Abstract
This study investigated the prospective associations between changes in 24-h movement behaviors and physical fitness (PF) components in preschool children; and examined how the reallocation of time between movement behaviours was associated with longitudinal changes in PF. This is a two-year longitudinal study of 200 Chinese children aged 3–4 years old. At baseline and follow-up, 24-h movement behaviors including moderate-to-vigorous physical activity (MVPA), light physical activity (LPA), screen-based sedentary behavior (SSB), non-screen-based sedentary behavior (NSB), and sleep were assessed. Balance, cardiorespiratory fitness, flexibility, muscle strength, muscular endurance, and speed-agility were measured using a balance beam test, 20-m shuttle run test, sit and reach test, handgrip test, sit-ups, and 4 × 10 m shuttle run test respectively. The robust compositional regression was employed to explore the association between changes in movement behaviours and PF components, and compositional longitudinal isotemporal substitution analysis was used for the time reallocation. LPA was positively associated with flexibility (β = 3.25, p < 0.05), while sleep was negatively associated with flexibility (β = −4.39, p < 0.05). MVPA was positively associated with muscular endurance (β = 1.36, p < 0.05) at follow-up. The addition of MVPA at the expense of other movement behaviors during the two years was associated with increased muscular strength at follow-up. Reallocations between sleep, NSB, SSB, and LPA showed significant associations with flexibility at follow-up. The impact of MVPA replacing other behaviors on muscular strength was smaller than other behaviors replacing MVPA. Our findings highlight the importance of maintaining PA time to promote PF levels in preschool children. Programs on encouraging a range of light to vigorous active play opportunities and balancing between sleep and PA are crucial for enhancing PF development in preschool children.
Similar content being viewed by others
Introduction
Physical fitness (PF) is the ability to perform daily physical activity (PA), including aerobic fitness, muscular strength, endurance, flexibility, speed, and balance1. For young children, higher fitness levels are positively related to lower fat mass index, increased bone strength, better intellectual maturity, and improved cognitive function2,3,4,5. Maintaining adequate levels of PF from early childhood is beneficial for health during adulthood6,7. However, some PF indicators of preschool children have declined alarmingly over the past few decades in many countries. For example, compared to 2014, the performance of young children in China in 2020 in two-legged continuous jumping, seated forward body bending, and standing long jump has decreased on average8. Moreover, Polish research indicated that boys experienced negative changes in standing long jump, flexibility, and throwing performance from 2008 to 20189.
Evidence showed that engagement with daily activities in preschoolers is strongly associated with increased PF10,11. Sufficient PA, limited sedentary time, and appropriate sleep duration can contribute to higher PF levels in preschool children. Vigorous physical activity (VPA) and moderate-to-vigorous physical activity (MVPA) are positively associated with cardiorespiratory fitness (CRF) and muscular strength among preschoolers12. Health-related PF in preschool children is negatively associated with total sedentary time13. Moreover, children with poor sleep quality or shorter sleep duration are more likely to exhibit lower muscle endurance, flexibility, and CRF14.
Sleep, sedentary behavior (SB), and PA constitute a continuum from inactivity to high activity over a 24-h period15,16. These movement behaviors coexist as a whole or as components, changes in the time spent on one behavior require changes in the time spent on another behavior, which may lead to changes in other health outcomes17. Compositional isotemporal substitution analysis is applied to estimate changes in health outcomes of time reallocation between 24-h movement behavior17. Many studies adopted compositional isotemporal substitution analysis to explore the association between 24-h movement behavior and PF without affecting changes in other behaviors and quantified the reallocation of time and changes in PF.
Previous cross-sectional studies have shown that reallocating to different types of movements has different effects on PF indicators in young children. Gu, et al. 18 found that replacing SB or light physical activity (LPA) with MVPA was associated with improved muscular strength and speed in Japanese preschool children. Reallocating 30 min of LPA or SB with 30 min of MVPA was related to higher lower limb strength and CRF in Chinese preschoolers19. Another Chinese study reported that adding MVPA at the expense of SB and sleep, MVPA at the cost of sleep was associated with muscular strength and speed-agility improvements, respectively20. A Brazilian study demonstrated similar results that CRF improvement by substituting SB or sleep with MVPA, and reallocating time between sleep and LPA improved speed-agility and lower body muscular strength21. However, there is a lack of longitudinal studies, which limits the ability to demonstrate associations between within-person changes in movement behaviors over time and PF outcomes among preschool children.
