Abstract
Enhanced Recovery After Surgery (ERAS) principles have been increasingly applied in various surgical disciplines to optimize patient outcomes and reduce recovery times. However, evidence regarding the application of ERAS-based nursing interventions in lumbar disc herniation (LDH) management remains limited. This study aimed to evaluate the efficacy of ERAS-based nursing interventions in improving recovery outcomes for patients undergoing surgical treatment for LDH. A total of 345 patients diagnosed with LDH and undergoing surgical treatment between February 2022 and February 2023 were retrospectively analyzed. Patients were divided into two groups: 174 received ERAS-based nursing interventions, while 171 received standard care. ERAS interventions included preoperative education, multimodal pain management, early mobilization, and psychological support. Clinical outcomes, including postoperative pain measured by the Visual Analog Scale (VAS), length of hospital stay (LOS), complication rates, and patient satisfaction, were assessed. Recovery milestones, such as time to ambulation and return to daily activities, were also analyzed.The ERAS group demonstrated significantly better outcomes compared to the standard care group. Postoperative VAS scores were lower in the ERAS group at 24 h (3.7 ± 1.2 vs. 5.1 ± 1.4, P < 0.001) and 48 h (2.8 ± 0.9 vs. 4.3 ± 1.2, P < 0.001). The ERAS group also had a shorter LOS (5.3 ± 1.7 days vs. 7.1 ± 2.2 days, P < 0.001), fewer complications (6.9% vs. 12.3%, P = 0.037), and higher patient satisfaction (92.6% vs. 78.9%, P < 0.001). Recovery milestones, including time to ambulation (18.5 ± 4.6 h vs. 30.2 ± 5.9 h, P < 0.001) and return to daily activities (7.4 ± 1.5 days vs. 10.2 ± 2.1 days, P < 0.001), were achieved earlier in the ERAS group. ERAS-based nursing interventions significantly improve recovery outcomes for patients undergoing surgical treatment for lumbar disc herniation. These findings highlight the importance of integrating ERAS principles into perioperative nursing care to enhance patient recovery and satisfaction.
Similar content being viewed by others
Introduction
Lumbar disc herniation (LDH) is a common degenerative condition of the spine, resulting from the displacement of intervertebral disc material, which compresses spinal nerve roots and causes significant pain, functional limitations, and impaired quality of life1,2,3,4. For patients with severe or persistent symptoms, surgical interventions, such as microdiscectomy or laminectomy, are often performed to relieve nerve compression and restore mobility5. However, the postoperative period poses challenges, including persistent wound pain, delayed functional recovery, and variability in patient satisfaction, which necessitate optimized perioperative care strategies6,7.
Enhanced Recovery After Surgery (ERAS) principles, initially developed for colorectal surgery, have emerged as a transformative approach in perioperative care across multiple surgical specialties8,9. These principles emphasize a multidisciplinary and patient-centered approach, integrating interventions such as preoperative education, multimodal analgesia, early mobilization, and individualized rehabilitation plans to minimize surgical stress, accelerate recovery, and improve patient outcomes10,11. The application of ERAS protocols in spinal surgery has shown promising results. For example, Dietz et al.12., through a meta-analysis, found that ERAS in spinal surgery can reduce complications, readmissions, length of stay, and opioid use, while improving patient-reported outcomes and functional recovery. Similarly, Wang et al.13., through a retrospective study, demonstrated that ERAS protocols are safe and associated with additional benefits for elderly patients undergoing anterior cervical discectomy and fusion.
In orthopedic and spinal surgery, preoperative and postoperative nursing interventions play a critical role in the successful implementation of ERAS principles. Effective nursing care not only facilitates early mobilization and patient adherence to recovery plans but also addresses challenges such as pain management and patient education. Previous studies have shown that individualized nursing strategies improve recovery outcomes in orthopedic procedures14. However, limited research has focused on the role of ERAS-based nursing interventions in managing patients undergoing surgery for lumbar disc herniation. Inconsistent nursing practices and the lack of standardized ERAS protocols in spinal surgery further underscore the need for robust evidence to guide clinical implementation15,16,17,18.
