Abstract
The iliopsoas plane block (IPB) is a novel analgesic technique that has been demonstrated to be effective for hip fracture and hip replacement surgery. This study aimed to assess the effect of IPB on postoperative quality of recovery following elective hip arthroplasty compared with femoral nerve block (FNB). One hundred patients underwent elective hip arthroplasty were randomly assigned to the IPB or FNB groups. The primary outcome was the quality of recovery 24 h after surgery. Secondary outcomes included the quality of recovery at 48 and 72 h after surgery, pain scores, quadriceps strength, first time out of bed, total opioid consumption, patient satisfaction, and complications. Compared with participants in the FNB group, Quality of recovery-15 score at 24-h was significantly higher in the IPB group (127 [123–130] vs. 117.5 [113.7–120.2]), with a median difference of 9 (95% CI, 7–11; P < 0.001). Moreover, the QoR-15 score of the IPB group was higher than that of the FNB group at 48 and 72 h after surgery (P < 0.001). However, there were no clinically significant differences between the two groups. Quadriceps strength was superior in the IPB group than that in the FNB group (P < 0.001). The first time out of bed was shorter in the IPB group than that in the FNB group (P < 0.001). This study found that IPB enhanced the quality of recovery in the first 24 h following hip arthroplasty compared with FNB.
Trial registration Chinese Clinical Trial Registry ChiCTR2200055289.
Similar content being viewed by others
Introduction
As the global population ages, the incidence of hip fractures and diseases such as femoral head necrosis is increasing1. Moreover, hip arthroplasty is becoming a frequent surgical procedure because patients desire higher functional requirements and a better quality of life2,3. Hip arthroplasty is usually associated with moderate to severe postoperative pain, which delays ambulation, increases the risk of thromboembolic events, and influences the quality of recovery4,5,6. Adequate pain management with minimal opioid-related side effects can facilitate early postoperative rehabilitation and improve functional recovery7,8. The regional anaesthetic technique, as part of a multimodal analgesic strategy, can reinforce postoperative pain control9,10.
Previous studies have indicated that the lumbar plexus block (LPB), femoral nerve block (FNB), and fascia iliaca compartment block (FICB) can reduce postoperative pain and opioid consumption in patients undergoing hip surgery. However, the conventional peripheral nerve block technique can induce quadricep muscle weakness, which delays ambulation after surgery10,11,12. Early physical therapy requires an approach that minimises pain during activity and is not limited to diminishing muscle strength. The ultrasound-guided iliopsoas plane block (IPB), a novel analgesic technique reported by Nielsen et al., selectively targets the articular branches of the femoral nerve, which provides sensory innervation of the anterior hip capsule13. Recent studies have demonstrated the efficacy of IPB in different hip-related procedures, including surgery for hip fracture and replacement, where it can provide superior analgesia without impairing motor function14,15.
Regional anaesthetic techniques for enhanced recovery after surgery (ERAS) have been shown to play an important role in improving the quality of recovery after hip surgery16,17,18. However, to date, no clinical studies have investigated whether IPB is effective in improving the quality of recovery following hip arthroplasty. We hypothesised that, relative to FNB, IPB can enhance recovery following hip arthroplasty. We designed a prospective, randomised, controlled observer-mask study to assess the effect of IPB on the quality of postoperative recovery after hip arthroplasty compared with FNB.
Patients and methods
Study design and participants
This randomised controlled trial was approved by the Medical Ethics Committee of the First Central Hospital of Baoding [2021]181 and complied with the Declaration of Helsinki. Written informed consent was obtained from all patients. The trial was registered before patient enrolment in the Chinese Clinical Trial Registry (ChiCTR2200055289; registration date: 5 January 2022; enrolment date: 20 January 2022; https://www.chictr.org.cn/searchprojEN.html). The inclusion criteria were as follows: age between 18 and 80 years, American Society of Anaesthesiologists (ASA) physical status I to III, and scheduled for elective hip arthroplasty. The exclusion criteria included allergy or intolerance to local anaesthetics, chronic pain, pre-existing neurological or anatomical deficits in the lower extremity on the side of the surgery, history of hepatic or renal insufficiency, mental/cognitive impairment, or unwillingness to participate.
