Abstract
The severity and progression of Interstitial Lung Disease (ILD) can vary due to environmental, cultural and genetic factors. The relationship between disease severity and factors that determine the health status of people with ILD living in lower middle-income countries like India has not been evaluated. This study aimed to determine whether there were relationships between disease severity with functional exercise capacity and Health Related Quality of Life (HRQoL) among people with ILD in India. This was a prospective, single center observational study. All participants performed Pulmonary Function Test (PFT) including Forced Vital Capacity (FVC) % predicted, Diffusing Capacity of the Lung for Carbon Monoxide (DLCO) % predicted, 6 min Walk Distance (6MWD), St. George’s Respiratory Questionnaire (SGRQ), modified Medical Research Council (mMRC) dyspnoea scale. Eighty participants with ILD were recruited from September 2020 and December 2022. There were strong correlations between 6MWD with DLCO % pred (Spearman rho 0.891) and between SGRQ Total score and DLCO % pred (Spearman rho 0.906). There were no correlations between 6MWD and FVC % pred (Spearman rho 0.206) or between SGRQ and FVC % pred (Spearman rho 0.113). This study demonstrated strong correlations between disease severity measured by DLCO % pred with both functional exercise capacity and HRQoL in people with ILD in India.
Similar content being viewed by others
Introduction
Interstitial lung disease (ILD) is an umbrella term for a large group of diseases that cause interstitial fibrosis of the lungs1 ILDs are characterized by symptoms such as dyspnea, fatigue, and reduced exercise tolerance, which can greatly impact patients’ quality of life2,3,4 The progression of ILDs can vary, from being stable, to slowly or rapidly progressive, with the overall prognosis being poor5,6 Despite recent improvements in treatment options and diagnostic techniques, the mortality rate for ILDs globally remains high7.
Clinical evaluation, histopathologic sampling, and high-resolution computed tomography (HRCT) are effective methods for detecting and classifying ILDs. Pulmonary function testing (PFT), particularly the diffusing capacity for carbon monoxide (DLCO), is the most sensitive method for assessing the progression of ILDs8 DLCO is regarded as the most sensitive approach for measuring ILD progression because it precisely evaluates gas exchange efficiency, revealing early anomalies even before significant changes in lung capacity or airflow become apparent8 DLCO, as compared to FVC, is directly associated with the severity of the disease, especially in diseases like IPF, where decreases in DLCO are strongly correlated with a worse prognosis, higher rates of morbidity, and mortality. Additionally, it provides early impairment detection since it is more sensitive to the microvascular alterations linked to fibrosis. DLCO is an important tool in clinical practice and research because it is a critical prognostic indicator that aids in tracking the evolution of the disease and is linked to a decrease in exercise capacity, an increase in symptoms, and a decreased survival rate8,9,10,11,12,13,14 Strong correlations have been found between decreasing values of DLCO, disease severity and increased morbidity in ILDs, particularly in cases of idiopathic pulmonary fibrosis (IPF)9 Forced vital capacity (FVC) is another standard measure of pulmonary function for evaluating ILDs with a reduction in FVC over time considered a reliable indicator of disease progression15 and an independent predictor of mortality in patients with IPF15,16.
The 6-minute walk test (6MWT) is used to measure functional exercise capacity in people with ILD and is known to be a predictor of mortality17 Reduced lung volumes caused by irreversible pathological changes in the lungs can lead to the debilitating symptoms of dyspnea and fatigue and reductions in exercise capacity, muscle strength, and endurance, which can negatively impact patients’ physical and mental well-being and quality of life18,19,20,21 Studies have shown a relationship between disease severity and functional exercise capacity, which helps to understand the effects of the disease on patients,22,23,24,25 but there are no studies in an Indian population.
In developing countries like India, ILDs are often underdiagnosed at early stages due to tests and investigations like DLCO and HRCT not typically being performed due to under resourcing, lack of testing unless, lack of standardized approach for diagnosis and a tendency to rely on a single physician’s judgment. Additionally, factors such as patient reluctance, hesitancy, and the assumption of alternative diagnoses further contribute to delays in accurate diagnosis and management26,27,28,29 Using other more readily accessible tests that could indicate the ILD severity may be of benefit. The relationship between disease severity and HRQoL may be impacted by these diagnostic gaps because severity may be underestimated or missed in its early stages, resulting in distinct patient experiences when compared to higher-income countries26,27,28,29 ILDs in India are largely caused by environmental exposures, including smoke from biomass fuels, outdoor air pollution, and occupational exposures. These exposures may have a distinct impact on the course and symptoms of disease and are different from those frequently studied in high-income countries. Patient perceptions and reports of their quality of life may also be influenced by cultural variables, such as expectations for caregiving, familial obligations, and the stigma attached to chronic illnesses. Furthermore, the severity and progression of ILDs can vary due to environmental, cultural and genetic factors26,27,28,29.