This study aims to evaluate the impact of ERAS-based nursing interventions on postoperative outcomes in patients undergoing surgery for lumbar disc herniation. By analyzing key recovery metrics, such as pain levels, functional milestones, length of hospital stay, and patient satisfaction, this research seeks to provide evidence-based insights into optimizing nursing care for this patient population. Additionally, this study aims to address the current gap in standardized nursing protocols tailored for spinal surgery, particularly for LDH patients, thereby contributing to the advancement of perioperative care in this field.
Materials and methods
Patient selection study design and participants
This retrospective cohort study aimed to evaluate the impact of nursing interventions based on Enhanced Recovery After Surgery (ERAS) principles on postoperative outcomes in patients undergoing lumbar disc herniation (LDH) surgery. Data were collected from adult patients (18 years or older) who underwent lumbar discectomy or laminectomy for LDH between February 2022 and February 2023.Inclusion Criteria: (1) Patients aged ≥ 18 years; (2) A confirmed diagnosis of lumbar disc herniation with corresponding clinical symptoms requiring surgical intervention; (3)Complete clinical data availability and adherence to follow-up assessments. Exclusion Criteria: (1) Patients undergoing revision surgery for LDH; (2) Significant comorbidities that could influence recovery outcomes (e.g., severe cardiovascular or neurological diseases); (3) Concurrent spinal conditions such as scoliosis or spinal stenosis requiring separate surgical management; (4) Refusal to follow postoperative care protocols or incomplete data records. The study was conducted in compliance with the Declaration of Helsinki and received approval from the Ethics Committee of Dazhou Central Hospital. All participants provided written informed consent prior to inclusion.
Surgical team
Surgeries were performed by a team of three experienced spine surgeons, each with at least 10 years of experience in performing lumbar discectomy procedures. All surgeries followed a standardized technique, ensuring consistency across cases. The surgical procedures were carried out under general anesthesia with the same protocol for all patients.
ERAS-Based perioperative nursing interventions
Patients in the ERAS group received a comprehensive range of nursing interventions aligned with Enhanced Recovery After Surgery (ERAS) principles. These interventions focused on optimizing perioperative care through evidence-based strategies. Preoperative education played a central role, with structured sessions designed to inform patients and their families about surgical procedures, postoperative expectations, and recovery goals. This education emphasized pain management techniques, the benefits of early mobilization, and potential complications, ensuring patients were well-prepared both physically and psychologically.
Intraoperatively, fluid management and patient monitoring were individualized to maintain hemodynamic stability and prevent complications. Postoperative care emphasized multimodal pain management, combining non-opioid analgesics with regional anesthesia to minimize reliance on opioids. Early mobilization was another cornerstone, initiated within 24 h post-surgery, with patients guided through progressive mobility exercises tailored to their abilities. Nutritional support, focused on early oral intake of protein-rich, easily digestible meals, was provided to enhance recovery and support wound healing. Nurses also conducted regular assessments to proactively identify and address potential complications, such as deep vein thrombosis (DVT) or infections, using standardized prevention protocols and interventions.
Implementation of ERAS protocol
The ERAS protocol was implemented with strong support from our hospital’s leadership and a multidisciplinary team, including surgeons, anesthesiologists, nursing staff, and physical therapists. The team worked collaboratively to adapt the ERAS guidelines to our institution’s practice, ensuring that key elements such as early mobilization, multimodal analgesia, and nutrition support were tailored to meet the needs of lumbar disc herniation (LDH) patients. Our experience in implementing ERAS involved a comprehensive training program for staff and patient education to enhance adherence to the protocol and promote its benefits.
Standard care
Patients receiving standard care were managed with conventional nursing protocols typically applied in clinical settings. Preoperative education was limited to basic instructions provided shortly before surgery, focusing on fasting requirements and hygiene practices, with minimal emphasis on postoperative expectations or rehabilitation. Pain management relied predominantly on opioid-based medications, administered as needed, with less incorporation of multimodal strategies. Mobilization efforts typically began later, often on the second or third postoperative day, and involved basic walking or passive exercises without individualized plans. Nutritional advice was general, with oral intake often delayed until full bowel function returned. Routine monitoring was conducted, but advanced assessments for potential complications, such as DVT or respiratory issues, were not systematically performed. The standard care approach, while effective for basic needs, lacked the proactive and holistic strategies integral to ERAS protocols.
