG-3’), which targeted the V3-V4 hypervariable region of the 16 S rRNA gene.
Quality filtering and amplicon sequencing analysis
Paired-end sequencing reads were merged via the fastq-join program using the default settings. Only combined reads that had a quality value score of > 20 for more than 99% of the sequences were extracted via the FASTX-Toolkit. Chimeric sequences were deleted using USEARCH ver.6.1. The joined amplicon sequence reads were processed through the QIIME 2 ver. 2020.6. A quality value score of < 33 and chimeric sequences were filtered, and the representative sequences were created using the DADA2 denoise-single plugin ver. 2017.6.0. The taxonomy of representative sequences was assigned using the Greengenes database ver. 13.8 by training a naïve Bayes classifier via the q2-feature-classifier plugin.
Alpha and beta diversity analysis
Alpha diversity indices (Chao1, Shannon and Simpson indices) were calculated via the alpha rarefaction plugin. The statistical significance of the Chao1, Shannon and Simpson indices among the groups was assessed using the Kruskal‒Wallis test via the alpha-group-significance plugin.
Beta diversity was analyzed using Jacaard and Bray‒Curtis distances using a core-metric-phylogenetic plugin (Qiime2). The Emperor tool was used to visualize the PCoA plots. The statistical significance of the similarity of bacterial communities among groups was assessed with an ANOSIM test using the beta-group significance plugin.
Linear discriminant analysis (LDA)
Comparisons of the relative abundances of taxa between locations and sample types were assessed using the linear discriminant analysis effect size (LEfSe). LEfSe uses a nonparametric Kruskal‒Wallis rank‒sum test to identify taxa with significantly different normalized relative abundances and performs an LDA to determine the effect size of each taxon. The taxa with an LDA result greater than 2 (with a p value < 0.05) were considered significant.
ITS sequencing
We analyzed the fungal microbiome by sequencing internal transcribed spacer 1 (ITS1). The ITS1 regions were amplified using the primers ITS1-F_KYO1 (5′- ACACTCTTTCCCTACACGACGCTCTTCCGATCT- NNNNN-CTHGGTCATTTAGAGGAASTAA-3′), ITS2_KYO2 (5′- GTGACTGGAGTTCAGACGTGTGCTCTTCCGATCT- NNNNN-TTYRCTRCGTTCTTCATC − 3′), 2ndF (5’- AATGATACGGCGACCACCGAGATCTACAC-Index2-ACACTCTTTCCCTACACGACGC-3’) and 2ndR (5’- CAAGCAGAAGACGGCATACGAGAT-Index1-GTGACTGGAGTTCAGACGTGTG-3’) and the dual index method. Libraries were paired-end sequenced on a 2 × 300-bp platform using a MiSeq system together with the MiSeq Reagent Kit version 3. The representative sequences were similarly created via the DADA2 denoise-single plugin. Taxonomy assignment of the resulting representative sequences was compared with the UNITE (ver. 9.0) reference database using the q2-feature-classifier plugin. We determined samples as negative for fungi in which no fungal DNA detection by ITS Next Gen Seq.
Predictive functionality analysis
Predictive functionality analysis of the bacterial 16 S rDNA communities was performed using PICRUSt2 (ver. 2.4.1). The representative sequences analyzed by QIIME2 and the reference sequence of the Integrated Microbial Genomes database (IMG) were aligned using HMMER ver. 3.3. The phylogenetic placement analyses were performed via EPA-NG ver. 0.3.3 and GAPPA ver. 0.6.0. The 16 S RNA gene copies were normalized using the caster package of R software. The gene families were predicted on the basis of the MetaCyc database. The data were compared by two-sided Welch’s t–test. Analysis was performed using STAMP (ver. 2.1.3).
KEGG pathway analysis
The KEGG orthologs predicted using PICRUSt2 were assigned to each pathway using the KEGG API. KEGG pathway analysis revealed related differentially expressed genes54,55. The advanced bubble chart shows the enrichment of differentially expressed genes in signaling pathways. The vertical axis label represents the pathway, and the horizontal axis label represents the fold changes compared with the CDL group.The size and color of the bubble represent the number of DEGs enriched in the pathway and enrichment significance, respectively.
