Abstract
This study compared the surgical performance of resident doctors and their supervising ophthalmic surgeons in trabeculotomy (LOT) ab externo using propensity score matching. We retrospectively analyzed surgical data on 248 eyes that underwent LOT ab externo at our hospital between April 2016 and December 2022. The procedures were performed by three full-time supervising ophthalmologists (≥ 5 years of experience) and 12 resident physicians (< 5 years of experience). Propensity score matching was used to adjust for significant variables identified through univariate analysis of five covariates: preoperative visual acuity, preoperative intraocular pressure [IOP], preoperative ophthalmoscopy score, presence of preoperative pseudophakia, and concomitant cataract surgery. Postoperative outcomes including IOP, eye drop scores, and complications, were evaluated at 3-month intervals up to 24 months. Survival curves showed no significant difference between the eyes operated by resident physicians and those by supervising ophthalmologists (P = 0.183). The median change in IOP (first quartile–third quartile) was also comparable between the two groups (P = 0.234). Furthermore, both groups had similar rates of anterior chamber hemorrhage and transient IOP elevation (P = 0.577 and 0.85, respectively). These findings suggest that resident physicians can achieve surgical outcomes and complication rates comparable to those of their supervising ophthalmic surgeons when performing LOT ab externo.
Similar content being viewed by others
Introduction
Glaucoma is a leading cause of irreversible visual field impairment, significantly impacting patients’ quality of life1,2. Lowering intraocular pressure (IOP) is crucial in the treatment of glaucoma3,4, with surgery being the treatment of choice for cases refractory to medication. Notably, outflow tract reconstruction is the cornerstone of glaucoma surgery, encompassing both intraocular and extraocular methods5. Intraocular glaucoma surgery, in particular, is often performed using minimally invasive glaucoma surgery (MIGS) techniques, including microhook, Kahook dual blade, and trabectome6. However, despite surgery being the preferred method of choice, the number of institutions actively performing trabeculotomy (LOT) ab externo is declining because of the complexity of the procedure. LOT ab externo is one of the classic glaucoma surgeries; however, its effectiveness has been demonstrated in numerous studies7,8. Since 2018, our hospital has adopted the Kahook dual blade technique as an alternative approach for MIGS. Our previous study demonstrated that incorporating sinusotomy during LOT ab externo leads to favorable outcomes in diurnal IOP variation9. Consequently, this technique frequently employed in our institution. Additionally, performing sinusotomy provides resident doctors with valuable experience in creating scleral flap, an important skill that enhances their training for subsequent trabeculectomy procedures10.
Regardless of familiarity, LOT ab externo requires proficiency in specific technical skills, particularly the precise dissection of Schlemm’s canal. Furthermore, there are limited reports comparing outcomes of LOT ab externo performed by supervising ophthalmologists versus resident physicians, especially with adjustment of background factors. This study aimed to evaluate and compare the surgical performance of resident doctors and their ophthalmic surgeon supervisors at our institution when performing LOT ab externo, using propensity score matching.
Methods
Of the 443 eyes that underwent LOT ab externo between April 2016 and December 2022 at our hospital, 248 eyes were included in this study. Of these, surgery for 95 eyes was performed by experienced ophthalmologists, whereas that for 153 was performed by residents. Exclusion criteria included eyes of the patients with the following characteristics: observation period < 3 months; IOP assessment by methods other than by Goldmann applanation tonometry; a history of intraocular surgery other than cataract surgery; intraoperative vitreous prolapse or other complications; age < 20 years; and a diagnosis of traumatic, neovascular glaucoma, or pediatric glaucoma.
