Abstract
This study investigates the relationship between absolute eosinophil count (AEC) and eosinophil percentage (EOS%) with response rates to immune checkpoint inhibitors (ICIs) in recurrent or metastatic head and neck squamous cell carcinoma (R/M HNSCC) patients. The analysis included data from R/M HNSCC patients treated with ICIs at Second Xiangya Hospital (2016–2021), assessing baseline characteristics, tumor specifics, immune-related adverse events, AEC, and EOS%. The correlation between these factors and ICI response rates was evaluated using logistic regression, while survival outcomes were analyzed through Kaplan-Meier curves and Cox models. Among 74 patients, 59 had low AEC and 15 high, with 53 presenting low EOS% and 21 high. Low AEC (44.07% response rate) and EOS% (47.17%) yielded better responses compared to high levels (40% and 33.33%, respectively). Median overall survival was longer for low AEC (22.63 vs. 18.00 months, P < 0.001) and low EOS% (22.07 vs. 19.73 months, P = 0.02). Both low AEC and EOS% correlated with improved survival odds (3.85 and 2.41 times respectively). Lower AEC and EOS% are independently linked to better survival and increased ICI response rates in R/M HNSCC patients, indicating their potential as predictors for ICI treatment outcomes.
Similar content being viewed by others
Introduction
Head and neck squamous cell carcinoma (HNSCC) represents a diverse set of tumors primarily originating from the oral cavity, oropharynx, hypopharynx, and larynx1. The incidence of HNSCC exhibits regional disparities and is commonly linked to exposure to tobacco carcinogens, excessive alcohol consumption, or both2. Current treatment approaches for HNSCC encompass surgical interventions, radiotherapy, chemotherapy, immunotherapy, either as monotherapies or in combination3. Despite advancements in preventive measures, diagnostic techniques, and therapeutic interventions, the 5-year survival rate for locally advanced HNSCC remains stagnant at approximately 50%, showing no significant improvement over the last decade4. The prognosis for recurrent or metastatic (R/M) HNSCC is notably bleak, with a median overall survival (OS) of roughly one year5.
Extensive research suggests that immune checkpoint inhibitors (ICIs) hold significant promise as standard treatment options for R/M HNSCC patients who have experienced treatment failure with platinum-based therapy6. Nivolumab and pembrolizumab, anti-PD1 antibodies, were approved for second-line R/M HNSCC based on CheckMate-141 and KEYNOTE-040 trials7,8. Pembrolizumab was also approved for first-line use in combination with platinum and 5-FU, and as monotherapy in PD-L1-positive patients, following KEYNOTE-0489. While ICIs present a promising avenue for treatment, the objective response rate (ORR) remains approximately 20% in first- and second-line R/M HNSCC patients not selected based on cancer PD-L1 expression10,11. Currently, the predictive significance of PD-L1 scoring remains inconsistent in research reports, and clinical practice has also observed that patients with high PD-L1 scores often exhibit poorer responses to PD-1 antibody therapy, while those with low PD-L1 scores tend to respond more sensitively9. Therefore, exploring alternative biomarkers becomes increasingly necessary.
Eosinophils are a mature and multifunctional class of white blood cells that regulate various innate and adaptive immune cells by releasing a multitude of cytokines and growth factors, such as CCL5, CCL6, CCL9, CXCL10, TGF-β and VEGF, through degranulation12,13. Eosinophils play a crucial role in the immune microenvironment’s regulation of tumorigenesis and progression. In various human tumors, such as melanoma14,15, colorectal cancer16,17, hepatocellular carcinoma18, and prostate cancer19, eosinophils exhibit anti-tumorigenic effects. The prognosis of cancer patients undergoing immunotherapy has been significantly associated with eosinophils levels. In patients with non-small cell lung cancer(NSCLC)20,21,22, metastatic melanoma23,24,25,26, and renal cell carcinoma27, peripheral blood eosinophilia is typically linked to longer survival. Conversely, in T-cell leukemia/lymphoma, peripheral blood acid granulocytes serve as an unfavorable prognostic factor28. In the treatment with ICIs, the relationship between peripheral blood absolute eosinophil count (AEC) and treatment response, as well as immune-related adverse events, has attracted increasing attention. Studies have found that in patients with NSCLC receiving ICIs therapy, a baseline AEC ≥ 0.125 × 10^9/L is significantly associated with the risk of ICI-related pneumonitis20. Moreover, patients with higher AEC levels may achieve better clinical outcomes in ICIs treatment. Additionally, the ORR and progression-free survival (PFS) in the high AEC group are significantly better than those in the low AEC group20. Despite the fact that indicators such as the Neutrophil-to-Lymphocyte Ratio (NLR), Lymphocyte-to-Monocyte Ratio (LMR), and Platelet-to-Lymphocyte Ratio (PLR) have been extensively studied and confirmed to be closely related to the tumor immune microenvironment and prognosis29,30, these indicators primarily focus on the dynamic balance of cell subsets directly involved in the anti-tumor immune response, such as neutrophils and lymphocytes. In comparison, eosinophils, as granulocytes with unique immune regulatory functions, have not yet fully elucidated the mechanisms of action of their absolute count and percentage (EOS%) in HNSCC. To elucidate the role of eosinophils in immunotherapy for patients with R/M HNSCC, we investigated the prognostic significance of pre-immunotherapy peripheral blood eosinophil levels in these patients. The objective is to offer more precise and personalized treatment approaches for clinical practice.