The decision to assign patients to either the ERAS protocol or standard care was made collaboratively between the medical team, the patients, and their families. After discussing the treatment options, including the benefits and potential risks of each approach, patients and their families made an informed decision about their care pathway. Efforts were made to ensure comparability between the two groups by matching key baseline characteristics such as age, comorbidities, and preoperative pain levels. Patients who were clinically stable and met specific criteria for early mobilization and multimodal pain management were offered the ERAS pathway. Those who did not meet these criteria or were treated before the protocol was introduced were assigned to standard care. Standard care in our clinic involved a more traditional, less structured approach to postoperative care, which still incorporated some principles of multimodal analgesia and early mobilization, but lacked the more formalized and coordinated approach of the ERAS protocol. This patient-centered approach allowed for greater involvement of patients and their families in the decision-making process. To provide a clearer comparison of nursing interventions between the two groups, we have included Supplementary Table 1, which outlines the key components of ERAS-based nursing interventions versus standard care. This structured comparison highlights the significant differences in preoperative education, pain management, mobilization strategies, nutritional support, psychological assistance, and complication prevention.
Outcome Measures-Primary outcomes
The primary outcomes of this study included postoperative pain scores, measured using the Visual Analog Scale (VAS) at 24 h, 48 h, and 7 days post-surgery, as well as the length of hospital stay and patient satisfaction scores. Pain assessments were conducted by trained nursing staff to ensure consistency and reliability. Hospital stay duration was recorded from the day of surgery to the day of discharge, and satisfaction was evaluated through structured questionnaires administered before discharge, focusing on pain management, recovery experience, and overall care quality. These measures were chosen to reflect the immediate effectiveness of ERAS-based nursing interventions in improving patient outcomes.
Secondary outcomes
Secondary outcomes were designed to provide a comprehensive evaluation of recovery and included readmission rates within 30 days, postoperative complication rates, and recovery milestones, such as the time to first ambulation and time to achieve independent walking. Complications were categorized into common postoperative issues, including wound infections, deep vein thrombosis, and gastrointestinal dysfunctions, and were verified through clinical evaluations and patient records. Recovery milestones were assessed based on daily observations by the clinical team, with a focus on functional mobility and independence in basic activities. These secondary outcomes aimed to capture the broader impact of ERAS-based interventions on both clinical recovery and patient functionality. Postoperative complications were systematically monitored using standardized clinical definitions. Infection rates were assessed based on Centers for Disease Control and Prevention (CDC) criteria for surgical site infections, while deep vein thrombosis (DVT) was diagnosed using Doppler ultrasound and clinical assessment guidelines. Urinary retention was defined according to post-void residual volume criteria. These standardized definitions ensured consistency and reliability in identifying postoperative complications.
Data collection
Clinical data were extracted from electronic medical records and validated independently by two researchers to ensure accuracy. Pain levels, hospital stay durations, and complication rates were recorded for all participants. Follow-up assessments were conducted at 1, 2, and 4 weeks post-surgery.
Sample size calculation
The sample size for this study was calculated using statistical tools available online (https://www.naukowiec.org/dobor.html; accessed December 31, 2022). Assuming a relative error rate of 7% (the level used in meta-analysis studies), we determined that a sample size of 165 patients would provide sufficient statistical power to detect significant differences in primary outcomes, with a significance level of p < 0.05. This sample size was selected to ensure adequate representation and robust results across both the ERAS and standard care groups.