Currently, the relationships between disease severity and factors that determine the health status of people with ILD living in lower-to middle-income countries like India have not been evaluated. Understanding these relationships may provide a measure of disease severity when other tests and investigations are unavailable. The aim of the study was to determine the relationship between disease severity, functional exercise capacity and health-related quality of life (HRQoL) in people with ILD in India, and to determine whether there were differences in these relationships according to sex and time since diagnosis.
Methods
Participants
People diagnosed with ILD who attended Kasturba Hospital, Manipal were recruited between September 2020 and December 2022. To be included in the study participants had to have an ILD diagnosed by HRCT,30,31 be able to perform a 6MWT, not had an acute exacerbation of ILD or any infection within the last 4 weeks and not have heart failure. The study was approved by the Kasturba Medical College and Kasturba Hospital Institutional Ethics Committee (IEC: 320/2020) and was registered in the Clinical Trials Registry of India (CTRI/2020/09/027788).32 Written informed consent was obtained from all the study participants and study was conducted in accordance with Declaration of Helsinki. In this study, ILD subtypes have been determined employing a multidisciplinary diagnostic (MDD) approach that involves collaboration among pulmonologists, radiologists, rheumatologists, and pathologists as needed. Clinical history, physical examination, serological testing, high-resolution computed tomography (HRCT) results, and, in certain situations, histological confirmation were used to classify ILDs. Because of its specific pathophysiology and treatment implications, RA-ILD was examined as a separate subgroup to highlight variations in clinical features and progression when compared to other forms of CTD-ILD.
The study classified patients with Non Specific Interstitial Pneumonia (NSIP) according to whether the illness was idiopathic or because of an underlying CTD. Patients with idiopathic NSIP were categorized separately, whereas those with secondary NSIP were included in the CTD-ILD category. This distinction was developed in order to enable the investigation of disease patterns and guarantee accurate grouping based on etiology.
A sample of 80 patients was chosen based on specified inclusion and exclusion criteria associated with the diagnosis of ILD.
This study is a subset of a larger study which is a randomized controlled trial (RCT)32 We calculated sample size for the RCT, the details have been published32 We recognize that the results generalizability may be constrained by the comparatively small sample size in terms of statistical power. Prior to the investigation, we did, however, perform a power calculation to make sure the sample size was adequate to identify clinically significant variations in key findings.
On the same day, all participants completed Pulmonary Function Tests (PFTs) consisting of spirometry (FEV1 and FVC), static lung volumes and DLCO which were compared to predicted normal values,33,34 a 6MWT according to standard protocol, with two tests conducted 30 min apart and the best distance used in analyses,35 the mMRC dyspnoea scale36 and the St George’s Respiratory Questionnaire (SGRQ)33,37.
PFTs, including spirometry and DLCO measurements, were performed using the Koko Spirometer (USA). This equipment was calibrated daily according to the manufacturer’s guidelines to ensure accuracy and consistency throughout the study. The predicted values for pulmonary function parameters were calculated using the ERS/ATS reference equations, which were selected to align with current clinical guidelines and ensure standardization across our measurements. Furthermore, to eliminate inter-device variability, all patients were assessed using the same spirometer. The tests were conducted by trained technicians who strictly adhered to the ATS/ERS guidelines for PFT performance33,34 This included proper patient preparation, adherence to technical standards, and the performance of at least three acceptable maneuvers for both spirometry and DLCO measurements. Only tests meeting the ATS/ERS quality criteria were included in the analysis. For spirometry, this required at least three reproducible maneuvers with a difference of ≤ 150 mL between the two highest FEV1 and FVC values. For DLCO, measurements were accepted if they met the criteria of a breath-hold time of 8–12 s, a washout volume of ≥ 0.75 L, and a sample collection time of 2–4 s. The mMRC is a self-assessment of the level of dyspnoea during mobility on a 0–4 scale with 0 rating ‘breathless while performing strenuous activities’ to 4 rating ‘too breathless to leave the house’ or ‘breathless when dressing’. The SGRQ examines the impact of respiratory disease across three domains: symptoms, impact and activity. The total score directly corresponds to the level of disability and has been validated in people with ILD, with a higher score indicating worse HRQoL37.
