Abstract
This study evaluates the effectiveness of ultrasound-guided fine needle aspiration biopsy (US-FNAB) in assessing additional positive axillary lymph node (ALN) metastasis following sentinel lymph node biopsy (SLNB) in clinically ALN-negative or N1 cases, aiming to refine patient management. A multi-center, retrospective analysis included 7617 patients with cT1-2 and cN0-1, who underwent US-FNAB for ALN and proceeding to SLNB or axillary lymph node dissection (ALND). Metastatic patterns were assessed, particularly focusing on correlations with positive FNAB results and additional ALN metastasis found during ALND, with statistical significance evaluated. Of those undergoing SLNB, 97.5% exhibited macrometastasis. In the SLNB-only group, 2.4% had 3 and more than 3 positive lymph node, compared to 19.2% in the SLNB & ALND group (P < 0.01). Among ALND patients, 63.3% had positive nodes, significantly higher in those with positive FNAB (91.9% vs. 22.8%, P < 0.001). Additionally, 40.9% were found to have additional positive ALNs in patients who underwent ALND following positive SLNB, with rates significantly higher in those with positive FNAB (60.3% vs. 35.4%, P < 0.001). LVI positivity, pT2-3, SLNR > 50% and positive FNAB were independent predictors of additional ALN metastasis in patients undergoing ALND after positive SLNB (P < 0.05). The proportion of additional positivity escalated with the number of positive SLNs. US-FNAB significantly improves the detection of additional ALN metastasis, guiding more effective strategy for ALN surgical decision-making. Our findings support the incorporation of US-FNAB into clinical practice to improve patient stratification and optimize treatment outcomes in early-stage breast cancer management.
Similar content being viewed by others
Introduction
For patients with breast cancer, it is often necessary to assess the staging of axillary lymph nodes (ALNs), as it serves as a strong prognostic indicator and decisive factor in formulating cancer treatment plans1,2. Traditional axillary lymph node dissection (ALND) has been used for staging, but currently, the frequency and scope of sentinel lymph node biopsy (SLNB) have increased as an alternative for early-stage cancer patients3,4. Notably, while SLNB can avoid unnecessary ALND in order to reduce complications associated with ALND, it is still an invasive procedure that may pose inconvenience for some patients who require two-stage surgeries5. Therefore, a technique that reliably assesses the likelihood of additional positive ALN retention after SLNB would have significant clinical benefits. Methods or minimally invasive surgeries used to determine ALN status would allow for SLNB to be performed if evidence confirms the absence of additional positive ALN metastasis. Conversely, patients who are found to have additional positive ALN metastases would proceed directly to ALND.
In terms of preoperative assessment for additional ALN positive metastasis, the sensitivity of physical examination is relatively low, ranging between 34–76%6,7. In various studies, when combined with ultrasound-guided fine-needle aspiration biopsy (US-FNAB) of suspicious lymph nodes, ultrasound (US) examination of ALNs shows higher diagnostic accuracy8,9. The sensitivity and specificity of US in assessing ALN metastasis are reported to be between 36 and 92% and 69–100%, respectively10,11. Building upon this, the further inclusion of US-FNAB may increase specificity to between 93–100%8,12,13.
However, most previous studies on US-FNAB involved small-scale, single-center patient populations, and the specific likelihood of additional ALN positive metastasis post-SLNB remains unclear. Thus, a multicenter study involving a larger patient population is required. The aim of our study is to evaluate the effectiveness of US-FNAB in assessing the incidence of additional ALN positive metastasis following SLNB in clinically ALN-negative or palpable ALN cases, in order to enhance clinical screening for patients who should exclusively undergo SLNB or require ALND.
Patients and methods
Patients
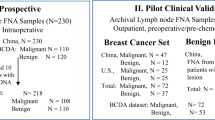
This retrospective study analyzed data from the Shanghai Jiao Tong University-Breast Cancer Database (SJTU-BCDB), a multicenter database. We identified consecutive patients diagnosed with clinical stage T1-2 N0-1M0 invasive breast cancer who were over 18 years old at the time of diagnosis and underwent ultrasound-guided fine-needle aspiration biopsy (US-FNAB) followed by surgical intervention between January 2009 and December 2023. Clinical nodal staging (cN0/cN1) was determined via physical examination and ultrasound, with cN1 defined by palpable or sonographically suspicious lymph nodes (cortical thickness > 3 mm, non-hilum blood flow, or irregular morphology). PET-CT was not routinely utilized in this cohort. The exclusion criteria included: (1) male patients; (2) diagnosis of carcinoma in situ without invasive disease; (3) synchronous bilateral breast cancer; and (4) history of prior or concurrent malignant diseases.