Materials and methods
Study participants
The study enrolled patients with R/M HNSCC who received anti-PD1 antibody monotherapy, including pembrolizumab, nivolumab, camrelizumab31,32, tislelizumab33, toripalimab34, and sintilimab35, at the Second Xiangya Hospital of Central South University from 2016 to 2021.The follow-up period concluded on June 30, 2023. Patients were excluded from the study if they met any of the following criteria: (1) incomplete or missing medical records, including baseline characteristics, treatment details, follow-up outcomes, or necessary laboratory results such as peripheral eosinophil counts; (2) loss to follow-up or death before undergoing post-treatment imaging to evaluate clinical response; (3) prior treatment with ICIs or other immunotherapies, or concurrent participation in other clinical trials or experimental therapies; (4) presence of primary tumors of unknown origin; (5) severe uncontrolled comorbidities including cardiac, renal, or hepatic dysfunction, or active infections such as HIV or hepatitis, or autoimmune diseases requiring systemic treatment; (6) history of another primary malignancy within the past 5 years; (7) age under 18 years or pregnancy or lactation at the time of enrollment; (8) inability to obtain informed consent such as deceased patients without legal representatives or poor compliance with study requirements. This retrospective study, conducted at a single center, was authorized by the Institutional Review Board (IRB) of Second Xiangya Hospital, Central South University (Ethics Approval No. 228, 2022) and adhered to the principles of the Declaration of Helsinki. Our study was designed as a retrospective study using only de-identified clinical data, which is in accordance with the exemption criteria of the U.S. Code of Federal Regulations, Title 45, Part 46 (specifically, 45 CFR § 46.104(d)(4): Secondary research uses of identifiable private information if the information is recorded without identifiers.). Due to the retrospective nature of the study, IRB of Second Xiangya Hospital waived the need of obtaining informed consent. Personal data were anonymized to ensure confidentiality throughout data analysis and reporting.
Clinical information
Baseline characteristics, such as age, gender, smoking and alcohol status, primary tumor site, tumor grade, T-stage, N-stage, M-stage, immune-oncology (I-O), immune-related adverse events, peripheral blood AEC and EOS%, were extracted from the electronic medical records of 74 patients with R/M HNSCC who were undergoing immunotherapy. All patients included in this study had an ECOG PS of 1. The baseline peripheral blood AEC was assessed as a baseline parameter immediately prior to the initial administration of PD-1 inhibitors on Cycle 1 Day 1 (C1D1). Based on the baseline AEC values, patients were stratified into low and high AEC subgroups. Patients with an AEC greater than or equal to 0.3*10^9/L were categorized into the high AEC group, while those below this threshold were assigned to the low AEC group. Patients with an EOS% greater than or equal to 2.9% were categorized into the high EOS% group, while those below this threshold were assigned to the low EOS% group.
Efficacy was evaluated according to Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1. Response was defined as the proportion of patients achieving partial response (PR), progressive disease (PD), or stable disease (SD) for at least 3 months from baseline. OS was defined as the time from treatment initiation to death from any cause. Disease status post-treatment was assessed through review of clinical progress records and radiological reports.