Statistical analysis
Descriptive statistics summarized patient characteristics and clinical outcomes. Continuous variables, such as VAS scores and hospital stay duration, were analyzed using t-tests or Mann-Whitney U tests, depending on data distribution. Categorical variables, such as complication rates and readmission rates, were compared using chi-square or Fisher’s exact tests. To ensure that the observed differences between the ERAS and standard care groups were not influenced by baseline imbalances, we performed multivariable logistic regression analysis to adjust for important variables, including demographic characteristics (age, gender) and clinical factors (such as body mass index (BMI), preoperative Visual Analog Scale (VAS) pain scores, and comorbidities like diabetes and hypertension). Additionally, Analysis of Covariance (ANCOVA) was conducted to further control for these variables when comparing postoperative outcomes such as pain levels, length of hospital stay, and recovery milestones. All statistical results presented in this study reflect these adjustments. These adjustments helped to ensure that the observed effects of ERAS-based nursing interventions were not confounded by these factors. Statistical significance was set at P < 0.05. Analyses were conducted using SPSS 25.0 (IBM, Armonk, NY, USA), and data visualizations were generated using R 4.0.5 and GraphPad Prism 8.0.
To address missing data, we employed listwise deletion, excluding cases with incomplete records for key variables such as pain scores, length of hospital stay, and recovery milestones. No imputation methods were applied, as the amount of missing data was minimal and did not significantly affect the results. This approach ensured that our analysis was based on complete data for all key variables.
Results
Baseline characteristics of patients
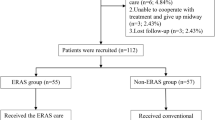
The inclusion and exclusion criteria are detailed in Fig. 1. A total of 345 patients with lumbar disc herniation (LDH) were included in the study, with 174 patients receiving ERAS-based nursing interventions and 171 patients receiving standard care. The two groups were comparable in terms of demographic and clinical characteristics, including age, gender, body mass index (BMI), smoking history, comorbidities such as diabetes and hypertension, and the severity of LDH (P > 0.05). Additionally, no significant differences were observed in physical activity levels, preoperative use of analgesics, or the number of affected levels between the groups (Table 1). These findings ensured a balanced comparison of the groups.
Postoperative complications
The incidence of postoperative complications was significantly lower in the ERAS group compared to the standard care group. Wound infection rates were reduced (1.1% vs. 5.3%, P = 0.016), as were delayed wound healing (0.6% vs. 4.1%, P = 0.009) and urinary retention (1.7% vs. 4.7%, P = 0.042). Other complications, such as deep vein thrombosis, respiratory complications, and neurological deficits, showed no significant differences between the groups (P > 0.05). Notably, fewer patients in the ERAS group required readmission due to pain-related issues (2.3% vs. 5.8%, P = 0.072), though this result did not reach statistical significance (Table 2).
Recovery milestones and hospital stay
Patients in the ERAS group demonstrated faster recovery milestones compared to those in the standard care group. The time to first ambulation was significantly shorter in the ERAS group (18.3 ± 5.1 h vs. 28.6 ± 7.4 h, P < 0.001), as was the time to independent walking (2.9 ± 0.8 days vs. 4.5 ± 1.3 days, P < 0.001). The length of hospital stay was also markedly reduced (3.8 ± 1.2 days vs. 5.3 ± 1.7 days, P < 0.001). ERAS patients resumed daily activities earlier (7.2 ± 1.6 days vs. 10.1 ± 2.4 days, P < 0.001) and returned to work or normal routines faster (14.7 ± 3.5 days vs. 19.2 ± 4.8 days, P < 0.001). Additionally, a higher proportion of patients in the ERAS group achieved early discharge (66.1% vs. 39.8%, P < 0.001) (Table 3).
Pain management and patient satisfaction
Pain levels, as measured by the Visual Analog Scale (VAS), were significantly lower in the ERAS group at all time points: 24 h (4.1 ± 1.3 vs. 5.5 ± 1.5, P < 0.001), 48 h (3.2 ± 1.1 vs. 4.6 ± 1.4, P < 0.001), and 7 days (2.1 ± 0.9 vs. 3.8 ± 1.2, P < 0.001). The proportion of patients with minimal pain (VAS < 3) at 7 days was higher in the ERAS group (79.9% vs. 57.3%, P < 0.001). Patient satisfaction was also significantly improved, with higher overall satisfaction scores (91.6 ± 8.4 vs. 77.9 ± 9.6, P < 0.001) and satisfaction with nursing care (93.7% vs. 80.7%, P < 0.001) in the ERAS group (Table 4).
