Abstract
Mental health disorders affect 15% of youth aged 10–19 years globally, typically emerging before age 15. While school-based peer-led programs show promise in improving physical health behaviours by leveraging existing social networks, reducing stigma, and demonstrating high implementation feasibility, their effectiveness for mental health outcomes remains unclear. This systematic review examined controlled trials of school-based, peer-led lifestyle interventions (physical activity, diet, or sleep) reporting mental health outcomes in adolescents aged 10–19 years. Six electronic databases were searched up to March 28, 2024. Seven studies met inclusion criteria, encompassing 7,060 adolescents from 151 schools across the UK, USA, Canada, and Norway. Interventions varied in frequency and duration, with six focusing on physical activity and one on diet. Meta-analyses revealed no significant effects for psychological difficulties (MD = 0.60, 95% CI -3.52 to 4.72; p = 0.32, k = 2), self-efficacy for physical activity (SMD = 0.18, 95% CI -3.08 to 3.44; p = 0.61, k = 2), or wellbeing (SMD = 0.0, 95% CI -2.94 to 2.94; p = 1.0, k = 2). These findings, while requiring cautious interpretation, highlight the pressing need for more comprehensive and rigorous research to better understand the impact of peer-led interventions on mental health outcomes.
Similar content being viewed by others
Introduction
Adolescents’ mental health poses a critical public health challenge, with mental disorders affecting one in seven 10–19-year-olds globally and accounting for 15% of the global burden of disease in this age group1. Mental ill-health typically emerges before the age of 152, contributing to adverse health, academic, and social outcomes3,4,5that often persist into adulthood6. Despite the treatability of these conditions, less than two-thirds of affected adolescents access professional help7,8. The Lancet Psychiatry Commission into youth mental health has called for urgent action, emphasising the need for evidence-based interventions and multidisciplinary wrap around care - an approach that integrates multiple services (e.g., mental health, educational, social, and family support) into a seamless, personalised network designed to fully address each young person’s unique needs9.
Mental and physical health outcomes are inextricably linked. Young people experiencing, or at risk of, mental ill-health demonstrate significantly poorer physical health compared to their peers10. Cardiometabolic risk factors, such as obesity, dyslipidaemia, and hypertension, often go undetected and therefore untreated, contributing to almost 80% of premature deaths in people with mental ill-health11. This health burden is compounded by higher levels of detrimental health behaviours, including poor diet, physical inactivity, and disrupted sleep, which contribute to a cycle of deteriorating mental and physical health12,13,14. In the context of the current global obesity epidemic declared by the World Health Organization, physical activity and diet have emerged as cornerstones of health interventions for adolescents. Interventions targeting these lifestyle risk factors offer a promising non-pharmacological approach that can both reduce the risk of developing, and treat symptoms of, mental and physical health conditions, simultaneously. Robust data from meta-analyses demonstrate the effectiveness of physical activity, diet, and sleep interventions for improving mental health in adult populations15,16,17 and increasingly strong evidence suggests physical activity can protect against depression in adolescents18. Furthermore, an emerging evidence base indicates diet quality correlates with depression severity16,19 and sleep patterns are bidirectionally related to depression and anxiety20,21, suggesting lifestyle interventions can provide a non-stigmatising approach to mental health care.
Schools represent an ideal setting for early mental health intervention22, with peer-led programs increasingly implemented across the globe, targeting diverse mental and physical health outcomes23. These interventions capitalise on the significance of peer influence during adolescence24 and evidence showing adolescents’ preference for seeking help from peers or informal sources of support for psychological needs25. Peer-led programs may be particularly attractive as a delivery method for low-intensity interventions within the school setting, given their relatively low use of resources, flexibility in design and delivery, and scalability to reach many students26.
Previous systematic reviews have examined peer-led mental health education interventions (e.g., bullying, mental health literacy) for mental health outcomes23,27 or the effectiveness of peer-led lifestyle interventions for changing health behaviours28,29, with results demonstrating small but promising changes on their respective outcomes across both peer recipients and peer leaders. However, to our knowledge, no review to date has synthesised the effectiveness of peer-led lifestyle behaviour interventions on mental health outcomes. Given the relationship between lifestyle behaviours and mental health, this systematic review aims to address this gap and evaluate the effectiveness of peer-led lifestyle interventions (physical activity, diet and sleep) on mental health outcomes in adolescents within the school-setting.
Methods
Protocol and registration
This review is reported in accordance with PRISMA guidelines30 and the protocol was pre-registered on PROSPERO (CRD42024511031).
