Abstract
Stress is a normal human physiological reaction that can unfavorably affect the body, such as cardiac and immunological disturbances. Several articles have shown how stress can affect the immune status. This study was designed to assess the impact of stress on the immune system using the WBC count as an indicator of immune status in the human body. In a tertiary care teaching hospital, a prospective observational study was carried out with a total of 309 samples collected; two complete blood counts were observed for each patient, one at the anesthesia clinic one week before the surgery and the other on the day of the surgery immediately following the beginning of the surgery; and each patient answered a Hospital Anxiety Depression Scale form just before presenting to the operating room for stress level assessment. Representative serum samples from patients with and without anxiety were assessed for proinflammatory and anti-inflammatory profiles via ELISA. In our study of 309 patients, 31.4% experienced stress, with the majority being females. Age did not significantly impact stress levels, but preoperative preparation and information gathering were significantly related to stress (P value.05), as the mean stress was highest among those using online searching as their primary source of information. The difference in immune mediators (WBCs, lymphocytes, and neutrophils) before and on the day of surgery was correlated with stress, with WBCs and lymphocytes showing a statistically significant decrease in P values (0.019, 0.016). In contrast, neutrophils increased acutely (P value.006). A total of 71.4% of patients suffering from postoperative complications were stressed before the procedures, with a strong association (P value of 0.003). In addition, the levels of the proinflammatory cytokines IL-1b, IL-6, TNF-a, and IL-2 were significantly increased by 4-, 10-, 2-, and 3-fold, respectively, in the sera of participants who were anxious compared with those who had no anxiety. Stress is associated with decreased WBCs and lymphocytes, and increased neutrophils. Therefore, stress should be considered a modifiable preoperative risk factor. Incorporating psychological assessments in anesthesia clinics may help identify and manage patients with high anxiety. The use of anxiolytics could be considered in selected cases, pending further evaluation of evidence.
Similar content being viewed by others
Introduction
Stress is a normal human physiological reaction. When the human body experiences a change or challenges (stressors), it produces physical and mental responses to adjust to the new situation. This can be positive, keeping us alert, motivated, and ready to avoid danger. However, stress is known to cause many other physiological changes that can unfavorably affect the body, such as cardiac and immunological disturbances. Stress is subjective and cannot be precisely measured; it can be estimated by a health care provider via many assessment tools1.
As this study aimed to investigate the effect of stress on the immune system, we found that the WBC count was the best indicator of immune status in the human body.
A white blood cell (WBC) count is a test that measures the number of white blood cells in the body and is often included with a complete blood count (CBC), which is commonly used to screen for different conditions that may affect overall health2. The immune system’s goal is to defend the body from pathogenic organisms and from substances that the body would be harmed by. White blood cells, or immune system cells, are carried by blood throughout the body and are also found in many organs, such as the bone marrow, thymus, lymph nodes, and spleen. White blood cells are present in a variety of varieties, but lymphocytes are the most crucial in this situation. The normal range is typically between 4,000 and 11,000/month in most healthy individuals3.
Moreover, stress is linked to modifications in the way the immune cell’s function. In other words, after stress, there is a noticeable decrease in both lymphocyte proliferation and natural killer cell activity. The available data suggests that stress may reduce functional immune system competence. Emotional stresses such as the death of a family member, divorce, and major depression all have immunological links, that is, depressed lymphocyte counts and decreased responsiveness of lymphocytes to mitogens4. There is a clear effect of acute stress on neutrophils, in which it causes an acute and abrupt increase in neutrophil count and thus plays an important role in immunity, as neutrophils are important immune cell mediators5.
To conduct this study, we had to look for specific populations who are experiencing certain life events that are supposed to be preceded by a significant amount of stress. A very good example of these populations is patients undergoing elective surgeries. These patients are supposed to express significant levels of stress and anxiety before surgery.