Given that the development of symptoms and the course of the disease in ILD usually intensify after the first few years of diagnosis, the 3-year diagnosis cut-off was chosen. This period of time permits enough disease progression for individuals to have had quantifiable changes in lung function, functional capability, and quality of life. Furthermore, the 3-year mark is a suitable window for studying the relationship between severity of the disease and outcomes because it is during this time that clinicians usually observe the early phases of disease stability or advancement.
Data analysis
Data analysis was performed using Jamovi 2.2.5 software. The Shapiro-Wilk test was used to determine normality of the variables. Based on normality assessment, mean, median, standard deviation (SD), interquartile range (IQR) were used to describe the findings. Spearman’s signed rank test was used to compute the correlation between 6MWD and DLCO % predicted and 6MWD and FVC % predicted. Chi square test was used to establish association between variables. Receiver Operating Characteristics (ROC) curve, specificity and sensitivity tests were used to test accuracy. We determined the strength of correlation on absolute values of r with a correlation defined as strong when r = 0.6 and above, moderate when r = 0.40–0.59 and weak when r = 0.2–0.3938 Statistical significance was defined as p < 0.05.
Results
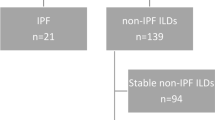
Eighty participants with ILD, mean (SD) age 59.5 (13) years, 41 males (51%), were recruited. (Fig. 1) Of the 80 participants, 39 (49%) were diagnosed as Idiopathic Pulmonary Fibrosis (IPF), 19 (24%) as Non-specific Interstitial Pneumonia (NSIP), 9 (11%) as sarcoidosis, 6 (8%) as Rheumatoid Arthritis associated Interstitial Lung Disease (RA-ILD), 7 (9%) as Connective Tissue Diseases associated Interstitial Lung Disease (CTD-ILD). Participant characteristics are shown in Table 1.
Diffusion capacity of the lungs for carbon monoxide % predicted (DLCO % pred)
The median DLCO % predicted values varied based on time since diagnosis, sex, and dyspnea severity. Participants diagnosed with ILD for less than 3 years had a median DLCO % predicted of 47 ml/min/mmHg (IQR: 30–64), compared to 44 ml/min/mmHg (IQR: 31–63) for those diagnosed for more than 3 years. Males exhibited a higher median DLCO % predicted (49 ml/min/mmHg; IQR: 30–64) than females (45 ml/min/mmHg; IQR: 31–62). Additionally, participants with mMRC Grade 2 dyspnea had a higher mean DLCO % predicted (60 ml/min/mmHg; IQR: 53–64) compared to those with Grade 3 dyspnea (44 ml/min/mmHg; IQR: 30–63), indicating a decline in pulmonary function with increasing dyspnea severity. (Table 2).
Forced vital capacity % predicted (FVC % pred)
Baseline median (IQR) FVC % predicted for participants with ILD diagnosed for less than 3 years was 75% predicted (41–111) and for those diagnosed for more 3 years was 73% predicted (44–110). The mean difference in FVC % predicted between participants diagnosed with ILD for ≤ 3 years and those diagnosed for > 3 years was 2%, with the associated 95% confidence interval (95% CI) indicating the precision of this estimate. Mean FVC% predicted for females was 75% predicted (41–110, p value = 0.138) and males was 71% predicted (42–111) with no difference between groups (p = 0.067). Mean FVC % predicted for participants who reported dyspnoea Grade 2 on mMRC was 80% predicted (42–110) and Grade 3 on mMRC was 71% predicted (41–111). (Table 2).
