Abstract
Sepsis is one of the risk factors for deep vein thrombosis (DVT). However, studies on risk factors for DVT in critically ill patients with sepsis are limited, and no specific assessment tool is available for evaluating the risk of DVT in this population. We aimed to determine the risk factors of DVT and develop a simple nomogram for this vulnerable population. In this retrospective observational study, patients with sepsis using Sepsis-3 criteria, who were admitted to the intensive care unit (ICU) of West China Hospital of Sichuan University from January 2015 to May 2022, were enrolled. Patients with a diagnosis of DVT before admitting to ICU, cancer, trauma, pregnancy, surgery more than 45 min, or long-term use of glucocorticoids were excluded. Patients were assigned to the DVT group or non-DVT group based on the results of ultrasonography. We generated receiver operating characteristic curves (ROC) to calculate the cut-off of the continuous variables. A forest plot and a nomogram were developed by multivariable logistic regression. A total of 1057 patients were finally included. The multivariable logistic regression analysis showed that age (≥ 48 years old, odds ratio (OR) = 2.99, 95% confidence interval (CI): 2.19–4.12, P < 0.001), the use of vasoactive drugs (≥ 336 h, OR = 5.66, 95%CI 4.05–7.99, P < 0.001), PaO2/FiO2 (≤ 275, OR = 1.68, 95%CI 1.24–2.27, P < 0.001), respiratory infection (OR = 1.44, 95%CI 1.02–2.06, P < 0.05), D-dimer level (≥ 3.6, OR = 1.59, 95%CI 1.12–2.26, P < 0.05), fibrinogen level (≤ 3.9, OR = 1.45, 95%CI 1.09–1.95, P < 0.05), physical prophylaxis (OR = 0.51, 95%CI 0.37–0.71, P < 0.001) were independently associated with DVT. There were no significant differences in the insertion of the central venous catheter (CVC) or peripherally inserted central catheter (PICC), Sequential Organ Failure Assessment (SOFA) score, duration of mechanical ventilation, stay in ICU, and length of hospitalization between the two groups, while the DVT group had a higher proportion of use of pharmacologic thromboprophylaxis (61.8% vs. 47.2%, P < 0.001). In critically ill patients with sepsis, physical prophylaxis was found as an independent protective factor for DVT. Advanced age, long-term use of vasoactive drugs, elevated D-dimer levels, decreased fibrinogen levels, low oxygenation index, and respiratory infection were independent risk factors for DVT.
Similar content being viewed by others
Introduction
Previous studies have established sepsis as a significant risk factor for the development of deep vein thrombosis (DVT)1,2,3. Evidence suggests DVT is associated with prolonged mechanical ventilation, extended intensive care unit (ICU) and hospital stays4,5,6, and exacerbation of sepsis-related pathophysiological disorders. A large cohort study further identified DVT as both a cause and consequence of sepsis, contributing to acute and chronic vascular complications7.
A multicenter prospective study by Kaplan et al. suggested that sepsis patients exhibit elevated venous thromboembolism (VTE) incidence despite guideline-adherent thromboprophylaxis5. The nonspecific clinical manifestations of deep vein thrombosis (DVT) in this population frequently lead to underdiagnosis, potentially resulting in severe complications including hypotension, hypoxia, and sudden death8. Therefore, early identification of patients at high risk of DVT and timely intervention are crucial. However, there is a lack of study and risk-scoring scale specifically for critically ill patients with sepsis. The Caprini scale is primarily used for surgical patients, whereas the Wells score is mainly used for outpatients. They both lack some of the high-risk factors seen in sepsis, such as systemic inflammatory response, multiple organ dysfunction, and invasive mechanical support.
This retrospective study aims to investigate the risk factors of DVT in patients with sepsis and serve as a foundation for the subsequent development of diagnostic criteria and risk stratification tools, thereby guiding clinical prevention and management.
Method
Study design
We conducted an observational study to analyze the clinical data of patients who met the diagnostic criteria of sepsis during their hospitalization in the ICU of West China Hospital of Sichuan University from January 2015 to May 2022. We followed the reporting standards set by Reporting of studies Conducted using Observational Routinely collected health Data in this study9. The study was approved by the ethics committee of West China Hospital of Sichuan University (Chengdu, China; approval number WCH 2023–2333). Informed consent was waived due to the retrospective and observational nature of the study. This study was conducted in accordance with the principles of the Declaration of Helsinki.