Comprehensive clinicopathological data were collected, which included age, menopausal status, type of surgical intervention, histopathology, tumor grade, pathologic tumor size, estrogen receptor (ER) status, progesterone receptor (PR) status, human epidermal growth factor receptor-2 (HER2) status, Ki-67 expression, total number of sentinel lymph nodes (SLNs) excised, and the number of positive SLNs. Patients were classified into two subgroups based on histological characteristics: invasive ductal carcinoma (IDC) and other histological types (HST). The Sentinel Lymph Node Ratio (SLNR) was defined as the number of positive SLNs divided by the total number of SLNs excised.
Ethical review
The study protocol received full approval from the Ethics Committee of Ruijin Hospital and was conducted in strict accordance with the ethical principles outlined in the 2013 revision of the Declaration of Helsinki. Given the retrospective nature of the investigation and the complete anonymization of all patient data, the Ethics Committee of Ruijin Hospital granted a waiver of informed consent requirement (Clinical Ethics Approval Number: [2020] 309).
Statistical analysis
Statistical analyses were performed using SPSS version 26 (SPSS, Inc., Chicago, IL, USA). Differences in the incidence of positive SLNs or additional ALNs between the negative and positive US-FNAB groups, as well as differences in clinical and pathological characteristics between the negative and positive ALN groups, were assessed using Chi-square or Fisher’s exact tests. Univariable and multivariate logistic regression was performed to calculate adjusted odds ratios (ORs) for factors associated with additional ALN metastasis. A p-value of < 0.05 was considered statistically significant.
Results
Number of lymph nodes in SLNB surgery: SLNB only vs. SLNB & ALND
A total of 4,481 patients underwent SLNB surgery, among which 2,820 underwent SLNB only, and 1,661 completed ALND after SLNB. The median number of lymph nodes in the SLNB only group and the SLNB & ALND group was 4, with an interquartile range of 3 to 6 (Fig. 1A).
Number and metastasis of lymph nodes in SLNB surgery. (A) The median number of lymph nodes in the SLNB only group and the SLNB & ALND group. (B) The proportions of patients with different number of positive SLNs in positive SLNB population. (C) The proportions of patients with different number of positive SLNs in negative FNAB group of positive SLNB population. (D) The proportions of patients with different number of positive SLNs in positive FNAB group of positive SLNB population. (E) The comparison of the proportion of patients with lymph node metastases between negative FNAB and positive FNAB group in SLNB only population. (F) The comparison of the proportion of patients with lymph node metastases between negative FNAB and positive FNAB group in SLNB & ALND population.
Lymph node metastasis during positive SLNB surgery
During the SLNB surgery, 97.5% of patients had macrometastasis. In the positive SLNB population, the proportions of patients with 1, 2, and ≥ 3 positive lymph nodes were 84.6%, 13.0% and 2.4%, respectively, in SLNB only group, while 55.5%, 25.3%, and 19.2%, respectively, in the SLNB & ALND group (Fig. 1B). In the SLNB & ALND group, compared to negative FNAB, positive FNAB showed a higher proportion of patients with ≥ 3 lymph node metastases (25.5% vs. 16.8%, P = 0.014), while no statistically significant difference was observed in the SLNB only group (4.1% vs. 2.0%, P = 0.381) (Fig. 1C-F).
Occurrence of positive lymph nodes during ALND surgery
Among all patients who underwent ALND, 63.3% had positive lymph nodes found during the procedure. The proportion of positive ALNs was higher in patients with positive FNAB compared to negative FNAB (91.9% vs. 22.8%, P < 0.001) (Fig. 2A). Similar results were observed in the clinical cN0 (pos. vs. neg. FNAB: 90.0% vs. 18.7%, P < 0.001) and cN1 (pos. vs. neg. FNAB: 94.0% vs. 34.8%, P < 0.001) subgroups (Fig. 2B-C).