Statistical analysis
All data analyses were performed using R, version 4.0.5 and SPSS, version 19.0. Optimal cut-off values were determined using maximally selected log-rank statistics. Continuous variables were presented as means with standard deviations or medians with interquartile ranges (IQRs) for normally and non-normally distributed data, respectively. Categorical variables were reported as numbers and percentages. Student’s t-test and Mann-Whitney U test were used for inter-group comparisons of continuous variables, while Pearson’s χ2 test was used for categorical variables. The Kaplan-Meier method was used to generate unadjusted survival curves and risk tables. Univariable logistic regression was conducted to calculate odds ratios for Clinical Response to Immunotherapy by AEC. Univariable and Stepwise multivariate Cox analysis were conducted to calculate Hazard ratios (HRs) to represent the risk for death. Clinically important factors, including age (≤ 60 vs. >60 years) and smoking status (never vs. former or current) were considered. Statistical significance was set at p < 0.05.
Results
Demographics and clinical characteristics
A total of 74 patients were enrolled in this study, and their demographic and clinical characteristics are summarized in Table 1. The median age of the cohort was 53.5 years (range: 28–76 years), with a predominance of male patients (66/74, 89.19%). The oral cavity was the most common primary tumor site (48/74, 64.86%). Based on AEC, 59 patients (59/74, 79.73%) were classified as low AEC, while 15 patients (15/74, 20.27%) were classified as high AEC. Similarly, 53 patients (53/74, 71.62%) had low EOS%, and 21 patients (21/74, 28.38%) had high EOS%. The distribution of PD-1 inhibitors by type was as follows: Pembrolizumab (25/74, 33.78%), Nivolumab (2/74, 2.70%), Camrelizumab (20/74, 27.03%), Nivolumab + Camrelizumab (1/74, 1.35%), Tislelizumab (13/74, 17.57%), Toripalimab (7/74, 9.46%), and Sintilimab (6/74, 8.11%).
Clinical response to immunotherapy by AEC
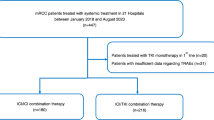
Patients with PD and SD exhibited higher AEC and EOS% compared to those with PR (Fig. 1A-B). Specifically, the median(range) AEC and EOS% in the PD group were 0.14 (0.00–0.90) and 1.00% (0.00–8.50%), respectively. In the SD group, the median(range) AEC and EOS% were 0.18 (0.02–1.30) and 2.00% (0.03–10.20%), respectively. In contrast, the PR group had median(range) values of 0.125 (0.00–0.50) for AEC and 0.90% (0.00–14.00%) for EOS%.
However, no statistically significant differences were observed among the three groups (Fig. 1C-D). Further analysis revealed no significant differences in AEC or EOS% between the PD and PR groups (AEC: p = 0.722; EOS%: p = 0.899) or between the SD and PR groups (AEC: p = 0.124; EOS%: p = 0.129). These results suggest that baseline eosinophil levels may not be significantly associated with treatment response in this cohort.
The partial response rate to immunotherapy was numerically higher in patients with low AEC or EOS% (AEC: 26/59, 44.07%; EOS%: 25/53, 47.17%) compared to those with high AEC or EOS% (AEC: 6/15, 40%; EOS%: 7/21, 33.33%) (Table 2). The odds ratios (ORs) for ICIs partial response rate in patients with low AEC or EOS% versus high AEC or EOS% were [AEC: OR (95% CI) 1.18 (0.38–3.92); EOS%: OR (95% CI) 1.79 (0.64–5.37)], indicating a trend towards higher response rates in the low AEC or EOS% groups.
Overall survival
Patients with low AEC or EOS% demonstrated longer median OS compared to those with high AEC or EOS% (AEC: 22.63 vs. 18 months; EOS%: 22.07 vs. 19.73 months). Furthermore, patients with low AEC or EOS% exhibited a significantly reduced risk of mortality following treatment with ICIs compared to those with high AEC or EOS% (AEC: P < 0.001; EOS%: P = 0.02) (Fig. 2A-B).
Univariable and multivariable analyses
Univariate Cox proportional regression analysis revealed that patients with low AEC had a 3.85-fold higher hazard ratio for OS compared to patients with high AEC (95% CI: 1.69–8.78, P = 0.001). Similarly, patients with low EOS% had a 2.41-fold higher hazard ratio for OS compared to patients with high EOS% (95% CI: 1.12–5.16, P = 0.02). Stepwise multivariate Cox analysis demonstrated that patients with low AEC or EOS% remained significantly associated with higher hazard ratios for OS (AEC: adjusted HR: 3.96, 95% CI: 1.72–9.15, P = 0.001; EOS%: adjusted HR: 2.64, 95% CI: 1.21–5.74, P = 0.014). None of the other variables in this study showed a significant association with OS except for age (Table 3).