The eye drop score was defined as one and two points for one component and a fixed-dose combination, respectively. Oral IOP-lowering medications were considered as one component with a score of one point. Best-corrected visual acuity measured immediately before surgery was used for visual acuity analysis and converted to logMAR visual acuity for statistical analysis. For assessment of preoperative visual fields using Humphrey visual field tests, cases with a mean deviation value ≥ − 6 dB were considered mild, those with mean values between − 6 and − 12 dB were moderate, between − 12 and − 20 dB were severe, and cases with < − 20 dB were designated as end-stage. The rotational range of the metal U-shaped probes (rotome; Nagata’s trabeculotomy probe, Inami, Tokyo, Japan) was determined by inserting the rotome into Schlemm’s canal and subsequently rotating it. However, in cases of improper insertion, there may be insufficient rotation for appropriate incision. In some cases, only one side of the rotome was rotated to complete the procedure. Operative time obtained from the surgical records was converted into minutes.
Glaucoma types were broadly classified as primary open-angle glaucoma, pseudoexfoliation glaucoma, secondary glaucoma (excluding pseudoexfoliation glaucoma), and ocular hypertension. Supervising ophthalmologists, defined as physicians with a board certification in ophthalmology (three physicians) were categorized as supervisors. In contrast, resident physicians without board certification (12 physicians) were categorized as residents. The experience of almost all residents was between 1 and 3 years. In Japan, ophthalmic board certification need a 5-year experience for ophthalmologist and some surgical experiences decided by Japanese ophthalmological society. The surgical data was stratified into two groups: supervisor group (LOTs performed by supervisor ophthalmologists) and resident group (LOTs performed by the resident physicians).
For postoperative assessment, IOP, and eye drop scores were evaluated at 1, 3, 6, 9, 12, 18, and 24 months postoperatively, calculating changes from baseline values to those at each examination point. Postoperative complications included anterior chamber hemorrhage > 1 mm and transient IOP elevation (Spike). Spike was defined as an increase in IOP of 10 mmHg or more from baseline within the first postoperative month. Survival analysis was also conducted, with death defined as two consecutive IOP reductions < 20% or a need for additional glaucoma surgery.
This study was approved by the Ethics Committee of Tenri Yorozu Consultation Center Hospital (Approval number: R23-10). The requirement for informed consent was waived because of the retrospective nature of the study and use of anonymized data. Details regarding the study design, target patients, data usage, and principal investigator are available on the official hospital website. This study adhered to the tenets of the Declaration of Helsinki for clinical research with human participants.
Surgical technique
The surgical technique for LOT ab externo involved creating a two-layered scleral flap. The first flap, measuring 4 mm × 4 mm, was dissected to expose a smaller flap within it, which provided access to the outer wall of Schlemm’s canal. Rotomes were then inserted into the upper and lower Schlemm’s canals and rotated into the anterior chamber to verify aqueous humor backflow. The second flap was removed, and sinusotomy was performed creating a 1-mm diameter hole in the first flap using a Kelly Descemet`s Membrane Punch® (Inami) at center of the first flap. Finally, the first flap was secured with two 10 − 0 nylon sutures, and the conjunctiva was closed with 8 − 0 Vicryl sutures to complete the procedure. Some patients presented with cataracts with glaucoma. In cases wherein LOT was performed alongside cataract surgery, patients were anesthetized using ophthalmic anesthesia (4% xylocaine), incisions were made at the 10 and 2 o’clock positions using a microvitreoretinal knife, and space was secured at the corner angle with purified sodium hyaluronate/sodium chondroitin sulfate (Viscoat 0.5; Alcon Japan Ltd, Toranomon, Minato-ku, Tokyo). Cataract surgery was performed through a 2.2-mm corneal incision, using phacoemulsification and in-the-bag intraocular lens.
Postoperatively, all patients received levofloxacin 1.5% and 0.1% betamethasone eye drops during hospitalization. Upon discharge, betamethasone was replaced with 0.1% fluorometholone eye drops for approximately 1 month. Bromfenac sodium hydrate was additionally administered to patients undergoing concurrent cataract surgery.
Study endpoints
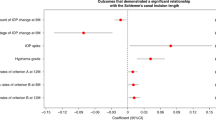
The primary endpoints were a comparison of survival rates between the supervisor and resident groups matched for background factors, investigation of factors related to survival rates, and a comparison of changes in IOP and eye drop scores from their baseline values to those at 12 months postoperatively. The secondary endpoints included comparisons of IOP and eye drop scores from baseline values to their corresponding values at each measurement point, incidence of anterior chamber hemorrhage and transient IOP elevation, and operative time.
