Abstract
Understanding the economic burden of road trauma (RT) can support healthcare and traffic policy. This prospective cohort study enrolled 1480 RT survivors in British Columbia, Canada. Healthcare and lost productivity costs were estimated in 2023 Canadian dollars. Productivity loss was measured at 2, 4, 6, and 12 months post-injury. Potential predictors included sociodemographic, psychological, medical, and trauma factors. Outcomes were analyzed with a generalized linear model and quantile regression. We found that average healthcare costs during the year following RT were $19,280 (median $3,791). Average lost productivity cost for people employed when injured was $4,390 (median $1,011). Older age, lower health-related quality of life (HRQoL), ≥ 2 comorbidities, Injury Severity Score (ISS) ≥ 9, Glasgow Coma Scale ≤ 13, and torso injury were significantly associated with higher healthcare costs. Employed participants had lower healthcare costs. Older age, being female, lower HRQoL, ≥ 2 comorbidities, ISS ≥ 9, spine/back and upper extremity injuries were significantly associated with higher lost productivity costs. These factors were more strongly associated with greater costs at the upper quantiles. This study highlights the economic burden of RT injuries and identifies factors associated with higher costs.
Similar content being viewed by others
Introduction
Globally, road trauma (RT) accounts for approximately 1.3 million fatalities and 50 million injuries annually1. RT injuries are an important public health problem in Canada and are the leading cause of death among Canadian youth2. Estimates of the annual cost of RT injuries in Canada range from $4.3 billion to $62.9 billion3,4. The burden of RT injuries has changed from early mortality to disability5,6,7. Non-fatal injuries impact economic outcomes due to long-term disability, early retirement, healthcare costs, and increased demands on an already overburdened healthcare system8,9. Even minor RT injuries can result in work absences or reduced productivity10,11,12.
Understanding the cost of RT helps translate the burden of RT into economic terms and guide policy-maker decisions about allocating resources to RT prevention initiatives. The economic costs of non-fatal injuries include both direct medical costs and indirect costs due to lost productivity. Medical costs, such as emergency department (ED) visits, hospitalizations, medications, and rehabilitation costs, have grown over the last decades due to an increasing number of non-fatal injuries13 and higher costs of healthcare. Productivity costs are based on absenteeism (time off work) and presenteeism (reduced productivity) at paid and unpaid work14,15. To date, few studies on the costs of RT injuries are available9,16,17,18,19,20,21,22,23,24,25,26,27 and there is little information about the long-term economic costs of RT9,17,18,19. Furthermore, many studies focus exclusively on direct costs and neglect costs related to lost productivity16,17,20,21.
Understanding cost estimates following RT injury and identifying predictors of high cost are essential for evaluating existing policies and identifying potential areas for cost saving. Knowing predictors of high RT injury costs may enable traffic policymakers to develop prevention programs or policies that target costly injury scenarios. This information may also help healthcare providers reduce the economic burden by identifying “high cost” patients and targeting them for early intervention such as focused rehabilitation programs, specialized therapy or increased community supports. Also, return to work and compensation policies may be improved with a better understanding of the characteristics of these patients. Previous studies have reported that older age, female sex, higher injury severity, and more comorbidities are associated with higher healthcare costs19,20. Male sex and higher injury severity are associated with higher long-term lost productivity costs19. Injury severity, admission to the intensive care unit, and length of hospital stay are associated with hospitalization costs16. The cost of motorcycle, bicycle, and pedestrian injuries is higher than for other road users16,17,19,28. Injuries to the spine, lower extremities or head are associated with higher healthcare costs20,22.
The current study aims to estimate healthcare and lost productivity costs in the year following injury among RT survivors (including all road users and injury severity levels). Additionally, we investigated the relationship between various sociodemographic, psychological, medical, and trauma-related factors and costs using a generalized linear model (GLM) to identify the significant cost-drivers of RT injuries. We also used quantile regression to study how significant factors impact costs across different quantiles of cost distribution representing both lower-cost and higher-cost patients.