Occurrence of additional positive lymph nodes in patients undergoing ALND after SLNB
Of those who underwent ALND following negative SLNB, 6.3% were found to have additional positive ALNs. Compared to negative FNAB, a higher proportion of patients with positive FNAB were found to have additional positive ALNs (22.6% vs. 5.2%, P < 0.001) (Fig. 3A). Similar results were noted in the cN0 and cN1 subgroups, with higher percentage of additional positive ALNs in positive FNAB group (cN0, pos. vs. neg. FNAB: 13.9% vs. 4.5%, P = 0.006; cN1, pos. vs. neg. FNAB: 42.1% vs. 8.0%, P < 0.001) (Fig. 3B-C).
Percentage of additional positive lymph nodes in patients undergoing ALND after SLNB. (A) The proportion of additional positive ALNs in patients undergoing ALND after negative SLNB. (B) The proportion of additional positive ALNs in cN0 patients undergoing ALND after negative SLNB. (C) The proportion of additional positive ALNs in cN1 patients undergoing ALND after negative SLNB. (D) The proportion of additional positive ALNs in patients undergoing ALND after positive SLNB. (E) The proportion of additional positive ALNs in cN0 patients undergoing ALND after positive SLNB. (F) The proportion of additional positive ALNs in cN1 patients undergoing ALND after positive SLNB.
Among patients who underwent ALND following positive SLNB, 40.9% were found to have additional positive ALNs. Compared to negative FNAB, positive FNAB group was observed to have higher proportion of additional positive ALNs (60.3% vs. 35.4%, P < 0.001) (Fig. 3D). Similar results were noticed in the cN0 and cN1 subgroups, displaying higher percentage of additional positive ALNs in positive FNAB group (cN0, pos. vs. neg. FNAB: 60.8% vs. 32.6%, P < 0.001; cN1, pos. vs. neg. FNAB: 59.2% vs. 41.9%, P = 0.026) (Fig. 3E-F). Further analysis indicated that LVI positivity (49.7%), pT2-3 (44.5%), SLNR > 50% (67.2%), and positive FNAB (60.2%) were associated with a higher rate of additional positive ALNs in ALND after positive SLNB (P < 0.05) (Table 1). Multivariable logistic regression analysis identified the following independent predictors of additional ALN metastasis: positive FNAB (OR = 2.78, 95% CI: 1.81–4.22, P < 0.001), SLNR > 50% (OR = 4.08, 95% CI: 2.73–6.10, P < 0.001), LVI positivity (OR = 1.82, 95% CI: 1.20–2.75, P = 0.005), and pT2-3 tumor size (OR = 1.56, 95% CI: 1.04–2.34, P = 0.031) (Table 1).
The relationship between at least one additional positive lymph node metastasis in ALND after SLNB and the number of positive SLN results
In the patient who underwent ALND with at least one additional positive lymph node, the proportion of patients with additional positive lymph nodes increased with the number of positive SLNs, particularly when there were 3 or ≥ 4 positive SLNs, where the proportions were 67.9% and 75.8%, respectively (P < 0.001) (Fig. 4A). Similar results were observed in the negative FNAB and positive FNAB subgroups. Notably, compared to negative FNAB subgroup, a higher proportion of additional positive ALNs was found in the positive FNAB subgroup, where the proportions for 2, 3, and ≥ 4 positive SLNs were 65.8%, 77.3%, and 90.9%, respectively (P < 0.001) (Fig. 4A).
In the clinical cN0 subgroup, similar results were observed. When there were 3 and ≥ 4 positive SLNs, the proportions of additional positive ALNs were 66.0% and 76.7%, respectively (P < 0.01) (Fig. 4B). However, compared to negative FNAB, a higher proportion of additional positive ALNs was observed in positive FNAB subgroup, displaying when there were 2, 3 or ≥ 4 positive SLNs, there will be 68.6%, 80.0% and 92.8% percentage of additional positive ALN (P < 0.001) (Fig. 4B).
