Abstract
This study investigated lidocaine distribution following patch application at peripheral position. The study included three parts. Animals in Part A (n = 12) were received 5% lidocaine patches on paravertebral (Group A1) or parasternal (Group A2) side, covering the distribution of the unilateral T3-T8 intercostal nerves. Part B (group B, n = 6) received bilateral patches along the T6-T8 intercostal nerve distribution. In Part C (n = 12), Group C1 severed the bilateral 5th-7th intercostal nerves followed by patch application approximately 0.5 cm lateral to the incisions, while Group C2 had the same patch placement without nerve cutting. All rabbits were euthanized 24 h after 5% lidocaine patch applied for 12 h. Dorsal root ganglia (DRG), fascia and spinal cord were collected. Lidocaine concentrations were determined using high-performance liquid chromatography. Lidocaine concentration in the DRGs on the treated side of A1 was significantly higher than that of A2. A1 and A2 exhibited lower lidocaine concentrations in contralateral DRGs compared to the treated side. In Group B, lidocaine concentration in DRG was higher in T6-T8 segments than in T3-T5 segments, with no significant difference in spinal cord concentration between segments. Group C showed significantly lower DRG lidocaine concentration in C1 compared to C2, with a slight decrease in spinal cord lidocaine concentration in C1. Intercostal nerves are the primary pathway for lidocaine transport from the periphery to the DRGs. Lidocaine patches should be applied as close to the spine as possible.
Similar content being viewed by others
Introduction
Lidocaine patches are typically considered peripheral analgesics, penetrating the stratum corneum to target peripheral nerve endings. Here, The principal mechanism of lidocaine as a local anaesthetic is through blockade of voltage-gated sodium channels leading to a reversible block of action, inhibiting pain signal transmission1,2,3. The potential propagation lidocaine may reduce the electrical activity of primary sensory neurons by interacting with transient receptor potential channels4,5.
Usually, lidocaine was administered via intradermal injections for neuropathic pain conditions like postherpetic neuralgia. Previous study demonstrated that lidocaine patches, similar to subcutaneous injections, achieve substantial lidocaine concentrations in both local skin and the dorsal root ganglion (DRG)6,7,8. These findings suggested a dual action on periphery and DRG for topical lidocaine8.
Drugs administered intranasally can reach the brain via the olfactory nerve or the trigeminal nerve9,10,11. Research indicates that the vagus and spinal nerve facilitate transneuronal transport from the gut to the brain and spinal cord, respectively12. Given the direct connection between intercostal nerves and spinal nerve DRG, we hypothesize that intercostal nerves might serve as a transport pathway from periphery to the DRG.
Typically, lidocaine patches are applied to painful areas. However, skin integrity is often compromised in conditions like surgical incisions or shingles, hindering lidocaine path applied directly. Zhang et al. demonstrated that injecting horseradish peroxidase (HRP) into the scapular region of rabbits led to HRP-positive cells in the C4-T10 spinal ganglia6, with a distribution area significantly larger than the scapular region itself. In addition, Nitro Yellow-labeled cells displayed an even wider distribution. Thus, it is speculated that lidocaine patches may act on a broader distribution than the application area, suggesting potential therapeutic effects of patches applied adjacent to damaged areas.
This study aims to investigate the influence of patch placement on lidocaine distribution and segmental characteristics. Additionally, we will explore the intercostal nerve as a potential transport pathway for lidocaine from the periphery to the DRG.
Materials and methods
Animals
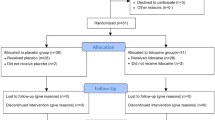
Thirty male rabbits (n = 30; weight:1800–2000 g) from Qingdao BioSino Antibody Biotechnology Co.,Ltd were housed individually in a controlled environment (22–25 °C) with ad libitum access to food and water for one week prior to experimentation. The study was conducted in accordance with the Guide Opinions on Treating Experimental Animals issued by the Ministry of Science and Technology (China) in 2006. All experiments involving animal procedures were approved by the Animal Ethics Committee of Shandong Second Medical University (Approval No. 2024SDL004) and were in accordance with the ARRIVE guidelines.