Methods
Participants and procedures
This study enrolled RT injury survivors from three British Columbia (BC) emergency departments (EDs) between July 2018 and March 2020 and followed them for one year. Detailed methods have been previously outlined29. All road users involved in a motor vehicle crash (cyclists, pedestrians, motorcyclists, and motor vehicle drivers and passengers) with all injury severity levels were eligible if they were at least 16 years old and entered the ED within 24 h following the crash. Non-BC residents and those who died within 30 days were excluded. Baseline interviews were conducted in-person by a research assistant during ED visits or hospital admissions, or by telephone in some cases. Interviews were completed within one week of injury except for in patients admitted to hospital with severe injuries who were not capable of being interviewed within this timeframe; over 98% of the interviews were conducted within two weeks after the injury and all interviews were completed within 35 days. Follow-up interviews were conducted by telephone, online survey, self-filled paper questionnaire or in-person (using a translator if required) depending on participant preference. For those unable to complete interviews independently (e.g., cognitive disability, language barrier), a proxy either assisted the participant or completed the questionnaire on the participant’s behalf. Injury type and severity was determined through medical chart reviews. Non-English speakers were interviewed through a translator (e.g., family) or multilingual research assistant in Cantonese, French, Korean, Mandarin, Punjabi, and Vietnamese (reflecting the common languages spoken in Greater Vancouver). Participants provided informed consent for interviews and for access to their healthcare information. The study protocol was reviewed and approved by the University of British Columbia clinical research ethics board (certificate H18-00284). All methods were performed in accordance with the relevant guidelines and regulations.
Measures
Costs, including healthcare and productivity costs, over a year following RT were estimated for each participant. Data on hospital and outpatient healthcare use during the year following the index visit were obtained from Population Data BC, a data repository containing individual-level longitudinal health records for all residents of BC30. De-identified patient data are compiled from several datasets linked by BC Personal Health Number. These include the Discharge Abstracts Database, which contains administrative and clinical data on patients admitted to hospital (including day surgery), long-term care, rehabilitation and other types of care; the National Ambulatory Care Reporting System, which contains ED visits and ambulance usage; the Medical Services Plan (MSP) Payment Information File, which contains data on medical services provided by practitioners in the province; and PharmaNet, which contains all prescriptions for drugs and medical supplies dispensed from BC community pharmacies and hospital outpatient pharmacies (See Data Statement). The Resource Intensity Weight (RIW) method was used to estimate hospital costs. RIWs are the relative case weights for Case Mix Groups (CMG) or the Day Procedure Group (DPG)/Comprehensive Ambulatory Care Classification System (CASC) used to measure the intensity of resource use associated with different diagnostic, surgical procedure, and demographic characteristics of an individual31,32. We calculated hospital costs per case by multiplying the case-specific RIW by the cost per weighted case provided by the Canadian Institute for Health Information (CIHI).
The Productivity Cost Questionnaire (iPCQ) was used to measure costs from productivity loss33. We collected this questionnaire at 2, 4, 6, and 12 months post-injury. The iPCQ assesses productivity losses from absenteeism, presenteeism, and losses associated with unpaid work. It also includes general questions regarding participants’ work status such as the weekly hours of paid work and the number of working days per week. The absenteeism module identifies the occurrence and length of short-term and long-term absenteeism from paid work. Absences beginning before the four-week recall period are considered long-term absences. The presenteeism module identifies reduced productivity at work. The unpaid work module asks participants if they performed less unpaid work because of physical or psychological problems. The productivity losses for the recall period were extrapolated to adjust for the length of period between two consecutive measurements. Productivity costs for a year following RT injury were calculated using the human capital approach34. The costs of productivity were calculated by multiplying the missed work or lost productivity hours by the average hourly wage rate obtained from Statistics Canada’s CANSIM database for a person in the same age group, sex, and interview time in BC35. The costs of unpaid productivity losses were calculated by multiplying the total hours of lost productivity by the average hourly wage for household care at the interview time in BC36. The iPCQ also asks participants about their productivity 4 weeks prior to the accident. Participants who reported pre-injury absence from work, were not in the working population (aged 16–64), or did not have paid employment were excluded from the calculation of lost productivity costs. Costs were adjusted to 2023 Canadian dollars (CAD) using the Statistics Canada Consumer Price Index37.
Baseline interviews assessed participants’ sociodemographic, psychological, medical, and trauma-related characteristics. Sociodemographic factors included age, sex, employment status, living situation, level of education, ethnicity, and years living in Canada. Psychological factors included pre-injury general somatic symptom severity, pain catastrophizing and psychological distress measured with the Patient Health Questionnaire-15 (PHQ-15)38, the Pain Catastrophizing Scale39, and the Patient Health Questionnaire-4 (PHQ-4)40,41, respectively. Higher scores on these scales indicate greater symptom severity, higher levels of catastrophic thinking, and more severe depression and/or anxiety, respectively. Pre-injury health-related quality of life (HRQoL) was evaluated using the Short Form 12 survey (SF-12)42, where higher scores indicate better health. The number of pre-injury comorbidities was the only medical factor measured at baseline. Comorbidities included eye disease, arthritis, diabetes, respiratory disease, heart disease, hypertension, stroke, epilepsy, kidney disease, psychiatric disorders, and other diseases self-reported by participants during the interviews. Trauma-related factors included ED visited, crash time, road user type, Injury Severity Score (ISS)43,44, Glasgow Coma Scale (GCS)45, and injury location.