6-minute walk distance (6 MWD)
Baseline mean (SD) 6MWD for participants with ILD diagnosed for less than 3 years was 248.7 m (47.78), and for those diagnosed for more 3 years was 242.2 m (38.20), 6MWD for females was 247.7 m (57.6), and males was 287.7 m (32.6). 6MWD for participants who reported dyspnoea Grade 2 on mMRC was 289.3 m (20.16) and Grade 3 on mMRC was 238.1 m, (45.23). (Table 2)
St. George’s respiratory questionnaire (SGRQ)
Baseline median (IQR) SGRQ Total score for participants with ILD diagnosed for less than 3 years was 39 (20–53) and for those diagnosed for more than 3 years was 38.4 (20–54) with no difference between groups (p = 0.510). Mean (IQR) SGRQ Total score for females was 37 (20–54), and males was 40 (20–53) (p = 0.521). Mean (IQR) SGRQ Total score for participants who reported mMRC Grade 2 was 37 (20–53) and mMRC Grade 3 was 49 (41–54) with a significant between-group difference. (Table 2).
Table 3 demonstrates the correlations between functional exercise capacity measured by 6MWD and pulmonary function values of DLCO% predicted and FVC% predicted for all participants, and for participants with mMRC of Grades 2 and 3. For all participants, there was a strong correlation between 6MWD and DLCO% predicted (Spearman rho 0.89, p < 0.001). There was no correlation between 6MWD and FVC% predicted (Spearman rho 0.20, p = 0.07). There was a strong correlation between SGRQ Total score and DLCO% predicted (Spearman rho 0.90, p < 0.001). There was no correlation between SGRQ Total score and FVC % predicted (Spearman rho 0.11, p = 0.324). (Figure 2a,b)
(a) Correlation between baseline DLCO % predicted with 6 MWD. (b) Correlation between baseline DLCO % predicted with SGRQ. %pred percentage predicted, 6MWD 6 Minute Walk Test, B Baseline, DLCO Diffusing capacity of the Lungs for Carbon monoxide, mts meters, r Spearman rho value, SGRQ St. George respiratory questionnaire.
Receiver operating characteristics (ROC) curve analysis
We graded individuals walking less than 300 m of 6MWD as severe impairment, 300–500 m as moderate impairment and more than 500 m as mild impairment. Individuals who score lower than 300 on the 6MWT frequently have a worse prognosis and substantial functional capacity decline. Walking more than 500 m is typically linked to mild functional impairment, whereas the 300–500 m range is regarded as moderate, showing some exercise capacity limitation but not as severe. The cutoff values for categorizing 6-minute walk distance (6MWD) into severe (< 300 m), moderate (300–500 m), and mild (> 500 m) impairment were based on our clinical judgment and assumptions tailored specifically for ILD patients, considering their disease severity and pathology. Given the progressive nature of ILD and its impact on functional capacity, we adopted these cutoffs to reflect the varying degrees of exercise limitation observed in this patient group. These categories align with the general understanding that walking less than 300 m indicates significant functional impairment and a poorer prognosis, while distances above 500 m suggest milder limitations.
We graded DLCO levels using commonly recognized thresholds used in clinical practice to assess the severity of gas exchange impairment. DLCO values are often expressed as a % of the anticipated value based on age, gender, height, and ethnicity, using the following grading system based on ATS/ERS guidelines39:
-
Mild impairment: DLCO ≥ 60% of predicted.
-
Moderate impairment: DLCO 40–59% of predicted.
-
Severe impairment: DLCO < 40% of predicted.
A lower DLCO number indicates more severe disease and a worse prognosis. This grading system represents the degree of gas exchange impairment.
The ROC curve analysis shows that the area under the curve (AUC) was 0.92. Our results show that participants walking 300 m to 500 m are likely to have DLCO% predicted values between 40 − 60%. Participants walking more than 500 m are likely to have DLCO % predicted values between 60% to lower limit of normal. Majority of the participants (58.8%) walking less than 300 m are likely to have DLCO% predicted values between 40-60% and 28.7% are likely to have DLCO% predicted values less than 40%. (Table 4; Fig. 3).
We graded individuals scoring 0–20 on SGRQ as severe impairment, 21–40 as moderate impairment and more than 41–60 as mild impairment.
The ROC curve analysis showed that the area under the curve (AUC) for SGRQ grades versus DLCO grades was more than 1 (range 1.0 to 1.84). Our results state that SGRQ grade of 41–60 are likely to have DLCO values between 40 − 60%. SGRQ grade 21–40 are likely to have DLCO values 60% − 40% or less than 40%. SGRQ grade 0–20 are likely to have DLCO values from normal to 40%. (Table 5; Fig. 4).