Patient population
The inclusion criteria were as follows: (1) diagnosed with sepsis; (2) adult patients aged ≥ 18 years old; (3) ICU stay > 72 h. We excluded patients who met any of the following criteria: (1) incomplete information on ultrasound; (2) pre-existing DVT prior to ICU admission; (3) incorporation of malignant tumors (such as leukemia and liver cancer); (4) long-term treatment with glucocorticoids; (5) trauma patients; (6) surgery ≥ 45 min; (7) pregnancy.
Diagnosis criteria
According to the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)10, sepsis was diagnosed by infection with Sequential Organ Failure Assessment (SOFA) score ≥ 2.
Based on the definition of the prevalence and incidence of DVT in ICU as defined in the existing literature4, patients with DVT diagnosed by venous ultrasonography within 72 h of admission to ICU were excluded. DVT was diagnosed if ultrasonography reported thrombosis in any vein listed in Supplementary Table S111.
Data collection
Clinical data were collected by reviewing the electronic medical record database of the Department of Critical Care Medicine of West China Hospital, Sichuan University.
From each patient, we thoroughly collected the following information: demographic characteristics (age, sex, body mass index (BMI), and ethnicity), medical data (SOFA score, Caprini score, vital signs on admission to ICU, medication use, rehabilitation, thromboprophylaxis, mechanical ventilation, and intravenous catheterization), diagnosis (etiology of sepsis, complications and comorbidities), laboratory tests (biochemistry, inflammatory index, hematology, coagulation, blood gas analysis, site of infection and microbiology), past medical history, and family history. The multiple imputation of chained equations (MICE) technology in R language was used to process missing data. The missing data situation is shown in Supplementary Table S2.
Statistical analysis
Demographic characteristics and other baseline values were described using descriptive statistics. Continuous variables were tested for normality by the Shapiro-Wilk test and Histogram. Data of normal distribution was described by means and standard deviations. Data of skewed distribution was reported as medians and interquartile ranges (IQR). Categorical variables were reported as percentages.
The χ2 test or Fisher’s exact probability method was used for the comparison of categorical variables, Wilcoxon rank sum test or t test for the comparison of continuous variables. Variables showing an univariable relationship with DVT (p < 0.1) were entered into a multivariable logistic regression model to calculate the odds ratio (OR) and 95% confidence interval (CI). We generated receiver operating characteristic curves (ROC) to calculate the cut-off of the continuous variables which were subsequently converted into binary data. A forest plot and nomogram based on the result of the multivariable logistic regression model were generated.
All statistical analyses were performed using packages implemented in R software, V.4.2.3, and the statistical significance of the two-sided tests performed was set at 0.05.
Results
Characteristics of the study population
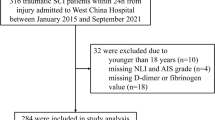
A total of 3143 patients diagnosed with sepsis using Sepsis-3 criteria were enrolled. 1057 patients were finally included in the analysis, of which 458 cases developed DVT and 599 cases without DVT (Fig. 1). The median age in the DVT group was 58 years (IQR 48–71) versus 51 years (IQR 37–67) in the non-DVT group. 68.7% of patients included were men and 30.6% had shock upon admission and required vasoactive drugs to maintain circulation. The most common comorbidities were hypertension (29.7%), diabetes (18.7%), and chronic obstructive pulmonary disease (6.1%) (Table 1).
Risk factors of DVT in sepsis patients
There were no significant differences between the patients with DVT and those without DVT in terms of BMI, SOFA score, Caprini score, platelet count, prothrombin time (PT), and activated partial thromboplastin time (APTT) at admission (p > 0.05). Compared with patients without DVT, patients with DVT had a longer median duration of mechanical ventilation (393.6 vs. 225.2 h; p < 0.001), vasoactive drugs (390.6 vs. 223.6 h; p < 0.001), ICU stay (19.8 vs. 11.8 d; p < 0.001), and hospitalization (28 vs. 20 d; p < 0.001) (Table 2).