Statistical analysis
Descriptive statistics were employed to summarize participant characteristics and cost outcomes including healthcare and lost productivity. The cost outcome distributions displayed a high level of skewness (see Supplementary Figures S1-S2). We used a GLM as the main analysis to identify predictors of cost outcomes and then quantile regression to quantify their effects across different quantiles of cost distribution.
We ran a GLM with a gamma distribution and log-link function to examine the association between potential predictors and mean healthcare costs. A GLM with a Tweedie distribution was used to examine the association between potential predictors and mean productivity costs. The Tweedie distribution can simultaneously support zeros and continuous nonnegative values46,47, which was the observed distribution for productivity costs in our data (Supplementary Figure S2). Quantile regression is a relatively new approach for analyzing healthcare costs. It has no assumptions about the outcome distribution and is robust to outliers; it also has more power to discover differences in the upper or lower tails of the distribution as coefficient estimates are generated by weighting different portions of the sample48,49. Some studies have reported that the effect of independent variables (predictors) on healthcare costs are different in low-cost patients than in high-cost patients50,51. We used quantile regression to assess the association of potential predictors with different specified quantiles of healthcare, and productivity, costs. We fitted quantile regression for the specified quantiles of 0.1, 0.25, 0.5, 0.75, and 0.90.
The results of multivariable GLM and quantile regression were presented as the relative difference in mean costs (exp(β)) with 95% confidence intervals and β with 95% confidence intervals, respectively. The initial multivariable GLM included all predictors that were significant at the 0.2 level in univariate analysis. The final GLM was constructed using a backward elimination algorithm based on the Akaike Information Criterion (AIC). Furthermore, the same set of variables selected in the final GLM were included in the multivariable quantile regression. Statistical significance was considered at the 0.05 level. All statistical analyses were performed using R version 4.0.5.
Missing data
The missing numbers of days lost or lost productivity were assumed to be zero. If a patient’s weekly paid work hours were missing, the national averages by sex were used: 38 h weekly for males and 34 h weekly for females52 The Markov Chain Monte Carlo (MCMC) method was used to impute missing values for baseline covariates. We conducted a sensitivity analysis comparing analysis of data with imputations (Tables 4–5) to the analysis without imputations (Supplementary Tables S1-S2).
Results
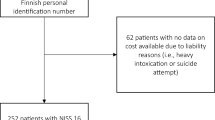
Figure 1 shows enrolled patients and exclusions for each outcome. Of 1480 participants, 800 (54.1%) were male, 981 (66.3%) employed, 154 (10.4%) students, and 200 (13.5%) retired; healthcare data was available on 1372 participants. The mean age was 43.1 years (range: 16 to 103 years) and the median ISS was 3.0 (range: 0 to 66) (Table 1). Table 2 shows detailed cost outcomes. Descriptive statistics of cost outcomes by participant characteristics, along with their univariate analyses are presented in Table 2. The differences in baseline characteristics between participants included in the analyses of healthcare and productivity loss costs and those not included are presented in Supplementary Tables S3-S4. For the healthcare cost analysis, baseline characteristics were largely similar. For the productivity cost analysis, more pronounced differences were observed due to the study’s focus on participants engaged in paid employment.
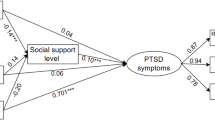
Heatmap visualizations of regression coefficients for significant predictors in the regression quantile models of healthcare costs (left plot) and productivity costs (right plot). The colors in each square of the plots correspond to the values of the regression coefficients in either the healthcare or productivity cost quantile regression models (Tables 4–5). This figure allows for the observation of patterns in the magnitude of coefficients across different quantiles using color gradients. HRQoL: health-related quality of life; SF-12: Short Form 12 survey; ISS: injury severity score.
Healthcare costs
The 1372 RT patients for whom we had healthcare records incurred healthcare costs of $26,452,367 during the year after their injury (mean=$19,280; SD = 50,066). The median healthcare cost was $3,791, with an IQR of $13,306-1,715 = 11,591 (Table 2). According to the multivariable GLM (Table 4), mean healthcare costs were significantly higher for older patients, those with lower baseline HRQoL (SF-12 < 100) and those with ≥ 2 comorbidities. Patients with higher ISS and lower GCS scores also had higher healthcare costs: mean healthcare costs were 9.2 times higher for patients with ISS ≥ 16 compared to those with ISS ≤ 3 (exp(β) = 9.23; 95% CI = 6.95–12.42). Mean healthcare costs were also significantly higher for patients with torso injuries compared to others. Being employed was associated with lower healthcare costs.