Elective surgery is a planned, nonemergency surgical procedure. In this study, elective surgeries were much preferred over emergency surgeries. Elective surgery differs from emergency surgery in that patients have time to prepare themselves and to be prepared for surgery, so we will have enough time to assess their preoperative stress. In addition, attempting to assess the stress level in a patient requiring emergent medical intervention may delay treatment, which may cause serious harm to the patient.
Preoperative care is the physical and psychological aid given to a patient before surgery to ensure their safety, as the preoperative period lasts from the time the patient is scheduled for surgery until they are taken to the operating room. Many preoperative tests and clinical evaluations can be performed during a preoperative outpatient session, one week or more before surgery, in addition to the preoperative care provided in the hospital. For example, studies suggest that individuals who are more stressed before surgery report greater postoperative complications, such as infections, pain, and long recovery times6.
In Palestine, there is a lack of literature reviews and medical research on psychological health issues. Therefore, this study aimed to explore the association of stress and preoperative psychological preparation with immune function, inflammatory markers, and surgical outcomes among adults undergoing elective surgeries under general anesthesia.
Methods
Study design and setting
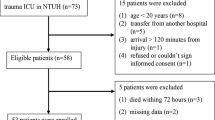
A prospective observational study was conducted between August and November 2023 among patients undergoing elective surgeries at An-Najah National University Hospital in Nablus, Palestine.
Study population
Our study included patients who underwent elective surgeries under general anesthesia and were older than 18 years at Al-Najah National University Hospital. All emergent and urgent surgeries; patients with infection, splenectomy, pregnancy, clinically diagnosed blood disorders, malignancies or psychological disorders; and patients taking drugs affecting WBC count, such as antibiotics, anticonvulsants, antihistamines, antithyroid drugs, arsenicals, barbiturates, chemotherapy, diuretics, sulfonamides, beta blockers, corticosteroids, epinephrine, heparin, and lithium, were excluded.
Sample size and sampling technique
According to the Palestinian health information center, our estimated population will be around (131000). By using Raosoft with a 5% margin of error, 95% confidence interval, and 1.96 Z score, the minimum required sample size was 294, adding 10% for error reduction, with a sample size = 309. The participants were recruited via a convenient sampling technique, ensuring that they met the inclusion criteria.
Measurement tool, validity, and reliability
The participants’ data were collected, and they were asked to provide informed consent for a self-administered questionnaire. It was taken from a standardized Hospital Anxiety Depression Scale (HADS). The HADS is a self-reported 14-item rating scale with a 4-point Likert scale (ranging from 0 to 3). It is designed to measure anxiety and depression (7 items for each subscale). The total score is the sum of the 14 items, and for each subscale, the score is the sum of the respective seven items ranging (from 0 to 21) and is divided into three categories: normal (0–7), borderline abnormal (8–10) and severe stress (11–21). However, in our study, we divided the data into no stress (0–8) and stress (9–21) groups according to previous studies, which revealed that the optimal cutoff was > 9 units for the HADS-A score and > 7 units for the HADS-D score. A demographics section was added at the beginning of the questionnaire, which included age, sex, and preoperative patient preparation.
This scale was used in previous studies, such as “Psychological distress and associated factors among Palestinian advanced cancer patients: A cross-sectional study”, which was published online in 20227. Additionally, the Arabic version of the scale that we used in our study has been confirmed to be a reliable and valid tool to assess mood states in hospitalized patients in a study titled “Development and Validation of Arabic Version of the Hospital Anxiety and Depression Scale”, which was published in the Saudi Journal of Anesthesia in 20178.
We also recorded the WBC, neutrophil, and lymphocyte counts at the clinic no more than one month before the surgery and on the day of surgery. This questionnaire was appropriate for our study, as we wanted to assess the level of anxiety as an acute process before surgery and its relationship with the WBC on the day of surgery.