In addition, SB can be divided into screen-based sedentary behavior (SSB) and non-screen-based sedentary behavior (NSB)22. Children and adolescents who experienced more SSB exhibited a higher risk of poor PF, cardiovascular health issues, and obesity compared to NSB23. In young children, the study by Hu et al. (2021) indicated preschoolers who spend more time in SSB are more likely to be overweight, but the relationship between NSB and overweight is not nonexistent24. Evidence suggested that certain forms of SB may have varying associations with preschoolers’ PF21. Nevertheless, the specific types of SB were not discriminated against in previous compositional isotemporal substitution analysis. Furthermore, existing research primarily focused on limited PF components. A comprehensive understanding of all PF components is essential for tailoring effective interventions for preschool children.
To fill the gap in longitudinal associations between movement behavior and PF among preschool children, and to investigate how reallocating time among these behaviors affects PF to promote healthy movement behaviors and optimize PF in young children, this study aimed to (1) analyze the longitudinal association between 24-h movement behaviors (MVPA, LPA, SSB, NSB, sleep) and PF components in Chinese preschoolers; and (2) explore how reallocations of time between movement behaviors were associated with changes in PF components, informing targeted intervention strategies.
Methods
Study design
This is a prospective cohort longitudinal study and adopted convenience sampling. This study was conducted under the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines. Ethical approval was obtained from the Research Ethics Committee of Beijing Normal University-Hong Kong Baptist University United International College. Signed consent forms were obtained from the kindergarten and parents before the study. Baseline data collection was carried out from October 2021 to December 2021, and two-year follow-up data collection was conducted from October 2023 to December 2023. The kindergartens provided children’s socio-demographic data such as the date of birth and gender.
At baseline assessment, anthropometric data were measured in the kindergarten activity room, followed by PF tests. Children were given a 2-min break between each test to minimise fatigue. All assessments were administered in the same order by the same assessors. The assessors had at least 5 years of experience in preschool children’s anthropometric and PF testing and completed a two-hour supervised training. Questionnaires were taken home by the children and completed by their parents on the assessment day. Accelerometers were placed on the children, who wore the monitors for seven consecutive days. The follow-up phase implemented the same assessment methods, device settings, process, and measurement protocol as the baseline phase.
Participants
From July 2021 to September 2021, formal invitation letters were sent to the administrators of the 45 registered kindergartens in Zhuhai, Guangdong Province, China. The study objectives, procedures, and expected contributions from the participating kindergartens were outlined in the invitation letters. Four kindergartens agreed to participate in this study. The inclusion criteria were: (1) children aged three to four years old, (2) typical developing children (i.e. they were not diagnosed with developmental, neurological disorders, gastrointestinal, or other chronic diseases that could impact a child’s health, physical abilities, or cognitive functions) based on parent report and school records25,26; and (3) would not transfer or drop out of kindergarten during data collection.
Measures
At baseline, participants’ anthropometric data, 24-h movement behaviors, and PF were measured. At the two-year follow-up, participants’ 24-h movement behaviors and PF were measured to track the association between 24-h movement behaviors and PF components.
Anthropometric measurements
Height and weight were measured with a stadiometer (Seca) and weight scale (Wujin, RGT-120), while the participants were barefoot and lightly clothed. Body mass index (BMI) was calculated by dividing body weight by the square of height (kg/m2).
Movement behaviors
PA was measured using the accelerometer (ActiGraph, GT3X-BT, Pensacola, FL, USA), which is a valid, cost-efficient, and widely used tool to assess PA levels in preschoolers 27. The kindergarten teachers and parents received written and video instructions for the usage and placement of the accelerometer. Parents were asked to register an activity diary for both wear and non-wear time. Participants wore the accelerometer on the right hip to monitor all activities for seven consecutive days, except during periods of sleep and water-based activities. The ActiLife software (version 6.13) was used for device initialization, data reduction and data analysis.
A recording epoch of 15 s was used, and valid wear time was considered to be at least 8 h of wear time over at least three days (two weekdays and one weekend day). Non-wear time was defined as 20 consecutive minutes of zero count/minute. Accelerometers were initialized at a sampling rate of 30 Hz and then reintegrated into 60-s epochs for analysis28,29. Time spent in different intensity domains was categorized using the cut-off points according to Butte et al.: sedentary: < 819 counts per minute (CPM); light: 820–3907 CPM; moderate: 3908–6111 CPM; and vigorous: ≥ 6112 CPM30.