Discussion
This is the first study to investigate the relationships between disease severity, measured by pulmonary function tests (DLCO% predicted and FVC% predicted) and dyspnea (using the mMRC scale), and health status parameters such as functional exercise capacity and HRQoL among people with ILD in India. This study found strong correlations between DLCO % predicted with both 6 MWD and SGRQ Total score whereas, there were no significant correlations between FVC% predicted with either 6 MWD and SGRQ Total score. Considering time since diagnosis, sex, and reported dyspnea, different patterns in pulmonary function and exercise capacity were identified among participants with ILD according to these characteristics. Individuals diagnosed for less than three years had a decline in DLCO % predicted values, but those diagnosed for more than three years had a slightly lower DLCO. Males consistently had higher DLCO % predicted and lower FVC% predicted compared to females. Dyspnea severity was associated with differences in pulmonary function, with those reporting higher mMRC grades (more dyspnea) often having lower DLCO % predicted and FVC% predicted values, suggesting that worsening dyspnea may correlate with greater physiological impairment in ILD. The sex disparity persisted in HRQoL assessments, with a focus on the influence of dyspnea severity on their overall wellbeing.
Survival for people with ILD in India is poor, with up to 46% mortality 4 years after diagnosis, indicating delayed diagnosis due to DLCO and high-resolution computed tomography (HRCT) not typically being performed due to access most likely owing to a lack of specialized diagnostic facilities and experience in many rural parts for the given population in India40,41,42 Predictors associated with worse survival include honeycombing of the lungs, current or past history of smoking, and past history of pulmonary tuberculosis41 Some of the factors which contribute to the delayed diagnosis are highlighted as lack of standardized care guidelines, lack of defined survival predictors, and high prevalence of pulmonary infections which may also contribute to the high mortality39.
Our study showed that a third of participants were past smokers. Tobacco smoking is a significant predictor of poor survival in patients with idiopathic pulmonary fibrosis (IPF)40,41 The lower smoking rates in our cohort (particularly among women) reflect regional sociocultural norms, where biomass fuel exposure often supersedes tobacco as an environmental risk factor for ILD. This aligns with findings from a study40,41 where biomass-associated ILD demonstrated distinct clinical features. In our cohort, [30%] of non-smokers reported prolonged biomass exposure, suggesting its potential role in disease pathogenesis. Other factors such as genetics, environmental exposures e.g. pollution etc., and the degree of lung fibrosis and honeycombing also play a role in the course of the disease42 Inability of patients to perform spirometry, a common test for lung function, is also associated with poor survival, likely because it indicates advanced disease42 Due to the expense and accessibility of advanced testing, studies conducted in India indicate that patients frequently place a higher priority on symptom management than on accurate diagnosis. Since symptoms like fatigue and dyspnea predominate their lived experience regardless of quantifiable disease progression by PFTs or HRCT, this could result in a mismatch between perceived disease severity and HRQoL. Reliance on more approachable instruments like the 6MWT or symptom-based evaluations may result from the lack of access to advanced diagnostic tests like DLCO and HRCT in many healthcare settings. Given that these alternative measurements may not accurately reflect severity of the disease in comparison to more advanced diagnostics, this could help to explain why the link between disease severity and HRQoL may differ across India.
Regardless of the fact that all patients with ILD experience progressive worsening of dyspnea, which has an influence on their overall quality of life,43 few studies have linked health status outcomes to physiological and radiological estimations of disease severity and extent, and none in an Indian population. The study by Martinez et al. (2000) found that chronic dyspnea is a significant contributor to poorer quality of life in patients with ILD, and that lung function variables such as FEV1 and FVC do not accurately reflect the impact of the disease on the patient’s health status9 with our study demonstrating similar findings. Contrary to other well-cited research, we found no significant relationship between FVC% predicted and HRQoL, which is consistent with Martinez et al. (2000). This disparity could be due to changes in cohort composition (e.g., ILD subtype distribution), the importance of non-spirometric variables (e.g., dyspnea, mental health comorbidities) in triggering HRQoL impairment, or differences in HRQoL evaluation methods. Disease-specific questionnaires may capture respiratory-specific limitations more sensitively than generic instruments, but severe disease stages may dissociate lung function from reported health status due to factors such as oxygen dependency or recurring exacerbations. Our findings demonstrate that HRQoL in ILD is a multicomponent outcome that requires a thorough evaluation that goes beyond spirometry. ILD is often classified into mild, moderate, and severe categories based on FVC% predicted, but this classification system has been criticized for its lack of correlation with patient outcomes44,45,46,47,48,49,50 In patients with idiopathic pulmonary fibrosis (IPF), a reduction in FVC% predicted of 5–10% following drug treatment is associated with worse survival outcomes, while an improvement change of 2–6% in FVC% predicted is considered the minimum clinically significant difference16.