In the clinical cN1 subgroup, when there were 2, 3 and ≥ 4 positive SLNs, the proportion of additional positive ALNs was 52.1%, 67.8% and 73.7%, respectively (P < 0.05) (Fig. 4C). The same results were observed in the negative FNAB and positive FNAB subgroups. Remarkably, compared to negative FNAB subgroup, a higher proportion of additional positive ALNs was noticed in the positive FNAB population when there were ≥ 2 positive SLNs (P < 0.001) (Fig. 4C).
Discussion
Although SLNB is less invasive than ALND, it has some drawbacks, such as insufficient comprehensive assessment of ALNs for some patients and the inconvenience of requiring two-stage surgeries5. If the ALN metastatic status can be determined in advance, patients can directly undergo a one-stage axillary surgery, avoiding multiple procedures. Therefore, employing a more reliable and minimally invasive method to evaluate ALNs in cancer patients would provide more assist in accurate axillary surgery.
Our study shows that patients who underwent ALND after SLNB had a higher proportion of three or more SLN metastases compared to those who only underwent SLNB, particularly in the subgroup with positive FNAB. Simultaneously, the proportion of positive ALNs was higher in the positive FNAB subgroup across the entire population, including the cN0 and cN1 groups, indicating that the results of FNAB contribute to the assessment of ALN status.
The NSABP B-32 study showed that the probability of non sentinel ALN positivity in SLN negative patients is less than 10%. In SLN negative patients, ALND can be safely avoided, thereby successfully avoiding or reducing complications caused by axillary lymph node dissection14,15. For patients with positive SLNs, previous meta-analyses have found that 53% of patients have ALN metastasis outside the sentinel, while for patients with SLN micrometastasis, the probability of non SLN metastasis decreases to 20%16. In patients with isolated tumor cells in SLNs, the metastasis rate to non SLNs decreases to 12%16,17,18. In our study, the proportion of positive ALNs post-negative SLNB was 6.3%, which consistent with the result of NSABP B-32. However, the patient with positive FNAB manifested higher possibility of non sentinel ALN positivity, even though the negative outcome of SLNB. About 40.9% of patients undergoing ALND following positive SLNB had additional positive ALNs, also showing rates significantly higher in those with positive FNAB. Consequently, a positive FNAB result provides a signal that more active intervention is required in the management of ALNs.
The proportion of additional positivity escalated with the number of positive SLNs, particularly in the cN0 population with positive FNAB, where the proportions of additional positive ALNs were 68.8%, 80.0%, and 92.8% for 2, 3, and ≥ 4 positive SLNs, respectively. The result suggests that in cN0 patients with positive FNAB, when there are two or more positive SLNs, ALND should be performed more actively. For cN0 patients with negative FNAB, ALND is recommended when there are three or more positive SLNs, consistent with the findings of the Z0011 study19. Houssami et al. (2007) similarly highlighted the role of preoperative US-FNAB in identifying patients with high nodal burden20, advocating for its integration to streamline surgical planning. Our findings reinforce this approach, particularly in cN1 patients where FNAB positivity strongly predicts additional ALN metastases. In the cN1 population, when there are two or more positive SLNs, more than half of the proportion presenting additional positive ALNs, regardless of whether the FNAB result is positive or negative. Therefore, patients with cN1 should undergo ALND more proactively, especially when exiting two or more positive SLNs, or patients should recommend to undergo preoperative neoadjuvant chemotherapy. In summary, this once again highlights the strong guiding role of FNAB positive results in ALN management.
Several studies have reported that patients with negative FNAB cytology should undergo SLNB4,21,22,23. Conversely, other studies suggest that the proportion of patients who can be exempt from SLNB ranges from 1–26%11,24. Our study indicates that among cN0 patients with positive FNAB, the proportion of positive ALNs during ALND can be as high as 90.0%, compared to 18.7% in negative FNAB patients (Fig. 2B). More detail analyses in cN0 patients who underwent SLNB followed by ALND showing that the proportion of those with positive ALN metastasis in the positive FNAB group was 13.9% and 60.8% when SLNB result is negative and positive, respectively, while in the negative FNAB group, it was 4.5% and 32.6%, respectively. Similar results were observed in the cN1 population, where the proportion of patients with positive ALN metastasis after SLNB in the positive FNAB group was 42.1% and 59.2% when SLNB result is negative and positive, respectively. These results suggest that SLNB remains the best choice for FNAB negative patients, but patients with positive FNAB should be further evaluated with other indicators to identify those who may be eligible to exempt SLNB and proceed directly to ALND.