Quantile regression analysis (Table 4) showed that older age and lack of employment were more strongly associated with higher healthcare costs among patients who are already high-cost. For example, compared to young patients (aged ≤ 34), elderly patients (aged ≥ 65) cost $16,095.48 (95% CI=$9,468.06-$22,722.90) more among high-cost patients (90 th quantile) and $1,780.11 (95% CI=$1,296.43-$2,263.80) more among low-cost patients (10 th quantile). The results suggest that lower HRQoL and higher ISS are also more strongly associated with higher healthcare costs at the upper quantiles (patients with higher healthcare costs) than at the lower quantiles. The effect of having ≥ 2 comorbidities was also more pronounced for patients at the upper quantiles of healthcare costs compared with those at the lower quantiles (β=$539.44; 95% CI=$239.37-$840.36 for the 10 th quantile; β=$13,979.09; 95% CI=$9,866.95-$18,092.98 for the 90 th quantile). According to the quantile regression analysis, healthcare costs were significantly higher at all quantiles for GCS ≤ 8. However, GCS of 9–13 was significantly associated with higher costs at the 50 th, 75 th, and 90 th quantiles. Torso injuries had a significant impact on the distribution of healthcare costs only at the 50 th quantile.
Productivity costs
The lost productivity costs for the 928 patients who were employed at time of injury totaled $4,073,964, with a mean of $4,390 (SD = 8,053). The median cost of lost productivity was $1,011 with an IQR of 5,162-0 = 5,162 (Table 2). According to multivariable GLM, mean cost of lost productivity was 53% higher for females than for males (Exp(β) = 1.53; 95% CI = 1.22–1.91) (Table 5). Patients aged 35–64 years had higher lost productivity costs than younger patients. Mean lost productivity costs were 2.2 times higher for patients with lower baseline HRQoL (SF-12 < 100) compared to those with higher HRQoL (SF-12 ≥ 100) (exp(β) = 2.20; 95% CI = 1.66–2.90). ISS ≥ 9 and ≥ 2 comorbidities were also associated with higher productivity costs compared to ISS ≤ 3 and no comorbidities, respectively. Mean productivity costs were significantly higher for patients with spine/back injury and upper extremity injury compared to others.
In the quantile regression analysis (Table 5), the estimated β for sex, age, and HRQoL increased from the 50 th to the 90 th quantile. However, the β for age was not statistically significant across these specified quantiles. For example, women incur $5,455.48 (95% CI=$2,901.56-$8,008.02) more than men among high-cost patients (90 th quantile) but only $696.72 (95% CI=$210.05-$1,183.04) more among medium-cost patients (50 th quantile). The impact of multiple comorbidities on the distribution of lost productivity costs was more pronounced at the upper quantiles compared to the lower quantiles (β=$1,806.31; 95% CI=$1,083.62-$2,528.72 for the 50 th quantile; β=$4,347.06; 95% CI=$553.60-$8,140.66 for the 90 th quantile). For ISS 9–15 and ISS ≥ 16, the distribution of lost productivity costs at the higher quantiles was more impacted by ISS than at the lower quantiles. Sustaining spine/back and upper extremity injuries had a greater impact on lost productivity costs distribution at the upper quantiles compared to the lower quantiles; however, these factors were not significant across all quantiles. Figure 2 shows the magnitude of coefficients across different quantiles for significant predictors of healthcare and productivity costs from both quantile regression models.
Discussion
In this multicentre, prospective cohort study of 1480 RT survivors with relatively minor injuries (median ISS = 3.0), we found that the costs of healthcare and productivity loss in the year after RT were substantial; the mean healthcare costs were estimated at CAD $19,280 (median=$3,791) and the mean lost productivity costs at CAD $4,390 (median=$1,011). We also found that measures of frailty and injury severity were associated with higher healthcare and productivity costs; and that most risk factors were more strongly associated with higher costs among high-cost patients. These findings suggest that healthcare costs could be reduced by investing in programs that improve traffic safety. Although the study is set within the context of the Canadian healthcare system—where publicly funded healthcare influences both cost structures and access—many of the key insights regarding cost drivers are likely to be relevant across healthcare systems. Nonetheless, we acknowledge that the absolute costs may not generalize to other countries due to differences in healthcare funding models, service pricing, and reimbursement practices.