Statistical analysis
The means (standard deviations [SDs]) and medians (interquartile ranges [IQRs]) were used to describe normally and nonnormally distributed data, respectively. The numbers and percentages were calculated for categorical variables. The data were analyzed using the Kruskal‒Wallis test or Mann‒Whitney test (two-sided) for continuous variables and Fisher’s exact test for categorical variables using StatView-J 5.0. P values < 0.05 were considered significant.
Data availability
The datasets generated and/or analyzed during the current study are available in the DDBJ Sequence Read Archive [https://www.ddbj.nig.ac.jp/index-e.html] under the accession numbers DRA016978 and DRA017081.
References
Thomas, R. M. & Jobin, C. Microbiota in pancreatic health and disease: the next frontier in Microbiome research. Nat. Rev. Gastroenterol. Hepatol. Jan. 17 (1), 53–64 (2020).
Ye, C., Dong, C., Lin, Y., Shi, H. & Zhou, W. Interplay between the human Microbiome and biliary tract Cancer. Implications Pathogenesis Therapy Microorganisms Oct. 20 (10), 2598 (2023).
Chandra, V. & McAllister, F. Therapeutic potential of microbial modulation in pancreatic cancer. Gut Apr. 27 (8), 1419–1425 (2021).
Nagata, N. et al. Metagenomic identification of microbial signatures predicting pancreatic Cancer from a multinational study. Gastroenterology Jul;163 (1), 222–238 (2022).
Di Carlo, P. et al. The microbiota of the bilio-pancreatic system: a cohort, STROBE-compliant study. Infect. Drug Resist. Jun. 11;12, 1513–1527 (2019).
Wei, M. Y. et al. The microbiota and Microbiome in pancreatic cancer: more influential than expected. Mol. Cancer May. 20 (1), 97 (2019).
Stasiewicz, M., Kwaśniewski, M. & Karpiński, T. M. Microbial Associations with Pancreatic Cancer: A New Frontier in Biomarkers. Cancers (Basel). Jul 27;13(15):3784 (2021).
Jia, X. et al. Characterization of gut microbiota, bile acid metabolism, and cytokines in intrahepatic cholangiocarcinoma. Hepatol. Mar. 71 (3), 893–906 (2020).
Papa, V. et al. The Role of Microbiota in Pancreatic Cancer. Cancers (Basel). Jun 11;15(12):3143 (2023).
Leung, P. S. & Chan, Y. C. Role of oxidative stress in pancreatic inflammation. Antioxid. Redox Signal. Jan. 11 (1), 135–165 (2009).
Ma, Y. & Hao, J. Dedifferentiation of epithelial cells incorporates immune reprogramming. Trends Cell. Biol. Apr. 31 (4), 237–240 (2021).
Guan, S. W., Lin, Q. & Yu, H. B. Intratumour Microbiome of pancreatic cancer. World J. Gastrointest. Oncol. May 15 (5), 713–730 (2023).
Chai, X. et al. Intratumor Microbiome features reveal antitumor potentials of intrahepatic cholangiocarcinoma. Gut Microbes Jan-Dec. 15 (1), 2156255 (2023).
Xin, H. Y. et al. Characterization of tumor Microbiome and associations with prognosis in intrahepatic cholangiocarcinoma. J. Gastroenterol. May. 59 (5), 411–423 (2024).
Geller, L. T. et al. Potential role of intratumor bacteria in mediating tumor resistance to the chemotherapeutic drug gemcitabine. Science Sep15;357 (6356), 1156–1160 (2017).
Thomas, S. C., Miller, G., Li, X. & Saxena, D. Getting off tract: contributions of intraorgan microbiota to cancer in extraintestinal organs. Gut 73 (1), 175–185 (2024).
Zong, Z., Zhou, F. & Zhang, L. The fungal mycobiome: a new hallmark of cancer revealed by pan-cancer analyses. Signal. Transduct. Target. Ther. Feb 1 (1), 50 (2023).
Narunsky-Haziza, L. et al. Pan-cancer analyses reveal cancer-type-specific fungal ecologies and bacteriome interactions. Cell. Sep. 29 (20), 3789–3806e17 (2022).
Aykut, B. et al. The fungal mycobiome promotes pancreatic oncogenesis via activation of MBL. Nat. Oct. 574 (7777), 264–267 (2019).