Application of Lidocaine patches
The hair corresponding to the intended application site was shaved gently to avoid damage. Afterward, rabbits were housed in a quiet, warm (22–25 °C), environment for 48 h with normal feeding. Rabbits were intravenously anesthetized by pentobarbital sodium (30 mg/kg) though ear vein.(See Timeline in below image).

DRG, dorsal root ganglia; ICN, intercostal nerve; CSF, cerebrospinal; HPLC, high-performance liquid chromatography.
Part A: Lidocaine patch applied paravertebrally or parasternally.
Twelve rabbits were randomly assigned to Groups A1 and A2 (n = 6/group). 5% lidocaine patch (14 cm × 5 cm) was applied to the left paravertebral (Group A1) or left parasternal area (Group A2), covering the distribution of T3-T8 intercostal nerves. After waking, return the rabbit to its cage. The patch was removed after 12 h, and animals were euthanized 24 h post-application. Blood and cerebrospinal fluid were collected before euthanasia (jugular vein and lumbar puncture, respectively). Rabbits were euthanized by intravenous injection of pentobarbital sodium. Subsequently, subcutaneous fascia (treated and contralateral side), bilateral T3-T8 DRGs and corresponding spinal cords were collected and dissected.
Part B: Lidocaine patch applied to T6-T8.
Six rabbits (Group B) received bilateral 5% lidocaine patches (10 cm×3.5 cm) covering the intercostal nerve distribution of T6-T8. Patches were removed after 12 h, followed by euthanasia at 24 h. Subcutaneous fascia, bilateral DRGs, and spinal cord from T3-T5 and T6-T8 segments were collected.
Part C: Lidocaine patch applied to T5-T7 after intercostal nerves severed.
Twelve rabbits were randomly assigned to Groups C1 and C2 (n = 6/group). In Group C1, bilateral T5-T7 intercostal nerves were surgically severed under anesthesia, followed by bilateral 5% lidocaine patch (10 cm×3.5 cm) application approximately 0.5 cm lateral to the incisions, covering T5-T7 intercostal nerves. Group C2 underwent the same surgical maneuver as group C1 with the intercostal nerve intact. The patch in group C2 covered the same position as in group C1. Following euthanasia, bilateral DRGs of T5-T7 and corresponding spinal cord were collected.
Measurement of drug concentration in tissues
Lidocaine concentrations were determined using high-performance liquid chromatography (HPLC). The HPLC system employed a Dikma C18 column (Dikma Technologies, 250 mm × 4.6 mm, 5 μm) and a mobile phase consisting of methanol and water (62:38, v/v) containing 0.3 mL acetic acid and 0.6 mL triethylamine per 100 mL. The system was operated at a pH of 4.9, a detection wavelength of 230 nm, a column temperature of 30 °C, and a flow rate of 0.8 mL/min. Lidocaine peaks were identified in chromatograms based on retention time compared to a lidocaine standard, and concentrations were quantified by peak area analysis.
Statistical analysis
Data was presented as means ± standard deviation. Independent sample t-tests was used to compare the difference between groups. The concentration of lidocaine in treated side and contralateral side were compared using paired t-testson. All data were analyzed using IBM SPSS 27 (IBM Corp., Armonk, NY, USA), and values with p < 0.05 were considered statistically significant.
Results
Effect of transport distance on Lidocaine concentration in DRG and spinal cord
No significant difference of lidocaine concentration was observed in subcutaneous fascia on the treated side between Group A1 and A2 after 12 h of patch application. No lidocaine was detected in the contralateral fascia (Table 1) by HPLC. Conversely, DRG lidocaine concentration was significantly higher on the treated site in Group A1 compared to Group A2. While lower lidocaine was also detected in contralateral DRGs. Both groups exhibited minimal lidocaine concentrations in the spinal cord, serum, and cerebrospinal fluid. Regardless of patch placement (paravertebral or parasternal), the highest lidocaine concentration was consistently found in the treated-side DRG, followed by treated-side subcutaneous fascia, spinal cord and contralateral DRG (Table 1).
Segmental distribution characteristics of Lidocaine in DRG and spinal cord
Lidocaine was detected in the subcutaneous fascia of T6-T8 segments but not in T3-T5 segments. DRG lidocaine concentration was higher in T6-T8 segments than T3-T5 segments, while spinal cord lidocaine levels did not significantly differ between these regions (Fig. 1).