SSB and NSB were measured using the leisure-time sedentary behaviors questionnaire (LTSBq)31. Parents were asked to report the frequency and duration of their child spent in SSB (e.g., watching TV; playing with a mobile phone, tablet, or electronic games; and using a computer) and NSB (e.g., reading, writing, or drawing and playing with toys) on weekdays and weekends. The average SSB and NSB time per day over the week was calculated respectively.
Parents were asked to report their child’s daily sleep time using the questionnaire. They needed to recall the children’s average sleep hours as follows: “On weekdays, how many hours does your child usually sleep at night?” and “On weekends, how many hours does your child usually sleep at night?”. The total sleep time was calculated as follows: ((weekdays sleep*5) + (weekends sleep*2))/7. This method has been validated in preschool children32,33.
Physical fitness
The 20-m shuttle run was used to assess CRF. During the test, participants ran back and forth at an initial speed of 6.5 km/h on two tracks 20 m apart, and then in increments of 0.5 km/h per minute. The test ended when the participant failed to reach the end lines concurrent with the audio signal on two consecutive occasions or when the participant stopped due to exhaustion. The test was conducted once. Once the child stopped, the last completed shuttle was recorded. The 20-m shuttle run has good test–retest reliability (r = 0.73–0.93) in children aged three to five years34.
The sit and reach test was used to measure flexibility. Participants sat with straight legs and pushed a mobile board with extended arms in maximal effort while keeping their knees static. The procedure was conducted twice, and the highest value was recorded. This measurement has been utilized in preschool children with good test–retest reliability (r = 0.75 to 0.93)35.
Sit-ups were used to assess the muscular endurance of the trunk. Participants lay on their backs with their knees bent and arms crossed over the other shoulder. They sat up and returned to the starting position. The number of correct lifts within 30 s was recorded. This test has good reliability (r = 0.68 to 0.94) in preschoolers 36.
Muscular strength was tested with a WCS-100 electronic dynamometer (Shanghai Wanqing Electronics Co., LTD.). Participants held the dynamometer and adjusted the grip distance, subsequently using maximum force to grasp the dynamometer. Two measurements were taken for both the left and right hand, with the highest recorded value being documented. This measurement has been utilized in preschool children with good reliability (r = 0.90 to 0.92) and validity37.
Dynamic balance was measured using a balance beam. Participants stood behind the start, facing the beam with arms out. The tester timed them crossing the beam, stopping the clock when either the foot or the finish line was crossed. The trial was conducted twice and the shortest time was recorded. The balance beam test has displayed adequate reliability and validity in younger children38.
Speed-agility was assessed by the 4 × 10 m shuttle run test. Participants made sharp turns around 10-m markers and touched the tester’s hand at each end before returning to the start. The best of the two tests was recorded. This test has been utilized in preschoolers with good reliability and validity39.
Data analysis
Statistical analyses were performed using SPSS 29.0 software (SPSS Inc., an IBM Company, Chicago, IL, USA) and R 4.3.3 software (R Foundation for Statistical Computing, Vienna, Austria). Confidence interval of 95% was used, and p < 0.05 was considered statistically significant.
Descriptive statistics were calculated for characteristics and variables. Continuous variables were presented with means and standard deviations, and counts and percentages were described as categorical variables. The compositional mean was computed by calculating the geometric mean for each behavior (sleep time, NSB, SSB LPA, and MVPA) and then normalizing the data to the same constant as the raw data, i.e. 1.
The relative nature of the movement behavior data is considered in the statistical analysis, which means that the source of relevant information is not the absolute values of the movement behaviours, but the ratios between them40. The compositions were represented as pivot coordinates, which is a special case of isometric logarithmic ratios (ILRs)41. The first pivot coordinate contains all the relative information about a primary activity, rather than the geometric mean of the other activities. It can also be expressed as a sum of log ratios. Five sets of pivotal coordinates were constructed, each with a different activity (sleep time, NSB, SSB, LPA, and MVPA) as the dominant activity.
To avoid possible influence from outlier observations, robust compositional regression models were used to explore the prospective associations between changes in movement behaviors and PF40,42. The follow-up PF parameters were dependent variables and the differences between follow-up and baseline movement behaviors (expressed in pivotal coordinates) were the explanatory variable. Covariates (age, gender, respective baseline PF parameter, and pivot coordinate representations of baseline movement behaviour composition) were included as explanatory variables. Five models (each corresponding to a set of differences between the respective pivot coordinates) were run for each PF parameter to capture the differences between follow-up and baseline for the aggregated relative effect of each composition (sleep time, NSB, SSB, LPA, and MVPA) to contributions of the remaining parts.
