Abstract
This study aimed to identify predictors of intrasinusidal alveolar antral artery (AAA) localization at the upper left first molar (UL6) region and develop a clinical risk prediction model. A retrospective analysis of 243 eligible cases with cone-beam computed tomography (CBCT) imaging was conducted, categorizing AAA into intrasinusidal and non-intrasinusidal groups. Multivariable logistic regression revealed three independent predictors: anatomical variations (OR = 0.270, 95% CI 0.102–0.716), lateral Maxillary sinus wall width (OR = 0.583, 95% CI 0.371–0.915), and sinus cavity width (OR = 1.176, 95% CI 1.063–1.302). The nomogram-based prediction model demonstrated moderate discriminative capacity (C-index = 0.758) with satisfactory calibration alignment between predicted and observed outcomes. Receiver operating characteristic analysis yielded an area under the curve of 0.758. The sensitivity and specificity of the model were 0.789 and 0.579, respectively, with an accuracy of 69.0%.The findings demonstrate that when AAA is not visualized on CBCT scans, application of this model to assess the risk of intrasinusidal AAA occurrence in the surgical area enables preoperative planning of the surgical approach, thereby enhancing procedural safety.
Similar content being viewed by others
Introduction
Anatomical studies of the alveolar maxillary sinus artery (AAA) began at the beginning of the 20th century. The anatomical characteristics of this artery were first systematically described by Strong1 in 1934, laying the foundation for subsequent studies, and in 1999, Solar et al.2 confirmed the constant presence of the AAA by anatomical studies of 18 cadaveric specimens, and their findings were supported by numerous subsequent studies3,4. The AAA is an anastomotic branch of the posterior superior alveolar artery and the infraorbital artery, and its course is mainly distributed in the anterolateral wall of the maxillary sinus, which provides the main blood supply for the periosteum of the sinus wall and the mucosal tissues5.
In clinical operations, the anatomical features of AAA directly affect the safety of many maxillary sinus-related surgeries, especially in the field of oral implantation, which is the most typical of maxillary sinus augmentation using lateral approach. Since Tatum proposed the procedure in 1976, hemorrhage due to intraoperative injury to the AAA remains one of the major complications, despite the fact that the technical system has evolved for more than 40 years6. Research data show7 that arterial rupture bleeding may occur during surgical window opening in approximately 10–57% of cases, depending on the difference in diameter of the AAA. This hemorrhage risk highlights the importance of accurate preoperative assessment of AAA.
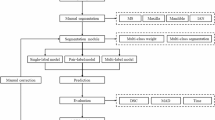
Based on comparative studies of available imaging devices8,9, cone-beam computed tomography (CBCT) has become the optimal choice for observing the anatomical structures associated with the maxillary sinus. Based on the anatomical relationship between the AAA and the bone wall, three types of characteristic bone foramina can be demonstrated in CBCT images: the intrasinusidal type, the intraosseous type, and the lateral sinus wall type10 (Fig. 1). Among them, the intraosseous type can be visualized directly by CBCT, and the lateral sinus wall type can be confirmed by direct visualization after intraoperative flap flipping, and the risk of injury in these two types is relatively controllable. However, there is a lack of effective preoperative prediction methods for the intrasinusidal type of AAA that is not visualized by CBCT.
Therefore, in this study, a risk prediction model for intrasinusidal AAA was constructed using multifactorial logistic regression analysis based on a large sample of CBCT imaging data. By analyzing the correlation between patients’ AAA anatomical parameters and AAA types, it is possible to effectively assess the preoperative risk of intrasinusidal AAA not visible by CBCT and formulate an individualized surgical plan, thus effectively reducing the incidence of intraoperative hemorrhage.
Materials and methods
Sample and study design
A total of 243 cases of CBCT from outpatients of the stomatology department of the Second People’s Hospital of Wuhu City and the Wuhu Traditional Chinese Medicine Hospital from December 2023 to February 18, 2024 were selected as the study subjects. This experimental study was categorized into intrasinusidal and non-intrasinusidal groups according to the type of UL6 point AAA.