Segmental distribution characteristics of lidocaine. Lidocaine was not detected in the subcutaneous fascia of the T3-T5 segments. The concentration of lidocaine in the dorsal root ganglia (DRGs) of the T6-T8 segments was higher than that in the DRGs of the T3-T5 segments. There was no statistically significant difference in lidocaine concentration in the spinal cord between the two segments (n = 6, *p < 0.05, **p < 0.01).DRG, dorsal root ganglia.
The role of intercostal nerves in Lidocaine transport
Severing intercostal nerves, DRG lidocaine concentration significantly reduced in Group C1 compared to Group C2. A slight decrease of lidocaine concentration in spinal cord was also detected in Group C1 (Fig. 2).
Effect of intercostal nerves on lidocaine transport. Severing intercostal nerves significantly decreased DRG lidocaine concentration in Group C1 compared to Group C2. Lidocaine concentration in the spinal cord of Group C1 was slightly lower than that of Group C2 (n = 6, *p < 0.05, **p < 0.01).DRG, dorsal root ganglia.
Discussion
This study demonstrated lidocaine concentrations in the DRGs increased as the patch was positioned closer to the DRG. However, the patch’s location did not significantly influence spinal cord lidocaine levels. The higher lidocaine concentration was primarily transported from the periphery to the DRGs via the intercostal nerves.
Lidocaine concentrations in the DRGs were consistently higher than those in the local skin, regardless of whether the drug was applied as a patch or injected intradermally8. Our findings further revealed that lidocaine levels were highest in the DRGs, followed by the local fascia, spinal cord, contralateral DRG, and serum. No lidocaine was detected in the cerebrospinal fluid. The higher lidocaine concentration in DRG was transferred by neither blood nor cerebrospinal fluid. High concentrations of lidocaine in the DRG may be associated with analgesic effects after local application. The alterations of ion channels in the DRG, such as Nav1.8, K2PI.I, contribute to peripheral neuropathic pain1,13,14,15. Whether topical application of lidocaine patch could produce analgesic effects by altering these ion channels need to be further investigated.
The asymmetrical distribution of lidocaine, with higher concentrations in the ipsilateral DRG, suggests a neuronal uptake mechanism. Lidocaine likely reaches the DRGs through nerve endings before trans-synaptic transport to the spinal cord. This process differs from neural conduction, as it involves a reduction in drug concentration. Consequently, only a fraction of the lidocaine initially reaching the DRGs eventually arrives at the spinal cord, resulting in lower levels in this region.
To elucidate the pathway of lidocaine transport to the DRG, T5-T8 intercostal nerves were severed. Subsequent lidocaine concentration measurements revealed significantly lower levels in the DRGs of Group C1 compared to Group C2, implicating intercostal nerves as the primary way for lidocaine transport from nerve endings to the DRG. Furthermore, paravertebral patch application yielded higher DRG concentrations than parasternal application, supporting the hypothesis that lidocaine is absorbed via intradermal nerve endings7 and transported retrogradely along intercostal nerves to the DRG. Thus, patch proximity to the spine correlated with drug delivery to the DRG.
Unlike the localized effects observed with nerve transport, lidocaine patches applied to lower thoracic nerve segments resulted in detectable drug levels in adjacent upper nerve segments, albeit at lower concentrations than the DRG in the treated site. Additionally, DRG concentrations within the patch application area exceeded those in adjacent uncovered regions. These findings suggest lidocaine distribution beyond the direct patch area via alternative pathways. Consistent with this, Zhang et al. demonstrated riboflavin spread from a scapular injection site to DRGs from C3 to T116. Given lidocaines’ smaller molecular weight and enhanced absorption/diffusion compared to riboflavin, it is anticipated to exhibit a broader DRG distribution and analgesic area than the patch itself.