The high costs in our study align with findings from other countries. In Saudi Arabia (2017), RT injury cost the hospital US $20,800 (CAD $26,832) on average16. In Australia (2010–2011), RT patients with persistent midline cervical tenderness generated mean healthcare costs of AUD $10,153 (CAD $10,369) over a 12-month period21. In the Netherlands (2017), mean healthcare costs for nonfatal RT injuries were €8,200 (CAD $11,972) and mean lost productivity costs were €5,900 (CAD $8,614) in the two years post injury19. Papadakaki et al. reported that, in 2013-24, mean healthcare costs of RT injury over a year were €734 (CAD $1,072) in Greece, €2266 (CAD $3,308) in Germany, and €5,697 (CAD $8,318) in Italy; mean lost productivity costs were €11,599 (CAD $16,934) in Greece, €7963 (CAD $11,625) in Germany, and €13,681 (CAD $19,974) in Italy53. Papadakaki’s higher estimates for lost productivity are likely because, unlike our study, Papadakaki also accounted for changes in employment status of a family member53.
We found healthcare costs were significantly higher in RT survivors with older age, lower pre-injury HRQoL, multiple comorbidities, higher ISS, lower GCS, and torso injury. We also found that older age, female sex, lower pre-injury HRQoL, having multiple comorbidities, higher ISS, spine/back and upper extremity injuries were all significantly associated with higher lost productivity costs. Quantile regression analyses revealed that the impact of these variables was more pronounced on the distribution of costs at higher quantiles compared to lower quantiles. In other words, these variables had a bigger impact on costs for the more expensive patients than for less expensive patients. For instance, among patients with HRQoL < 100, healthcare costs increased by $638, $858, $1346, $5146, and $9144 at 10 th, 25 th, 50 th, 75 th, and 90 th quantiles, respectively (Table 4). These findings highlight the heterogeneity of healthcare utilization within the population and provide detailed information on predictors of RT injury costs within each subpopulation. Identifying predictors of higher costs in high-cost subgroups is important for health policymakers because targeting these patients for cost containment measures, such as tailored interventions to reduce disability and increase return to paid and unpaid work, could lead to substantial savings.
Our findings align with previous research indicating that older patients have higher healthcare costs19,20, productivity costs19, and total (healthcare + productivity) costs9 Alghnam reported that the effect of older age on healthcare costs distribution was greater at the upper quantiles16. This may be explained by age-related factors that exacerbate RT injury and lead to prolonged recovery times, extended hospital stays, and consequently, increased costs54. In contrast to our findings, Vlegel and Naumann reported that males incurred higher lost productivity costs compared to females19,55. Despite men having higher average wages than women in Canada, this discrepancy may be explained by the fact that women in our sample reported more hours of lost productivity in unpaid work. Consistent with a prior study of adult trauma patients, we found that lower pre-injury HRQoL was associated with higher healthcare costs56. Our study also highlighted the significance of multiple comorbidities in increasing healthcare and productivity costs. This finding aligns with the adverse effects of poor pre-injury health on the recovery process and return-to-work post-injury57,58. Unsurprisingly, similar to previous research16,19,20,22,59, we found that higher ISS was associated with higher healthcare and lost productivity costs. Like our study, previous studies have also reported that healthcare costs were higher for patients with lower GCS16,17. These findings are likely because individuals with higher ISS or lower GCS require extended stays in hospitals that offer elevated levels of care.
This study has notable strengths, including its prospective design spanning 12 months with five rounds of data collection on lost productivity. We used validated scales to assess HRQoL, somatic symptom severity, psychological distress, and pain catastrophizing. Use of administrative data to estimate healthcare costs is another strength. Moreover, to improve generalizability, no limitations were placed on road user type, injury severity level, or language. It is important to recognize some limitations as well. First, self-reported pre-injury HRQoL, somatic symptom severity, and psychological distress may be subject to recall bias. Second, our cost estimates may underestimate the total economic burden of RT injury: We did not include private-pay healthcare costs, legal costs, property damage costs, life years lost costs, and compensation costs relating to pain, stress, and suffering. Further, we did not assess the long-term healthcare costs beyond the first year; injured persons often have increased long-term healthcare utilization60. Older individuals and those experiencing significant pain, who likely utilize more healthcare resources, may have been less inclined to participate in the study. Third, we used average national hourly wages instead of the participants’ actual wages to estimate lost productivity costs.