Discussion
Our study effectively determined that peripheral blood AEC and EOS% serve as a prognostic factor for OS in R/M HNSCC undergoing treatment with ICIs. Low AEC or EOS% was significantly associated with better OS in R/M HNSCC patients. The study suggests that tumor tissue PD-L1 expression levels are associated with improved efficacy of ICIs in R/M HNSCC36,37. However, AEC and EOS% can be obtained through clinical testing, making it more convenient than PD-L1 detection. To our knowledge, this is the first study in R/M HNSCC patients demonstrating the prognostic value of baseline peripheral blood AEC and EOS% for those receiving immunotherapy.
Our multivariate analysis results indicate that baseline peripheral blood AEC and EOS% are reliable predictors of disease progression and mortality rates in R/M HNSCC. This finding underscores the potential importance of a patient’s immune system characteristics prior to immunotherapy initiation in predicting treatment response and survival outcomes. AEC and EOS%, as markers of the immune system, may reflect the immune system’s status and its response to the tumor microenvironment (TME)38,39. Eosinophils have been proposed as predictive factor and may even serve as terminal effector cells after ICIs therapy, especially with anti-CTLA-4 and anti-PD-1 antibodies23,40,41,42. Therefore, analyzing baseline AEC enhance our understanding of a patient’s immune status and aid in identifying individuals who may derive significant benefit from immunotherapy.
Eosinophils may influence tumor progression either directly through interactions with tumor cells or indirectly by modulating the TME, and their presence has been correlated with patient prognosis in various cancer types43. However, the role of eosinophils appears to be context-dependent, differing significantly between peripheral blood circulating immune cells and tumor-infiltrating cells, as well as across cancer types. Recent studies have demonstrated that in patients with advanced or metastatic NSCLC, a high baseline AEC is associated with better outcomes following nivolumab therapy20,21. Similarly, in metastatic melanoma, a baseline AEC ≥ 1.5% has been linked to favorable OS34. These findings suggest that peripheral blood eosinophils may serve as a positive prognostic marker in certain cancers during ICIs treatment.
In contrast, our study observed that patients with high AEC or EOS% had significantly shorter OS compared to those with lower levels. This divergence may be attributed to the unique immunological characteristics of HNSCC, where eosinophils might play a distinct role in modulating the TME or systemic immune response. For instance, in solid tumors such as cervical cancer, oral squamous cell carcinoma, and T-cell leukemia/lymphoma, tumor-infiltrating eosinophils have been reported to exhibit pro-tumorigenic functions and are often associated with poor prognosis28,44,45,46,47,48,49,50. Increased eosinophil infiltration in cervical cancer lesions, along with higher eosinophil proportions, has been linked to a weaker anti-tumor response, facilitating tumor invasion and leading to lower OS rates44. Similarly, in oral squamous cell carcinoma, dense eosinophilic infiltration has been identified as an unfavorable prognostic factor48. Utsunomiya et al. further reported that an elevated peripheral blood AEC was an independent adverse prognostic factor in adult T-cell leukemia/lymphoma patients28. These findings align with our observations in HNSCC, suggesting that the role of eosinophils may vary depending on the cancer type and the specific immune context. The discrepancy between our results and those from studies in NSCLC or melanoma highlights the need for further investigation into the dual roles of eosinophils in different cancer types. Potential explanations for this divergence include differences in tumor biology, the composition of the TME, and the systemic immune response to ICI therapy.
Emerging evidence suggests that the precise localization of eosinophils in and around tumors could be a crucial factor in the development and advancement of both solid tumors and hematologic malignancies. Eosinophils have been implicated in promoting angiogenesis through the secretion of various cytokines including VEGF, basic fibroblast growth factor, IL-6, IL-8, GM-CSF, platelet-derived growth factor, TGF-β, and CCL1143,44,45. They also interact with tumor-associated macrophages to enhance cytokine release, particularly under conditions of local hypoxia46. Studies using eosinophil-deficient mouse models suggest that eosinophils are associated with increased risk of experimentally induced tongue squamous cell carcinoma47. In cervical cancer, rapid tumor growth induces eosinophils recruitment and aggregation, particularly under hypoxic conditions. Reduced eosinophil levels, characterized by decreased CD80 and CD86 expression alongside increased production of anti-inflammatory cytokines, contribute to immune evasion by tumor cells. Induced eosinophils significantly promote cervical cancer cell proliferation and inhibit apoptosis, thus contributing to disease progression48. Conversely, lower eosinophil levels may indicate a robust immune response against tumors, correlating with better prognosis40.