Inclusion Criteria: (1) AAA observable in UL6 point slices and the diameter of the AAA was measurable. (2) Age between 18 and 80 years. (3) No other major diseases such as fracture, tumor, or other major diseases of the maxillary sinus. (4) Perfect information of the case. Exclusion criteria: (1) poor image quality (blurred imaging, AAA is too small to measure). (2) Age not in the interval. (3) History of serious disease in the maxillary sinus. (4) Incomplete information about the case.
According to the EPV (Events Per Variable) principle of logistic regression sample size estimation11, the EPV should be in the range of 10–20 for robust results. The detection rate of AAA at point UL6 in our research group collection was 42.4% (300 cases of observable AAA detected in 707 CBCT cases), assuming an EPV = 10, a total of 10 study factors (Distance from upper margin of AAA to floor of maxillary sinus excepted as not representative) were included, so the number of CBCTs required was 10 × 10 = 100, and the total sample size required (AAA observable at point UL6 in CBCT) was 100 ÷ 42.4% ≈ 236 cases. The final selection for inclusion in this trial was 243 cases.
Ethics
The study was approved by the Medical Ethics Committee of the Second People’s Hospital of Wuhu City before it was conducted (Approval date 2024.9.19; Approval No. 2024-KY-135). All participants provided written informed consent before participating in the research and retained the right to withdraw from the study at any stage without consequence. All methods were performed following the Declaration of Helsinki.
Data collection methods
The samples in this study were collected using cone-beam CT (SS-X9010DMax-3DE. Meiya Optoelectronics, No. 668 Wangxiang Road, Hi-tech Development Zone, Shushan District, Hefei City, Anhui Province, China), I-CAT software was selected as (MYDCS V3.0), the scanning range was set to 140 mm×100 mm, and the voxel was 0.25 mm; scanning conditions were 60–90 kv, 2–10 ma, exposure time 20 s. The examinee stood in the standing position, looked straight ahead, made the Frankfort plane parallel to the ground, took the intercuspal position, and the mandibular bracket fixed the head position. Cone-beam CT single 360° unspliced scanning was used to acquire data. The third of the five slices of UL6 pointing (five slices covering all the proximal-medial and distal-medial root images of UL6) was selected as the slice for the measurement data. The data collection for this experiment was done by three different practitioners who took the average of the measurements as the final sample data.
The data collected for the study included (1) the type of AAA, (2) the width of the lateral wall of the maxillary sinus, (3) the width of the maxillary sinus cavity at the location of the AAA, (4) the height of the alveolar ridge, (5) the width of the alveolar ridge, (6) the diameter of the AAA, (7) the vertical distance from the upper edge of the AAA to the floor of the maxillary sinus, (8) the distance from the upper edge of the AAA to the floor of the maxillary sinus, (9) the distance between the AAA and the apex of the alveolar ridge, (10) anatomical variations in the AAA. (For the above measurement protocols, refer to Pablo Varela-Centelles et al.12 and de Albuquerque et al.4, see Fig. 2 for details and Fig. 3 for anatomical variations). The basic data of the patients in the cases were also collected including age and sex.
(A) AAA diameter: the maximum caliber of the bone foramen imaged (mm); (B) Width of the lateral wall of the maxillary sinus: make a horizontal line across the center of the AAA, intersecting with the medial and lateral walls of the bone of the maxillary sinus, and the distance between the two intersections is the width (mm); (C) Distance from the upper edge of the AAA to the floor of the maxillary sinus; (D) Width of the maxillary sinus cavity in the position of the AAA: horizontal distance from the medial wall of the bone relative to the upper edge of the AAA position to the contralateral bone wall (millimeters); (E) vertical distance from the upper edge of the AAA to the floor of the maxillary sinus; (F) width of the alveolar ridge; (G) height of the alveolar ridge; (H) distance from the AAA to the top of the alveolar ridge.