It has been reported that US-FNAB is more sensitive in detecting LN metastasis in patients with larger primary cancers, as lymph node metastasis tends to be higher in larger breast cancer cohorts25. Our study demonstrates that FNAB positivity, SLNR > 50%, LVI positivity, and larger tumor size (pT2-3) are independent predictors of additional ALN metastasis in patients undergoing ALND after positive SLNB. The multivariable analysis revealed that patients with positive FNAB had a 2.75-fold increased risk of additional ALN involvement, while SLNR > 50% was associated with the highest risk. These findings align with previous studies highlighting the role of SLNR and FNAB in axillary staging but further quantify their predictive value in a large multicenter cohort. The strong association between LVI positivity and additional ALN metastasis underscores the biological aggressiveness of tumors with LVI, which may facilitate nodal spread. Similarly, the correlation between pT2-3 tumors and residual ALN involvement supports the notion that larger tumors are more likely to harbor occult nodal disease. These factors collectively provide a robust framework for preoperative risk stratification, enabling clinicians to tailor surgical interventions more effectively.
In conclusion, US-FNAB is a useful tool for the preoperative assessment of axillary lymph nodes in breast cancer patients. It serves as a reliable method for evaluating axillary metastasis and is valuable in planning appropriate axillary management for patients with early breast cancer.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Wang, G. et al. Prognostic significance of occult lymph node metastases in breast cancer: a meta-analysis. BMC Cancer ; 21. (2021).
Bryan, R. M., Mercer, R. J., Bennett, R. C. & Rennie, G. C. Prognostic factors in breast cancer and the development of a prognostic index. J. Br. Surg. 73, 267–271 (1986).
Goyal, A., Newcombe, R. G., Chhabra, A. & Mansel, R. E. Morbidity in breast Cancer patients with Sentinel node metastases undergoing delayed axillary lymph node dissection (ALND) compared with immediate ALND. Ann. Surg. Oncol. 15, 262–267 (2007).
Fraile, M. et al. Julián Fj Fau - Fusté F, Llatjós M Fau - Castellà E,. Sentinel node biopsy as a practical alternative to axillary lymph node dissection in breast cancer patients: an approach to its validity. Annals of Oncology. ; 11: 701-5. (2000).
Purushotham, A. D. et al. Fau - Myles JP, Myles Jp Fau - Duffy SW,. Morbidity after sentinel lymph node biopsy in primary breast cancer: results from a randomized controlled trial. Journal of Clinical Oncology. ; 23: 4312-21. (2005).
van Nijnatten, T. J. A. et al. Differences in axillary ultrasound protocols among prospective de-escalating axillary surgical staging trials in clinically node negative early breast cancer patients. Eur. J. Radiol. ; 181. (2024).
Oruwari, J. U. N., Chung, M. A., Koelliker, S., Steinhoff, M. M. & Cady, B. Axillary staging using ultrasound-guided fine needle aspiration biopsy in locally advanced breast cancer. Am. J. Surg. 184, 307–309 (2002).
Zhuang, L. et al. Predicting axillary metastasis in breast cancer using lymphatic contrast-enhanced ultrasound-guided fine-needle aspiration of one lymph node. Br. J. Radiol. ; 97. (2024).
Moore, A. et al. Distinct lymph nodal sonographic characteristics in breast cancer patients at high risk for axillary metastases correlate with the final axillary stage. Br. J. Radiol. 81, 630–636 (2008).
Verbanck, J. et al. Value of axillary ultrasonography and sonographically guided puncture of axillary nodes: A prospective study in 144 consecutive patients. J. Clin. Ultrasound. 25, 53–56 (1997).
Jain, A. et al. The role of Ultrasound-Guided Fine-Needle aspiration of axillary nodes in the staging of breast Cancer. Ann. Surg. Oncol. 15, 462–471 (2007).