While AEC and EOS% provide valuable insights into the immune response, it is important to acknowledge the significance of other peripheral blood biomarkers, such as the NLR, LMR, and PLR, which are widely recognized for their roles in cancer immunity. These indices, derived from neutrophils, lymphocytes, and monocytes, have been extensively studied and are often considered more directly involved in immune regulation and tumor progression49,50,51. For example, NLR has been associated with systemic inflammation and poor prognosis in various cancers, while LMR and PLR have shown promise in predicting treatment response and survival outcomes43,44,45. Compared to these established biomarkers, the role of AEC and EOS% in cancer immunity is less well-defined and requires further investigation. However, the ease of testing and the potential for AEC and EOS% to reflect specific aspects of the immune response, particularly in the context of immunotherapy, highlight their unique value as complementary biomarkers. Future studies should aim to integrate AEC and EOS% with other immune indices to provide a more comprehensive understanding of their collective impact on cancer prognosis and treatment outcomes.
Furthermore, our study results suggest a negative correlation between the ICIs response rate and peripheral blood AEC or EOS%, although the statistical difference between the two groups was not significant, possibly due to the small sample size. The results of this study suggest that monitoring AEC can be used to guide treatment decisions and design personalized treatment plans for R/M HNSCC patients. Further research should include larger-scale clinical cohorts and deeper molecular mechanism studies to validate this finding and explore the specific role of eosinophils in R/M HNSCC development and potential therapeutic targets.
This study has several limitations, including a small sample size that restricts statistical power and generalizability, and a single-arm, retrospective, single-center design that lacks a control group, limiting the strength of our conclusions. Additionally, the limited availability of PD-L1 status data and the absence of toxicity assessments further reduce the comprehensiveness of our findings. The cutoff values for AEC and EOS%, as well as the multiparameter model, require validation in larger, diverse cohorts through prospective studies. While we evaluated overall survival, disease-free survival and quality of life were not assessed due to limited follow-up data. Future studies should address these limitations to provide a more holistic understanding of immunotherapy outcomes.
Conclusion
In this study, we found that low peripheral blood AEC and EOS% was significantly associated with increased odds of response to ICIs in patients with R/M HNSCC, suggesting a potential role for peripheral blood AEC and EOS% in predicting response to immunotherapy and identifying favorable candidates for immunotherapy.
A-B) Levels of peripheral blood absolute eosinophil count and eosinophil percentage in patients with progressive disease (PD), stable disease (SD), and partial response (PR). C-D) Immunotherapy response type by peripheral blood absolute eosinophil count and eosinophil percentage in patients with recurrent or metastatic mucosal head and neck squamous cell carcinoma.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Sung, H. et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249. https://doi.org/10.3322/caac.21660 (2021).
Cohen, E. E. W. et al. The society for immunotherapy of Cancer consensus statement on immunotherapy for the treatment of squamous cell carcinoma of the head and neck (HNSCC). J. Immunother Cancer. 7, 184. https://doi.org/10.1186/s40425-019-0662-5 (2019).
Caudell, J. J. et al. NCCN Guidelines® insights: head and neck cancers, version 1.2022. J. Natl. Compr. Canc Netw. 20, 224–234. https://doi.org/10.6004/jnccn.2022.0016 (2022).
Johnson, D. E. et al. Head and neck squamous cell carcinoma. Nat. Rev. Dis. Primers. 6, 92. https://doi.org/10.1038/s41572-020-00224-3 (2020).
Wise-Draper, T. M., Bahig, H., Tonneau, M., Karivedu, V. & Burtness, B. Current therapy for metastatic head and neck cancer: evidence, opportunities, and challenges. Am. Soc. Clin. Oncol. Educ. Book. 42, 1–14. https://doi.org/10.1200/edbk_350442 (2022).
Ferris, R. L. & Licitra, L. PD-1 immunotherapy for recurrent or metastatic HNSCC. Lancet 394, 1882–1884. https://doi.org/10.1016/s0140-6736(19)32539-5 (2019).
Ferris, R. L. et al. Nivolumab for recurrent Squamous-Cell carcinoma of the head and neck. N Engl. J. Med. 375, 1856–1867. https://doi.org/10.1056/NEJMoa1602252 (2016).
Cohen, E. E. W. et al. Pembrolizumab versus methotrexate, docetaxel, or cetuximab for recurrent or metastatic head-and-neck squamous cell carcinoma (KEYNOTE-040): a randomised, open-label, phase 3 study. Lancet 393, 156–167. https://doi.org/10.1016/s0140-6736(18)31999-8 (2019).