Our study provided a thorough understanding of the relationships between pulmonary function, functional exercise capacity, and quality of life in ILD patients by classifying patients based on their time since diagnosis sex, and levels of dyspnea. Dyspnoea in ILD is likely related to the increased work of breathing due to the interstitial fibrosis which is reflected in low FVC% predicted and reduced DLCO51,52 Some studies suggest that baseline FVC % predicted can predict the risk of death independently, while others suggest that changes in clinical and physiological variables such as changes in dyspnea score and FVC over 6 and 12 months may provide more accurate prognostic information52,53 Customizing treatment techniques requires an understanding of the relationships between various factors such as exercise capacity, DLCO, baseline FVC% predicted, changes in dyspnea score, and other variables. As indicated in our study, changes in dyspnea score, DLCO, exercise capacity, and health-related quality of life are more than baseline FVC% predicted, enabling physiotherapists and clinicians to prioritize interventions primarily concentrated at relieving symptoms54.
The SGRQ is commonly used to assess HRQoL in people with IPF and is used as a key endpoint in some clinical trials50,16,55 A previous study found that patients with SGRQ Total scores higher than 30 points had a significantly higher mortality, with a hazard ratio of 2.04756,57 In our study the median SGRQ Total score was approximately 39 points, suggesting that our participants were at a high risk of mortality whether they were diagnosed less than or greater than 3 years previously. Previous studies have also demonstrated a correlation between the SGRQ scores and pulmonary function in people with ILD, showing the impact of reduced lung function on HRQoL58,59,60 Our study has added to this literature by demonstrating a strong correlation between functional exercise capacity measured by the 6MWD and DLCO, indicating that a decrease in diffusion capacity due to ILD directly impacts functional capacity.
There are some limitations to our study. It was a single-center study, and there may be selection bias. To confirm our findings, further large prospective studies are needed to investigate the relationship between disease severity variables and predictors of health status. Further longitudinal studies should investigate the relationship between these variables and mortality rates. Additionally, our study only included participants with mild to moderate disease severity based on DLCO values, and results may differ in more severe disease. The recruitment approach of including 80 participants in the study was intended to produce a representative sample of individuals with diverse disease severity and subtypes.
Conclusion
This is the first study that investigates the correlations between pulmonary function (DLCO % and FVC% predicted), dyspnea severity (mMRC scale), functional exercise capacity (6MWD), and HRQoL (SGRQ Total score) among individuals with ILD in India. DLCO % predicted showed strong correlations with 6MWD and SGRQ, while FVC% predicted did not. Our results indicate significant relationships between disease severity (measured by DLCO) and both functional exercise capacity (measured by 6MWD) and health-related quality of life (measured by the SGRQ) for participants with Grade 2 and Grade 3 dyspnoea. There were no relationships with disease severity measured by FVC% predicted and a strong positive relationship measured by DLCO % predicted. These findings suggest that DLCO is a more useful measure than FVC% predicted to determine the impact of ILD on the functional exercise capacity and HRQoL of people in living with this disease in India. Variations in lung function and exercise capacity were observed based on sex, dyspnea severity, and time since diagnosis, with males showing higher DLCO % and lower FVC%, and severe dyspnea associated with poorer outcomes. However, where there is limited availability of DLCO testing, other tests such as 6-minute walk test and questionnaires such as SGRQ may give an indication of disease severity and the impact of ILD on patients’ lives. These are particularly important findings if access to diagnostic equipment is unavailable.
Data availability
All the data collected for the research in question are not published in any other media or data dissemination tool, nor are they stored in specific repositories. However, upon request, the data may be made available at any time. To request access to the data, contact the corresponding author (email address: vaishali.kh@manipal.edu).