The peripheral placement of the lidocaine patch did not influence spinal cord lidocaine concentrations. Neither paravertebral nor parasternal application resulted in significant differences in spinal cord levels. Moreover, within Group B, lidocaine concentrations were comparable between the treated site (T6-T8 segments) and the adjacent non-treated site (T3-T5 segments). Data from Group B also showed undetectable levels of lidocaine in T3-T5 subcutaneous tissue but significantly higher concentrations of T3-T5 DRG than those observed in the corresponding spinal cord segments. This suggested that the unapplied segments of lidocaine were not derived from the spinal cord or fascia. There were other potential lidocaine transit pathways, such as the mesenteric, thoracic sympathetic, and celiac nerves6,7.
Mirror pain (MP) is characterized by pain and hyperalgesia at both the injury site and its contralateral counterpart16,17,18,19. This phenomenon, also observed in postherpetic neuralgia, prompted the investigation of lidocaine distribution in contralateral DRGs. While lidocaine was detected in contralateral DRGs but not fascia, and serum levels were significantly lower than contralateral DRG levels, these findings excluded serum or patch diffusion as sources of contralateral drug. MP is linked to symmetrical spinal cord neural connections18,19, suggesting a spinal origin for contralateral DRG lidocaine. Although spinal lidocaine concentrations exceeded those in contralateral DRGs, supporting this hypothesis, a static study cannot definitively confirm this source. Previous research on decerebrate animals also supports the existence of spinal mirror image pathways20,21.
Previous research suggests the existence of a high-conductivity interstitial fluid channel in mammalian subcutaneous loose connective tissue22. Additionally, Song et al. discovered that the migration trajectory of Alcian blue dye in rainbow fish was located in the fascia between tissues23. It was therefore speculated that lidocaine could also be transported through the fascia, leading to the measurement of lidocaine concentration in the fascia in this study. In Groups A1 and A2, lidocaine was detected in the fascia on the treated side, but not on the contralateral side. Similarly, in Group B, lidocaine was detected in the fascia at the treated site (T6-T8 segments) but not in the adjacent non-treated site (T3-T5 segments). These findings suggest that lidocaine may not be transported through the fascia. However, applied lidocaine patches on cats for 72 h, lidocaine and its metabolites were detected in the contralateral dermis and epidermis, but not the fascia24. In this study, we did not investigate whether lidocaine could be detected in the fascia if the patch application time was long enough, warranting further research.
There were several limitations in this study. The hairs were shaved before the lidocaine patches were applied. However, the fine downy hairs were not completely removed, which may have an impact on the transdermal absorption of lidocaine. Additionally, multiple time points were not set to represent the dynamics of lidocaine concentrations in DRG and other tissures. Moreover, the association between lidocaine concentration and analgesic effect in each tissue was not further observed in this experiment. Further studies are needed.
In conclusion, lidocaine transport distance and patch position significantly impact DRG concentration. The results implied that optimal pain relief may be achieved by applying the patch as close to the pain area as possible. If a direct application is impractical, placing the patch near the spine maximizes lidocaine delivery to the DRGs via intradermal nerve endings, accelerating analgesic effects.
Data availability
The data that support the findings of this study are available on request from the corresponding author upon reasonable request.
References
Sheets, M. F. & Hanck, D. A. Molecular action of Lidocaine on the voltage sensors of sodium channels. J. Gen. Physiol. 121, 163–175 (2003).
Mick, G. & Correa-Illanes, G. Topical pain management with the 5% Lidocaine medicated plaster–a review. Curr. Med. Res. Opin. 28, 937–951 (2012).
Kirillova, I. et al. Effect of local and intravenous Lidocaine on ongoing activity in injured afferent nerve fibers. Pain 152, 1562–1571 (2011).
Jara-Oseguera, A., Simon, S. A. & Rosenbaum, T. TRPV1: on the road to pain relief. Curr. Mol. Pharmacol. 1, 255–269 (2008).
Baron, R., Binder, A. & Wasner, G. Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol. 9, 807–819 (2010).
Zhang, Y. H. et al., Experimental study on the mechanism of the treatment of postherpetic neuralgia by intradermal drug injection. Chin. J. Anesthesiology, 35–37 (2003).
Zhang, Y. H. et al., Observation on retrograde neural tracing of nerve ending receptor passage with lidocaine tracer through intradermal injection. 128–130 (2006).
Jiao, W. Q. et al. Drug distribution in skin and DRG following Lidocaine patch application in rabbits. Chin. J. Pain Med. 28, 306–310 (2022).