Statistical methods
SPSS 26.0 and R software were applied to statistically analyze the data. Kolmogorov–Smirnov method was used to test the normality of the measurement data, and the independent samples t-test was applied for the data that conformed to normal distribution expressed as mean ± standard deviation, while the Mann–Whitney U test was applied for the data that were not normally distributed expressed as M (P25, P75). In this study, count data were expressed as percentages and the χ2 test was applied. Binary logistic regression was used to analyze the factors affecting the AAA being intrasinusidal in UL6 point CBCT, which was used to establish a risk prediction model, and the model was presented visually. Repeated sampling by Bootstrap method was used for adequate internal validation of the model, and calibration and discrimination of the model were measured using calibration curves and ROC curves, and the consistency index (C-index) was calculated. P < 0.05 was considered as statistically significant difference.
Results
Comparison of patients’ general information
In 243 cases of UL6 point AAA observable by CBCT, the number of AAA type as intrasinusidal was 128.Comparison between the groups revealed differences in anatomical variation, maxillary sinus lateral wall width, and sinus cavity width, age, height of the alveolar ridge, diameter of the AAA, width of the alveolar ridge, and distance from the upper edge of the AAA to the top of the alveolar ridge, all of which were statistically significant (P < 0.05), whereas the differences between the two groups for sex, vertical distance from the upper edge of the AAA to the bottom of the sinus, and distance from the upper edge of the AAA to the bottom of the sinus were not statistically significant (P > 0.05) .Between the two groups, as shown in Table 1. (See annex for details).
Multifactorial analysis of AAA as intrasinusidal at point UL6
The type of AAA at point UL6 observed in CBCT as intrasinusidal was used as the dependent variable (yes = 1, no = 0), and the statistically different indicators in the one-way analysis were included in the binary logistic regression, and the results of the study showed that anatomical variation, width of the lateral wall of the maxillary sinus, and width of the sinus cavity were the influencing factors for the type of AAA at point UL6 as intrasinusidal (P < 0.05). See Tables 2 and 3 for details.
Construction of the following line drawing model at UL6 point AAA for the intrasinusidal type
A column-line graph prediction model was constructed based on the factors influencing the AAA to be intrasinusidal at point UL6 (anatomical variation, maxillary sinus lateral wall width, sinus cavity width) by using the R software and the rms program package, as detailed in Fig. 4. The probability of the occurrence of the AAA to be intrasinusidal at point UL6 was obtained based on the scoring of the results of the factors selected in the model, and each score was summed up as a total score, and the higher the total score, the greater the probability of the AAA to be intrasinusidal at point UL6 was. The higher the total score, the higher the probability that the AAA foramen at point UL6 is intrasinusidal. For example, in one patient with a maxillary sinus lateral wall width of 1 mm, no anatomical variations, and a sinus cavity width of 24 mm, the patient’s corresponding scores in the column line diagram were 52.50, 24.50, and 92.50, for a total score of 169.50, corresponding to a 95% probability of occurrence of a intrasinusidal type.
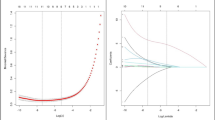
Bootstrap self-sampling method was used to validate the raw data by taking 1000 repetitive samples, which resulted in a model consistency index (C-index) of 0.758, a calibration curve in the neighborhood of the ideal curve, an AUC of 0.758, and a sensitivity and specificity of 0.789 and 0.579, respectively, with an accuracy of 69.0%, which is shown in Figs. 5 and 6.
Discussion
Reasons for choosing the point at UL6
The selection of UL6 as the reference point for the study was based on several considerations.
Firstly, as the first permanent tooth erupting from the maxillary dentition, the maxillary first molar has been used for a relatively long time in the mouth, and because it is the tooth that bears the main occlusal function, it is used more frequently and subjected to more force. At the same time, the anatomical structure of the maxillary first molar is more special, there are more grooves, and the position is backward, which is easy to appear in the dead space of oral cleaning. The above reasons lead to a much higher probability of caries and periodontal disease13. It also increases the likelihood of premature loss of the maxillary first molar as an indication for implant restoration. It has also been shown, that patients with periodontal disease have more severe bone loss of the maxillary first molar in symmetrical dentition14. This also represents a possible bone deficit in the implant area, which can be solved precisely by external elevation of the maxillary sinus to address the challenge of bone augmentation.