Search strategy and selection criteria
Six electronic databases were searched (Medline, Embase, Emcare, CINAHL, Scopus and PSYCinfo) using subject heading, keyword and MeSH term searches for “adolescents”, “students”, “school”, “life style”, “exercise”, “diet”, “sleep”, “mental health”, “mental disorders”, “happiness” and “resilience” (see Supplementary file 1 for the full search strategy). Database searches were limited to peer-reviewed journal articles published in English language from inception until March 2024.
Inclusion/exclusion criteria
The population, intervention, comparison, outcomes and study type (PICOS) framework was used to develop the eligibility criteria. Population: studies where participants’ mean age was 10–19 years. Interventions: school-based interventions (i.e., health promotion, experiential, educational) that focused on improving lifestyle behaviours (e.g., physical activity, diet, sleep) and involved a peer-led component (i.e., delivered by adolescents to adolescents) were eligible. Comparator: age-matched comparison groups including no intervention, waitlist control, or an alternate intervention that did not involve a peer-led mental health or lifestyle component were eligible. Outcomes: studies reporting changes in mental health outcomes from pre- to post-intervention were eligible. Studies only reporting acute affect (i.e., mood) were excluded. Study design: randomised controlled trials and non-randomised controlled trials were eligible.
Data extraction
Search results were imported into Covidence (Veritas Health Innovation, Melbourne, Australia) where duplicates were removed. All stages of screening were completed independently and in duplicate by two authors (JB, MS, RC, CS, JE, EE, GG, MB, BJ, ET), with disagreements resolved by discussion with the senior author (CM). Data were extracted in duplicate by two authors independently (JB, MS, RC, CS, JE, EE, GG, MB, BJ, ET), with disagreements resolved by discussion between authors. A standardised data extraction form was used to extract the following data from eligible studies: study characteristics (e.g., design, country), participant details (e.g., sample size, demographic characteristics), intervention details (e.g., components, duration), outcome measures, results for relevant outcomes. Authors of included studies were contacted to provide additional data for inclusion in the meta-analysis if required.
Risk of bias and evidence quality assessment
Study quality and risk of bias was assessed independently in duplicate using the Cochrane Risk of Bias (RoB) tool for randomised controlled trials31, with discrepancies resolved between authors. The Cochrane RoB tool evaluates study-specific RoB across the following domains: randomisation and recruitment, deviations from intended intervention, missing outcome data, measurement of outcomes and selection of reported results. Domains are categorised as low, some, or high risk of bias after assessing criterion on a 4-point scale (“yes/probably yes”, “no/probably no”, “no information” and “not applicable”).
Outcomes of interest
Mental health outcomes included both positive aspects, such as psychological and subjective wellbeing (i.e., meaning, purpose, life satisfaction), and negative aspects, such as symptoms of mental ill-health (i.e., depression, anxiety, distress). In addition, psychosocial factors related to mental health, such as self-esteem, self-efficacy, resilience, and body image, were considered.
Data synthesis
Intervention effect sizes (differences between intervention and control groups) for outcome data were calculated across all studies and standardised to Hedges G32 along with the standard error. Studies were grouped by the mental health domain of the outcome for analyses. Random-effects meta-analyses were conducted due to expected heterogeneity. All analyses used an inverse variance method with restricted maximum-likelihood estimator for tau2 and Hartung-Knapp adjustment for random-effects model. Standardised mean differences (SMDs) were used as the effect measure for meta-analyses, to allow comparison of data from different scales. If means and standard deviations (SDs) were not reported in a study, authors were contacted twice before means and SDs were calculated based on available data, using recommended formulas (e.g., using sample size, median and range)33. Meta-analyses were conducted if at least two studies reported the same mental health outcome. Effect sizes were categorised as small (0.2), medium (0.5), or large (0.8 or greater)34, with significance level set at 0.0535. Cochrane’s Q test was used to assess statistical heterogeneity and the I2 statistic to quantify the proportion of the overall outcome effect attributed to heterogeneity. The following cut-off values for the I2 statistic were used: 0–29% = no heterogeneity; 30–49% = moderate heterogeneity, 50–74% = substantial heterogeneity and 75–100% = considerable heterogeneity. When meta-analyses included ≥ 10 studies, publication bias was assessed with visual inspection of funnel plots and tested using the Begg-Mazumdar and Egger’s regression method, with a p-value < 0.05 suggesting the presence of bias. Where significant bias was detected, a Duval and Tweedie trim-and-fill analysis was applied. Heterogeneity was explored with subgroup and sensitivity analyses. All analyses were conducted in R version 4.2.0 (“Mountain Hydrangea”, 2023-07-07).