Randomization and blinding
The patients were randomly assigned to the IPB or FNB groups. Randomisation was performed using a computer-generated list of random numbers to allocate patients to one of the two study groups in a 1:1 ratio. We used a sealed opaque envelope to abide by a stratified randomisation schedule in sequential order. Except for the nerve block team, which included a senior anaesthesiologist and an anaesthesia nurse, all other participants and outcome assessors were blinded to the group allocation.
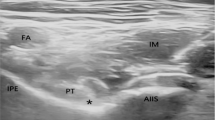
Ultrasound-guided block procedures
Patients in the IPB group were placed in the supine position, and a low-frequency ultrasound probe (M-Turbo, Sonosite, USA) was placed distal to the anterior superior iliac spine along the transverse plane. Next, the probe was rotated approximately 30° in an anticlockwise direction and moved along the inguinal ligament until the head of the femur entered the acetabular rim. After local infiltration with 1% lidocaine, a needle was inserted through the sartorius and iliopsoas muscles until it reached the plane between the iliopsoas muscle and the iliofemoral ligament. Once the position of the needle tip was confirmed, 10 mL of 0.5% ropivacaine was injected.
FNB was performed as follows: patients were first placed in the supine position, and a high-frequency linear transducer (M-Turbo, Sonosite) was then placed on the inguinal crease. The femoral artery and femoral nerves were clearly identified. After local infiltration of 1% lidocaine, a needle was inserted in the lateral-to-medial direction using an in-plane approach. Once the position of the needle tip was confirmed, 10 mL of 0.5% ropivacaine was injected adjacent to the femoral nerve.
After the completion of IPB or FNB, a lateral femoral cutaneous nerve block using 5 mL of 0.5% ropivacaine was administered to patients in both groups.
General anaesthesia and postoperative analgesia
On the day of surgery, the patients were admitted to the operating room, and vital signs were assessed via ECG, non-invasive or invasive blood pressure measurement, and pulse oximetry. After a 3-min preoxygenation step, general anaesthesia was induced via intravenous administration of 0.05 mg/kg of midazolam, 0.1–0.2 mg/kg of etomidate, and 1–2 µg/kg of remifentanil. Upon loss of consciousness, 0.6 mg/kg of rocuronium was used for endotracheal intubation placement. During anaesthesia, all patients maintained bispectral index system values between 40 and 60. Pressure-controlled ventilation was used to maintain the end-tidal partial pressure of carbon dioxide between 45 and 55 mmHg. The maintenance of anaesthesia was achieved with sevoflurane at a minimum alveolar concentration of 0.8 to 1, remifentanil at 0.1 to 0.3 µg/kg/min, propofol 2–5 mg/kg/h, and intermittent doses of rocuronium. After surgery, patients were transferred to the post-anaesthesia care unit (PACU). Perioperatively, the patients received 1000 mg of paracetamol and 200 mg of celecoxib orally as part of a multimodal analgesic regimen. If the patients had a visual analogue scale (VAS) score ≥ 4, opioids were intravenously administered as a rescue analgesic drug.
Outcome assessment
The primary outcome was the quality of recovery 24 h after surgery using the QoR-15 questionnaire. This questionnaire, with scores ranging from 0 (very poor recovery) to 150 (excellent recovery), includes five dimensions of health: physical independence, comfort, patient support, emotion, and pain. Secondary outcomes included quality of recovery at 48 and 72 h after surgery; maximum pain score at 12, 24, and 48 h after surgery; quadriceps strength at 12, 24, and 48 h after surgery; the first time out of bed (defined as the time between the end of surgery and taking at least three steps with the help of a walker, recorded after the first 10 h after surgery, and reassessed on the first day after surgery19); total opioid consumption; patient satisfaction (0–10; 0: worst, 10: great satisfaction); and the incidence of complications (i.e. postoperative dizziness, deep vein thrombosis, delirium, nausea, and vomiting). Postoperative pain was evaluated using a VAS (0–10: 0, no pain; 10, worst pain). Rescue analgesia with opioids was administered when the VAS score exceeded 3. Quadriceps strength was assessed by knee extension using the manual muscle testing (MMT) grade (knee extension was evaluated in a supine position with the patient’s hip and knee flexed at 45° and 90°, respectively). The patients were asked to extend the knee first against gravity and then against resistance. Knee extension was graded from 0 to 5; 0: no muscle contraction; 1, muscle contraction present but unable to move the joint; 2, able to move the joint but not resist gravity; 3, able to resist gravity but not bear substantial resistance; 4, able to bear certain levels of substantial resistance; and 5, able to bear full resistance. All data for each variable listed above were collected by an independent and blinded research associate.