We collected 309 paper questionnaires in which each patient completed the survey while preparing for the operation in the day care department. We then entered patients’ information into an online Google form for better ranking, preparing for analysis.
Sample collection
Blood samples from patients diagnosed with anxiety were collected into serum separator tubes (SST, gold-top) and allowed to clot at room temperature for approximately 30 min. Samples were centrifuged at 1500–2000 × g for 10 min to obtain clear serum. Serum samples were aliquoted and stored at -80 °C until cytokine analysis. Two CBCs were collected: the first was routinely done at the anesthesia clinic, and researchers recorded the readings from the medical files at An-Najah National University Hospital. The second blood sample, drawn immediately during the anesthesia induction phase before surgery, was processed by the specialized staff at An-Najah National University Laboratory to perform both the CBC and the cytokine analysis using serum obtained from the same blood sample.
Background variables and outcomes
Immunity status of patients determined via WBC counts and lymphocyte and neutrophil percentages as immune system mediators. Surgical outcomes (postoperative complications) were assessed by calling patients and asking about fever, wound infection, and any local or systemic signs of inflammation within 72 h after surgery.
Luminex MAGPIX tests
Multiplexed sandwich enzyme-linked immunosorbent assay‐based technology (Cat# MHSTCMAG-70 K; R&D Systems) was used to simultaneously determine the concentrations of multiple cytokines (IL-6, IL-2, IL-1β, IL-10, and TNF-α). Samples from each group were analyzed as described in the manufacturer’s instructions.
Statistical analysis
The data were coded, categorized, and entered into the Social Science Statistical Package (IBM-SPSS), version 21.0. Descriptive statistics are presented as frequencies and percentages for categorical variables and medians and interquartile ranges (IQRs) for continuous variables. The Pearson test was used to assess correlations. Either the chi-square test or Fisher’s exact test, as appropriate, was used to test the significance of differences between categorical variables. The Mann‒Whitney test was used for differences in the means between categories. The significance level was established at a p-value < 0.05.
Results
A total of 309 patients participated in the study. The mean age of the participants was 43.08 years (ranging from 27 to 59), with 70.6% male and 29.4% female. Most of the patients were prepared preoperatively by their doctors (71.5%) (Table 1).
Table 2 displays the influence of demographic variables on patients’ stress levels. While age was not significantly associated with stress (P = 0.146), other factors were noteworthy. The participants aged 18–28 years reported the highest stress at a rate of 29.9%, whereas the oldest group reported very minimal stress. Gender differences were evident: with a P value of less than 0.001, women experienced stress more frequently (52.7.4%) than men did. The impact of preoperative preparation on stress was also statistically significant, as the majority of respondents (41%) attributed stress to their research via the internet. These findings underscore the importance of considering demographic factors when assessing stress in clinical settings.
Table 3 presents the effects of stress and preoperative preparations on patients’ outcomes postoperatively. Both factors had a statistically significant effect on postoperative complications, with P values of 0.003 and 0.002, respectively. Most of the patients with wound infection experienced stress (70%), and 75% of the patients with systemic inflammatory symptoms were stressed preoperatively. While 80% of patients complaining of local infection had their preoperative preparation by searching websites, half of those who experienced systemic infection were prepared by their doctors, and the other half were prepared by searching on the internet for general knowledge about their surgery. Notably, none of the patients whose information was obtained from a scientific brochure were susceptible to postoperative complications.
Table 4 indicate that there is a significant and worthwhile relationship between stress and our immune system indicators (leukocytes, lymphocytes, and neutrophils), in which there was an obvious decrease in both leukocytes and lymphocytes among stressed patients, with values of 0.019 and 0.016, respectively. Otherwise, the mean neutrophil count increased during acute stress, with a P value of 0.009.
Table 5 shows that there was no statistically significant relationship between preoperative preparation and changes in WBCs, lymphocytes, or neutrophils, as there was no significant difference between their means post- and preoperatively. The P values were 0.334, 0.812, and 0.752, respectively.