The models mentioned above were used to predict the association between longitudinal time reallocation between movement behaviours and changes in PF parameters. Differences between the pivotal coordinate representation of the hypothetical follow-up and the mean baseline movement behavioural composition were calculated to estimate changes in PF parameters associated with one-to-one reallocations17. Estimated differences in PF were made for the 5-, 15-, and 20-min pairwise reallocations separately. The decision was made to limit the duration of reallocations to a maximum of 15 min to reflect the actual change in MVPA20,21.
Results
Descriptive statistics
At baseline, the mean age of 200 preschool children was 3.5 years and 53.0% of participants were boys (Fig. 1). Over two years, time spent in NSB and LPA increased by 22.9% and 5.0%, respectively. The time spent in SSB, MVPA, and sleep decreased by 55.9%, 3.7%, and 14.2%, respectively (see details in Table 1).
Compositional analysis
The compositional regression analyses between 24-h movement behavior components and PF are shown in Table 2. The results indicated that LPA was positively associated with flexibility (β = 3.25, p < 0.05). Sleep was negatively associated with flexibility (β = −4.39, p < 0.001). MVPA was positively associated with muscular strength (β = 1.36, p < 0.01).
Isotemporal reallocation
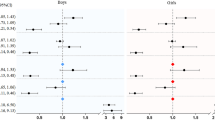
The estimated changes in PF parameters associated with isotemporal substitutions between behaviours are shown in Table 3, Figs. 2, and 3. The addition of sleep at the expense of NSB, SSB, and LPA was associated with a significant decrease in flexibility (with NSB: −0.16 to −0.04; with SSB: −0.33 to −0.03; with LPA: −0.44 to −0.05). Reallocating 15 min from other movement behaviors to MVPA was associated with increased muscular strength (with NSB: 0.12 to 0.61; with SSB: 0.09 to 0.60; with LPA: 0.13 to 0.75; with sleep: 0.10 to 0.60) showed significant associations.
Estimated change in follow-up muscular strength associated with time reallocation between baseline and follow-up movement behaviour composition. LPA, light physical activity; MVPA, moderate-to-vigorous physical activity; NSB, non-screen-based sedentary behavior; SSB, screen-based sedentary behavior.
The reallocation from NSB, SSB, and LPA to sleep revealed a symmetric reduction in flexibility. Reallocating 15 min from NSB, SSB, and LPA to sleep was associated with predicted decreases in flexibility (0.10, 0.18, 0.24, respectively). The reallocations of 15 min from sleep to NSB, SSB, and LPA showed significantly higher predicted 0.10, 0.16, and 0.24 changes in flexibility. Reallocations of sleep to NSB, SSB, and LPA were associated with better flexibility. Reallocations from NSB, SSB, and LPA to sleep were associated with worse flexibility (Fig. 2).
The associations were asymmetric. Reallocations of MVPA to other behaviors were associated with better muscular strength, whereas reallocations from other behaviors to MVPA were associated with worse muscular strength. The largest increase in muscular strength occurred when MVPA replaced LPA, followed by NSB, sleep, and SSB. Increasing MVPA time at the cost of NSB, SSB, LPA, and sleep yielded significantly higher predicted changes in muscular strength (0.37, 0.35, 0.44, and 0.35, respectively). When 15 min were reallocated from MVPA to NSB, SSB, LPA, and sleep, muscular strength was predicted to be 0.52, 0.50, 0.59, and 0.50, respectively. The benefits of increasing time in MVPA at the cost of other behaviors were lower than the negative effects of reallocating time away from MVPA to other behaviors (Fig. 3).
Discussion
This two-year longitudinal study suggested that 24-h movement behaviors were associated with flexibility and muscular strength in Chinese preschoolers. The effect of reallocation between NSB, SSB, LPA, and sleep on flexibility was symmetric. The reallocation of time between low-intensity movement behaivors (i.e. NSB, SSB, sleep, and LPA) and MVPA had asymmetric effects on muscular strength.
This study found that MVPA was positively associated with muscular strength, which is consistent with previous studies20,43. Another finding of this study suggested that LPA was positively associated with flexibility in preschool children. Engaging in typical forms of LPA, such as walking and playing, encourages a wide range of movements that require stretching and bending. These activities are beneficial for developing flexibility and joint mobility, as they naturally incorporate dynamic movements that promote the elongation of muscles and the full range of motion in joints44. Moreover, the cumulative effect of consistent participation in LPA is likely to enhance motor competence45. Children who develop high levels of motor competence are better equipped to engage in various physical activities. This enhanced capability allows children to perform movements that improve their flexibility46. This finding indicates that even low-intensity activities can effectively enhance flexibility in preschool children. Given the observed trend of decreasing flexibility in this study, it is crucial to encourage active participation in LPA among preschool children.