References
King, T. E. Jr Clinical advances in the diagnosis and therapy of the interstitial lung diseases. Am. J. Respir Crit. Care Med. 172 (3), 268–279. https://doi.org/10.1164/rccm.200503-483OE (2005).
Raghu, G. et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am. J. Respir. Crit. Care Med. (6), 788–824. https://doi.org/10.1164/rccm.2009-040GL (2011).
Holland, A. E. & Hill, C. Physical training for interstitial lung disease. Cochrane Database Syst. Rev. 4 https://doi.org/10.1002/14651858.CD006322.pub2 (2008).
Markovitz, G. H. & Cooper, C. B. Review series: rehabilitation in Non COPD: mechanisms of exercise limitation and pulmonary rehabilitation for patients with pulmonary fibrosis/restrictive lung disease. Chron. Resp. Dis. 7 (1), 47–60. https://doi.org/10.1177/1479972309348654 (2010).
King, T. E. Jr, Pardo, A. & Selman, M. Idiopathic pulmonary fibrosis. Lancet 378 (9807), 1949–1961. https://doi.org/10.1016/S0140-6736(11)60052-4 (2011).
Park, J. H. et al. Prognosis of fibrotic interstitial pneumonia: idiopathic versus collagen vascular disease–related subtypes. Am. J. Respir Crit. Care Med. 175 (7), 705–711. https://doi.org/10.1164/rccm.200607-912OC (2007).
Panos, R. J., Mortenson, R. L., Niccoli, S. A. & King, T. E. Jr Clinical deterioration in patients with idiopathic pulmonary fibrosis: causes and assessment. Am. J. Med. 88 (4), 396–404. https://doi.org/10.1016/0002-9343(90)90495-Y (1990).
Kumar, D. P. Assessment and follow-up of interstitial lung disease. Indian J. Rheumatol. 16 (Suppl 1), S69–78 (2021).
Ley, B., Collard, H. R. & King, T. E. Jr Clinical course and prediction of survival in idiopathic pulmonary fibrosis. Am. J. Respir Crit. Care Med. 183 (4), 431–440. https://doi.org/10.1164/rccm.201006-0894CI (2011).
Hutchinson, J. P., McKeever, T. M., Fogarty, A. W., Navaratnam, V. & Hubbard, R. B. Increasing global mortality from idiopathic pulmonary fibrosis in the twenty-first century. Ann. Am. Thorac. Soc. 11 (8), 1176–1185. https://doi.org/10.1513/AnnalsATS.201404-145OC (2014).
Lederer, D. J. & Martinez, F. J. Idiopathic pulmonary fibrosis. N Engl. J. Med. 378 (19), 1811–1823. https://doi.org/10.1056/NEJMra1705751 (2018).
Cottin, V. et al. Burden of idiopathic pulmonary fibrosis progression: a 5-year longitudinal follow-up study. PLoS One. 12 (1), e0166462. https://doi.org/10.1371/journal.pone.0166462 (2017).
Kolb, M. & Vašáková, M. The natural history of progressive fibrosing interstitial lung diseases. Respir Res. 20 (1), 57. https://doi.org/10.1186/s12931-019-1022-1 (2019).
Raghu, G. et al. Idiopathic pulmonary fibrosis (an update) and progressive pulmonary fibrosis in adults: an official ATS/ERS/JRS/ALAT clinical practice guideline. Am. J. Respir Crit. Care Med. 205 (9), e18–47. https://doi.org/10.1164/rccm.202202-0399ST (2022).
Richeldi, L. et al. Relative versus absolute change in forced vital capacity in idiopathic pulmonary fibrosis. Thorax 67 (5), 407–411. https://doi.org/10.1136/thoraxjnl-2011-201184 (2012).
Zappala, C. J. et al. Marginal decline in forced vital capacity is associated with a poor outcome in idiopathic pulmonary fibrosis. Eur. Respir J. 35 (4), 830–836. https://doi.org/10.1183/09031936.00155108 (2010).
Caminati, A., Bianchi, A., Cassandro, R., Mirenda, M. R. & Harari, S. Walking distance on 6-MWT is a prognostic factor in idiopathic pulmonary fibrosis. Respir Med. 103 (1), 117–123. https://doi.org/10.1016/j.rmed.2008.07.022 (2009).