Conclusions
This study highlights the substantial economic burden of RT injuries, even among survivors with relatively minor physical trauma. Our findings demonstrate that certain patient characteristics—such as older age, lower pre-injury HRQoL, multiple comorbidities, and greater ISS—not only predict higher healthcare and productivity costs but do so more strongly among the highest-cost individuals. These insights underscore the importance of early identification of at-risk individuals to target interventions that could yield meaningful cost savings. Beyond quantifying costs, our results point to broader implications: improving pre-injury health and minimizing ISS through traffic safety and prevention strategies could substantially reduce both personal and system-wide economic burdens. Moreover, applying advanced statistical methods such as quantile regression allowed us to uncover differential effects across the cost spectrum—information that traditional mean-based analyses would miss. This level of detail offers actionable evidence for policymakers to design targeted prevention and rehabilitation programs, especially for high-cost subgroups.
Data availability
The data that support the findings of this study are available from PopDataBC but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the corresponding author upon reasonable request and with permission of PopDataBC (contact the data access lead for PopDataBC at: dataaccess@popdata.bc.ca). Access to data provided by the Data Stewards is subject to approval but can be requested for research projects through the Data Stewards or their designated service providers. The following data sets were used in this study: Fee for Service (MSP); Discharge Abstract Database (DAD); National Ambulatory Care Reporting System (NACRS); Pharmanet. You can find further information regarding these data sets by visiting the PopData project webpage at: https://my.popdata.bc.ca/project_listings/21-100/collection_approval_dates. All inferences, opinions, and conclusions drawn in this publication are those of the author(s), and do not reflect the opinions or policies of the Data Steward(s).
References
World Health Organization. Global Road Safety Report 2018 [June 17, 2018]. Available from: https://www.who.int/publications/i/item/9789241565684
Kitchen, P., Kaida, L., Akhtar-Danesh, N. & Williams, A. Unintentional injury deaths among youth in Ontario, Canada from 2000 to 2015: rates are falling but there are caveats. Can. Geographer/Le Géographe Canadien. 65 (3), 255–266 (2021).
Parachute The Cost of Injury in Canada (Parachute), (2015).
Vodden, K., Smith, D., Eaton, F. & Mayhew, D. Analysis and Estimation of the Social Cost of Motor Vehicle Collisions in Ontario. N0779 (Transport Canada), (2007).
Polinder, S. et al. A systematic review of studies measuring health-related quality of life of general injury populations. BMC Public. Health. 10, 1–13 (2010).
Rissanen, R., Ifver, J., Hasselberg, M. & Berg, H. Y. Quality of life following road traffic injury: the impact of age and gender. Qual. Life Res. 29 (6), 1587–1596 (2020).
Goniewicz, K., Goniewicz, M., Pawłowski, W. & Fiedor, P. Road accident rates: strategies and programmes for improving road traffic safety. Eur. J. Trauma Emerg. Surg. 42, 433–438 (2016).
Connelly, L. B. & Supangan, R. The economic costs of road traffic crashes: Australia, States and territories. Accid. Anal. Prev. 38 (6), 1087–1093 (2006).
Zakeri, R., Nosratnejad, S., Sadeghi-Bazargani, H., Dalal, K. & Yousefi, M. The economic burden of road traffic injuries until one-year after hospitalization: A survey study. Accid. Anal. Prev. 163, 106459 (2021).
Hours, M. et al. Outcomes one year after a road accident: results from the ESPARR cohort. Accid. Anal. Prev. 50, 92–102 (2013).
Murgatroyd, D. F., Harris, I. A., Tran, Y., Cameron, I. D. & Murgatroyd, D. Predictors of return to work following motor vehicle related orthopaedic trauma. BMC Musculoskelet. Disord. 17, 171 (2016).
Gopinath, B. et al. Prognostic indicators of social outcomes in persons who sustained an injury in a road traffic crash. Injury 46 (5), 909–917 (2015).
Global Burden of Disease Collaborative Network. Global burden of disease study 2019 (GBD 2019) results. Seattle, United States: institute for health metrics and evaluation (IHME). [November, 2023]. Available from: http://ghdx.healthdata.org/gbd-results-tool
Zhang, W., Bansback, N. & Anis, A. H. Measuring and valuing productivity loss due to poor health: A critical review. Soc. Sci. Med. 72 (2), 185–192 (2011).
Krol, M., Brouwer, W. & Rutten, F. Productivity costs in economic evaluations: past, present, future. Pharmacoeconomics 31 (7), 537–549 (2013).
Alghnam, S. et al. Healthcare costs of road injuries in Saudi Arabia: A quantile regression analysis. Accid. Anal. Prev. 159, 106266 (2021).
Alghnam, S. et al. Cost of healthcare rehabilitation services following road traffic injuries: results from a Level-I trauma center in Saudi Arabia. J. Fam. Commun. Med. 29 (1), 1 (2022).