The proportion of sex, insertion of central venous catheter (CVC) or peripherally inserted central catheter (PICC), bedridden status before admission, emergency surgery, recent fracture history, cases of shock requiring vasopressors, utilization of antiplatelet, drugs to improve circulation, and glucocorticoid were similar between the two groups (p > 0.05). Significant differences in intermittent pneumatic compression and anticoagulation were found between DVT and non-DVT patients (p < 0.001) (Supplementary Table S3).
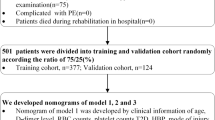
Multivariable logistic regression showed that independent risk factors for DVT were older age, prolonged use of vasoactive drugs, elevated D-dimer, absence of intermittent pneumatic compression, decreased fibrinogen, low oxygenation index, and respiratory infection (Table 3). Whereas anticoagulation treatment did not reach statistical significance. Based on the final multivariable model, a forest plot (Fig. 2) and a nomogram were generated (Fig. 3).
Subgroup analysis of patients with chemoprophylaxis
There was no significant difference in the duration and dosage of anticoagulation between the patients with and without DVT (Supplementary Table S4). The prevalence of comorbidities did not differ significantly among patients on anticoagulant or antiplatelet regimens (Supplementary Table S5 and S6).
Nomogram for predicting the probability of DVT in patients with sepsis. Each variable is individually plotted on the nomogram axis and assigned a partial score from the upper point scale. The sum of all partial scores yields a total score, which is then projected onto the lower total point scale to determine the corresponding predicted probability of DVT.
Discussion
Patients in the ICU exhibit a higher risk of DVT compared to general hospital populations. Studies on DVT in critically ill patients have been conducted since the 1980s, but explorations specifically for sepsis are still inadequate12,13. Current risk stratification tools demonstrate limited clinical utility in sepsis due to non-specific risk categorization and inadequate weighting of critical sepsis-related factors14,15. Both the Caprini and the Wells scores are initially developed for the evaluation of DVT in the general population, which may not be reliable in septic patients. For instance, the latest update of the Caprini scale assigns only one point to serious infection16. Septic patients often present with altered mental status or are sedated, posing challenges in accurately evaluating certain clinical signs and symptoms included in the Wells score. Consequently, the risk of DVT in patients with sepsis may be underestimated by existing scales. Besides, international guidelines lack recommendations on DVT risk assessment models for critically ill patients17. Therefore, no applicable scale exists for evaluating DVT in critically ill patients with sepsis. To address these limitations, the development of a specific assessment tool that incorporates the unique risk factors and pathophysiological markers associated with sepsis is needed.
To our knowledge, this is one of few studies evaluating DVT risk factors specifically in classical sepsis patients after rigorous exclusion of major confounders including trauma, cancer, and pregnancy. In this study, we analyzed data from 1057 patients with sepsis and developed a nomogram for the prediction of DVT. The result showed that the use of intermittent pneumatic compression was a protective factor for DVT. Consistent with our findings, a prospective cohort study conducted in the adult medical-surgical ICU showed that pneumatic compression was associated with a lower risk of VTE, irrespective of concurrent administration of pharmacologic thromboprophylaxis18. However, mechanical thromboprophylaxis in critically ill patients is still debated19. A multicenter randomized controlled trial demonstrated that adding pneumatic compression to pharmacologic thromboprophylaxis did not result in a significantly lower incidence of DVT20. Another study by Charlisa D. Gibson also found that there was no added benefit of dual chemical and mechanical prophylaxis compared to chemoprophylaxis alone21. A meta-analysis demonstrated that in critically ill adults, low-molecular-weight heparin significantly reduces DVT incidence compared to controls, including a composite of no prophylaxis, placebo, or compression stockings only, while unfractionated heparin and mechanical compression demonstrated potential benefit22. However, despite the appropriate use of pharmacologic thromboprophylaxis, critically ill patients still demonstrated high rates of DVT, which vary from 7.8–37.5%5,20,21,23,24,25. In our study, the proportion of patients receiving pharmacologic thromboprophylaxis in the DVT group was greater than that in the group without DVT, while the subgroup analysis showed no statistical difference in anticoagulant duration or dose between the two groups. Critical knowledge gaps persist regarding the optimal dosing frequency of thromboprophylaxis and therapeutic drug monitoring timing in ICU patients26. We speculated that currently recommended DVT prophylaxis strategies may not be as effective in critically ill populations compared with patients in the general ward, and the current level of anticoagulation for sepsis may be insufficient. However, clinical characteristics vary, and the balance of thrombotic and bleeding risk can change daily among critically ill patients, making it difficult to initiate and determine the dosage of anticoagulation for individual patients.