Sample size estimation
A recent study showed that the minimal clinically important difference in QoR-15 scores for perioperative interventions was 6.020. Our experience indicated that the standard deviation of the QoR-15 24 h after surgery was 8. A sample size of 82 patients was required to achieve 90% power to detect differences in a two-tailed type I error at the 5% level. To account for potential dropouts or protocol violations, 100 participants were enrolled in this study.
Statistical analysis
All statistical analyses were performed using IBM SPSS version 26. Quantitative variables are expressed as mean or median. Continuous outcomes were tested for normality using the Kolmogorov–Smirnov test. Normally distributed data are expressed as mean ± standard deviation, and intergroup comparisons were performed using independent sample t-tests. Non-normally distributed data are expressed as median (interquartile range), and intergroup comparisons were performed using Mann–Whitney U tests. Categorical variables such as sex, ASA physical status, and complications were reported as both numbers and percentages and then compared using the chi-square test or Fisher’s exact test. The 95% confidence intervals (CI) for differences in the mean (for continuous outcomes) or relative risk (for categorical outcomes) were calculated. For any non-normally distributed continuous outcome, we used the asymptotic Hodges–Lehmann estimate and a 95% CI to estimate the median difference. P < 0.05 was considered statistically significant.
Results
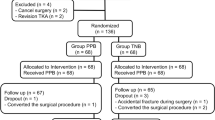
One hundred and sixty-eight patients were initially recruited, 100 of whom were ultimately enrolled and completed the study. A CONSORT diagram of this study is shown in Fig. 1. The patient characteristics and operation duration were similar between the two groups (Table 1).
Compared with patients who received an FNB block, the primary outcome QoR-15 score 24 h after surgery was significantly higher in patients who received an IPB block ([127 {123–130}] vs. [117.5 {113.7–120.2}]), with a median difference of 9 (95% CI, 7–11); P < 0.001) (Table 2; Fig. 2). The median differences (95% CI) in the QoR-15 domains at 24 h after surgery between the groups included pain 0 (0–0), physical comfort 2 (1–3), physical independence 3 (2–3), psychological support 2 (2–2), and emotions 3 (2–3) (Table 2; Fig. 3). Individual QoR-15 items with results at both baseline and 24 h are listed in Table 3. Moreover, the QoR-15 score of the IPB group was higher than the FNB group at both 48 h ([131.5{128.7–135}] vs. [128 {123–130}]) and 72 h ([137 {134–139}] vs. [133 {131–135}]) after surgery, with a median difference of 4 (95% CI, 2–6 and 2–5, respectively; P < 0.001) (Table 2; Fig. 2). In addition, quadriceps strength was higher in the IPB group than that in the FNB group at both 12 and 24 h after surgery (P < 0.001, Table 2). The first time out of bed was shorter in the IPB group than that in the FNB group (P < 0.001; Table 2).
No significant differences were observed between the IPB group and the FNB group in terms of the baseline QoR-15 score, VASmax scores, total opioid consumption, quadriceps strength at 48 h after surgery, patient satisfaction, and complications (P > 0.05, Table 2; Fig. 2).
Discussion
A suitable nerve block technique for hip arthroplasty requires an improvement in the quality of recovery through an approach that minimises pain during activity and does not limit activity by diminishing muscle strength. This randomised controlled trial observed that IPB provided a higher quality of postoperative recovery, superior quadriceps strength, and early ambulation in patients who underwent hip arthroplasty. The median difference of 9 points for the QoR-15 score at 24 h after surgery was greater than the minimal clinically important difference updated to 6.0 points by Myles PS and his colleague20. Except for the pain domain, the other QoR-15 domains were improved by IPB. Moreover, IPB rivals FNB in terms of pain management and morphine consumption. However, there were no significant differences in patient satisfaction or complications between the groups.