Lyu, Z. et al. Analysis of the relationship between bile duct and duodenal microbiota reveals that potential dysbacteriosis is the main cause of primary common bile duct stones. Synth. Syst. Biotechnol. Nov. 24 (4), 414–428 (2021).
Han, J., Wu, S., Fan, Y., Tian, Y. & Kong, J. Biliary microbiota in choledocholithiasis and correlation with duodenal microbiota. Front. Cell. Infect. Microbiol. Apr. 29;11, 625589 (2021).
Del Castillo, E. et al. The microbiomes of pancreatic and duodenum tissue overlap and are highly subject specific but differ between pancreatic Cancer and noncancer subjects. Cancer Epidemiol. Biomarkers Prev. Feb. 28 (2), 370–383 (2019).
Kohi, S. et al. Alterations in the duodenal fluid Microbiome of patients with pancreatic Cancer. Clin. Gastroenterol. Hepatol. Feb. 20 (2), e196–e227 (2022).
Pushalkar, S. et al. The pancreatic Cancer Microbiome promotes oncogenesis by induction of innate and adaptive immune suppression. Cancer Discov Apr. 8 (4), 403–416 (2018).
Kamisawa, T. & Okamoto, A. Biliopancreatic and pancreatobiliary refluxes in cases with and without pancreaticobiliary maljunction: diagnosis and clinical implications. Digestion 73 (4), 228–236 (2006).
Xiao, M. et al. The dysregulation of biliary tract microflora is closely related to primary choledocholithiasis: a multicenter study. Sci. Rep. Apr. 18 (1), 9004 (2024).
Song, X. A metagenomic study of biliary Microbiome change along the cholecystitis-carcinoma sequence. Clin. Transl Med. Jun. 10 (2), e97 (2020).
Okuda, S. et al. Unveiling Microbiome profiles in human inner body fluids and tumor tissues with pancreatic or biliary tract cancer. Sci. Rep. May. 24 (1), 8766 (2022).
Saab, M. et al. Characterization of biliary microbiota dysbiosis in extrahepatic cholangiocarcinoma. PLoS One. Mar 9 (3), e0247798 (2021).
Chen, B., Fu, S. W., Lu, L. & Zhao, H. A preliminary study of biliary microbiota in patients with bile duct stones or distal cholangiocarcinoma. Biomed. Res. Int. Sep. 25;2019, 1092563 (2019).
Ito, Z. et al. Dysbiosis of the Fecal and Biliary Microbiota in Biliary Tract Cancer. Cancers (Basel). Oct 31;14(21):5379 (2022).
Li, Z. et al. Characteristics of bile microbiota in cholelithiasis, Perihilar cholangiocarcinoma, distal cholangiocarcinoma, and pancreatic cancer. Am. J. Transl Res. May. 15 (5), 2962–2971 (2022).
Dangtakot, R. et al. Profiling of Bile Microbiome Identifies District Microbial Population between Choledocholithiasis and Cholangiocarcinoma Patients. Asian Pac J Cancer Prev. Jan 1;22(1):233–240 (2021).
Maekawa, T. et al. Possible involvement of Enterococcus infection in the pathogenesis of chronic pancreatitis and cancer. Biochem. Biophys. Res. Commun. Dec. 2 (4), 962–969 (2018).
Avilés-Jiménez, F. et al. Microbiota studies in the bile duct strongly suggest a role for Helicobacter pylori in extrahepatic cholangiocarcinoma. Clin Microbiol Infect. Feb;22(2):178.e11-178.e22 (2016).
Song, X. et al. A metagenomics study of biliary Microbiome change along the cholecystitis-carcinoma sequence. Clin. Transl Med. Jun. 10 (2), e97 (2020).
Chakladar, J. et al. The pancreatic Microbiome is associated with carcinogenesis and worse prognosis in males and smokers. Cancers (Basel). 12 (9), 2672 (2020). Sep 18.
Nejman, D. et al. The human tumor Microbiome is composed of tumor type-specific intracellular bacteria. Sci. May. 29 (6494), 973–980 (2020).
Shukla, R. et al. Metagenomic analysis of biliary microbial flora in patients with gallbladder Cancer or Gallstones-Associated chronic cholecystitis. Cancer Invest. Jul. 42 (6), 478–490 (2024).