A narrative synthesis approach36 was used to analyse and present findings given the small number of studies. Studies were grouped by outcome and individual study outcomes were examined and reported descriptively. Heterogeneity was explored through examination of study characteristics and methodological variations. A vote counting tool, as recommended by Popay and colleagues36, was implemented to visually illustrate when a study reported a positive effect, a negative effect or did not report for a given outcome (Supplementary File 3).
Results
Literature search and screening
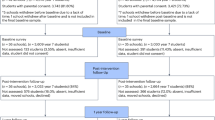
Database searches identified 5212 records. Following removal of duplicates, and title and abstract screening, 106 full-text articles were retrieved, of which 7 were included (see Fig. 1 for study selection and exclusion reasons).
Study characteristics
Table 1 provides an overview of included studies. The included studies encompass 7,060 adolescents from 151 schools with study samples ranging from 114 to 2120 participants. Interventions were implemented in the UK37,38,39, USA40, Canada41 and Norway42 between 2010 and 2024. Six studies used a randomised controlled design, and one study used a quasi-experimental design40. Three studies cited using an established theory (e.g., Social Cognitive Theory)38,39,40 and three cited principles that underpinned the program (e.g., goal-directed behaviour, self-efficacy)37,41,42. All studies aimed to improve the targeted lifestyle behaviour(s), while two studies also specifically aimed to improve mental health42,43.
Intervention characteristics
Five interventions focused on physical activity37,38,39,42,43, one on nutrition41, and one on both physical activity and nutrition36. Interventions ranged from daily38,39, twice per week37,42, weekly41,43, to every three weeks40, and lasted from six to 29 weeks in duration. See Table 1 for details on intervention session length, frequency and duration.
Peer-leaders
Peer-leaders consisted of year nine students37,43, pupils aged 15–18 years38, and final year health students40. Three studies39,41,42 did not describe the peer-leaders. Across all studies, except Avitsland et al.42, peer-leaders were older than peer-recipients. The intervention by Avitsland et al.42 was fundamentally different in that peer-leaders were not selected and trained, but in each lesson, children organically emerged as leaders for the activity.
Selection of peer-leaders
Selection of peer-leaders was generally not well reported, however, studies reported older pupils volunteering39, school staff nominating students37,38,41, and peer-leaders being selected based on their understanding of the population, ability to provide support to peer-recipients and their role-modelling capabilities40.
Training of peer-leaders
Training of peer-leaders was well described in one study38, one study provided no detail37, and the remaining studies provided a vague description of the training process. Collectively, peer-leadership training involved providing information about the research protocol, educational content for lessons, teaching methods and activities, strategies to promote engagement and motivation, and mentoring and social support principles. Time spent training peer-leaders varied from a single lunchtime session39, a 1-hour session37, 2 full days with 30-minute booster sessions each week41, weekly43, and twice weekly for 10 weeks40. It was unclear whether the training occurred during class time at school, during break time at school or outside of school time. Two interventions38,39 included the use of closed social media groups to provide additional support (i.e., answer questions, give tips, provide information) and a place for discussion for peer-leaders.
Role of peer-leaders
Peer leaders across the included studies primarily facilitated health-related activities, delivered educational content and provided social support. Their responsibilities often included leading specific activities, such as guiding physical activity sessions37,38,39,43, or running classroom-based lessons focused on health behaviours, such as physical activity or nutrition40,41. Four studies38,40,41,43 involved peer leaders delivering structured educational content using pre-prepared materials to promote health behaviours, and providing social support and peer accountability was explicitly mentioned in three studies37,38,40. Adult supervision was present in five studies37,38,39,40,41, with teachers or facilitators occasionally stepping in to support or oversee activities. The extent of the peer-leaders involvement varied considerably across studies, ranging from partial facilitation of activities41,43to delivering the majority of the intervention independently38,40.
Risk of bias and quality assessment
Six studies were considered to be at ‘high risk’ of bias37,38,39,40,41,43 due to deviations from the intended intervention (5/7) or not randomly allocating students (1/7). One study was considered to have ‘some risk’ of bias42. See Table 2 for the full risk of bias assessment for each study.