Quality of life and functional recovery
Patients in the ERAS group reported better quality of life and functional recovery outcomes. The SF-36 physical component scores (72.8 ± 10.4 vs. 66.2 ± 11.3, P < 0.001) and mental component scores (74.3 ± 9.6 vs. 69.1 ± 10.1, P < 0.001) were significantly higher in the ERAS group. Similarly, the EQ-5D index favored the ERAS group (0.85 ± 0.05 vs. 0.78 ± 0.06, P = 0.018). A greater proportion of ERAS patients achieved full recovery in activities of daily living (89.7% vs. 76.6%, P = 0.006) and returned to work or daily activities within the follow-up period (83.3% vs. 71.3%, P = 0.024). Functional independence scores were higher in the ERAS group (91.4 ± 8.7 vs. 81.6 ± 9.4, P < 0.001), along with greater improvements in emotional well-being (93.1% vs. 78.9%, P < 0.001) and fatigue reduction (8.1 ± 1.2 vs. 6.4 ± 1.5, P < 0.001) (Table 5).
Discussion
Lumbar disc herniation (LDH) surgery is a common intervention aimed at alleviating pain and restoring function in patients with significant neurological symptoms19,20. However, optimizing postoperative recovery remains a challenge, particularly in managing wound pain and functional rehabilitation. This study demonstrates that nursing interventions based on Enhanced Recovery After Surgery (ERAS) principles significantly improve postoperative outcomes, including reduced pain levels, faster recovery milestones, and enhanced patient satisfaction compared to standard care. These findings align with the growing body of evidence supporting the application of ERAS protocols across various surgical specialties.
One of the key findings of this study is the significant reduction in postoperative pain in the ERAS group, as measured by lower Visual Analog Scale (VAS) scores at 24 h, 48 h, and 7 days post-surgery. Multimodal analgesia, a core component of the ERAS protocol, likely contributed to this improvement by minimizing reliance on opioids while providing effective pain relief. Similar benefits of ERAS-based pain management have also been reported in spinal surgery. Wainwright et al.21. highlighted that utilizing evidence-based practices and enhancing ERAS pathways to optimize clinical procedures can enable faster recovery, reduce morbidity, alleviate pain, and improve long-term outcomes for patients undergoing major spinal surgeries. The reduced pain levels observed in our study also facilitated early mobilization, an essential factor in preventing complications such as deep vein thrombosis (DVT) and delayed wound healing. Another important outcome of this study is the shorter length of hospital stay in the ERAS group22,23. Patients in this group achieved functional recovery milestones, such as first ambulation and independent walking, significantly earlier than those in the standard care group. Early mobilization and structured rehabilitation programs, integral to the ERAS pathway, were instrumental in expediting recovery. These findings are consistent with those of Dietz et al.3., who demonstrated that ERAS protocols significantly reduce hospital stay duration and enhance functional recovery in orthopedic and spinal surgeries. Shorter hospital stays not only alleviate the psychological and emotional burden on patients and their families but also contribute to reduced healthcare costs.
Recent studies have demonstrated the benefits of ERAS protocols in lumbar disc procedures, showing improvements in postoperative recovery, reduced hospital stays, and lower complication rates. Debono et al.11. provided ERAS guidelines for lumbar spinal fusion, emphasizing the importance of multimodal analgesia, early mobilization, and patient education, which align with our findings. Similarly, Smith et al.24. reported that implementing ERAS in lumbar spine fusion surgery led to improved patient satisfaction and faster recovery. Wang et al.25. further developed an ERAS approach for lumbar spinal fusion, which optimized anesthesia, early ambulation, and opioid-sparing analgesia to improve postoperative outcomes. A systematic review by Zaed et al.26. on ERAS in spinal surgeries found that ERAS protocols significantly improve postoperative pain control and reduce complication rates, further supporting the clinical relevance of our results. Our study extends this evidence by demonstrating that ERAS-based interventions for lumbar disc herniation surgery not only reduce hospital stays and expedite recovery milestones but may also contribute to long-term functional benefits. These findings underscore the potential of ERAS to enhance both short-term and long-term outcomes in spinal surgery.