Burtness, B. et al. Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): a randomised, open-label, phase 3 study. Lancet 394, 1915–1928. https://doi.org/10.1016/s0140-6736(19)32591-7 (2019).
Pembro Ups Survival in PD-L1-positive HNSCC. Cancer Discov. 9, Of8, (2019). https://doi.org/10.1158/2159-8290.Cd-nb2018-151
Wu, D. et al. The global landscape of neoadjuvant and adjuvant anti-PD-1/PD-L1 clinical trials. J. Hematol. Oncol. 15, 16. https://doi.org/10.1186/s13045-022-01227-1 (2022).
Varricchi, G. et al. Eosinophils: the unsung heroes in cancer? Oncoimmunology 7, e1393134. https://doi.org/10.1080/2162402x.2017.1393134 (2018).
Wechsler, M. et al. (ed, E.) Eosinophils in health and disease: A State-of-the-Art review. Mayo Clin. Proc. 96 2694–2707 https://doi.org/10.1016/j.mayocp.2021.04.025 (2021).
Carretero, R. et al. Eosinophils orchestrate cancer rejection by normalizing tumor vessels and enhancing infiltration of CD8(+) T cells. Nat. Immunol. 16, 609–617. https://doi.org/10.1038/ni.3159 (2015).
Lucarini, V. et al. IL-33 restricts tumor growth and inhibits pulmonary metastasis in melanoma-bearing mice through eosinophils. Oncoimmunology 6, e1317420. https://doi.org/10.1080/2162402x.2017.1317420 (2017).
Harbaum, L. et al. Peritumoral eosinophils predict recurrence in colorectal cancer. Mod. Pathol. 28, 403–413. https://doi.org/10.1038/modpathol.2014.104 (2015).
Reichman, H. et al. Activated eosinophils exert antitumorigenic activities in colorectal Cancer. Cancer Immunol. Res. 7, 388–400. https://doi.org/10.1158/2326-6066.Cir-18-0494 (2019).
Kataoka, S., Konishi, Y., Nishio, Y., Fujikawa-Adachi, K. & Tominaga, A. Antitumor activity of eosinophils activated by IL-5 and eotaxin against hepatocellular carcinoma. DNA Cell. Biol. 23, 549–560. https://doi.org/10.1089/dna.2004.23.549 (2004).
Furbert-Harris, P. et al. Inhibition of prostate cancer cell growth by activated eosinophils. Prostate 57, 165–175. https://doi.org/10.1002/pros.10286 (2003).
Chu, X. et al. Association of baseline peripheral-blood eosinophil count with immune checkpoint inhibitor-related pneumonitis and clinical outcomes in patients with non-small cell lung cancer receiving immune checkpoint inhibitors. Lung Cancer. 150, 76–82. https://doi.org/10.1016/j.lungcan.2020.08.015 (2020).
Tanizaki, J. et al. Peripheral blood biomarkers associated with clinical outcome in Non-Small cell lung Cancer patients treated with nivolumab. J. Thorac. Oncol. 13, 97–105. https://doi.org/10.1016/j.jtho.2017.10.030 (2018).
Hu, M. et al. Easily applicable predictive score for MPR based on parameters before neoadjuvant chemoimmunotherapy in operable NSCLC: a single-center, ambispective, observational study. Int. J. Surg. 110, 2275–2287. https://doi.org/10.1097/js9.0000000000001050 (2024).
Gebhardt, C. et al. Myeloid cells and related chronic inflammatory factors as novel predictive markers in melanoma treatment with ipilimumab. Clin. Cancer Res. 21, 5453–5459. https://doi.org/10.1158/1078-0432.Ccr-15-0676 (2015).
Pozorski, V. et al. Neutrophil-to-eosinophil ratio as a biomarker for clinical outcomes in advanced stage melanoma patients treated with anti-PD-1 therapy. Pigment Cell. Melanoma Res. 36, 501–511. https://doi.org/10.1111/pcmr.13109 (2023).
Rosner, S. et al. Peripheral blood clinical laboratory variables associated with outcomes following combination nivolumab and ipilimumab immunotherapy in melanoma. Cancer Med. 7, 690–697. https://doi.org/10.1002/cam4.1356 (2018).
Martens, A. et al. Baseline peripheral blood biomarkers associated with clinical outcome of advanced melanoma patients treated with ipilimumab. Clin. Cancer Res. 22, 2908–2918. https://doi.org/10.1158/1078-0432.Ccr-15-2412 (2016).