Previous studies using compositional and isotemporal substitution analysis have reported that increasing MVPA while decreasing SB can lead to enhanced PF performance18,21. However, it is noteworthy that most studies have not included sleep in isotemporal substitution models47. The finding of this study indicated that reallocating 15 min from sleep to NSB, SSB, and LPA was positively associated with flexibility in preschool children. Evidence suggests an inverted U-shaped relationship between sleep duration and PF among preschoolers, whereby both inadequate and excessive sleep are associated with lower PF performance48. Specifically, insufficient sleep may hinder recovery and energy levels49, while excessive sleep may result in reduced engagement in active behaviors, contributing to lower PF levels. In this study, 22% of participants (44/200) exceeded recommendations sleep time (10–13 h/day for preschoolers)50. There is a tendency for the negative effects of sleep on physical fitness to intensify as sleep duration increases beyond optimal levels. Therefore, more attention needs to be paid to avoiding excessive sleep duration in the management of children’s sleep schedules., Although flexibility is one of PF components, this finding should be interpreted with caution due to the unclear underlying mechanisms of the association between sleep and flexibility in children48.
Consistent with previous studies, the findings showed an asymmetrical association in muscular strength depending on whether MVPA time was increased or decreased18,20. In this study, the benefits estimated for the reallocation time to MVPA were not as large as the estimated worsening of the muscular strength when the same duration was reallocated away from MVPA. The asymptotic dose–response relationships between PA and muscular strength indicate that the relative benefits gained from preventing a decrease in current levels of MVPA are greater than those achieved by an equivalent increase in MVPA. Since preschool children’s PF level declines over time9, the maintenance of MVPA is an essential goal during early childhood. The implications of this study highlight the urgency of promoting sustained engagement in MVPA, as even small reductions may lead to disproportionately negative effects on PF outcomes. However, the confidence intervals for the absolute values of the estimated changes in muscular strength resulting from reallocations to and from MVPA were found to overlap42. This overlap implies that we cannot extrapolate this asymmetrical association to broader populations or different contexts beyond our study sample.
The reallocation between movement behaviors and muscular strength showed that the change in predicted muscular strength was biggest for the MVPA alternative to LPA compared to the NSB, sleep, and SSB. The difference in energy consumption between MVPA and LPA is small; thus, there is a higher probability of interchangeability between MVPA and LPA to enhance PF outcomes51. While SSB is more detrimental due to prolonged static postures52, NSB often involves intermittent postural shifts and light physical activity, which may already confer mild musculoskeletal benefits53. Replacing NSB with MVPA could thus introduce a more potent stimulus for muscle development, by transitioning from light to vigorous activity. In contrast, SSB’s highly sedentary nature may engender compensatory biomechanical adaptations (e.g., reduced posture variability, prolonged sitting) that are less responsive to short-term MVPA substitution53. This aligns with studies linking screen time to reduced motor skill proficiency54,55.
The main strength of this study is the longitudinal study design to explore the association between movement behaviors in preschoolers. Another strength is the discrimination between the type of activity during SB. However, this study has several limitations. Although the longitudinal design is adopted, measurements were conducted at only two-time points, which may not have detected the pattern of movement behaviors and PF changes42. Moreover, although necessary to identify the types of SB activities, the use of self-reported measurement may result in the vulnerable recall of results and social desirability bias. Besides, the representativeness and generalizability of the study findings are limited due to the convenience sampling approach. Future studies should be conducted with samples from different regions and apply the stratified random sampling approach.
Conclusion
There are association between changes in movement behaviours and PF components among Chinese preschoolers. Increasing NSB, SSB, and LPA time at the expense of sleep time was positively associated with flexibility. Reallocating time from inactive behaviors to MVPA was positively associated with muscular strength. These findings highlight the importance of maintaining time spent in PA to promote PF levels in preschool children. Kindergartens, communities, and families should implement programs and create a supportive environment to encourage light to vigorous active play and limit sedentary time, emphasizing the balance between sleep and physical activity to foster PF development in preschool-aged children.
Data availability
Data are available from the corresponding author on reasonable request.
References
Ortega, F. B., Ruiz, J. R., Castillo, M. J. & Sjöström, M. Physical fitness in childhood and adolescence: A powerful marker of health. Int. J. Obes. 32, 1–11. https://doi.org/10.1038/sj.ijo.0803774 (2008).