Statistical analyses
The Mann–Whitney U test and Fisher’s exact test were performed for baseline analysis. Significant differences identified from these analyses were further examined using logistic regression, with relevant postoperative outcome factors as covariates. Propensity score matching was then performed for covariates determined to be significant. The Wilcoxon signed-rank sum test was employed to analyze matched continuous variables. Survival analysis was performed on the two matched groups to generate Kaplan–Meier curves, which were compared using the log-rank test. Statistical significance was defined as two-tailed P-values < 0.05. IBM SPSS Statistics Ver22.0 (IBM Ltd., Japan) and EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria), were used for statistical analysis. More precisely, the software is a modified version of R commander designed to add statistical functions frequently used in biostatistics.
Results
Patient background
No significant differences in age, sex, visual field impairment classification, glaucoma type, and rotome rotation range were observed between the supervising and resident groups (P = 0.506, 0.241, 0.053, 0.32, and 0.68, respectively) (Table 1). Significant differences in median preoperative IOP were noted, with a median IOP of 20 (17–26.8) mmHg in the supervisor group and 18 (15–21.5) mmHg in the resident group (P = 0.001). The median number of preoperative eye drop scores was 4 (3–4) in the supervisor group and 4 (3–5) in the resident group, which was significantly different (P = 0.005). The median preoperative visual acuity logarithm of the minimum angle of resolution (logMAR) values also showed significant differences (P = 0.02), with a logMAR of 0.097 (0–0.22) and 0.155 (0.045–0.3) in the supervisor and the resident groups, respectively. Similarly, significant differences were observed with preoperative pseudophakia use and concurrent cataract surgery (P = 0.003 and 0.013, respectively). In addition, operative times between the two groups were significantly different, with 22.9 ± 9.68 min in the supervisor group and 47.1 ± 16.4 min in the resident group (P < 0.001).
Propensity score matching
Propensity score matching was performed using preoperative data for IOP, eyeglass use, visual acuity, and pseudophakia use and concurrent cataract surgery as covariates, with the exception of operative time. After matching, no significant differences were observed in any of the baseline characteristics between the supervisor and resident groups (Table 2).
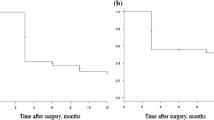
Survival curves after propensity matching
Comparison of survival curves after propensity matching revealed no significant differences between the two groups (P = 0.183) (Fig. 1).
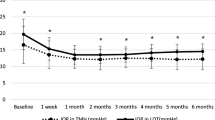
IOP and eye drop scores after propensity matching
Changes in IOP at 12 months postoperatively were comparable between the two groups after propensity matching, with a median change of 5 (2–8.5) mmHg in the resident group and 4 (0.92–9.25) mmHg in the supervisor group (P = 0.234) (Table 3). Moreover, changes in eye drop score at 12 months postoperatively showed no statistical significance (P = 0.656), with a change of 1 (0–2) point for both the supervisor and resident groups.
Postoperative complications
No significant differences were noted in the incidence of postoperative complications including anterior chamber hemorrhage and transient IOP elevation between the two groups after matching (P = 0.85 and 0.577, respectively).
Discussion
Baseline comparisons revealed that, compared with the resident group, the supervisor group performed LOT ab externo on eyes with significantly higher preoperative IOP and performed significantly fewer concurrent cataract surgeries. In contrast, the eyes operated on by the resident group had significantly higher preoperative eye drop use and better preoperative visual acuity compared with those in the supervisor group. These results suggest that the resident group more frequently performed combined surgeries for patients with coexisting cataract and glaucoma. Conversely, the supervisor group tended to operate upon patients with mild cataracts but significant visual field impairment, as evidenced by the significantly higher IOP in eyes treated by this group.