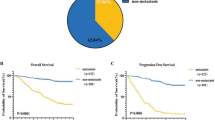
Figure 1 indicates that there were significantly increased levels of the proinflammatory cytokines IL-1b, IL-6, TNF-a, and IL-2 by 4-, 10-, 2-, and 3-fold, respectively, in the sera of participants who were anxious compared with those who had no anxiety. On the other hand, the concentration of the anti-inflammatory cytokine IL-10 was 2.3-fold lower in the anxiety group than in the control group, which indicates a disturbance in the inflammatory balance of that particular group. These findings underscore the role of acute stress and anxiety in the immune system and could provide insights into potential therapeutic targets.
Multiplexed sandwich enzyme-linked immunosorbent assays were used to determine simultaneously the concentrations of IL-1β, IL-6, TNF-α, IL-2, and IL-10. Analyses were performed as described by the manufacturer’s kit. The data are presented as the means ± SDs (n = 10 in healthy donors and n = 15 in people with anxiety). Significance was determined via Newman–Keuls two-way analysis of variance (ANOVA). Interleukin 1 beta (IL-1β), interleukin 6 (IL-6), tumor necrosis factor-alpha (TNF-α), interleukin 2 (IL-2), and interleukin 10 (IL-10).
Discussion
The current study findings revealed that 31.4% of patients who participated experienced stress. Furthermore, many studies indicate a link between preoperative stress and poor patient outcomes, which suggests that significant levels of patient-reported preoperative anxiety independently predict a greater risk of in-hospital mortality or major morbidity9. Thus, to reduce preoperative stress, it is necessary and recommended that every patient have their anxiety assessed. Although there were a few cases of postoperative complications (4.5%), this might be attributed to the antibiotics being administered to patients post-operation, potentially masking the occurrence of these complications. According to our study, 71.2% of patients who experienced complications after surgery were suffering from anxiety preoperatively, which is consistent with many studies that emphasized that increasing preoperative anxiety levels lead to disrupted recovery from anesthesia, control of postoperative pain, and patient satisfaction10,11. In our study, there was no direct correlation between changes in white blood cells and complications after the operation, so we cannot prove that changes in white blood cells, neutrophils, or lymphocytes increase the chance of postoperative complications.
In our study population, stress among females was greater than that among males, which is consistent with other studies indicating that female patients reported significantly more preoperative anxiety than male patients did12,13. Another study revealed that females have higher anxiety levels and that women have greater immune responsiveness than men do; moreover, sex hormones can alter immune responses, potentially increasing their susceptibility to autoimmune disorders and stress-related issues, thereby increasing their immune status14.
An evaluation of the effects of age groups on anxiety revealed that age was not found to affect anxiety levels, as individuals across all age groups presented similar levels of anxiety; thus, there was no specific age group susceptible to stress or a change in immune state. Several previous studies have shown that anxiety varies by age group, with younger people showing greater susceptibility to stress and worry under different conditions15,16.
White blood cells (WBCs) and their differentials were utilized as immune mediators, in alignment with a similar previous study, which revealed significant and positive relationships between stress-induced changes in perceived stress and the number of leukocytes and neutrophils and negative relationships between stress-induced changes in the CD4+/CD8 + ratio and stress-induced changes17. This study revealed that patients who experienced anxiety had a lower mean white blood cell count than did those who did not, which was statistically significant and compatible with another study that clarified the complex interaction between WBCs and stress. Humans respond to acute stress by increasing the quantity of leukocytes, or white blood cells, in the blood. These leukocytes originate from the lymph nodes, bone marrow, and spleen, among other locations. However, as the stress disappears, these cells either return to their original compartments or migrate to other organs (such as the skin or lungs). Leukocytes enter the bloodstream minutes after stress begins. Monocytes, lymphocytes, T helper cells, cytotoxic T cells, B cells, and natural killer cells all decrease in number throughout this phase, but neutrophils continue growing. Understanding the entire dynamics of this response is essential. While later measures predominantly show trafficking (decreased numbers), early measurements during stress primarily reflect mobilization (increased numbers). This disparity explains why, during and after acute stress, human studies frequently indicate an increase in blood leukocyte counts, whereas other studies show decreases5.