Herrmann, T. et al. Eosinophil counts as a relevant prognostic marker for response to nivolumab in the management of renal cell carcinoma: a retrospective study. Cancer Med. 10, 6705–6713. https://doi.org/10.1002/cam4.4208 (2021).
Utsunomiya, A. et al. Clinical significance of a blood eosinophilia in adult T-cell leukemia/lymphoma: a blood eosinophilia is a significant unfavorable prognostic factor. Leuk. Res. 31, 915–920. https://doi.org/10.1016/j.leukres.2006.10.017 (2007).
Kang, D. et al. A systematic review and meta-analysis of prognostic indicators in patients with head and neck malignancy treated with immune checkpoint inhibitors. J. Cancer Res. Clin. Oncol. 149, 18215–18240. https://doi.org/10.1007/s00432-023-05504-5 (2023).
Wang, Q., Yin, X., Wang, S. & Lu, H. Inflammatory markers as prognostic markers in patients with head and neck squamous cell carcinoma treated with immune checkpoint inhibitors: a systematic review and meta-analysis. Front. Oncol. 14, 1429559. https://doi.org/10.3389/fonc.2024.1429559 (2024).
Zhao, X. et al. Final analysis of a phase II trial of neoadjuvant chemoimmunotherapy for locoregionally advanced head and neck squamous cell carcinoma. Oral Oncol. 156, 106918. https://doi.org/10.1016/j.oraloncology.2024.106918 (2024).
Wu, D. et al. Neoadjuvant chemo-immunotherapy with camrelizumab plus nab-paclitaxel and cisplatin in resectable locally advanced squamous cell carcinoma of the head and neck: a pilot phase II trial. Nat. Commun. 15, 2177. https://doi.org/10.1038/s41467-024-46444-z (2024).
Liang, H. et al. Safety and efficacy of neoadjuvant therapy with Tislelizumab plus chemotherapy for locally advanced head and neck squamous cell carcinoma: a single-arm, retrospective study. Cancer Immunol. Immunother. 74, 108. https://doi.org/10.1007/s00262-025-03953-0 (2025).
Ou, X. et al. Induction Toripalimab and chemotherapy for organ preservation in locally advanced laryngeal and hypopharyngeal cancer: A Single-Arm phase II clinical trial. Clin. Cancer Res. 30, 344–355. https://doi.org/10.1158/1078-0432.Ccr-23-2398 (2024).
Li, X. et al. Induction chemotherapy combined with immunotherapy in locally advanced head and neck squamous cell carcinoma. BMC Cancer. 21, 622. https://doi.org/10.1186/s12885-021-08373-8 (2021).
Chung, C. H. et al. Phase II Multi-institutional clinical trial result of concurrent cetuximab and nivolumab in recurrent and/or metastatic head and neck squamous cell carcinoma. Clin. Cancer Res. 28, 2329–2338. https://doi.org/10.1158/1078-0432.Ccr-21-3849 (2022).
Pai, S. I. et al. SUPREME-HN: a retrospective biomarker study assessing the prognostic value of PD-L1 expression in patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck. J. Transl Med. 17, 429. https://doi.org/10.1186/s12967-019-02182-1 (2019).
Reichman, H., Karo-Atar, D. & Munitz, A. Emerging roles for eosinophils in the tumor microenvironment. Trends Cancer. 2, 664–675. https://doi.org/10.1016/j.trecan.2016.10.002 (2016).
Grisaru-Tal, S., Rothenberg, M. E. & Munitz, A. Eosinophil-lymphocyte interactions in the tumor microenvironment and cancer immunotherapy. Nat. Immunol. 23, 1309–1316. https://doi.org/10.1038/s41590-022-01291-2 (2022).
Simon, H. U. et al. Interleukin-2 primes eosinophil degranulation in hypereosinophilia and wells’ syndrome. Eur. J. Immunol. 33, 834–839. https://doi.org/10.1002/eji.200323727 (2003).
Sosman, J. A. et al. Evidence for eosinophil activation in cancer patients receiving Recombinant interleukin-4: effects of interleukin-4 alone and following interleukin-2 administration. Clin. Cancer Res. 1, 805–812 (1995).
Ellem, K. A. et al. A case report: immune responses and clinical course of the first human use of granulocyte/macrophage-colony-stimulating-factor-transduced autologous melanoma cells for immunotherapy. Cancer Immunol. Immunother. 44, 10–20. https://doi.org/10.1007/s002620050349 (1997).