Following the introduction of the multimodal analgesia concept, regional anaesthetic techniques have played an important role in providing early-stage analgesia after a hip surgery. Studies have identified the key benefits of regional anaesthesia techniques on the quality of recovery after hip arthroplasty. The PROSPECT guidelines recommend fascia iliaca block as an important component of multimodal analgesia for hip arthroplasty10. Chen et al. reported that the FICB block could enhance the quality of recovery 24 h after hip arthroplasty21. However, Aliste et al. reported that fascia iliaca block resulted in quadriceps motor block in 90% of patients who underwent hip arthroplasty22. A recently published randomised controlled trial observed no differences in opioid consumption at 24 h between patients receiving SFICB and those receiving a sham block23. Owing to the complexity of the sensory supply to the hip joint, the determination of an optimal regional anaesthetic technique that has been determined remains controversial. Current optimal analgesic strategies focus on providing adequate pain management while hastening functional recovery rather than achieving satisfactory low pain. Moreover, it is imperative to accelerate the postoperative recovery of patients undergoing surgery.
Compared with traditional forms of regional analgesia, IPB has potential advantages, including the absence of motor blockage and comparable average pain scores. This may facilitate early mobilisation and participation in rehabilitation, thereby leading to increased patient satisfaction and quality of postoperative recovery. The PENG block proposed by Giron-Arango et al. is a highly similar interfacial plane block that targets the IP for analgesia of the anterior hip capsule24. Kukreja et al. measured the effect of the PENG block on the quality of recovery after THA25. These results show that the PENG block improved postoperative recovery at 24 and 48 h following THA. However, compared with the IPB, the four times higher injection volume and final needle tip position adopted in the PENG block may influence the spread extensively (probably tends to target the high branches of the femoral nerve within the FIC), which may cause quadriceps function weakness and result in motor block in a few patients. Recent studies support these findings26,27,28,29. Recently certain clinical trials and case reports on the safety and efficacy of IPB have indicated that it may be reliable for hip surgery14,15,30,31. Jessen et al.15. demonstrated that there was no difference between active IPB and placebo groups in terms of pain at rest or during follow-up. However, IPB greatly reduced opioid consumption compared to the placebo group. Wang et al. showed that IPB could rival FNB in terms of opioid consumption or postoperative pain relief; however, IPB showed better quadriceps strength retention during early functional rehabilitation training30. Zheng et al. reported that patients with hip arthroplasty who underwent IPB showed equal analgesic efficacy and better quadriceps strength retention after the block than those receiving FICB31. These results are in accordance with those of the current study. Recent studies have raised several questions. Kim et al. reported that IPB did not improve postoperative analgesia following total hip arthroplasty under general anaesthesia with multimodal analgesia32. We speculate the inability of IPB to improve pain management may be attributed to the choice of analgesics varies; a transdermal buprenorphine patch and nefopam may have facilitated remarkable pain alleviation.
Early rehabilitation training may translate into a better postoperative quality of recovery. For ERAS, using VAS pain scores alone to evaluate new regional anaesthetic techniques is not sufficiently comprehensive because it omits patients’ psychological health. We considered these factors when choosing the outcome criteria and adopted the QoR-15 score to evaluate the overall quality of recovery33,34,35. The subjective postoperative experience of patients is becoming increasingly important for assessing the quality of recovery from various surgeries. The 15-item quality of recovery instrument is a patient-centred measurement used to comprehensively measure the clinical impact of an intervention. Moreover, its advantage is that it includes five health dimensions: physical independence, comfort, patient support, emotions, and pain33. Here, we demonstrated that patients receiving an IPB block showed significantly improved postoperative recovery 24 h after surgery, and achieved significant clinical significance at the same time.
The evaluation of clinical significance should focus on patient-centred outcome measure. This is a complex concept which may be influenced by some intrinsic factors such as mood, feelings, options, symptoms and function improvement. At the same time, we should focus on what patients experience. In this study, the regional anesthesia technique has a beneficial effect on pain control, which may reduce opioid consumption, thereby avoiding opioid-related nausea and vomiting. The quality of recovery-15 is a multidimensional patient-reported outcome. Regarding the QoR-15 patient’s answers, the patients acquired a superior score in IPB group after hip arthroplasty, however, a statistically significant change does not necessarily translate to clinical significance. The patients in IPB group may retain quadriceps strength at 12 and 24 h after surgery and ambulate starting from the first postoperative day, which can contribute to emotion and mood regulation via encouraging patients improve range of motion after hip surgery and perform activities of daily living function sports. These patients who received hip arthroplasty generally experienced significant preoperative pain and functional limitations, which may cause psychological distress such as stress, anxiety, and so on. So, in a similar clinical context, group IPB patients exhibited a significantly better prognostic experience on the first postoperative day with marked differences in functional recovery or clinical outcomes between the two groups. people. negatively influences.