This study is highly coherent with our study in which there was a significant correlation between the changes in lymphocytes and neutrophils and stress levels. There was a clear increase in the neutrophil percentage among stressed patients, which is explained above, and in contrast, there was a significant decrease in the lymphocyte count. Similar results have been obtained in many studies that demonstrated how stress levels affect the numbers and functions of leukocytes and their precursors and that the immunological response decreases with increasing stress exposure18. Some stressors lead to the activation of the hypothalamic‒pituitary‒adrenal (HPA) axis as well as the sympathetic nervous system, thereby interfering with immune and inflammatory signals. Several proinflammatory cytokines have been associated with systemic inflammation, and their modulation of mood and appetite has been suggested to contribute to anxiety. The study’s findings revealed significantly increased levels of IL-1β, IL-6, TNF-α, and IL-2, along with a notable decrease in IL-10, reflecting a disruption in the inflammatory balance among anxious patients. These results reinforce the role of acute stress and anxiety in modulating immune responses and may help identify potential therapeutic targets.
This phenomenon is further illustrated by findings from a physiological stress model involving parachutists, where researchers measured plasma catecholamine and cortisol levels in addition to enumerating blood T and NK cells. The number of T and NK cells increased immediately after a high jump, followed by a significant decrease one hour later, highlighting the dynamic and time-sensitive nature of immune cell trafficking in response to acute stress19.
According to previous studies, stressors stimulate the hypothalamic‒pituitary‒adrenal axis and the sympathetic nervous system, which disrupts immunological and inflammatory responses. Proinflammatory cytokines are linked to systemic inflammation. Research comparing the cytokine profiles of people with and without anxiety revealed increased levels of proinflammatory cytokines and decreased levels of anti-inflammatory cytokines, indicating that stress plays a role in immune responses and immunity. A meta-analysis of 34 studies was performed that measured circulating inflammatory markers, and 15 studies that measured stimulated production of inflammatory markers before and after exposure to acute stress were included. The results revealed significant stress-related increases in the levels of circulating interleukin (IL)-1β, IL-6, IL-10, and tumor necrosis factor (TNF), but not in the levels of IL-1ra, IL-2, interferon-γ, or C-reactive protein20.
The study revealed that the sources of preoperative information about the procedure significantly affect stress levels. In particular, individuals who obtained information from the internet experienced higher levels. This highlights the importance of engaging with healthcare providers to reduce anxiety. Previous studies have debated the effect of preoperative education on post-surgery pain10. Some studies, such as “Preoperative education for hip or knee replacement,” have suggested that preoperative education stratified according to physical, psychological, and social needs can be beneficial, especially for patients with depression, anxiety, or unrealistic expectations21.
In this research, our strengths included ease of communication with patients, the presence of an anesthesia clinic that facilitates access to patient information and laboratory results preoperatively, the ability to draw blood samples during surgery, and the ease of transporting samples to a laboratory at the university to obtain CBCs.
However, there were several limitations, such as the collection of samples from a single hospital, which might affect the ability to generalize our results. Another difficulty we faced was the inability to accurately assess postoperative complications due to antibiotic intake post-operation as a protocol in the hospital and the difficulty of asking patients one by one about their complications, as many of them did not respond immediately or at the right time.