Mental health
Meta-analysis
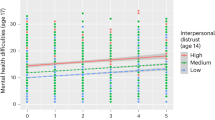
Two studies42,43 utilised the Strengths and Difficulties questionnaire which reports psychological difficulties, expressed as the total difficulties score, which ranges from 0 to 40 with higher scores signifying worse outcomes. This meta-analysis included a total of 1907 participants, revealing a non-significant effect (MD = 0.6, 95% CI −3.52 to 4.72; p 0.32; Fig. 2). Moderate heterogeneity was present in the analysis (Cochran’s Q = 1.47, p = 0.23; I2 = 32%).
Wellbeing
Meta-analysis
Two studies reported on wellbeing using two different tools - the Warwick-Edinburgh Mental Wellbeing Scale and the KIDSCREEN-27. For the latter, the psychological wellbeing subscale, which aligns with the construct of wellbeing, was used in the analysis. This meta-analysis included a total of 1297 participants. The pooled analysis revealed no effect on peer-recipients’ wellbeing (SMD = 0.00, 95% CI −2.94 to 2.94; p 1.0; Fig. 3). The analysis displayed substantial, significant heterogeneity between studies (Cochran’s Q = 12.6, p < 0.001; I2 = 92%).
Self-efficacy for physical activity
Meta-analysis
Two studies39,40 examined the impact of peer-led lifestyle interventions on self-efficacy for physical activity, encompassing a total of 282 participants. The meta-analysis revealed a non-significant small favourable effect (SMD = 0.18, 95% CI −3.08 to 3.44; p 0.0.61, Fig. 4), with considerable heterogeneity between studies (Cochran’s Q = 4.07, p = 0.04; I2 = 75%).
Self-efficacy
Narrative synthesis
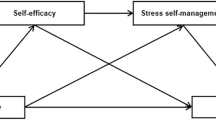
Self-efficacy was assessed more broadly in four studies, though studies varied substantially in both the measurement approach and the specific domain of self-efficacy assessed. Two studies focused on dietary self-efficacy40,41, one on walking self-efficacy39, and one on self-efficacy for support-seeking for physical activity37. The HART Project40 and Goals for Health41 both examined dietary self-efficacy but employed different measurement approaches, precluding quantitative synthesis. The HART Project reported significant positive changes in self-efficacy while Goals for Health found initial improvements in the intervention group (ES = 0.05), however they were not sustained at final follow-up. Notably, significant gender and racial differences were identified in dietary self-efficacy outcomes in the Goals for Health intervention, such that males reported less confidence in their ability to eat healthier than females and African Americans reported lower self-efficacy to eat healthier than Caucasian Americans41. For physical activity-related self-efficacy, the WISH study39 reported no significant between-group differences post-intervention. In contrast, GoActive37 focused on self-efficacy for seeking support for physical activity, reporting significant improvements in the intervention group (difference: 0.5, 95% CI: 0.1 to 0.9, p = 0.03).
Emotional Regulation
Narrative synthesis
One study examined emotional regulation outcomes through a peer-led walking intervention, reporting no significant difference38.
Sensitivity analyses
Sensitivity analyses were planned but could not be conducted due to the limited number of studies included in each meta-analysis.
Publication bias
No pooled analyses included ≥ 10 studies, therefore formal evaluation of publication bias was not possible.
Discussion
Peer-led interventions to promote adolescent health are implemented globally. This systematic review and meta-analysis aimed to examine the effect of school-based peer-led lifestyle interventions on adolescents’ mental health. The seven included studies reported on mental health, wellbeing, emotional regulation and self-efficacy. Meta-analyses for psychological difficulties, wellbeing and self-efficacy showed no significant effects. However, there is some limited evidence suggesting that the interventions might have a potential positive impact on self-efficacy. While the meta-analysis indicated a small, statistically non-significant effect size, the narrative synthesis found improvements in various self-efficacy measures in 3 out of 4 studies. Due to the small number of studies, mixed findings, and variability in mental health domains and measurement tools used, the evidence for the use of peer-led lifestyle interventions for mental health outcomes is weak.
Our findings contribute to the evolving understanding of peer-led interventions at the intersection of health behaviours and mental health outcomes. While a prior review, focusing on physical activity, found that school-based interventions positively impacted mental health outcomes such as anxiety, resilience, and wellbeing44, our review, which predominantly included physical activity interventions (5/7 included studies) reveals more nuanced results when health behaviour interventions are specifically delivered through peer-led approaches. The literature suggests variable effectiveness for mental health outcomes across different types of peer-led programs. Some interventions improved self-confidence and quality of life, while others demonstrated no effect or even negative impacts on measures such as learning stress and general mental health43. This variability is reflected in the current review of lifestyle interventions targeting mental health outcomes, suggesting that refined implementation strategies may be needed for lifestyle-based approaches to mental health promotion. A key factor might be the limited mental health-specific training provided to peer leaders in many of the reviewed studies, which likely constrained intervention effectiveness. This highlights the need for more comprehensive peer leader preparation that integrates both lifestyle and mental health components.