He, Z. et al. <i > Campylobacter jejuni promotes colorectal tumorigenesis through the action of cytolethal distending toxin</i >. Gut Feb. 68 (2), 289–300 (2019).
Duijster, J. W., Franz, E., Neefjes, J. & Mughini-Gras, L. Bacterial and parasitic pathogens as risk factors for cancers in the Gastrointestinal tract: A review of current epidemiological knowledge. Front. Microbiol. Dec. 8, 12:790256 (2021).
Kim, I. H. et al. Clinical significance of isolated biliary candidiasis in patients with unresectable cholangiocarcinoma. Hepatobiliary Pancreat. Dis. Int. Oct. 15 (5), 533–539 (2016).
Nogueira, F., Sharghi, S., Kuchler, K. & Lion, T. Pathogenetic impact of Bacterial- fungal interactions. Microorganisms Oct. 16 (10), 459 (2019).
Kiesel, V. A. et al. Pyruvate carboxylase and cancer progression. Cancer Metab. Apr. 30 (1), 20 (2021).
Li, D. et al. The roles of Epigallocatechin gallate in the tumor microenvironment, metabolic reprogramming, and immunotherapy. Front. Immunol. Jan. 29, 15:1331641 (2024).
Keeley, T. S., Yang, S. & Lau, E. The Diverse Contributions of Fucose Linkages in Cancer. Cancers (Basel). Aug 24;11(9):1241 (2019).
Chen, X., Wu, B. & Wang, P. G. Glucuronides in anti-cancer therapy. Curr. Med. Chem. Anticancer Agents Mar. 3 (2), 139–150 (2003).
Tucker, O. N., Dannenberg, A. J., Yang, E. K. & Fahey, T. J. 3 Bile acids induce cyclooxygenase-2 expression in human pancreatic cancer cell lines. Carcinog. Mar. 25 (3), 419–423 (2004).
Malhotra, P., Palanisamy, R., Caparros-Martin, J. A. & Falasca, M. Bile Acids and Microbiota Interplay in Pancreatic Cancer. Cancers (Basel). Jul 11;15(14):3573 (2023).
Gál, E. et al. Bile accelerates carcinogenic processes in pancreatic ductal adenocarcinoma cells through the overexpression of MUC4. Sci. Rep. Dec. 16 (1), 22088 (2020).
Zhang, X. et al. Analysis of bile acid profile in plasma to differentiate cholangiocarcinoma from benign biliary diseases and healthy controls. J. Steroid Biochem. Mol. Biol. Jan. 205, 105775 (2021).
Wallace, E. N. et al. An N-glycome tissue atlas of 15 human normal and cancer tissue types determined by MALDI-imaging mass spectrometry. Sci. Rep. Jan. 4 (1), 489 (2024).
Taniguchi, N. & Kizuka, Y. Glycans and cancer: role of N-glycans in cancer biomarker, progression and metastasis, and therapeutics. Adv. Cancer Res. 126, 11–51 (2015).
Kanehisa, M. & Goto, S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 28, 27–30 (2000).
Kanehisa, M., Furumichi, M., Sato, Y., Matsuura, Y. & Ishiguro-Watanabe, M. KEGG: biological systems database as a model of the real world. Nucleic Acids Res. 53, D672–D677 (2025).
Acknowledgements
The authors would like to thank the Bioengineering Lab. Co., Ltd., in particular.
the director, Dr. Yoshihiro Handa, for generation of all sequence data analysis.
Author information
Authors and Affiliations
Contributions
H.M. and K.S. conceived and designed the study. S.F., K.O., K.I., M.K, Y.S., Y.N., D.S., I.M., Y.Y. and H.I. recruited the subjects. Y.N., H.K. and K.T. analyzed the data. H.M. and K.S. wrote the paper. H.N., K.D., H.W., and K.S. supervised the study. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mizutani, H., Fukui, S., Oosuka, K. et al. Biliary microbiome profiling via 16 S rRNA amplicon sequencing in patients with cholangiocarcinoma, pancreatic carcinoma and choledocholithiasis. Sci Rep 15, 16966 (2025). https://doi.org/10.1038/s41598-025-00976-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-00976-6