It should be highlighted that the high incidence of DVT was more than a failure to provide thromboprophylaxis. Rather, this means patients with sepsis frequently develop DVT and clinicians should maintain a high clinical suspicion for DVT in these patients even when appropriate prophylaxis has been used5. Flow stasis, endothelial damage, and hypercoagulability often occur contemporarily in critically ill patients with sepsis, so they are more likely to meet Virchow’s triad4. Moreover, the dysregulated hemostasis and coagulation in severe sepsis differ from that of non-infectious critical illnesses. Although exact mechanisms remain incompletely understood, sepsis-induced endotheliopathy and associated molecular dysfunction have been well documented. Coagulopathy has been proposed to play a key role through the crosstalk between inflammation and coagulation pathways as a result of the destructive endothelial response of the host27. Inflammation, immunity, and coagulation participate in the systemic endothelial injury altogether, leading to hypercoagulability and impaired fibrinolysis28,29. This imbalance between procoagulant and anticoagulant pathways not only exacerbates the inflammatory response but also potentiates thrombosis, thereby establishing a self-perpetuating cycle of thrombo-inflammation30,31.
Our findings revealed that the prolonged use of vasoactive drugs was a significantly independent risk factor for DVT in patients with sepsis. Cook et al. also identified vasopressor use as a risk factor for acquired DVT in the ICU32. Prolonged use of vasoactive drugs often indicates microcirculatory disturbance and endothelial dysfunction, which again suggests the positive associations between endothelium and thrombosis. Besides, we found that the decreased oxygenation index and respiratory infection were associated with DVT. Previous studies have found that hypoxia is associated with the incidence of thrombosis33,34. A real-world study revealed that patients with respiratory infections were more likely to have pulmonary embolism as initial VTE presentation than other types of infection35. A letter published in Thrombosis Journal refers to hypoxia as a possible cause as well as a consequence of thrombosis in sepsis patients36. Thus, a better understanding of the pathways between endothelial dysfunction and hypoxia in thrombus formation could aid in the development of novel prophylactic therapies against thrombosis. Further, the key to preventing DVT may lie in controlling the pathophysiologic disorders of sepsis.
In addition, age, D-dimer levels, and fibrinogen levels were independently associated with DVT in patients with sepsis. There were no significant differences in the insertion of CVC or PICC, SOFA score, duration of mechanical ventilation, ICU stay, and hospitalization between the two groups, which is similar to previous studies15,21,37.
The risk assessment tool for DVT and optimal anticoagulation management has not been established in critically ill patients with sepsis. Large, well-designed, randomized control trials specifically studying thromboprophylaxis in patients with severe sepsis and septic shock are necessary to improve the prevention of DVT and advance our understanding and care of these vulnerable patients.
Our study has several strengths. We specifically focused on critically ill patients with sepsis. The potential interference of common risk factors of DVT such as trauma, cancer, and pregnancy were excluded in the selection of the study population. Nevertheless, our study has some limitations. First, the single-center/facility nature and small sample size of our study hinder the generalizability of our findings. Although our study of 1,057 patients surpasses the sample sizes of most sepsis-associated DVT studies conducted in Chinese populations38,39, this sample size may still be insufficient for robust subgroup analyses, particularly in smaller strata such as antiplatelet therapy recipients. Second, our study did not differentiate between proximal and distal thromboses, which exhibit distinct clinical implications regarding both progression risk and therapeutic management. Furthermore, our nomogram requires external validation in independent cohorts and comparative evaluation against established risk assessment tools. Since the present study was retrospective, patients in ICU were not regularly screened for DVT. The exclusion of patients without venous ultrasound records may have disproportionately removed lower-risk DVT candidates from our study, potentially introducing selection bias. We cannot completely exclude the possibility of DVT that occurred before ICU admission, although we attempted to mitigate this possibility by excluding patients with the presence of DVT or without ultrasound data at baseline. Nevertheless, our study is still important for further understanding of the risk factors for DVT in critically ill patients with sepsis, as well as clinical practice.