Conclusion
This study sheds light on how deeply preoperative anxiety can shape patients’ postoperative experiences, not only in terms of surgical complications but also in their immune responses, as seen through changes in leukocyte counts. Women in particular appeared more vulnerable to preoperative stress, while age did not show a clear pattern. These observations reaffirm the importance of preparing patients psychologically, not just medically, before surgery. Providing emotional support and clear information may ease patients’ anxiety and potentially reduce postoperative complaints. Future studies are encouraged to delve deeper into how stress affects immune function and to evaluate whether safe, evidence-based interventions, such as anxiolytics, could support patients’ physical and psychological recovery alike.
Data availability
All data from the current work are obtainable from the corresponding author. a.hanani@najah.edu.
Abbreviations
- WBCs:
-
White blood cells
- HADS:
-
Hospital Anxiety Depression Scale
- MAGPIX test:
-
Multiplexed sandwich enzyme-linked immunosorbent assay-based technology
- HAP:
-
Hypothalamic–Pituitary Adrenal
- TNF:
-
Tumor necrosis factor
- IL-2:
-
Interleukin 2
- IL-6:
-
Interleukin 6
- IL-1B:
-
Interleukin 1 beta
References
Giudice, M. D. et al. Haruka Wada, what is stress?? A systems perspective. Integr. Comp. Biol. 58 (Issue 6), 1019–1032 (2018).
Higuera, V. Mar. WBC (white blood cell) count: purpose, procedure, and results. Healthline 2024, 7 (2024). www.healthline.com/health/wbc-count.
Kutlu, H., Avci, E. & Özyurt, F. White blood cells detection and classification based on regional convolutional neural networks. Med. Hypotheses. 135, 109472. https://doi.org/10.1016/j.mehy.2019.109472 (2020).
Institute of Medicine (US) Committee on Military Nutrition Research; Marriott BM, editor. Food Components to Enhance Performance: An Evaluation of Potential Performance-Enhancing Food Components for Operational Rations. Washington (DC): National Academies Press (US). 10, Endocrine and immune system responses to stress (1994).
Dhabhar, F. S., Malarkey, W. B., Neri, E. & McEwen, B. S. Stress-induced redistribution of immune cells–from barracks to boulevards to battlefields: a Tale of three hormones–Curt Richter award winner. Psychoneuroendocrinology 37 (9), 1345–1368. https://doi.org/10.1016/j.psyneuen.2012.05.008 (2012).
Johnstone, J. How to provide preoperative care to patients. Nurs. Stand. 35 (12), 72–76. https://doi.org/10.7748/ns.2020.e11657 (2020).
Abu-Odah, H., Molassiotis, A., Zhao, I. Y., Su, J. J. & Allsop, M. J. Psychological distress and associated factors among Palestinian advanced cancer patients: a cross-sectional study. Front. Psychol. 13, 1061327. https://doi.org/10.3389/fpsyg.2022.1061327 (2022).
Altirkawi, K. Development and validation of Arabic version of the Hospital Anxiety and Depression Scale (2022).
Williams, J. B. et al. Preoperative anxiety as a predictor of mortality and major morbidity in patients aged > 70 years undergoing cardiac surgery. Am. J. Cardiol. 111 (1), 137–142. https://doi.org/10.1016/j.amjcard.2012.08.060 (2013).
Louw, A., Diener, I., Butler, D. S. & Puentedura, E. J. Preoperative education addressing postoperative pain in total joint arthroplasty: review of content and educational delivery methods. Physiother Theory Pract. 29 (3), 175–194. https://doi.org/10.3109/09593985.2012.727527 (2013).
Turksal, E., Alper, I., Sergin, D., Yuksel, E. & Ulukaya, S. Efeitos Da Ansiedade pré-operatória Na recuperação anestésica e Na dor pós‐operatória Em Pacientes submetidos a nefrectomia Para Doação [The effects of preoperative anxiety on anesthetic recovery and postoperative pain in patients undergoing donor nephrectomy]. Braz J. Anesthesiol. 70 (3), 271–277. https://doi.org/10.1016/j.bjan.2020.03.010 (2020).