Our results showed no effect on wellbeing, with substantial heterogeneity, reflecting the complex and multidimensional nature of this construct. Wellbeing is influenced by numerous individual, social, and environmental factors, making it challenging to isolate the specific impacts of peer-led lifestyle interventions. Addressing this conceptual and methodological complexity will be crucial for future research aiming to elucidate the wellbeing effects of such programs. Our non-significant findings for self-efficacy align with literature suggesting it may function more as a mediator of behavioural change than a direct intervention outcome45. While self-efficacy is associated with predicting physical activity engagement, the directionality of this relationship remains unclear, with research indicating it primarily serves as a covariate influencing other psychosocial factors46. This understanding suggests future peer-led interventions should consider designing components that enhance self-efficacy as a pathway to behavioural change, rather than treating it solely as an outcome measure. The null findings observed for emotional regulation can be attributed to several key factors. The intervention’s primary emphasis on physical activity likely provided insufficient opportunities for emotional learning and regulatory skill development. The brief, activity-focused sessions prioritised behavioural engagement whereas emotional regulation typically develops through nuanced social interactions and explicit instruction in coping strategies, rather than through physical activity alone47,48. Moreover, the structured walking sessions may not have generated the diverse emotional experiences necessary for developing and practicing regulation skills.
A common theme across all outcomes was the potential influence of baseline characteristics, with many participants demonstrating relatively normal baseline levels of mental health, wellbeing, and self-efficacy. These initial characteristics may have created ceiling effects that limited the detection of measurable improvements, particularly given peer-led programs appear most effective when focused on specific, well-defined health behaviours or straightforward health education initiatives29,49. The variability in measurement tools across studies further complicated the synthesis of these outcomes, emphasising the need for standardised assessment approaches in future research. To address these limitations, future studies should consider implementing more sensitive measurement tools capable of detecting subtle changes in generally healthy populations, while potentially stratifying analyses by baseline levels to better understand intervention effects across different participant subgroups. This approach, combined with tailored interventions targeting individuals with specific needs, may help to uncover subtler benefits and optimise the design of peer-led programs.
Intervention design varied considerably across studies, particularly in terms of duration and intensity. Physical activity interventions ranged from brief, structured walking sessions to comprehensive programs incorporating multiple lifestyle behaviours. While physical activity is well-documented to improve mental health outcomes, the non-significant findings in this review suggest interventions may not have reached sufficient thresholds of intensity or duration to produce measurable improvements in adolescents. Furthermore, most interventions focused primarily on physical activity, with limited integration of other evidence-based lifestyle components such as diet and sleep that are known to influence mental health outcomes12,14.
Studies demonstrated marked variation in peer leader recruitment and preparation, with some implementing structured selection processes and comprehensive training programs, while others relied on voluntary participation without explicit criteria. This variability in peer leader preparation likely influenced intervention delivery quality and consistency. Feedback from the GoActive trial highlighted this challenge, with mentors expressing the need for clearer instruction and increased teacher support37. These findings align with King and Fazel’s27 observation that limited guidance exists for peer leader best practices, underscoring the need for standardised protocols.
Contextual factors within the school setting presented unique challenges for intervention implementation. The need to balance intervention fidelity with practical constraints of the school environment often resulted in adaptations that may have affected program effectiveness. The practical constraints of school-based delivery often necessitated flexible implementation protocols, making it difficult to determine the extent to which interventions were delivered as intended. Additionally, the level of staff support and resources available varied across settings, influencing the quality of peer leader supervision and program delivery. These contextual variations highlight the importance of developing interventions that can maintain effectiveness while accommodating the practical constraints of educational settings.
Strengths and limitations
Our systematic review adhered to rigorous methodological approaches and employed comprehensive search strategies across multiple databases. The broad inclusion of mental health domains allowed for a holistic examination of psychological outcomes, while our multi-method synthesis enabled comprehensive evidence synthesis. However, limitations arose from the included studies’ generally high risk of bias, small sample sizes, and inconsistent measurement tools. Additionally, the use of self-report measures and potential ceiling effects in generally healthy populations may have limited the ability to detect meaningful changes. These findings should therefore be interpreted cautiously.