Prospective clinical studies across diverse healthcare settings with protocolized ultrasound screening intervals and medication adherence timelines are necessary to clarify baseline thrombosis prevalence and to differentiate proximal or distal DVT outcomes. Multicenter validation of the nomogram against established scores in diverse populations is also needed. While heparin remains the primary treatment of DVT, its efficacy is limited, and superior alternatives are still lacking. Recent research reveals the interplay between immunity and coagulation. Understanding these mechanisms could improve thrombotic risk assessment and anti-inflammatory anticoagulant therapies40.
Conclusions
In summary, in critically ill patients with sepsis, physical prophylaxis was found as an independent protective factor for DVT. In contrast, age, use of vasoactive drugs, D-dimer level, fibrinogen level, oxygenation index, and respiratory infection were noted as independent risk factors for DVT. Patients with sepsis in ICU are more likely to develop DVT, thromboprophylaxis should be implemented in this population unless contraindicated. Further studies are needed to explore risk stratification strategies and innovative approaches for DVT prevention, perhaps beyond the existing traditional methods.
Data availability
The data used in this study can be obtained by the corresponding author upon request.
Abbreviations
- ALB:
-
Albumin
- ALT:
-
Alanine transaminase
- APTT:
-
Activated partial thromboplastin time
- AST:
-
Aspartate transaminase
- AT-III:
-
Antithrombin III
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- CRP:
-
C-reactive protein
- CVC:
-
Central venous catheter
- DVT:
-
Deep vein thrombosis
- FDP:
-
Fibrinogen degradation product
- GNB:
-
Gram-negative bacteria
- GPB:
-
Gram-positive bacteria
- HDL:
-
High density lipoprotein
- INR:
-
International normalized ratio
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile ranges
- NE:
-
Neutrophilic granulocyte
- OR:
-
Odds ratio
- PICC:
-
Peripherally inserted central catheter
- PLT:
-
Platelet
- PT:
-
Prothrombin time
- ROC:
-
Receiver operating characteristic curves
- SOFA:
-
Sequential organ failure assessment
- TBIL:
-
Total bilirubin
- TT:
-
Thrombin time
- VTE:
-
Venous thromboembolism
- WBC:
-
White blood cell
References
Myles, P. S. Preoperative sepsis and postoperative thrombosis. BMJ 349, g5444. https://doi.org/10.1136/bmj.g5444 (2014).
Mejer, N. et al. Increased risk of venous thromboembolism within the first year after Staphylococcus aureus bacteraemia: A nationwide observational matched cohort study. J. Intern. Med. 275 (4), 387–397. https://doi.org/10.1111/joim.12147 (2014).
Donze, J. D., Ridker, P. M., Finlayson, S. R. & Bates, D. W. Impact of sepsis on risk of postoperative arterial and venous thromboses: large prospective cohort study. BMJ 349, g5334. https://doi.org/10.1136/bmj.g5334 (2014).
Boddi, M. & Peris, A. Deep vein thrombosis in intensive care. Adv. Exp. Med. Biol. 906, 167–181. https://doi.org/10.1007/5584_2016_114 (2017).
Kaplan, D. et al. VTE incidence and risk factors in patients with severe sepsis and septic shock. Chest 148(5), 1224–1230. https://doi.org/10.1378/chest.15-0287 (2015).
Malato, A. et al. The impact of deep vein thrombosis in critically ill patients: A meta-analysis of major clinical outcomes. Blood Transfus. 13(4), 559–568. https://doi.org/10.2450/2015.0277-14 (2015).
Yeh, Y. T. et al. Deep venous thrombosis and risk of consequent Sepsis event: A retrospective nationwide Population-Based cohort study. Int. J. Environ. Res. Public. Health 18(15). https://doi.org/10.3390/ijerph18157879 (2021).
Shorr, A. F. & Jackson, W. L. Jr. Deep vein thrombosis in the intensive care unit: underappreciated, understudied, and undertreated. J. Crit. Care 20(4), 301–303. https://doi.org/10.1016/j.jcrc.2005.08.003 (2005).
Benchimol, E. I. et al. The reporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med. 12(10), e1001885. https://doi.org/10.1371/journal.pmed.1001885 (2015).
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8), 801–810. https://doi.org/10.1001/jama.2016.0287 (2016).