In contrast, Kim et al.32. demonstrated that IPB did not improve the quality of recovery or patient satisfaction compared to that in the sham block, possibly because early-stage motor functional recovery may improve the overall quality of recovery; in a similar analgesic context, the sham block did not prolong the motor block. However, FNB may weaken quadriceps muscle strength and delay mobilisation. Moreover, the minimal clinically important difference measured by the QoR-15 scale was updated to 6.020, indicating that there were no clinically significant differences in the quality of recovery at 48 and 72 h after surgery in this study. We attribute this discrepancy to the fact that patients’ physical independence was effectively improved during the first 24 h postoperatively, and this may be enough to improve other elements of postoperative recovery such as physical independence, comfort, patient support and emotions. Besides, a single-injection IPB block is only effective for a limited time, so, we failed to detect any obvious clinical differences at 48 and 72 h after surgery. In our study, patients in the IPB group were able to flex and lift the affected limb immediately after surgery and were able to get out of bed and walk a short distance relatively soon after the procedure. The patient’s emotions and psychological states were greatly comforted.
In the current trial, quadriceps strength was higher in the IPB group than that in the FNB group at 12 h ([5 {4–5}] vs. [3 {2–3}]) and 24 h ([5 {5–5}] vs. [4 {3–5}]) after surgery. An IPB is a motor-sparing block. Kim et al. recently demonstrated that compared to that in the sham block, IPB did not influence quadriceps strength during the postoperative period, and there was no significant difference between the two study groups32. The Jessen trial confirmed the observation made in our studies that IPB using 10 mL of local anaesthetic rarely weakens the quadriceps muscle strength15.
Although we did not observe the weakness of the quadriceps muscle or postoperative falls in the IPB group, a few patients might have displayed slightly impaired thigh muscle strength in the limb on the side of surgery, and the quadriceps strength at 12 h in the IPB group was higher than that in the FNB group ([5 [4–5] vs. [3 {2–3}]). We speculated that a single injection of 10 mL ropivacaine might be excessive, which would affect motor testing. Wang et al.14 showed that the quadriceps strength of patients in the IPB group was no more than MMT grade 4 of 5 upon arrival at the PACU, which is sufficient for out-of-bed functional exercise. In contrast, Nielsen et al. reported no significant reduction in the maximal muscle force of knee extension was observed 1 h after IPB with 5 mL lidocaine13,36. Thus, 10 mL has the risk of spreading to the motor branches of the femoral nerve, and further studies should focus on the optimal dose and concentration of the local anaesthetic used for IPB.
Our study had several limitations. First, owing to the lack of adequate controls, in the future, we should investigate the effect of IPB relative to that of a sham block with respect to the quality of recovery after hip surgery, which may help us establish the validity and safety of IPB. Second, the long-term quality of recovery was not evaluated; we only assessed the QoR-15 scores within three days of hip arthroplasty. Further studies are needed to investigate the long-term quality of functional recovery including 7days, one months, three months etc. Furthermore, the strength of the quadriceps muscles is rough and subjective, masking many potential confounding factors, such as the participants’ and examiner’s position, the duration of action of local anesthetic drugs, the patient’s pain, and cooperation. Finally, the relatively small sample size may have limited the robustness of secondary outcomes. This size limitation means that the potential adverse effects of IPB, such as infection or in-hospital falls, may have been overlooked. Future studies with larger sample sizes are needed to address these limitations and provide more reliable results.
Conclusions
Compared with FNB, IPB can improve postoperative recovery quality, provide effective pain relief, preserve quadriceps function, shorten the first time out of bed, and facilitate earlier mobility in patients undergoing hip arthroplasty.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due as a part of a series of studies which have not been completed, but are available from the corresponding author on reasonable request.