Henriksson, P. et al. Physical fitness in relation to later body composition in pre-school children. J. Sci. Med. Sport 22, 574–579. https://doi.org/10.1016/j.jsams.2018.11.024 (2019).
Gómez-Bruton, A. et al. Association between physical fitness and bone strength and structure in 3- to 5-year-old children. Sports Health 12, 431–440. https://doi.org/10.1177/1941738120913645 (2020).
Latorre-Román, P. Á., Mora-López, D. & García-Pinillos, F. Intellectual maturity and physical fitness in preschool children. Pediatr. Int. 58, 450–455. https://doi.org/10.1111/ped.12898 (2016).
Veraksa, A., Tvardovskaya, A., Gavrilova, M., Yakupova, V. & Musálek, M. Associations between executive functions and physical fitness in preschool children. Front. Psychol. 12 (2021). https://doi.org/10.3389/fpsyg.2021.674746
García-Hermoso, A., Izquierdo, M. & Ramírez-Vélez, R. Tracking of physical fitness levels from childhood and adolescence to adulthood: A systematic review and meta-analysis. Transl. Pediatr. 11, 474 (2022).
Haynes, A. et al. Participation in sport in childhood and adolescence: Implications for adult fitness. J. Sci. Med. Sport 24, 908–912 (2021).
China Institute of Sport Science. Fifth National Physical Fitness Monitoring Bulletin. https://www.ciss.cn/zhxw/info/2021/32028.html (2021).
Żegleń, M., Kryst, Ł, Kowal, M. & Woronkowicz, A. Changes in physical fitness among preschool children from Kraków (Poland) from 2008 to 2018. J. Phys. Act. Health 17, 987–994 (2020).
Sigmundsson, H. & Haga, M. Motor competence is associated with physical fitness in four- to six-year-old preschool children. Eur. Early Child. Educ. Res. J. 24, 477–488. https://doi.org/10.1080/1350293X.2016.1164411 (2016).
Mačak, D. et al. The effects of daily physical activity intervention on physical fitness in preschool children. J. Sports Sci. 40, 146–155. https://doi.org/10.1080/02640414.2021.1978250 (2022).
Leppänen, M. et al. Longitudinal physical activity, body composition, and physical fitness in preschoolers. Med. Sci. Sports Exerc. 49 (2017).
Lu, Y. et al. The Association of different sedentary patterns and health-related physical fitness in pre-schoolers. Front. Pediatr. 9 (2022). https://doi.org/10.3389/fped.2021.796417
Fonseca, A. P. L. M., de Azevedo, C. V. M. & Santos, R. M. R. Sleep and health-related physical fitness in children and adolescents: A systematic review. Sleep Sci. 14, 357–365 (2021).
Rollo, S., Antsygina, O. & Tremblay, M. S. The whole day matters: Understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J. Sport Health Sci. 9, 493–510. https://doi.org/10.1016/j.jshs.2020.07.004 (2020).
Tremblay, M. S. et al. Canadian 24-hour movement guidelines for children and youth: An integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab. 41, S311–S327. https://doi.org/10.1139/apnm-2016-0151/M27306437 (2016).
Dumuid, D. et al. The compositional isotemporal substitution model: A method for estimating changes in a health outcome for reallocation of time between sleep, physical activity and sedentary behaviour. Stat. Methods Med. Res. 28, 846–857. https://doi.org/10.1177/0962280217737805 (2019).
Gu, Y. et al. Isotemporal substitution of accelerometer-derived sedentary behavior and physical activity on physical fitness in young children. Sci. Rep. 14, 13544. https://doi.org/10.1038/s41598-024-64389-7 (2024).
Lu, Z. et al. Reallocation of time to moderate-to-vigorous physical activity and estimated changes in physical fitness among preschoolers: A compositional data analysis. BMC Public Health 24, 2823. https://doi.org/10.1186/s12889-024-20290-6 (2024).
Song, H. et al. 24-H movement behaviors and physical fitness in preschoolers: A compositional and isotemporal reallocation analysis. J. Exerc. Sci. Fit. 22, 187–193. https://doi.org/10.1016/j.jesf.2024.03.002 (2024).
Lemos, L. et al. 24-hour movement behaviors and fitness in preschoolers: A compositional and isotemporal reallocation analysis. Scand. J. Med. Sci. Sports 31, 1371–1379. https://doi.org/10.1111/sms.13938 (2021).
Arundell, L., Fletcher, E., Salmon, J., Veitch, J. & Hinkley, T. A systematic review of the prevalence of sedentary behavior during the after-school period among children aged 5–18 years. Int. J. Behav. Nutr. Phys. Act. 13, 1–9 (2016).