Secondly, from the anatomical point of view, the point of the maxillary first molar, AAA distance from the alveolar ridge is small, and it is easy to be in the range of the surgical area of the maxillary sinus augmentation using lateral approach12, therefore, it is of clinical significance to select the maxillary first molar as the study area.
Some scholars compared the detection rate of AAA in the maxillary sinus on the right and left sides, and the result was not statistically significant4. Therefore, a unilateral design was selected for this study to improve homogeneity. Upon comparison, it was found that the physician who collected the data used significantly less time to measure the data on the left side than on the right side, and in order to improve the efficiency of the measurements, the left side of the study protocol was finally adopted.
Discussion of the AAA study
With the development of imaging technology in recent years, the anatomical study of AAA has entered the stage of precise imaging. Various types of imaging equipment are used to observe AAA to understand its alignment structure, location and diameter, etc., as an important index for preoperative reference. CBCT was used as an auxiliary tool for this experimental study because of its advantages of high imaging resolution, multi-space angle imaging, obvious contrast of different tissue structures, and high precision15.
According to the statistics, the actual detection rate of AAA in this experiment was 42.4%, which was different from the 76.3% detected by foreign scholars16, and this was considered to be caused by the differences in ethnicity and the precision of the imaging equipment used. The small diameter of AAA or the complete concealment of AAA (superficial and intrasinusidal type) prevented the accurate presentation of AAA17, and these combined factors resulted in a much lower detection rate than that of foreign studies.
Of the 243 cases with UL6 point AAA in the inclusion criteria, 128 (52.6%) were intrasinusidal, 107 (44%) were intraosseous, and 8 (3.2%) were superficial. This result is very close to the findings of Eda Didem Yalcin et al.18, indicating that more than half of the AAA were observed to be located in the subperiosteum, and the intrasinusidal type contained cases with occult imaging features (not visible in CBCT), but exactly what percentage is still unknown with the currently available studies. This situation greatly increases the difficulty of clinical surgical path planning and confirms the clinical urgency of establishing a prediction model for occult AAA.
Analysis of factors influencing AAA as intrasinusidal
Logistic regression analysis revealed that anatomical variation (OR = 0.270, 95% CI 0.102–0.716), sinus lateral wall width (OR = 0.583, 95% CI 0.371–0.915) and sinus cavity width (OR = 1.176, 95% CI 1.063–1.302) were independent predictors of intrasinusidal type AAA formation factors (P < 0.05). The following is the analysis of each influence factor.
Anatomical variations: anatomical variations can be understood as the phenomenon of finding more than one bone hole in a section, i.e., the presence of small branches in the AAA. Fayek et al.19 found branching in 8.7% of cases in his study. Another research group, Ang et al.20, found a higher percentage of branching in anatomical variations in his study and refined the observation of branching, emphasizing the importance of performing preoperative observation of branching. According to the results of the present study, anatomical variant double branching was found in 13.1% of cases, and a rare case of triple branching was also observed (see Fig. 7). For homogeneity reasons, only one branch near the sinus floor was included in the study for the anatomical variant cases, and data were collected for this branch. Statistically, 21.2% (7/32) of this branch were found to be intrasinusidal. In addition, a large number of samples were found to have a double branch traveling from point Upper left second premolar(UL5) to Upper left first molar(UL6) and then becoming a single branch during data collection. It has been noted21 that the thickness of the lateral wall of the maxillary sinus decreases gradually from the cusp toward the second molar and that the diameter of the AAA is positively correlated with it. In other words, the more posterior the site, the smaller the diameter of the AAA, which also explains the phenomenon of branch disappearance. Since there are relatively few studies on AAA branching, the mechanism of branch formation has not been elucidated in the existing literature.