Scholten, A. C., Polinder, S., Panneman, M. J., Van Beeck, E. F. & Haagsma, J. A. Incidence and costs of bicycle-related traumatic brain injuries in the Netherlands. Accid. Anal. Prev. 81, 51–60 (2015).
van der Vlegel, M., Haagsma, J. A., de Munter, L., de Jongh, M. A. & Polinder, S. Health care and productivity costs of non-fatal traffic injuries: a comparison of road user types. Int. J. Environ. Res. Public Health. 17 (7), 2217 (2020).
Chini, F., Farchi, S., Camilloni, L., Giarrizzo, M. L. & Giorgi Rossi, P. Health care costs and functional outcomes of road traffic injuries in the Lazio region of Italy. Int. J. Injury Control Saf. Promotion. 23 (2), 145–154 (2016).
Ackland, H. M. et al. Health resource utilisation costs in acute patients with persistent midline cervical tenderness following road trauma. Injury 43 (11), 1908–1916 (2012).
Nguyen, H. et al. The economic burden of road traffic injuries: evidence from a provincial general hospital in Vietnam. Inj. Prev. 19 (2), 79–84 (2013).
Air, T. M., McFarlane, A. C. & Psychother, D. Posttraumatic stress disorder and its impact on the economic and health costs of motor vehicle accidents in South Australia. J. Clin. Psychiatry. 64 (2), 175–181 (2003).
Bastida, J. L., Aguilar, P. S. & González, B. D. The economic costs of traffic accidents in Spain. J. Trauma. Acute Care Surg. 56 (4), 883–889 (2004).
Banstola, A., Kigozi, J., Barton, P. & Mytton, J. Economic burden of road traffic injuries in Nepal. Int. J. Environ. Res. Public Health. 17 (12), 4571 (2020).
García-Altés, A. & Puig-Junoy, J. What is the social cost of injured people in traffic collisions? An assessment for Catalonia. J. Trauma. Acute Care Surg. 70 (3), 744–750 (2011).
García-Altés, A. & Pérez, K. The economic cost of road traffic crashes in an urban setting. Inj. Prev. 13 (1), 65–68 (2007).
Olesen, A. V., Petersen, K. D. & Lahrmann, H. S. Attributable hospital costs, home care costs and risk of long-term sickness benefits following traffic injuries by road user type. J. Transp. Health. 22, 101104 (2021).
Shum, L. K., Chan, H., Erdelyi, S., Pei, L. X. & Brubacher, J. R. Predictors of poor health and functional recovery following road trauma: protocol of a British Columbian inception cohort study. BMJ Open. 11 (4), e049623 (2021).
PopulationdataBC. Population data BC 2023 [December, 2023]. Available from: www.popdata.bc.ca.
Pink, G. H. & Bolley, H. B. Physicians in health care management: 3. Case mix groups and resource intensity weights: an overview for physicians. CMAJ: Can. Med. Association J. 150 (6), 889 (1994).
Pink, G. H. & Bolley, H. B. Physicians in health care management: 4. Case mix groups and resource intensity weights: physicians and hospital funding. CMAJ: Can. Med. Association J. 150 (8), 1255 (1994).
Bouwmans, C. et al. The iMTA productivity cost questionnaire: a standardized instrument for measuring and valuing health-related productivity losses. Value Health. 18 (6), 753–758 (2015).
Pritchard, C. & Sculpher, M. Productivity Costs: Principles and Practice in Economic Evaluation (Office of Health Economics, 2000).
Statistics Canada. Table: 14-10-0063-01 Employee wages by industry, monthly, unadjusted for seasonality. 2023 [November, 2023]. Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1410006301
Statistics Canada. Table: 14-10-0328-01 Job vacancies, proportion of job vacancies and average offered hourly wage by selected characteristics, quarterly, unadjusted for seasonality. 2023 [November, 2023]. Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1410032801
Statistics Canada. Consumer Price Index, Tables 18-10-0005-01 Consumer Price Index, annual average, not seasonally adjusted. 2023 [November, 2023]. Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1810000501
Kocalevent, R-D., Hinz, A. & Brähler, E. Standardization of a screening instrument (PHQ-15) for somatization syndromes in the general population. BMC Psychiatry. 13, 91 (2013).
Sullivan, M. J., Bishop, S. R. & Pivik, J. The pain catastrophizing scale: development and validation. Psychol. Assess. 7 (4), 524–532 (1995).
Lowe, B. et al. A 4-item measure of depression and anxiety: validation and standardization of the patient health Questionnaire-4 (PHQ-4) in the general population. J. Affect. Disord. 122 (1–2), 86–95 (2010).