Implications for future research and practice
More research is needed to evaluate the effectiveness of peer-led lifestyle interventions for mental health outcomes within school settings. Future studies should investigate optimal intervention dosage and explore combining multiple lifestyle behaviours for synergistic effects on mental health outcomes. This is grounded in accumulating evidence showing that lifestyle behaviours simultaneously influence overlapping mechanisms, including inflammation, neuroplasticity, and stress regulation—potentially creating amplified benefits for mental health compared to single-behaviour interventions17,50,51. Additionally, research should examine innovative approaches to integrate mental and physical health promotion utilising existing school structures. A key priority is the development of sustainable peer leadership frameworks that embed within educational systems rather than function as standalone programs. This approach aligns with the World Health Organisation’s Health Promoting Schools Framework, which advocates a whole-school approach addressing curriculum, school ethos and environment, and community engagement, and includes major stakeholders in an adolescent’s life such as peers, parents and teachers52. Evidence suggests this approach offers greater efficacy than conventional strategies for promoting mental health and preventing risk behaviours53,54. Building on this foundation, peer-led interventions require unique considerations such as utilising standardised peer leader selection criteria, comprehensive training protocols addressing both content and leadership development, and flexible implementation guidelines that maintain program fidelity while adapting to diverse school contexts55. Establishing robust monitoring systems will be essential to assess immediate outcomes, long-term sustainability, and cost-effectiveness of these interventions.
Conclusion
This systematic review indicates peer-led lifestyle interventions had limited effectiveness for improving adolescent mental health outcomes in school settings. Meta-analyses revealed non-significant effects across all mental health outcomes. These findings highlight several priorities for future research: the need for high-quality studies with robust methodological designs, standardisation of measurement approaches, and careful consideration of intervention characteristics including dose and delivery format. Given the potential of peer-led approaches to promote both physical and mental health in school settings, future research should focus on identifying effective implementation strategies and developing sustainable programs that can be integrated into existing school structures. Particular attention should be paid to comprehensive evaluation of both immediate and long-term outcomes to better understand the potential of these interventions for supporting adolescent mental health.
Data availability
Data extracted from included studies, including data used in all analyses, and R code used for analyses can be made available upon reasonable request to the corresponding author.
References
World Health Organization. Mental health of adolescents. https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health
Solmi, M. et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol. Psychiatry. 27, 281–295 (2022).
Patel, V., Flisher, A. J., Hetrick, S. & McGorry, P. Mental health of young people: a global public-health challenge. Lancet 369, 1302–1313 (2007).
Jokela, M., Ferrie, J. & Kivimäki, M. Childhood problem behaviors and death by midlife: the British National child development study. J. Am. Acad. Child. Adolesc. Psychiatry. 48, 19–24 (2009).
Post, R. M. et al. Early-Onset bipolar disorder and treatment delay are risk factors for poor outcome in adulthood. J. Clin. Psychiatry. 71, 5308 (2010).
Ford, T., Collishaw, S., Meltzer, H. & Goodman, R. A prospective study of childhood psychopathology: independent predictors of change over three years. Soc. Psychiatry Psychiatr Epidemiol. 42, 953–961 (2007).
Radez, J. et al. Why do children and adolescents (not) seek and access professional help for their mental health problems? A systematic review of quantitative and qualitative studies. Eur. Child. Adolesc. Psychiatry. 30, 183–211 (2021).
Merikangas, K. R. et al. Service utilization for lifetime mental disorders in U.S. Adolescents: results of the National comorbidity Survey–Adolescent supplement (NCS-A). J. Am. Acad. Child. Adolesc. Psychiatry. 50, 32–45 (2011).
McGorry, P. D. et al. The lancet psychiatry commission on youth mental health. Lancet Psychiatry. 11, 731–774 (2024).
Lawrence, D., Hancock, K. J. & Kisely, S. The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers. BMJ 346, 2539 (2013).
Carney, R. et al. The clinical and behavioral cardiometabolic risk of children and young people on mental health inpatient units: A systematic review and meta-analysis. Gen. Hosp. Psychiatry. 70, 80–97 (2021).
O’Neil, A. et al. Relationship between diet and mental health in children and adolescents: A systematic review. Am. J. Public. Health. 104, e31–e42 (2014).