Domar, A. D. P. D., Everett, L. L. R. N. & Keller, M. G. Preoperative anxiety: is it a predictable entity?? Anesth. Analgesia. 69 (6), 763–767 (1989).
Celik, F. & Edipoglu, I. S. Preoperative anxiety and fear of anesthesia were evaluated via the APAIS score. Eur. J. Med. Res. 23 (1), 41. https://doi.org/10.1186/s40001-018-0339-4 (2018).
Ansar Ahmed, S., Penhale, W. J. & Talal, N. Sex hormones, immune responses, and autoimmune diseases. Mechanisms of sex hormone action. Am. J. Pathol. 121 (3), 531–551 (1985).
O’Neill, C. D. P. D. et al. Sex and age differences in anxiety and depression levels before and after aerobic interval training in cardiac rehabilitation. J. Cardiopulmon. Rehabil. Prevent. 42 (1), 15–21. https://doi.org/10.1097/HCR.0000000000000617 (2022).
Varma, P., Junge, M., Meaklim, H. & Jackson, M. L. Younger people are more vulnerable to stress, anxiety and depression during the COVID-19 pandemic: a global cross-sectional survey. Prog Neuropsychopharmacol. Biol. Psychiatry. 109, 110236. https://doi.org/10.1016/j.pnpbp.2020.110236 (2021).
Maes, M. et al. The effects of psychological stress on leukocyte subset distribution in humans: evidence of immune activation. Neuropsychobiology 39 (1), 1–9. https://doi.org/10.1159/000026552 (1999).
Maydych, V. et al. Impact of chronic and acute academic stress on lymphocyte subsets and monocyte function. PLoS One. 12 (11), e0188108. https://doi.org/10.1371/journal.pone.0188108 (2017).
Schedlowski, M. et al. Changes in natural killer cells during acute psychological stress. J. Clin. Immunol. 13 (2), 119–126. https://doi.org/10.1007/BF00919268 (1993).
Alotiby, A. Immunology of stress: a review Article. J. Clin. Med. 13 (21), 6394. https://doi.org/10.3390/jcm13216394 (2024).
McDonald, S., Page, M. J., Beringer, K., Wasiak, J. & Sprowson, A. Preoperative education for hip or knee replacement. Cochrane Database Syst. Rev. 2014 (5), CD003526. https://doi.org/10.1002/14651858.CD003526.pub3 (2014).
Acknowledgements
We would like to express our sincere gratitude to An-Najah National University, An-Najah National University Hospital, and all the participating hospitals for their invaluable support in providing resources and facilitating the research process.
Author information
Authors and Affiliations
Contributions
SY, RM, RY, AS and JA contributed to the literature review, data collection, data analysis, and initial drafting of the manuscript. AAH and JZ were involved in study design, patient eligibility assessment, literature review, and provided essential revisions. They also drafted the manuscript, ensured data integrity, and critically reviewed the research to enhance its intellectual content. AAH and JZ conceptualized the study, ensured data integrity, and provided critical intellectual input. They also conceived and designed the research, supervised and coordinated data analysis, critically reviewed the interpretation of results, and assisted with the final manuscript preparation. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethical approval for this study was obtained from the Institutional Review Board (IRB) at An-Najah National University (approval number: Med.may.2023/13) and the administration of An-Najah National University Hospital for access to data and patient interviews. Informed consent was obtained from all participants prior to their involvement in the study. The participants were fully informed about the study’s purpose, procedures, and the confidentiality of their data. All participants consented to the anonymous use of their clinical data for research purposes, with the assurance that the data would only be used for clinical research and publication in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yaseen, S., Morgan, R., Yaseen, R. et al. Impact of stress and preoperative psychological preparation on immunity, inflammatory responses, and surgical outcomes in adults undergoing elective surgery with general anesthesia in Palestine. Sci Rep 15, 26253 (2025). https://doi.org/10.1038/s41598-025-01869-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-01869-4