Puxeddu, I. et al. Human peripheral blood eosinophils induce angiogenesis. Int. J. Biochem. Cell. Biol. 37, 628–636. https://doi.org/10.1016/j.biocel.2004.09.001 (2005).
Munitz, A., Levi-Schaffer, F. & Eosinophils New’ roles for ‘old’ cells. Allergy 59, 268–275. https://doi.org/10.1111/j.1398-9995.2003.00442.x (2004).
Salcedo, R. et al. Eotaxin (CCL11) induces in vivo angiogenic responses by human CCR3 + endothelial cells. J. Immunol. 166, 7571–7578. https://doi.org/10.4049/jimmunol.166.12.7571 (2001).
Cormier, S. A. et al. Pivotal advance: eosinophil infiltration of solid tumors is an early and persistent inflammatory host response. J. Leukoc. Biol. 79, 1131–1139. https://doi.org/10.1189/jlb.0106027 (2006).
da Silva, J. M. et al. Eosinophil depletion protects mice from tongue squamous cell carcinoma induced by 4-nitroquinoline-1-oxide. Histol. Histopathol. 29, 387–396. https://doi.org/10.14670/hh-29.387 (2014).
Xie, F. et al. The infiltration and functional regulation of eosinophils induced by TSLP promote the proliferation of cervical cancer cell. Cancer Lett. 364, 106–117. https://doi.org/10.1016/j.canlet.2015.04.029 (2015).
Horiuchi, K., Mishima, K., Ohsawa, M., Sugimura, M. & Aozasa, K. Prognostic factors for well-differentiated squamous cell carcinoma in the oral cavity with emphasis on immunohistochemical evaluation. J. Surg. Oncol. 53, 92–96. https://doi.org/10.1002/jso.2930530209 (1993).
von Wasielewski, R. et al. Tissue eosinophilia correlates strongly with poor prognosis in nodular sclerosing Hodgkin’s disease, allowing for known prognostic factors. Blood 95, 1207–1213 (2000).
Enblad, G., Sundstrom, C. & Glimelius, B. Infiltration of eosinophils in Hodgkin’s disease involved lymph nodes predicts prognosis. Hematol. Oncol. 11, 187–193. https://doi.org/10.1002/hon.2900110404 (1993).
Acknowledgements
The authors gratefully acknowledge the voluntary participation of all study subjects.
Funding
This research was funded by the National Natural Science Foundation of China (No.82173341, No.82303133); China Postdoctoral Science Foundation (No. 2022M723559); Natural Science Foundation of Hunan Province (No.2023 JJ20087, No.2022JJ30963, No.2021JJ40951); the Science and Technology Innovation Program of Hunan Province (No.2023RC3082); Project of Hunan Health Commission (No. B202307017799, No.B202309018525); Changsha Distinguished Young Scholars grant (No.kq2209007).
Author information
Authors and Affiliations
Contributions
Qin YX, Yao SH, Huang HM, Wang JC, and Zhu GC conceived and designed the study. Qin YX, Yao SH, Wang XW, Luo AJ, and Zhu GC contributed to the study design. Qin YX, Yao SH, Huang HM, Chen CH, and Zhu GC acquired the data. Qin YX, Yao SH, Huang HM, S L, and Zhu GC ensured the quality control of data and algorithms. Qin YX, Yao SH, Huang HM, Wang JC, and Zhu GC performed data analysis and interpretation. Qin YX, Yao SH, Huang HM, S L, and Zhu GC conducted the statistical analysis. Qin YX, Yao SH, Huang HM, Xiao YY and Chen CH prepared the manuscript; all authors reviewed and edited the manuscript, read, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the Institutional Review Board at the Second Xiangya Hospital (Ethics Approval No. 228, 2022).
Approval for human experiments
The study was designed as a retrospective study using only de-identified clinical data, which is in accordance with the exemption criteria of the U.S. Code of Federal Regulations, Title 45, Part 46 (specifically, 45 CFR § 46.104(d)(4): Secondary research uses of identifiable private information if the information is recorded without identifiers.). Due to the retrospective nature of the study, IRB of Second Xiangya Hospital waived the need of obtaining informed consent. Personal data were anonymized to ensure confidentiality throughout data analysis and reporting.
Consent to participate
All authors certify that neither this manuscript nor any substantially similar content under their authorship has been published or is being considered for publication elsewhere, in any language.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qin, Y., Yao, S., Huang, H. et al. Peripheral eosinophils and immunotherapy response in patients with recurrent or metastatic HNSCC. Sci Rep 15, 17351 (2025). https://doi.org/10.1038/s41598-025-01457-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-01457-6