Winkler, N. A. O. et al. Comparison of diagnostic sensitivity and Procedure-Related pain of concurrent Ultrasound-guided Fine-needle aspiration and Core-needle biopsy of axillary lymph nodes in patients with suspected or known breast Cancer. J. Breast Imaging. 5, 436–4444 (2023).
Kuenen-Boumeester, V. et al. Ultrasound-guided fine needle aspiration cytology of axillary lymph nodes in breast cancer patients. A preoperative staging procedure. Eur. J. Cancer. 39, 170–174 (2003).
Veronesi, U. et al. A randomized comparison of Sentinel-Node biopsy with routine axillary dissection in breast Cancer. N. Engl. J. Med. 349, 546–553 (2003).
Krag, D. N. et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 11, 927–933 (2010).
Kim, T., Giuliano, A. E. & Lyman, G. H. Lymphatic mapping and Sentinel lymph node biopsy in early-stage breast carcinoma. Cancer 106, 4–16 (2005).
Cserni, G. et al. Meta-analysis of non-sentinel node metastases associated with micrometastatic Sentinel nodes in breast cancer. Br. J. Surg. 91, 1245–1252 (2004).
van Deurzen, C. H. et al. Non-sentinel lymph node metastases associated with isolated breast cancer cells in the Sentinel node. J. Natl Cancer Inst. 100, 1574–1580 (2008).
Giuliano, A. E. et al. Locoregional recurrence after Sentinel lymph node dissection with or without axillary dissection in patients with Sentinel lymph node metastases. Ann. Surg. 252, 426–433 (2010).
Houssami, N., Ciatto, S., Turner, R. M., Cody, H. S. & Macaskill, P. Preoperative Ultrasound-Guided needle biopsy of axillary nodes in invasive breast Cancer. Ann. Surg. 254, 243–251 (2011).
Holwitt, D. M. et al. Scientific presentation award: the combination of axillary ultrasound and ultrasound-guided biopsy is an accurate predictor of axillary stage in clinically node-negative breast cancer patients. Am. J. Surg. 196, 477–482 (2008).
Baruah, B. P., Goyal, A., Young, P., Douglas-Jones, A. G. & Mansel, R. E. Axillary node staging by ultrasonography and fine-needle aspiration cytology in patients with breast cancer. Br. J. Surg. 97, 680–683 (2010).
Sallout, L. et al. Fine‐needle aspiration biopsy of axillary lymph nodes: A reliable diagnostic tool for breast cancer staging. Cancer Cytopathol. 132, 103–108 (2023).
Bonnema, J. et al. Ultrasound‐Guided aspiration biopsy for detection of nonpalpable axillary node metastases in breast Cancer patients: new diagnostic method. World J. Surg. 21, 270–274 (1997).
Koelliker, S. L., Chung, M. A., Mainiero, M. B., Steinhoff, M. M. & Cady, B. Axillary lymph nodes: US-guided Fine-Needle aspiration for initial staging of breast Cancer—Correlation with primary tumor size. Radiology 246, 81–89 (2008).
Acknowledgements
We would like to express our gratitude to Juanjuan Zheng from the Medical Record Department of Quanzhou First Hospital affiliated with Fujian Medical University for providing statistical assistance. This work was supported by the Startup Fund for scientific research, Fujian Medical University (Grant number: 2021QH1237), the Natural Science Foundation Project of Fujian Province (2023J011775), and the High Level Talents Innovation and Entrepreneurship Project of Quanzhou City (2023C007YR).
Author information
Authors and Affiliations
Contributions
DB-C and ZP-H designed the study. YJ-L analyzed the data, wrote and revised the manuscript. MR-D and SY-L analyzed the data, organized photos and revised the manuscript. Y-J, YJ-N, YQ-H and W-F helped with the data analysis, visualization and manuscript modification. All authors have read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, Y., Dong, M., Liao, S. et al. A multi-center retrospective analysis of ultrasound-guided fine needle aspiration biopsy for detecting additional positive axillary node metastasis in early breast cancer. Sci Rep 15, 18485 (2025). https://doi.org/10.1038/s41598-025-01353-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01353-z
Keywords
This article is cited by
-
Efficacy of Ultrasonography in Early Detection of Breast Cancer: A Systematic Review
SN Comprehensive Clinical Medicine (2026)