Beauchamp, M. R., Puterman, E. & Lubans, D. R. Physical inactivity and mental health in late adolescence. JAMA Psychiatry. 75, 543–544 (2018).
Short, C. E. et al. Physical activity recommendations from general practitioners in Australia. Results from a National survey. Aust N Z. J. Public. Health. 40, 83–90 (2016).
Singh, B. et al. Effectiveness of physical activity interventions for improving depression, anxiety and distress: an overview of systematic reviews. Br. J. Sports Med. 57, 1203–1209 (2023).
Firth, J. et al. The effects of dietary improvement on symptoms of depression and anxiety: A Meta-Analysis of randomized controlled trials. Psychosom. Med. 81, 265 (2019).
Firth, J. et al. A meta-review of lifestyle psychiatry: the role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry. 19, 360–380 (2020).
Carney, R. & Firth, J. Exercise interventions in child and adolescent mental health care: an overview of the evidence and recommendations for implementation. JCPP Adv. 1, e12031 (2021).
Khalid, S., Williams, C. M. & Reynolds, S. A. Is there an association between diet and depression in children and adolescents? A systematic review. Br. J. Nutr. 116, 2097–2108 (2016).
Alvaro, P. K., Roberts, R. M. & Harris, J. K. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep 36, 1059–1068 (2013).
Lam, L. T. & Lam, M. K. Sleep disorders in early childhood and the development of mental health problems in adolescents: A systematic review of longitudinal and prospective studies. Int. J. Environ. Res. Public. Health. 18, 11782 (2021).
Patel, V., Saxena, S., Frankish, H. & Boyce, N. Sustainable development and global mental health—a lancet commission. Lancet 387, 1143–1145 (2016).
Dodd, S. et al. School-based peer education interventions to improve health: a global systematic review of effectiveness. BMC Public. Health. 22, 2247 (2022).
Blakemore, S. J. & Robbins, T. W. Decision-making in the adolescent brain. Nat. Neurosci. 15, 1184–1191 (2012).
Lynch, L., Moorhead, A., Long, M. & Hawthorne-Steele, I. The role of informal sources of help in young People’s access to, engagement with, and maintenance in professional mental health Care—A scoping review. J. Child. Fam Stud. 32, 3350–3365 (2023).
Collier, P. J. Developing Effective Student Peer Mentoring Programs: A Practitioner’s Guide To Program Design, Delivery, Evaluation, and Training (Taylor & Francis, 2023).
King, T. & Fazel, M. Examining the mental health outcomes of school-based peer-led interventions on young people: A scoping review of range and a systematic review of effectiveness. PLOS ONE. 16, e0249553 (2021).
Vangeepuram, N., Angeles, J., Lopez-Belin, P., Arniella, G. & Horowitz, C. R. Youth peer led lifestyle modification interventions: A narrative literature review. Eval Program. Plann. 83, 101871 (2020).
Lavelle, M. A., Knopp, M., Gunther, C. W. & Hopkins, L. C. Youth and peer mentor led interventions to improve Biometric-, nutrition, physical activity, and Psychosocial-Related outcomes in children and adolescents: A systematic review. Nutrients 15, 2658 (2023).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, n71 (2021).
Higgins, J. P., Savović, J., Page, M. J., Elbers, R. G. & Sterne, J. A. Assessing risk of bias in a randomized trial. in Cochrane Handbook for Systematic Reviews of Interventions 205–228 (John Wiley & Sons, Ltd, (2019). https://doi.org/10.1002/9781119536604.ch8
Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front. Psychol. 4, 863 (2013).
Hozo, S. P., Djulbegovic, B. & Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 5, 13 (2005).
Sullivan, G. M. & Feinn, R. Using effect Size—or why the P value is not enough. J. Grad Med. Educ. 4, 279 (2012).
Jakobsen, J. C., Wetterslev, J., Winkel, P., Lange, T. & Gluud, C. Thresholds for statistical and clinical significance in systematic reviews with meta-analytic methods. BMC Med. Res. Methodol. 14, 120 (2014).
Popay, J. et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews: A Product from the ESRC Methods Programme. (2006). https://doi.org/10.13140/2.1.1018.4643
Corder, K., Brown, H. E., Schiff, A. & van Sluijs, E. M. F. Feasibility study and pilot cluster-randomised controlled trial of the goactive intervention aiming to promote physical activity among adolescents: outcomes and lessons learnt. BMJ Open. 6, e012335 (2016).