Complication rates were also notably lower in the ERAS group, with significant reductions in wound infections, urinary retention, and delayed wound healing. These outcomes emphasize the effectiveness of proactive monitoring and prevention strategies embedded within the ERAS framework. For example, Frassanito et al.27. reported similar reductions in complications with the implementation of ERAS in orthopedic procedures, attributing the improvement to comprehensive patient management and early intervention protocols. Patient satisfaction and quality of life metrics further highlight the benefits of ERAS-based nursing interventions. Higher scores in both the physical and mental components of the Short Form-36 (SF-36) survey, as well as the EuroQol-5D index (EQ-5D), indicate that patients in the ERAS group experienced a more positive recovery trajectory. Additionally, a larger proportion of ERAS patients returned to work or resumed daily activities within the follow-up period. These findings underscore the holistic nature of ERAS protocols, which address not only clinical outcomes but also broader aspects of patient well-being. While the lower complication rates in the ERAS group were statistically significant, they also hold clinical relevance. Specifically, the reductions in infection rates, DVT, and urinary retention likely translated into meaningful patient benefits, including decreased need for antibiotics, reduced risks associated with prolonged immobilization, and enhanced overall recovery. Fewer complications may also contribute to improved patient satisfaction, lower healthcare costs, and reduced risk of readmission. The use of standardized definitions to monitor complications further strengthens the validity of our findings. These results highlight the potential of ERAS-based nursing interventions in not only accelerating recovery but also improving perioperative safety and reducing preventable postoperative morbidities.
The length of hospital stay (LOS) in our study, particularly in the standard care group, was longer compared to international practices, where lumbar discectomy is commonly performed as an outpatient procedure (USA) or with next-day discharge (Europe). This difference can be attributed to several factors, including institutional protocols that required a minimum inpatient observation period to monitor pain control, neurological function, and early rehabilitation progress before discharge. Additionally, patient and physician preferences influenced LOS, as some patients and families preferred a longer hospital stay for postoperative reassurance, and physicians were generally more cautious, particularly in older patients or those with comorbidities. Furthermore, healthcare system differences, such as hospital reimbursement structures and discharge policies, historically favored longer inpatient stays compared to fast-track recovery models seen in other regions. Despite these differences, our findings reinforce the benefits of the ERAS protocol, which significantly reduced LOS by promoting early mobilization, multimodal pain management, and structured discharge planning. Future efforts should focus on further optimizing fast-track recovery protocols within our institution while ensuring patient safety and satisfaction.
While our study demonstrates significant short-term benefits of ERAS-based nursing interventions in pain management, recovery milestones, and hospital stay duration, it is important to consider their clinical relevance, particularly in terms of long-term functional outcomes. Although we did not directly measure long-term functional recovery or quality of life beyond 30 days, the significant reduction in pain scores and faster recovery milestones suggest that ERAS interventions could positively impact patients’ ability to return to work and daily activities. Moreover, shorter hospital stays and lower pain levels are likely to reduce the risk of postoperative complications, enhance overall functional capacity, and improve quality of life. Previous research supports the notion that early postoperative recovery, such as that facilitated by ERAS protocols, can contribute to improved long-term outcomes, including greater functional independence, reduced readmission rates, and better overall well-being28,29. However, the lack of extended follow-up in our study limits our ability to confirm these effects. Future research with longer follow-up periods is needed to evaluate the sustained benefits of ERAS interventions on functional recovery and quality of life in spinal surgery. These findings suggest that the improvements observed in our study may have meaningful implications for the long-term health and functional recovery of patients undergoing lumbar disc herniation surgery. Despite these promising results, this study has limitations. The retrospective design limits the ability to establish causal relationships between ERAS interventions and observed outcomes. Furthermore, the study was conducted at a single institution, which may affect the generalizability of the findings. Future research should focus on multicenter, prospective studies to validate these results and explore their applicability across diverse healthcare settings. We acknowledge the inherent limitations of our retrospective design, including potential selection bias and confounding factors due to non-randomized treatment allocation. To mitigate these, we applied multivariable regression analysis to adjust for key variables such as age, gender, and comorbidities like diabetes and hypertension. While we did not use propensity score matching, we believe the multivariable adjustments provided a robust method to control for confounders. Additionally, variations in patient demographics, such as age, gender, and comorbidities, may influence the effectiveness of ERAS interventions. Future prospective or randomized controlled trials involving larger and more diverse populations are needed to further validate these findings, refine ERAS protocols, and minimize bias, ultimately enhancing their applicability in spinal surgery.