Sinus lateral wall width: Analysis of the data showed that the thickness of the lateral wall of the sinus (OR = 0.603, 95% CI 0.384–0.945) showed a negative correlation with the risk of developing intrasinusidal AAA. The reason for this is speculated to be understood as a thicker lateral sinus wall provides a stronger bony structure that completely encases AAA and reduces the likelihood of its migration into the intrasinusidal space. When the thickness of the bony wall is thinner than the AAA diameter, the integrity of the bony envelope is disrupted and the vessel is susceptible to migration toward the intrasinusidal space. The accuracy of this conjecture needs to be further verified due to the lack of support from relevant literature.
Sinus cavity width: After analyzing the results, it was found that the sinus cavity width was positively correlated with the risk of intrasinusidal AAA. The study by Xiaofei Zheng et al.22 found that in maxillary sinus lifting the sinus cavity width was positively correlated with the bone resorption of the grafts and that narrower maxillary sinuses had better blood supply to wider maxillary sinuses. Gustavo Avila et al.23 also concluded that the sinus cavity width was negatively correlated with the percentage of new bone formation after his study. Combining the two conclusions it can be concluded that the narrower the sinus cavity the more adequate the blood supply to the operative area. In other words, the smaller the ratio of bone wall width to vessel diameter, the poorer the ability of the bone wall to encapsulate blood vessels, coupled with the pneumatization of the maxillary sinus, the bone changes on the side close to the Schneiderian membrane, resulting in the migration of AAA to the subperiosteum. This study is the first to correlate sinus cavity width with intrasinusidal type and analyze its potential mechanism as an independent risk factor, but it is only a conjecture still needs to be verified by further studies.
Prospects of the UL6 point AAA intrasinusidal risk prediction model in clinical practice
The successful implementation of maxillary sinus augmentation using lateral approach, a standard procedure for bone augmentation, is highly dependent on the precise localization of the AAA. Preoperative AAA evaluation using CBCT has become established clinical practice24,25. If the AAA cannot be effectively assessed preoperatively, it may damage the AAA leading to severe intraoperative hemorrhage, making it impossible to continue the surgery, and even in the case of less bleeding, it may affect the surgical field and prolong the operation time. Also intraoperative hemorrhage is detrimental to the stability of the graft filler26. It has been shown that significant postoperative pain may also occur after injury to the AAA27. For these reasons, assessment of AAA in the operative area becomes a prerequisite for successful surgery. Although CBCT demonstrates high localization accuracy, completely occult subperiosteal AAA lacking bony canal markings presents as “imaging blind zones” and cannot be assessed, still posing a hemorrhage risk.
Pre-collection of data required for modeling in practical clinical applications. According to the modeling requirements, the location of the surgical opening needs to be determined preoperatively by the width of the lateral wall at that location, the width of the sinus cavity, and by determining whether anatomical variation exists in that side of the AAA. Substituting the above data into a columnar line drawing, the probability of a intrasinusidal type of AAA at that opening location can be obtained in the absence of an image of the bone hole. After applying the model to determine the type of occult artery at the operative site, a preliminary hemorrhage risk assessment of occult AAA can be obtained, thus guiding the operator in preoperative path planning and reducing the risk of intraoperative hemorrhage.
In the future, this model can be combined with the field of artificial intelligence to develop an automated CBCT analysis system to improve the efficiency of AAA localization and better serve clinical work.
Feasibility and scientific validity of the UL6 point AAA bone hole as a intrasinusidal predictive model with.
The visualization of logistic regression results is often in the form of a column-line graph, which enables accurate prediction of AAA intrasinusidal type. In this study, based on the CBCT study of the included experiments, we explored the independent risk factors of AAA for intrasinusidal type at point UL6 and constructed a column-line graph model, with a sensitivity and specificity of 0.789 and 0.579, respectively, and an area under the ROC curve of 0.758, with the calibration curve near the ideal curve, which indicates that the model has a high degree of calibration and is of high value for clinical application.
Conclusions
In this study, we showed that anatomical variations, sinus lateral wall width and sinus cavity width are the influencing factors for AAA at UL6 points to be of intrasinusidal type, and we used this to establish a risk prediction models with good performance, which is instructive for predicting the presence or absence of AAA located entirely intrasinusidally at a specific location in the clinic. Of course, there are some limitations in this study, such as the lack of multicenter participation in the sample is relatively homogeneous; there may be image omission due to the precision limitations of CBCT, etc.