Murphy, M. H. et al. Effectiveness of the walking in schools (WISH) study, a peer-led walking intervention for adolescent girls: results of a cluster randomised controlled trial. Int. J. Behav. Nutr. Phys. Act. 21, 19 (2024).
Carlin, A., Murphy, M. H., Nevill, A. & Gallagher, A. M. Effects of a peer-led walking in schools intervention (the WISH study) on physical activity levels of adolescent girls: a cluster randomised pilot study. Trials 19, 31 (2018).
Thompson, M. A. & Nigg, C. R. Effect of an adolescent peer-led health curriculum on peer educators and participants. Health Educ. J. 80, 337–350 (2021).
Forneris, T. et al. Results of a rural School-Based Peer-Led intervention for youth: goals for health. J. Sch. Health. 80, 57–65 (2010).
Åvitsland, A. et al. Effects of school-based physical activity interventions on mental health in adolescents: the school in motion cluster randomized controlled trial. Ment Health Phys. Act. 19, 100348 (2020).
Tymms, P. B. et al. Clustered randomised controlled trial of two education interventions designed to increase physical activity and well-being of secondary school students: the MOVE project. BMJ Open. 6, e009318 (2016).
Andermo, S. et al. School-related physical activity interventions and mental health among children: a systematic review and meta-analysis. Sports Med. - Open. 6, 25 (2020).
Cataldo, R., John, J., Chandran, L., Pati, S. & Shroyer, A. L. W. Impact of Physical Activity Intervention Programs on Self-Efficacy in Youths: A Systematic Review. ISRN Obes. 586497 (2013). (2013).
Salmon, J., Brown, H. & Hume, C. Effects of strategies to promote children’s physical activity on potential mediators. Int. J. Obes. 33, S66–S73 (2009).
Compas, B. E. et al. Coping, emotion regulation, and psychopathology in childhood and adolescence: A meta-analysis and narrative review. Psychol. Bull. 143, 939–991 (2017).
Sahi, R. S., Eisenberger, N. I. & Silvers, J. A. Peer facilitation of emotion regulation in adolescence. Dev. Cogn. Neurosci. 62, 101262 (2023).
McHale, F. et al. A systematic literature review of Peer-led strategies for promoting physical activity levels of adolescents. Health Educ. Behav. 49, 41–53 (2022).
Lopresti, A. L., Hood, S. D. & Drummond, P. D. A review of lifestyle factors that contribute to important pathways associated with major depression: diet, sleep and exercise. J. Affect. Disord. 148, 12–27 (2013).
Bourke, M. et al. Clusters of healthy lifestyle behaviours are associated with symptoms of depression, anxiety, and psychological distress: A systematic review and meta-analysis of observational studies. Clin. Psychol. Rev. 118, 102585 (2025).
Langford, R. et al. The world health organization’s health promoting schools framework: a Cochrane systematic review and meta-analysis. BMC Public. Health. 15, 130 (2015).
Implementing Mental Health Promotion (Springer International Publishing, 2019). https://doi.org/10.1007/978-3-030-23455-3.
Goldberg, J. M. et al. Effectiveness of interventions adopting a whole school approach to enhancing social and emotional development: a meta-analysis. Eur. J. Psychol. Educ. 34, 755–782 (2019).
Lekamge, R. B. et al. Systematic review and Meta-analysis of the effectiveness of Whole-school interventions promoting mental health and preventing risk behaviours in adolescence. J. Youth Adolesc. 54, 271–289 (2025).
Funding
This project received no specific funding. CM receives an Investigator Grant from the Medical Research Future Fund (1193862).
Author information
Authors and Affiliations
Contributions
J.B., C.M. and P.B. conceptualized the study. J.B. completed database searching. J.B., M.S., R.C., C.S., E.E., E.T., M.B., B.J. and G.G completed article screening and data extraction. J.B. and C.S. completed critical appraisal. All authors contributed to conflict resolution during screening. J.B. was responsible for data curation and analysis. J.B. and C.M. contributed to data interpretation. J.B. and M.S. wrote the original draft. C.M. and P.B. provided senior advice. All authors contributed to reviewing and editing of the final manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Disclaimer
PB is a staff member of the World Health Organization. The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the decisions, policy, or views of the World Health Organization.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Brinsley, J., Schmidt, M., Curtis, R. et al. Effectiveness of peer-led health behaviour interventions on adolescent’s mental health and wellbeing: a systematic review and meta-analysis. Sci Rep 15, 16480 (2025). https://doi.org/10.1038/s41598-025-01053-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01053-8