In the survival analysis, no significant differences were observed between the two groups after propensity score matching. Similarly, changes in IOP and eye drop scores at 12 months postoperatively showed no significant differences. These findings imply that surgical outcomes and complications rates were not significantly influenced by the level of surgeon experience.
While no previous studies have compared LOT ab externo outcomes between supervisor and resident groups, studies have examined outcomes of trabeculectomy resection performed by these groups. Lima et al.11 reported a significantly lower success rate for trabeculectomy resection performed by residents compared to that for the resection performed by supervisors. Conversely, Walkden et al.12 reported no significant difference in trabeculectomy resection performance between residents under supervision and their supervisors. These studies underscore the need for adequate training and supervision for residents when performing ophthalmologic surgical procedures. Furthermore, residents with no prior experience in performing trabeculectomy resections were reported to have poor suturing skills, which improved significantly following simulation-based training13. However, since most cataract surgeries are currently performed with phacoemulsification14, opportunities for residents to practice scleral flap creation and suturing have decreased. Since flap creation and suturing are essential for trabeculectomy, it is difficult to provide partial sutures to residents. However, the techniques involved in LOT ab externo, such as flap creation and suturing, are technically less demanding compared with those in trabeculectomy. Therefore, training in such surgical techniques may help residents to strengthen their surgical skills for future trabeculectomy procedures.
In the present study, no significant differences were observed in the rotational range of the rotome during LOT ab externo procedure between the supervisor and resident groups. In some cases, premature perforation can prevent bilateral rotome rotation. While research on LOT ab interno suggests no significant correlation between extent of incision and surgical outcomes15, significant differences have been reported in outcomes between LOT ab externo and sutured LOT with wide incisions5,16. This discrepancy may be attributed to the anatomy of the aqueous humor outflow pathways, encompassing the fibrovascular column, Schlemm’s canal, collecting ducts, and aqueous humor veins17. While the fibrovascular column and Schlemm’s canal are distributed throughout the circumference, the collecting ducts are sparsely distributed18. Notably, a full LOT ab externo incision is achieved by rotating the rotome up and down to create a 120° opening, while a half-incision only creates a 60° opening. It is, therefore, possible that the observed IOP-lowering effect in the present study was not significantly related to rotome rotation range owing to potential bottleneck in the collecting ducts at the 120° and 60° incisions.
Regarding postoperative complications, no significant differences were observed in the incidence of transient IOP elevation and anterior chamber hemorrhage, suggesting comparable complication rates between the procedures performed by the residents and supervisors. Although Descemet’s membrane detachment, which can occur in LOT ab externo, was observed in a few patients in this study, and none of them required additional procedures. Moreover, residents required significantly longer operative times (44.9 ± 16.2 min) than did their supervisors. While this might be attributed to the learning curve and focus on precise technique, it is crucial to explain this potential delay to patients beforehand when a resident is the performing surgeon.
Despite the insights offered in our study, certain limitations should be acknowledged. First, the study was conducted at a single institution with a relatively small sample size. Second, the observation period was short, and the number of patients who were followed up for 24 months was limited. This lack of long-term follow-up can be attributed to the fact that our institution is an acute care hospital, where many patients are referred to their local doctors after surgery. Lastly, we defined supervisors as full-time ophthalmologists with ≥ 5 years of experience at our hospital, whereas residents were defined as any other doctor who were not supervisors. This definition underestimates the experience of most residents who had prior experience in other institutions but were new to our hospital. Nevertheless, all residents had < 5 years of experience and had never performed LOT ab externo at other hospitals; this criterion thus had minimal impact on our analysis. We believe that a comparison between residents with very limited surgical experience and supervisors should be considered in the future. Third, some resident`s surgery is supervised by senior doctors. While we thoroughly review all surgical records, it is difficult to quantify the extent of senior doctors’ assistance during residents’ surgeries.