Standardized protocols for implementing ERAS-based nursing interventions remain a critical need. Variability in nursing practices can undermine the effectiveness of ERAS strategies, leading to inconsistent patient outcomes. Developing evidence-based guidelines will ensure that ERAS principles are consistently applied, further optimizing recovery and improving patient satisfaction.
Conclusion
In conclusion, this study highlights the efficacy of ERAS-based nursing interventions in improving postoperative outcomes for patients undergoing lumbar disc herniation surgery. These interventions significantly reduce postoperative pain, shorten hospital stays, and enhance patient satisfaction and quality of life. By integrating strategies such as multimodal analgesia, early mobilization, and structured patient education, ERAS-based care provides a comprehensive approach to optimizing recovery. These findings support the broader adoption of ERAS principles in spinal surgery and emphasize the importance of developing standardized nursing protocols to ensure effective implementation. Further research is needed to validate these findings and refine ERAS-based interventions for diverse patient populations.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Ashok, A. et al. The enhanced recovery after surgery (ERAS) protocol to promote recovery following esophageal cancer resection. Surg. Today. 50 (4), 323–334 (2020).
Ljungqvist, O. ERAS–enhanced recovery after surgery: moving evidence-based perioperative care to practice. JPEN J. Parenter. Enter. Nutr. 38 (5), 559–566 (2014).
Naftalovich, R., Singal, A. & Iskander, A. J. Enhanced recovery after surgery (ERAS) protocols for spine surgery - review of literature. Anaesthesiol. Intensive Ther. 54 (1), 71–79 (2022).
Wainwright, T. W. et al. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: enhanced recovery after surgery (ERAS(®)) society recommendations. Acta Orthop. 91 (1), 3–19 (2020).
Soffin, E. M. et al. Design and implementation of an enhanced recovery after surgery (ERAS) program for minimally invasive lumbar decompression spine surgery: initial experience. Spine 44 (9), E561–e570 (2019).
Barclay, K. L., Zhu, Y. Y. & Tacey, M. A. Nausea, vomiting and return of bowel function after colorectal surgery. ANZ J. Surg. 85 (11), 823–828 (2015).
Jiang, H. H., Jian, X. F., Shangguan, Y. F., Qing, J. & Chen, L. B. Effects of enhanced recovery after surgery in total knee arthroplasty for patients older than 65 years. Orthop. Surg. 11 (2), 229–235 (2019).
Catarci, M. et al. ERAS pathway in colorectal surgery: structured implementation program and high adherence for improved outcomes. Updates Surg. 73 (1), 123–137 (2021).
Forsmo, H. M. et al. Pre- and postoperative stoma education and guidance within an enhanced recovery after surgery (ERAS) programme reduces length of hospital stay in colorectal surgery. Int. J. Surg. (London England). 36 (Pt A), 121–126 (2016).
Brodersen, F., Wagner, J., Uzunoglu, F. G. & Petersen-Ewert, C. Impact of preoperative patient education on postoperative recovery in abdominal surgery: A systematic review. World J. Surg. 47 (4), 937–947 (2023).
Debono, B. et al. Consensus statement for perioperative care in lumbar spinal fusion: enhanced recovery after surgery (ERAS®) society recommendations. Spine Journal: Official J. North. Am. Spine Soc. 21 (5), 729–752 (2021).
Dietz, N. et al. Enhanced recovery after surgery (ERAS) for spine surgery: A systematic review. World Neurosurg. 130, 415–426 (2019).