References
Bhandari, M. & Swiontkowski, M. Management of acute hip fracture. N. Engl. J. Med.377, 2053–2062 (2017).
Kurtz, S., Ong, K., Lau, E., Mowat, F. & Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg. Am.89, 780–785 (2007).
Pabinger, C., Lothaller, H., Portner, N. & Geissler, A. Projections of hip arthroplasty in OECD countries up to 2050. Hip Int.28, 498–506 (2018).
Wylde, V., Rooker, J., Halliday, L. & Blom, A. Acute postoperative pain at rest after hip and knee arthroplasty: Severity, sensory qualities and impact on sleep. Orthop. Traumatol. Surg. Res.97, 139–144 (2011).
Hsia, H. L. et al. Acute pain is associated with chronic opioid use after total knee arthroplasty. Reg. Anesth. Pain Med.43, 705–711 (2018).
Van Heghe, A. et al. Effects of orthogeriatric care models on outcomes of hip fracture patients: A systematic review and meta-analysis. Calcif. Tissue Int.110, 162–184 (2022).
Morrison, R. S. et al. Relationship between pain and opioid analgesics on the development of delirium following hip fracture. J. Gerontol. Biol. Sci. Med. Sci.58, 76–81 (2003).
Højer Karlsen, A. P., Geisler, A., Petersen, P. L., Mathiesen, O. & Dahl, J. B. Postoperative pain treatment after total hip arthroplasty: A systematic review. Pain156, 8–30 (2015).
Gottlieb, M. & Long, B. Peripheral nerve block for hip fracture. Acad. Emerg. Med.28, 1198–1199 (2021).
Anger, M. et al. PROSPECT working group** and the European society of regional anaesthesia and pain therapy. PROSPECT guideline for total hip arthroplasty: A systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia76, 1082–1097 (2021).
Jaeger, P. et al. Adductor Canal block versus femoral nerve block and quadriceps strength: A randomized, double-blind, placebo-controlled, crossover study in healthy volunteers. Anesthesiology118, 409–415 (2013).
Behrends, M. et al. Preoperative fascia Iliaca block does not improve analgesia after arthroscopic hip surgery, but causes quadriceps muscles weakness: A randomized, Double-blind trial. Anesthesiology129, 536–543 (2018).
Nielsen, N. D. et al. Spread of injectate around hip articular sensory branches of the femoral nerve in cadavers. Acta Anaesthesiol. Scand.62, 1001–1006 (2018).
Wang, C. G., Yang, Y., Yang, M. Y., Wang, X. L. & Ding, Y. L. Analgesic effect of Iliopsoas plane block for hip fracture. Perioper. Med.11, 15 (2022).
Jessen, C. et al. Efficacy of Iliopsoas plane block for patients undergoing hip arthroscopy: A prospective, triple-blind, randomized, placebo-controlled trial. Reg. Anesth. Pain Med. (2023).
Zhao, J. & Davis, S. P. An integrative review of multimodal pain management on patient recovery after total hip and knee arthroplasty. Int. J. Nurs. Stud.98, 94–106 (2019).
Debono, B. et al. Consensus statement for perioperative care in lumbar spinal fusion: Enhanced recovery after surgery (ERAS®) society recommendations. Spine J.21, 729–752 (2021).
Morrell, A. T. et al. Enhanced recovery after primary total hip and knee arthroplasty: A systematic review. J. Bone Jt. Surg. Am.103, 1938–1947 (2021).
Pascarella, G. et al. Impact of the pericapsular nerve group (PENG) block on postoperative analgesia and functional recovery following total hip arthroplasty: A randomised, observer-masked, controlled trial. Anaesthesia76, 1492–1498 (2021).
Myles, P. S. & Myles, D. B. An updated minimal clinically important difference for the QoR-15 scale. Anesthesiology135, 934–935 (2021).
Chen, L. et al. Effect of perioperative ultrasound guided fascia Iliaca compartment block in elderly adults with hip fractures undergoing arthroplasty in spinal anesthesia-a randomized controlled trial. BMC Geriatr.23, 66 (2023).