In summary, the establishment of this model provides a scientific basis for clinicians in preoperative planning, especially in the case of AAA bony foramen that is not visible in CBCT images, which can help doctors to anticipate the risk in advance, optimize the surgical plan, and reduce the likelihood of accidental intraoperative injury to AAA.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Alves, N., Ceballos, F. & Deana, N. F. Anastomosis between the posterior superior alveolar artery and the infra-orbital artery: A review of current terminology. Int. J. Morphol. 40 (1), 18–23. https://doi.org/10.4067/s0717-95022022000100018 (2022).
Solar, P. et al. Blood supply to the maxillary sinus relevant to sinus floor elevation procedures. Clin. Oral Implants Res. 10 (1), 34–44. https://doi.org/10.1034/j.1600-0501.1999.100105.x (1999).
de Sousa, C. P. et al. Evaluation of the presence and positioning of the posterior upper alveolar artery in the lateral wall of the maxillary sinus by cone-beam computed tomography. Acta Sci. Dent. Sci. 7 (3), 26–30. https://doi.org/10.31080/asds.2023.07.1583 (2023).
de Albuquerque, L. R. C. et al. Alveolar antral artery in edentulous patients and their visualization through cone beam computed tomography. Morphologie 105 (348), 64–68. https://doi.org/10.1016/j.morpho.2020.08.003 (2021).
Zhou, Q., Feng, Q. & Zhu, D. The radiological evaluation of the anatomy of the alveolar antral artery and the lateral wall thickness using cone-beam computed tomography: A retrospective study. Curr. Med. Imaging Rev. 20 (0), 0–0. https://doi.org/10.2174/1573405619666230306093633 (2023).
Iancu, I. et al. A systematic review of sinus floor augmentation complications. Does graft type influence the complications rate? Revista Română De Stomatologie. 69 (2), 69–79. https://doi.org/10.37897/rjs.2023.2.2 (2023).
Valentini, P. Prevention and management of intra-operative complications in maxillary sinus augmentation using the lateral approach? A review 16–26. https://doi.org/10.58240/1829006x-2023.19.2-16 (2023).
Karslioğlu, H. et al. The radiological evaluation of posterior superior alveolar artery by using CBCT. Curr. Med. Imaging Rev. 17 (3), 384–389. https://doi.org/10.2174/1573405616666200628134308 (2021).
Bernardi, S. et al. Anatomy of maxillary sinus: Focus on vascularization and underwood septa via 3D imaging. Tomography 10 (4), 444–458. https://doi.org/10.3390/tomography10040034 (2024).
Testori, T. et al. Maxillary sinus elevation difficulty score with lateral wall technique. Int. J. Oral Maxillofac. Implants 35 (3), 631–638. https://doi.org/10.11607/jomi.8034 (2020).
Gao, Y. & Zhang, J. Sample size was determined for the logistic-regression analysis. Evid.-Based Med. 18 (02), 122–124 (2018).
Varela-Centelles, P. et al. Study of factors influencing preoperative detection of alveolar antral artery by CBCT in sinus floor elevation. Sci. Rep. https://doi.org/10.1038/s41598-020-67644-9 (2020).
Umaiyal, P. Fixed prosthesis in missing maxillary first molar among medium aged adult: A retrospective study. Biosci. Biotechnol. Res. Commun. 14 (10), 01–06. https://doi.org/10.21786/bbrc/14.10.1 (2021).
Jiang, Y. et al. Clinical, radiographic characterizations and complications of maxillary molar in a periodontitis population: A retrospective study based on CBCT radiography. Clin. Oral Investig. 27 (5), 2335–2346. https://doi.org/10.1007/s00784-022-04845-8 (2023).
Devi, K. R. R. et al. Radiographic assessment of maxillary sinus lateral wall and anatomy of posterior superior alveolar artery: A cone-beam computed tomographic. Eur. J. Anat. 26 (4), 399–408. https://doi.org/10.52083/rlfi8348 (2022).