Thorne, R. G., Pronk, G. J., Padmanabhan, V. & Frey, W. H. 2nd. Delivery of insulin-like growth factor-I to the rat brain and spinal cord along olfactory and trigeminal pathways following intranasal administration. Neuroscience 127, 481–496 (2004).
Schaefer, M. L., Böttger, B., Silver, W. L. & Finger, T. E. Trigeminal collaterals in the nasal epithelium and olfactory bulb: a potential route for direct modulation of olfactory information by trigeminal stimuli. J. Comp. Neurol. 444, 221–226 (2002).
Illum, L. Transport of drugs from the nasal cavity to the central nervous system. Eur. J. Pharm. Sciences: Official J. Eur. Federation Pharm. Sci. 11, 1–18 (2000).
Wang, X. et al. Peripheral nerves directly mediate the transneuronal translocation of silver nanomaterials from the gut to central nervous system. Sci. Adv. 9, eadg2252 (2023).
Mao, Q. et al. Role of dorsal root ganglion K2p1.1 in peripheral nerve injury-induced neuropathic pain. Mol. Pain. 13, 1744806917701135 (2017).
Mao, Q. et al. DNMT3a-triggered downregulation of K(2p) 1.1 gene in primary sensory neurons contributes to paclitaxel-induced neuropathic pain. Int. J. Cancer. 145, 2122–2134 (2019).
Mao, Q. et al. Transcriptome analysis of MicroRNAs, circrnas, and mRNAs in the dorsal root ganglia of paclitaxel-induced mice with neuropathic pain. Front. Mol. Neurosci. 15, 990260 (2022).
Nie, H. et al. Gene expression profiling of contralateral dorsal root ganglia associated with Mirror-Image pain in a rat model of complex regional pain syndrome Type-I. J. Pain Res. 14, 2739–2756 (2021).
Liu, P. W. et al. Advances in the study of peripheral and central neural mechanisms of mirror pain. Chongqing Med. J. 47, 1664–1666 (2018).
Huang, D. & Yu, B. The mirror-image pain: an unclered phenomenon and its possible mechanism. Neurosci. Biobehav. Rev. 34, 528–532 (2010).
Drinovac Vlah, V. & Bach-Rojecky, L. Mirror-Image Pain Update: Complex Interactions Between Central and Peripheral Mechanisms. Molecular neurobiology (2024).
Woolf, C. J. Long term alterations in the excitability of the flexion reflex produced by peripheral tissue injury in the chronic decerebrate rat. Pain 18, 325–343 (1984).
Fitzgerald, M. The contralateral input to the dorsal Horn of the spinal cord in the decerebrate spinal rat. Brain Res. 236, 275–287 (1982).
Li, H. Y. et al. Fluid flow along venous adventitia in rabbits: is it a potential drainage system complementary to vascular circulations? PloS One. 7, e41395 (2012).
Song, X. J. et al., One of the meridian essences:fascia-interstitial-interstitial fluid system-experimental verification and biological significance. in New Era, New Thinking, New Leap, New Development – 2019 Chinese Acupuncture and Moxibustion Society Annual Meeting and 40th Anniversary Review. 99–106 (China, 2019).
Ko, J. C., Maxwell, L. K., Abbo, L. A. & Weil, A. B. Pharmacokinetics of Lidocaine following the application of 5% Lidocaine patches to cats. J. Vet. Pharmacol. Ther. 31, 359–367 (2008).
Acknowledgements
This work was funded by Weifang Municipal Health Commission (WFWSJK-2023-002) and Weifang Weifang Science and Technology Bureau (2023GX032).
Author information
Authors and Affiliations
Contributions
Ren ZJ and Xu G designed the study. Zhai YJ analyzed the data. Xu G and Liu YP conducted experiments and drafted the manuscript. Yu ZJ and Huang YP reviewed and edited the original draft. All authors revised the draft and approved this version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, G., Zhai, Y., Yu, Z. et al. Drug distribution in dorsal root ganglion after peripheral application of Lidocaine patch. Sci Rep 15, 16913 (2025). https://doi.org/10.1038/s41598-025-01169-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01169-x