Varrias, D. et al. The use of Point-of-Care ultrasound (POCUS) in the diagnosis of deep vein thrombosis. J. Clin. Med. 10(17). https://doi.org/10.3390/jcm10173903 (2021).
Pandey, A., Patni, N., Singh, M. & Guleria, R. Assessment of risk and prophylaxis for deep vein thrombosis and pulmonary embolism in medically ill patients during their early days of hospital stay at a tertiary care center in a developing country. Vasc. Health Risk Manag. 5, 643–648. https://doi.org/10.2147/vhrm.s6416 (2009).
Moser, K. M., LeMoine, J. R., Nachtwey, F. J. & Spragg, R. G. Deep venous thrombosis and pulmonary embolism. Frequency in a respiratory intensive care unit. JAMA 246(13), 1422–1424 (1981).
Hayssen, H. et al. Systematic review of venous thromboembolism risk categories derived from caprini score. J. Vasc. Surg. Venous Lymphat Disord. 10(6), 1401–1409. https://doi.org/10.1016/j.jvsv.2022.05.003 (2022).
Li, L. et al. Prevention, treatment, and risk factors of deep vein thrombosis in critically ill patients in Zhejiang Province, China: A multicenter, prospective, observational study. Ann. Med. 53(1), 2234–2245. https://doi.org/10.1080/07853890.2021.2005822 (2021).
Cronin, M. et al. Completion of the updated Caprini risk assessment model (2013 Version). Clin. Appl. Thromb. Hemost. 251076029619838052. https://doi.org/10.1177/1076029619838052 (2019).
Heijkoop, E. R. H. et al. Preferences for thromboprophylaxis in the intensive care unit: An international survey. Acta Anaesthesiol. Scand. 69(4), e70009. https://doi.org/10.1111/aas.70009 (2025).
Arabi, Y. M. et al. Use of intermittent pneumatic compression and not graduated compression stockings is associated with lower incident VTE in critically ill patients: A multiple propensity scores adjusted analysis. Chest 144(1), 152–159. https://doi.org/10.1378/chest.12-2028 (2013).
Helms, J., Middeldorp, S. & Spyropoulos, A. C. Thromboprophylaxis in critical care. Intensive Care Med. 49(1), 75–78. https://doi.org/10.1007/s00134-022-06850-7 (2023).
Arabi, Y. M. et al. Adjunctive intermittent pneumatic compression for venous thromboprophylaxis. N Engl. J. Med. 380(14), 1305–1315. https://doi.org/10.1056/NEJMoa1816150 (2019).
Gibson, C. D. et al. Prevalence and predictors of deep vein thrombosis in critically ill medical patients who underwent diagnostic duplex ultrasonography. J. Intensive Care Med. 35(10), 1062–1066. https://doi.org/10.1177/0885066618813300 (2020).
Fernando, S. M. et al. VTE prophylaxis in critically ill adults: A systematic review and network meta-analysis. Chest 161(2), 418–428. https://doi.org/10.1016/j.chest.2021.08.050 (2022).
Beitland, S. et al. Venous thromboembolism in the critically ill: A prospective observational study of occurrence, risk factors and outcome. Acta Anaesthesiol. Scand. 63(5), 630–638. https://doi.org/10.1111/aas.13316 (2019).
Tang, X. et al. Modern thromboprophylaxis protocol based on guidelines applied in a respiratory intensive care unit: a single-center prospective cohort study. Thromb. J. 20(1), 76. https://doi.org/10.1186/s12959-022-00439-2 (2022).
Lawall, H. et al. Prevalence of deep vein thrombosis in acutely admitted ambulatory non-surgical intensive care unit patients. BMC Res. Notes 7, 431. https://doi.org/10.1186/1756-0500-7-431 (2014).
Cauchie, P. What do we know about thromboprophylaxis and its monitoring in critically ill patients?? Biomedicines 9 8. https://doi.org/10.3390/biomedicines9080864 (2021).
Chang, J. C. Sepsis and septic shock: Endothelial molecular pathogenesis associated with vascular microthrombotic disease. Thromb. J. https://doi.org/10.1186/s12959-019-0198-4 (2019).
Levi, M. & van der Poll, T. Coagulation and sepsis. Thromb. Res. 149, 38–44. https://doi.org/10.1016/j.thromres.2016.11.007 (2017).