Tofangchiha, M. et al. Anatomical localization of posterior superior alveolar artery: A retrospective study by cone-beam computed tomography. Dent. Med. Probl. 59 (3), 407–412. https://doi.org/10.17219/dmp/145894 (2022).
Yang, D. H. & Lee, N. V. A simple method of managing the alveolar antral artery during sinus lift surgery. Int. J. Otolaryngol. Head Neck Surg. 10 (03), 131–146. https://doi.org/10.4236/ijohns.2021.103014 (2021).
Yalcin, E. D. & Akyol, S. Relationship between the posterior superior alveolar artery and maxillary sinus pathology: A cone-beam computed tomography study. J. Oral Maxillofac. Surg. 77 (12), 2494–2502. https://doi.org/10.1016/j.joms.2019.07.009 (2019).
Fayek, M. M., Amer, M. E. & Bakry, A. M. Evaluation of the posterior superior alveolar artery canal by cone-beam computed tomography in a sample of the Egyptian population. Imaging Sci. Dent. 51 (1), 35–40. https://doi.org/10.5624/isd.20200146 (2021).
Ang, K. Y., Ang, K. L. & Ngeow, W. C. The prevalence and location of the posterior superior alveolar artery in the maxillary sinus wall: A preliminary computed-cone beam study. Saudi Dent. J. 34 (7), 629–635. https://doi.org/10.1016/j.sdentj.2022.08.010 (2022).
Yeung, A. W. K. et al. The use of CBCT in evaluating the health and pathology of the maxillary sinus. Diagnostics 12 (11), 2819–2819. https://doi.org/10.3390/diagnostics12112819 (2022).
Zheng, X. et al. Influence of maxillary sinus width on transcrestal sinus augmentation outcomes: Radiographic evaluation based on cone beam CT. Clin. Implant Dent. Relat. Res. 18 (2), 292–300. https://doi.org/10.1111/cid.12298 (2015).
Avila, G. et al. The influence of the bucco-palatal distance on sinus augmentation outcomes. J. Periodontol. 81 (7), 1041–1050. https://doi.org/10.1902/jop.2010.090686 (2010).
Alves, N. et al. Analysis of the presence, location and morphometry of the alveolar antral artery by cone-beam computed tomography in Chilean adults. Int. J. Morphol. 38 (6), 1760–1766. https://doi.org/10.4067/s0717-95022020000601760 (2020).
Rinaldi, F. et al. Volumetric evaluation of maxillary sinuses using CBCTS: Radiographic study. Ital. J. Anat. Embryol. 127 (2), 47–50. https://doi.org/10.36253/ijae-14681 (2023).
Laovoravit, V., Kretapirom, K. & Pornprasertsuk-Damrongsri, S. Prevalence and morphometric analysis of the alveolar antral artery in a group of Thai population by cone beam computed tomography. Oral Radiol. 37 (3), 452–462. https://doi.org/10.1007/s11282-020-00478-3 (2020).
Kolte, R. A. et al. Association of location and diameter of alveolar antral artery to crest of alveolar bone in dentate and partially edentulous patients—A cone-beam computed tomography study. J. Indian Soc. Periodontol. 25 (1), 55–55. https://doi.org/10.4103/jisp.jisp_603_19 (2021).
Author information
Authors and Affiliations
Contributions
Zhipeng Wang(First Author): Conceptualization, Methodology, Investigation, Writing - Original Draft; Visualization.Xiaowen Hou: Data Curation, Software, Formal Analysis.Qi Liu: Project administration.YuQing ShangGuan: Validation .Hua Zhou(Corresponding Author): Conceptualization, Funding acquisition, Resources, Supervision, Writing - Review & Editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, Z., Hou, X., Liu, Q. et al. Construction of the risk prediction model of the alveolar antral artery as the intrasinusidal type at the point of UL6. Sci Rep 15, 17529 (2025). https://doi.org/10.1038/s41598-025-01475-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01475-4