Aliste, J. et al. Randomized comparison between pericapsular nerve group (PENG) block and suprainguinal fascia Iliaca block for total hip arthroplasty. Reg. Anesth. Pain Med.46(10), 874–878 (2021).
Safa, B. et al. Ultrasound-guided suprainguinal fascia Iliaca compartment block and early postoperative analgesia after total hip arthroplasty: A randomised controlled trial. Br. J. Anaesth.133(1), 146–151 (2024).
Girón-Arango, L. et al. Pericapsular nerve group (PENG) block for hip fracture. Reg. Anesth. Pain Med.43(8), 859–863 (2018).
Kukreja, P. et al. Quality of recovery after pericapsular nerve group (PENG) block for primary total hip arthroplasty under spinal anaesthesia: A randomised controlled observer-blinded trial. Br. J. Anaesth.130, 773–779 (2023).
Yeoh, S. R., Chou, Y., Chan, S. M., Hou, J. D. & Lin, J. A. Pericapsular nerve group block and Iliopsoas plane block: A scoping review of quadriceps weakness after two proclaimed Motor-Sparing hip blocks. Healthcare10, 1565 (2022).
Endersby, R. V. W. et al. Motor Blockade after Iliopsoas plane (IPB) and pericapsular nerve group (PENG) blocks: A little May go a long way. Acta Anaesthesiol. Scand.65, 135–136 (2021).
Mistry, T. & Sonawane, K. B. Gray zone of pericapsular nerve group (PENG) block. J. Clin. Anesth.58, 123–124 (2019).
Yu, H. C. et al. Inadvertent quadriceps weakness following the pericapsular nerve group (PENG) block. Reg. Anesth. Pain Med.44, 611–613 (2019).
Wang, C. G. et al. A randomized controlled trial of Iliopsoas plane block vs. femoral nerve block for hip arthroplasty. BMC Anesthesiol.23, 197 (2023).
Zheng Yl, Gao, X. M., Li, X. P., Gao, C. J. & Wang, F. Comparison of the efficacy of ultrasound guided Iliopsoas plane block and fascia Iliaca compartment block in patients undergoing hip arthroplasty. J. Clin. Anesthesiol.39, 346–350 (2023).
Kim, J. Y. et al. Iliopsoas plane block does not improve pain after primary total hip arthroplasty in the presence of multimodal analgesia: A single institution randomized controlled trial. Reg. Anesth. Pain Med. (2024).
Stark, P. A., Myles, P. S. & Burke, J. A. Development and psychometric evaluation of a postoperative quality of recovery score: The QoR-15. Anesthesiology118, 1332–1340 (2013).
Myles, P. S. Measuring quality of recovery in perioperative clinical trials. Curr. Opin. Anaesthesiol.31, 396–401 (2018).
Kleif, J., Waage, J., Christensen, K. B. & Gögenur, I. Systematic review of the QoR-15 score, a patient- reported outcome measure measuring quality of recovery after surgery and anaesthesia. Br. J. Anaesth.120, 28–36 (2018).
Nielsen, N. D. et al. An Iliopsoas plane block does not cause motor blockade-A blinded randomized volunteer trial. Acta Anaesthesiol. Scand.64, 368–377 (2020).
Funding
This work was supported by grants from Science and Technology Plan Project of Baoding (2241ZF238), the Natural Science Foundation project of Hebei Province (H2024104012) and the Traditional Chinese Medicine Scientifc Research Project of Hebei Province (2025547).
Author information
Authors and Affiliations
Contributions
Study concept: C.G.W., B.W.J.; Study protocol: C.G.W., B.W.J.; Statistical analysis: Y.G.; Analysis and interpretation of data: Y.H.B., Y.N.H., K.F.Z., X.C., Y.B.; LDesign of case report form and database components: C.G.W., B.W.; JWriting of the first draft of the manuscript: C.G.W., B.W.J.; Critically editing and revising the manuscript and final approval: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This randomised controlled trial was approved by the Medical Ethics Committee of the First Central Hospital of Baoding [2021]181.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jiang, Bw., Guo, Y., Han, Yn. et al. Iliopsoas plane block versus femoral nerve block for postoperative quality of recovery following hip arthroplasty: a randomized controlled trial. Sci Rep 15, 15723 (2025). https://doi.org/10.1038/s41598-025-00978-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-00978-4