Schouten, M., Wiersinga, W. J., Levi, M. & van der Poll, T. Inflammation, endothelium, and coagulation in sepsis. J. Leukoc. Biol. 83(3), 536–545. https://doi.org/10.1189/jlb.0607373 (2008).
Levi, M. & Poll, T. Coagulation in patients with severe sepsis. Semin Thromb. Hemost. 41(1), 9–15. https://doi.org/10.1055/s-0034-1398376 (2015).
Semeraro, N., Ammollo, C. T., Semeraro, F. & Colucci, M. Sepsis, thrombosis and organ dysfunction. Thromb. Res. 129(3), 290–295. https://doi.org/10.1016/j.thromres.2011.10.013 (2012).
Cook, D. et al. Deep venous thrombosis in medical-surgical critically ill patients: Prevalence, incidence, and risk factors. Crit. Care Med. 33(7), 1565–1571. https://doi.org/10.1097/01.ccm.0000171207.95319.b2 (2005).
Yan, S. F., Mackman, N., Kisiel, W., Stern, D. M. & Pinsky, D. J. Hypoxia/Hypoxemia-Induced activation of the procoagulant pathways and the pathogenesis of ischemia-associated thrombosis. Arterioscler. Thromb. Vasc Biol. 19(9), 2029–2035. https://doi.org/10.1161/01.atv.19.9.2029 (1999).
Hamer, J. D., Malone, P. C. & Silver, I. A. The PO2 in venous valve pockets: Its possible bearing on thrombogenesis. Br. J. Surg. 68(3), 166–170. https://doi.org/10.1002/bjs.1800680308 (1981).
Frasson, S. et al. Infection as cause of immobility and occurrence of venous thromboembolism: Analysis of 1635 medical cases from the RIETE registry. J. Thromb. Thrombolysis 41(3), 404–412. https://doi.org/10.1007/s11239-015-1242-2 (2016).
Evans, C. E. Hypoxia and HIF activation as a possible link between sepsis and thrombosis. Thromb. J. 17, 16. https://doi.org/10.1186/s12959-019-0205-9 (2019).
Alikhan, R. et al. Risk factors for venous thromboembolism in hospitalized patients with acute medical illness: analysis of the MEDENOX study. Arch. Intern. Med. 164(9), 963–968. https://doi.org/10.1001/archinte.164.9.963 (2004).
Wang, L. et al. Factors influencing DVT formation in sepsis. Thromb. J. 22(1), 11. https://doi.org/10.1186/s12959-024-00582-y (2024).
Chen, X., Huang, J., Liu, J., Deng, H. & Pan, L. Venous thromboembolism risk factors and prophylaxis of elderly intensive care unit patients in a Chinese general hospital. Ann. Palliat. Med. 10(4), 4453–4462. https://doi.org/10.21037/apm-21-464 (2021).
Galli, E., Maggio, E. & Pomero, F. Venous thromboembolism in sepsis: from bench to bedside. Biomedicines 10(7). https://doi.org/10.3390/biomedicines10071651 (2022).
Acknowledgements
We thank Yimai Xyu for assistance with data attraction.
Funding
This study was supported by the NASPAS project of West China Hospital of Sichuan University [Grant No. HX-H2312442]. This funding body had no influence on the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
J.S. and X.T. contributed equally to this article. W.H.Y., J.S., T.J.Z., and R.Z. contributed to study conception and design. J.S. and X.T. takes responsibility for drafting the manuscript. W.H.Y., T.J.Z. and R.Z. provided critical consultancy on the study implementation. JS analyzed the data. W.H.Y., J.S., X.T., R.Z., T.J.Z. interpreted the data. L.Y., M.L.H., X.C., and X.L. contributed to data acquisition. W.H.Y. are responsible for revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The study was approved bythe ethics committee of West China Hospital of Sichuan University (Chengdu, China; approval number WCH 2023–2333). Informed consent was waived due to the retrospective and observational nature of the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Su, J., Tie, X., Zhou, R. et al. Risk factors and a nomogram model for deep vein thrombosis in critically ill patients with sepsis: a retrospective analysis. Sci Rep 15, 16641 (2025). https://doi.org/10.1038/s41598-025-01660-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01660-5