In conclusion, our study revealed no significant difference between resident physicians and their supervising ophthalmic surgeons regarding the surgical outcomes or complication rates of LOT ab externo procedures performed by them. These findings indicate that LOT ab externo is an effective procedure, regardless of ophthalmology training, and should be performed extensively by residents to gain proficiency in the techniques involved in surgeries such as trabeculectomy.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
References
Quaranta, L. et al. Quality of life in glaucoma: a review of the literature. Adv. Ther. 33, 959–981 (2016).
McKean-Cowdin, R. et al. Impact of visual field loss on health-related quality of life in glaucoma: the Los Angeles Latino eye study. Ophthalmology 115, 941–948e1 (2008).
Kass, M. A. et al. The ocular hypertension treatment study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch. Ophthalmol. 120, 701–713 (2002).
Leske, M. C., Heijl, A., Hyman, L. & Bengtsson, B. Early manifest glaucoma trial: design and baseline data. Ophthalmology 106, 2144–2153 (1999).
Takata, M., Ishikawa, H., Ikeda, T. & Gomi, F. Conventional trabeculotomy versus gonioscopy-assisted transluminal trabeculotomy: a retrospective cohort study. J. Clin. Med. 11, 46 (2021).
Gurnani, B. & Tripathy, K. Minimally invasive glaucoma surgery. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK582156/ (2022).
Mori, S. et al. A comparison of the 1-year surgical outcomes of Ab externo trabeculotomy and Microhook Ab interno trabeculotomy using propensity score analysis. BMJ Open. Ophthalmol. 5, e000446 (2020).
Wada, Y., Nakatsu, A. & Kondo, T. Long-term results of trabeculotomy Ab externo. Ophthalmic Surg. 25, 317–320 (1994).
Matsuoka, M. et al. Dampening of diurnal intraocular pressure fluctuation by combined trabeculotomy and sinusotomy in eyes with open-angle glaucoma. J. Glaucoma. 22, 290–293 (2013).
Harms, H. & Dannheim, R. Trabeculotomy ab externo. Trans. Ophthalmol. Soc. 89, 589–590 (1970).
Lima-Fontes, M. et al. Comparison of trabeculectomy outcomes performed by residents in training and ophthalmologists. J. Glaucoma. 32, 320–326 (2023).
Walkden, A. et al. Trabeculectomy training in England: are we safe at training? Two year surgical outcomes. Eye (Lond). 32, 1253–1258 (2018).
Annoh, R. et al. The impact of simulation-based trabeculectomy training on resident core surgical skill competency. J. Glaucoma. 32, 57–64 (2023).
Liu, Y. C., Wilkins, M., Kim, T., Malyugin, B. & Mehta, J. S. Cataracts. Lancet 390, 600–612 (2017).
Chihara, E. & Chihara, T. Turn back elevation of once reduced IOP after trabeculotomy Ab externo and Kahook dual blade surgeries combined with cataract surgery. Clin. Ophthalmol. 14, 4359–4368 (2020).
Chin, S. et al. Reduction of intraocular pressure using a modified 360-degree suture trabeculotomy technique in primary and secondary open-angle glaucoma: a pilot study. J. Glaucoma. 21, 401–407 (2012).
Johnson, M., McLaren, J. W. & Overby, D. R. Unconventional aqueous humor outflow: a review. Exp. Eye Res. 158, 94–111 (2017).
Hann, C. R., Bentley, M. D., Vercnocke, A., Ritman, E. L. & Fautsch, M. P. Imaging the aqueous humor outflow pathway in human eyes by three-dimensional micro-computed tomography (3D micro-CT). Exp. Eye Res. 92, 104–111 (2011).
Acknowledgements
We would like to thank Hitoshi Obayashi for their guidance with the statistical analysis. We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Contributions
TS and HN have designed the study. TS acquired and analyzed the data. TS wrote the manuscript. HN revised the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sakamoto, T., Nisiwaki, H. Comparison of trabeculotomy ab externo outcomes between resident physicians and supervising ophthalmologists using propensity score matching. Sci Rep 15, 16669 (2025). https://doi.org/10.1038/s41598-025-01151-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01151-7