Kroenke, K., Spitzer, R. L., Williams, J. B. W. & Lowe, B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics 50 (6), 613–621 (2009).
Ware, JE. SF-36 health survey. Manual and interpretation guide. Health Inst. 6 (1-6), 22 (1993).
Osler, T., Rutledge, R., Deis, J. & Bedrick, E. ICISS: an international classification of disease-9 based injury severity score. J. Trauma. 41 (3), 380–386 (1996).
Barnard, R. T., Loftis, K. L., Martin, R. S. & Stitzel, J. D. Development of a robust mapping between AIS 2 + and ICD-9 injury codes. Accid. Anal. Prev. 52, 133–143 (2013).
Matis, G. & Birbilis, T. The Glasgow coma Scale–a brief review past, present, future. Acta Neurol. Belg. 108 (3), 75–89 (2008).
Kurz, C. F. Tweedie distributions for fitting semicontinuous health care utilization cost data. BMC Med. Res. Methodol. 17, 1–8 (2017).
Smyth, G. K. (ed) Regression analysis of quantity data with exact zeros. Proceedings of the Second Australia-Japan Workshop on Stochastic Models in Engineering, Technology and Management, Gold Coast, Australia; : Citeseer. (1996).
Koenker, R. & Bassett, G. Jr Regression quantiles. Econometrica: J. Econometric Soc. 46, 33–50 (1978).
Sherwood, B., Wang, L. & Zhou, X. H. Weighted quantile regression for analyzing health care cost data with missing covariates. Stat. Med. 32 (28), 4967–4979 (2013).
Yen, C-R. et al. An analysis of patient variables that influence intravenous patient-controlled analgesic use of morphine with quantile regression. J. Am. Soc. Anesthesiologists. 112 (3), 688–695 (2010).
Moreira, S. & Barros, P. P. Double health insurance coverage and health care utilisation: evidence from quantile regression. Health Econ. 19 (9), 1075–1092 (2010).
Statistics Canada. Table: 14-10-0320-02 Average usual hours and wages by selected characteristics, monthly, unadjusted for seasonality. [November, 2023]. Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1410032002
Papadakaki, M. et al. Hospitalization costs and estimates of direct and indirect economic losses due to injury sustained in road traffic crashes: results from a one-year cohort study in three European countries (The REHABILAID project). Trauma 19 (4), 264–276 (2017).
Yadollahi, M., Pazhuheian, F., Jamali, K. & Hadi Niakan, M. Hospitalization due to traffic accidents among the elderly, Shiraz, 2018; mortality, severity, and injury pattern. Archives Trauma. Res. 9 (3), 106–110 (2020).
Naumann, R. B., Dellinger, A. M., Zaloshnja, E., Lawrence, B. A. & Miller, T. R. Incidence and total lifetime costs of motor vehicle–related fatal and nonfatal injury by road user type, united States, 2005. Traffic Inj. Prev. 11 (4), 353–360 (2010).
de Munter, L. et al. Prognostic factors for medical and productivity costs, and return to work after trauma. PLoS One. 15 (3), e0230641 (2020).
Papic, C. et al. Factors associated with long term work incapacity following a non-catastrophic road traffic injury: analysis of a two-year prospective cohort study. BMC Public. Health. 22 (1), 1498 (2022).
De Munter, L., Polinder, S., Havermans, R. J., Steyerberg, E. W. & de Jongh, M. A. Prognostic factors for recovery of health status after injury: a prospective multicentre cohort study. BMJ Open. 11 (1), e038707 (2021).
Hoang, H. et al. The costs of traumatic brain injury due to motorcycle accidents in Hanoi, Vietnam. Cost Eff. Resource Allocation. 6 (1), 1–7 (2008).
Cameron, C. M., Kliewer, E., Purdie, D. M. & McClure, R. J. Long term health outcomes after injury in working age adults: a systematic review. J. Epidemiol. Commun. Health. 60 (4), 341 (2006).
Funding
This work was supported by the Canadian Institutes of Health Research (Grant # 461108).
Author information
Authors and Affiliations
Contributions
The protocol for this study was developed by JRB, HC, SB and JAS. SM analyzed data. SM and JRB wrote the first draft of the manuscript. JAT, HC, DRH and JRB oversaw participant recruitment. All authors helped interpret study findings and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Momenyan, S., Chan, H., Taylor, J.A. et al. Healthcare and productivity costs among Canadian road trauma survivors over the year following injury. Sci Rep 15, 17723 (2025). https://doi.org/10.1038/s41598-025-01233-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-01233-6