You, C. & Cui, Y. Examining the hazards of sedentary behavior: An overview of the risks of screen-based sedentary behavior. Theor. Nat. Sci. 29, 226–236 (2024).
Hu, R., Zheng, H. & Lu, C. The association between sedentary screen time, non-screen-based sedentary time, and overweight in Chinese preschool children: A cross-sectional study. Front. Pediatr. 9, 767608 (2021).
Noggle, A. K. & Stites, M. L. Inclusion and preschoolers who are typically developing: The lived experience. Early Childh. Educ. J. 46, 511–522. https://doi.org/10.1007/s10643-017-0879-1 (2018).
Sdravou, K. et al. Feeding problems in typically developing young children, a population-based study. Children 8, 388 (2021).
Bornstein, D. B., Beets, M. W., Byun, W. & McIver, K. Accelerometer-derived physical activity levels of preschoolers: A meta-analysis. J. Sci. Med. Sport 14, 504–511. https://doi.org/10.1016/j.jsams.2011.05.007 (2011).
Brønd, J. C. & Arvidsson, D. Sampling frequency affects the processing of actigraph raw acceleration data to activity counts. J. Appl. Physiol. 120, 362–369. https://doi.org/10.1152/japplphysiol.00628.2015 (2016).
Martins, C. et al. The combination of three movement behaviours is associated with object control skills, but not locomotor skills, in preschoolers. Eur. J. Pediatr. 180, 1505–1512. https://doi.org/10.1007/s00431-020-03921-z (2021).
Butte, N. F. et al. Prediction of energy expenditure and physical activity in preschoolers. Med. Sci. Sports Exerc. 46, 1216–1226. https://doi.org/10.1249/mss.0000000000000209 (2014).
Lu, C., Shen, T., Huang, G. & Corpeleijn, E. Environmental correlates of sedentary behaviors and physical activity in Chinese preschool children: A cross-sectional study. J. Sport Health Sci. 11, 620–629. https://doi.org/10.1016/j.jshs.2020.02.010 (2022).
Goodlin-Jones, B. L., Sitnick, S. L., Tang, K., Liu, J. & Anders, T. F. The children’s sleep habits questionnaire in toddlers and preschool children. J. Dev. Behav. Pediatr. 29 (2008).
Vale, S. & Mota, J. Adherence to 24-hour movement guidelines among Portuguese preschool children: The prestyle study. J. Sports Sci. 38, 2149–2154. https://doi.org/10.1080/02640414.2020.1775385 (2020).
Cadenas-Sanchez, C. et al. Assessment of cardiorespiratory fitness in preschool children: Adaptation of the 20 metres shuttle run test. Nutr. Hosp. 30, 1333–1343 (2014).
Amado-Pacheco, J. C. et al. Feasibility and reliability of physical fitness tests among colombian preschool children. Int. J. Environ. Res. Public Health 16, 3069 (2019).
Vlahov, E., Baghurst, T. M. & Mwavita, M. Preschool motor development predicting high school health-related physical fitness: A prospective study. Percept. Mot. Skills 119, 279–291. https://doi.org/10.2466/10.25.PMS.119c16z8 (2014).
Madić, D., Sporiš, G. & Kezić, A. Reliability and usefulness of bulb dynamometer for measuring hand grip strength in preschool children. Age (years) 5, 1.04 (2017).
Latorre-Román, P. A. et al. Analysis of dynamic balance in preschool children through the balance beam test: A cross-sectional study providing reference values. Gait Posture 83, 294–299. https://doi.org/10.1016/j.gaitpost.2020.11.004 (2021).
Cadenas-Sanchez, C. et al. Assessing physical fitness in preschool children: Feasibility, reliability and practical recommendations for the PREFIT battery. J. Sci. Med. Sport 19, 910–915. https://doi.org/10.1016/j.jsams.2016.02.003 (2016).
Pawlowsky-Glahn, V., Egozcue, J. J. & Tolosana-Delgado, R. Modeling and Analysis of Compositional Data. (John Wiley & Sons, 2015).
Hron, K., Filzmoser, P. & Thompson, K. Linear regression with compositional explanatory variables. J. Appl. Stat. 39, 1115–1128. https://doi.org/10.1080/02664763.2011.644268 (2012).
Pelclová, J. et al. Are longitudinal reallocations of time between movement behaviours associated with adiposity among elderly women? A compositional isotemporal substitution analysis. Int. J. Obes. 44, 857–864. https://doi.org/10.1038/s41366-019-0514-x (2020).