Wang, P. et al. Enhanced recovery after surgery (ERAS) program for anterior cervical discectomy and fusion (ACDF) in patients over 60 years old. Clin. Interv. Aging. 18, 1619–1627 (2023).
Hass, S., Jaekel, C. & Nesbitt, B. Nursing strategies to reduce length of stay for persons undergoing total knee replacement: integrative review of key variables. J. Nurs. Care Qual. 30 (3), 283–288 (2015).
Robertson, S. C. Enhanced recovery after surgery (ERAS) spine pathways and the role of perioperative checklists. Adv. Tech. Stand. Neurosurg. 49, 73–94 (2024).
Soldozy, S. et al. Enhanced recovery after surgery in intramedullary and extramedullary spinal cord lesions: perioperative considerations and recommendations. Spinal Cord. 57 (9), 729–738 (2019).
Sobański, D. et al. A study of 179 patients with degenerative stenosis of the lumbosacral spine to evaluate differences in quality of life and disability outcomes at 12 months, between Conservative treatment and surgical decompression. Med. Sci. Monitor: Int. Med. J. Experimental Clin. Res. 29, e940213 (2023).
Staszkiewicz, R. et al. Assessment of quality of life, pain level and disability outcomes after lumbar discectomy. Sci. Rep. 13 (1), 6009 (2023).
Kögl, N., Petr, O., Löscher, W., Liljenqvist, U. & Thomé, C. Lumbar disc Herniation—the significance of symptom duration for the indication for surgery. Deutsches Arzteblatt Int. 121 (13), 440–448 (2024).
Zhang, A. S. et al. Lumbar disc herniation: diagnosis and management. Am. J. Med. 136 (7), 645–651 (2023).
Wainwright, T. W., Immins, T. & Middleton, R. G. Enhanced recovery after surgery (ERAS) and its applicability for major spine surgery. Best Pract. Res. Clin. Anaesthesiol. 30 (1), 91–102 (2016).
Noba, L. et al. Enhanced recovery after surgery (ERAS) reduces hospital costs and improve clinical outcomes in liver surgery: a systematic review and Meta-Analysis. J. Gastrointest. Surgery: Official J. Soc. Surg. Aliment. Tract. 24 (4), 918–932 (2020).
Zhou, B. et al. ERAS reduces postoperative hospital stay and complications after bariatric surgery: A retrospective cohort study. Medicine 100 (47), e27831 (2021).
Smith, J. et al. Enhanced recovery after surgery (ERAS) program for lumbar spine fusion. Perioperative Med. (London England). 8, 4 (2019).
Development of an Enhanced Recovery After. Surgery (ERAS) approach for lumbar spinal fusion. J. Neurosurg. Spine. 26 (4), 411–418 (2017).
Zaed, I. et al. Current state of benefits of enhanced recovery after surgery (ERAS) in spinal surgeries: A systematic review of the literature. Neuro-Chirurgie 68 (1), 61–68 (2022).
Frassanito, L. et al. Enhanced recovery after surgery (ERAS) in hip and knee replacement surgery: description of a multidisciplinary program to improve management of the patients undergoing major orthopedic surgery. Musculoskelet. Surg. 104 (1), 87–92 (2020).
Bogani, G. et al. Enhanced recovery after surgery (ERAS) in gynecology oncology. Eur. J. Surg. Oncology: J. Eur. Soc. Surg. Oncol. Br. Association Surg. Oncol. 47 (5), 952–959 (2021).
Sauro, K. M. et al. Enhanced recovery after surgery guidelines and hospital length of stay, readmission, complications, and mortality: A Meta-Analysis of randomized clinical trials. JAMA Netw. Open. 7 (6), e2417310 (2024).
Acknowledgements
Thanks to the nurses in the department for their help with the project.
Author information
Authors and Affiliations
Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participation
Written informed consent was obtained from all participants. This research was performed in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Dazhou Central Hospital.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yang, H., Yang, Q., Pu, M. et al. Efficacy of nursing interventions based on the enhanced recovery after surgery (ERAS) in patients with lumbar disc herniation. Sci Rep 15, 21947 (2025). https://doi.org/10.1038/s41598-025-01116-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01116-w