Reisberg, K., Riso, E.-M. & Jürimäe, J. Associations between physical activity, body composition, and physical fitness in the transition from preschool to school. Scand. J. Med. Sci. Sports 30, 2251–2263. https://doi.org/10.1111/sms.13784 (2020).
Regnier, M. & Cheng, Y. Finally, we can relax: A new generation of muscle models that incorporate sarcomere compliance. Biophys. J. 110, 521–522. https://doi.org/10.1016/j.bpj.2015.12.025 (2016).
Foweather, L. et al. Fundamental movement skills in relation to weekday and weekend physical activity in preschool children. J. Sci. Med. Sport 18, 691–696. https://doi.org/10.1016/j.jsams.2014.09.014 (2015).
Lopes, V. P., Stodden, D. F. & Rodrigues, L. P. Effectiveness of physical education to promote motor competence in primary school children. Phys. Educ. Sport Pedagog. 22, 589–602. https://doi.org/10.1080/17408989.2017.1341474 (2017).
Grgic, J. et al. Health outcomes associated with reallocations of time between sleep, sedentary behaviour, and physical activity: a systematic scoping review of isotemporal substitution studies. Int. J. Behav. Nutr. Phys. Act. 15, 69. https://doi.org/10.1186/s12966-018-0691-3 (2018).
Xiong, X. et al. Association between sleep duration and physical fitness in children aged 3–6 years: A cross-sectional study from China. Int. J. Environ. Res. Public Health 19, 6902 (2022).
Barrios, C. S., Jay, S. Y., Smith, V. C., Alfano, C. A. & Dougherty, L. R. Stability and predictive validity of the parent-child sleep interactions scale: A longitudinal study among preschoolers. J. Clin. Child Adolesc. Psychol. 47, 382–396. https://doi.org/10.1080/15374416.2017.1357125 (2018).
W. H. Organization. Guidelines on Physical Activity, Sedentary Behaviour and Sleep for Children Under 5 Years of Age 36–36 (2019).
Chang, Z. & Wang, S. Study on the isochronous substitution effect of movement behavior on physical health of preschool children. Sports Sci. 40, 50–57. https://doi.org/10.16469/j.css.202010006 (2020).
Pekpak, N. & Altunalan, T. Relationship between screen time with posture and motor coordination in childhood: A descriptive study. Turk. Klin. J. Pediatr. Türk. Klin. Pediatr. Dergisi 33, 41–47. https://doi.org/10.5336/pediatr.2024-101303 (2024).
Howie, E. K., Coenen, P., Campbell, A. C., Ranelli, S. & Straker, L. M. Head, trunk and arm posture amplitude and variation, muscle activity, sedentariness and physical activity of 3 to 5 year-old children during tablet computer use compared to television watching and toy play. Appl. Ergon. 65, 41–50. https://doi.org/10.1016/j.apergo.2017.05.011 (2017).
Webster, E. K., Martin, C. K. & Staiano, A. E. Fundamental motor skills, screen-time, and physical activity in preschoolers. J. Sport Health Sci. 8, 114–121. https://doi.org/10.1016/j.jshs.2018.11.006 (2019).
Kwofie, N. A., Janssen, X. & Reilly, J. J. Associations between sedentary behavior and motor competence in 3- to 4-year-olds: A systematic review. J. Motor Learn. Dev. 1–23. https://doi.org/10.1123/jmld.2023-0079 (2024).
Author information
Authors and Affiliations
Contributions
Conceptualisation: HQS and WCL; methodology: HQS and NKL; software: BRZ and YL; validation: NKL and HQS; formal analysis: HQS; investigation: BRZ and YL; resources: YL and WCL; data curation: YL and BRZ; writing-original draft preparation: HQS, NKL, and WCL; writing-review and editing: HQS and WCL; visualisation: BRZ and HQS; supervision: YL and WCL; project administration: HQS, YL and WCL. All authors have read and agreed to the published version of the manuscript. WCL is corresponding author.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval information, institution and number(s)
This study involves human participants and was approved by the Research Ethics Committee of Beijing Normal University-Hong Kong Baptist University United International College (REC-2021-14). Parents of participants gave written informed consent to participate in the study. This study followed the ethical rules of the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Song, H., Zhang, B., Lu, N. et al. Longitudinal associations between 24-hour movement behaviors and physical fitness in preschoolers: a compositional isotemporal substitution analysis. Sci Rep 15, 32379 (2025). https://doi.org/10.1038/s41598-025-01231-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-01231-8