Panagiotou, M., Polychronopoulos, V. & Strange, C. Respiratory and lower limb muscle function in interstitial lung disease. Chron. Resp. Dis. 13 (2), 162–172. https://doi.org/10.1177/1479972315626014 (2016).
Camcioglu, B. et al. Respiratory and peripheral muscle strength, functional exercise capacity, dyspnea, fatigue and physical activity in patients with interstitial lung disease. Eur. Respir. J. 44 (Suppl 58) (2014).
De Vries, J. & Drent, M. Quality of life and health status in interstitial lung diseases. Curr. Opin. Pulm Med. 12 (5), 354–358. https://doi.org/10.1097/01.mcp.0000239553.93443.d8 (2006).
Mavroudi, M. et al. Sleep disorders and health-related quality of life in patients with interstitial lung disease. Sleep. Breath. 22, 393–400. https://doi.org/10.1007/s11325-017-1579-1 (2018).
Khanna, D. et al. Correlation of the degree of dyspnea with health-related quality of life, functional abilities, and diffusing capacity for carbon monoxide in patients with systemic sclerosis and active alveolitis: results from the scleroderma lung study. Arthritis Rheum. 52 (2), 592–600. https://doi.org/10.1002/art.20787 (2005).
Holland, A. E., Hill, C. J., Glaspole, I., Goh, N. & McDonald, C. F. Predictors of benefit following pulmonary rehabilitation for interstitial lung disease. Respir Med. 106 (3), 429–435. https://doi.org/10.1016/j.rmed.2011.11.014 (2012).
Olson, A. L., Brown, K. K. & Swigris, J. J. Understanding and optimizing health-related quality of life and physical functional capacity in idiopathic pulmonary fibrosis. Patient Relat. Outcome Meas. 29–35. https://doi.org/10.2147/PROM.S74857 (2016).
Villalba, W. O. et al. Six-minute walk test for the evaluation of pulmonary disease severity in scleroderma patients. Chest 131 (1), 217–222. https://doi.org/10.1378/chest.06-0630 (2007).
Singh, S. et al. Interstitial lung disease in India. Results of a prospective registry. Am. J. Respir Crit. Care Med. 195 (6), 801–813. https://doi.org/10.1164/rccm.201607-1484OC (2017).
Sen, T. & Udwadia, Z. F. Retrospective study of interstitial lung disease in a tertiary care centre in India. Indian J. Chest Dis. Allied Sci. 52 (4), 207 (2010).
Dhooria, S. et al. Incidence, prevalence, and National burden of interstitial lung diseases in India: estimates from two studies of 3089 subjects. PLoS One. 17 (7), e0271665. https://doi.org/10.1371/journal.pone.0271665 (2022).
Raghu, G. & Mehta, S. Interstitial lung disease (ILD) in India: insights and lessons from the prospective, landmark ILD-India registry. Lung India. 33 (6), 589. https://doi.org/10.4103/0970-2113.192874 (2016).
Sneider, M. B. & Kershaw, C. D. The importance of imaging in the assessment of interstitial lung diseases. J. Thorac. Imaging. 38, S2–6 (2023).
Nathan, S. D. et al. HRCT evaluation of patients with interstitial lung disease: comparison of the 2018 and 2011 diagnostic guidelines. Ther. Adv. Respir Dis. 14, 1753466620968496 (2020).
Amin, R. et al. Effect of a home-based pulmonary rehabilitation program on functional capacity and health-related quality of life in people with interstitial lung disease–A randomized controlled trial protocol. Respir Med. 201, 106927. https://doi.org/10.1016/j.rmed.2022.106927 (2022).
Al-Ashkar, F., Mehra, R. & Mazzone, P. J. Interpreting pulmonary function tests: recognize the pattern, and the diagnosis will follow. Cleve Clin. J. Med. 70 (10), 866–881 (2003).
Modi, P. & Cascella, M. Diffusing capacity of the lungs for carbon monoxide.
Casanova, C. et al. The 6-min walk distance in healthy subjects: reference standards from seven countries. Eur. Respir J. 37 (1), 150–156 (2011).
Pedro, P. I. et al. Benefits of pulmonary rehabilitation in patients with chronic obstructive pulmonary disease and interstitial lung disease with the same dyspnea severity. Pulmonology 25 (2), 117–118 (2019).
Chang, J. A., Curtis, J. R., Patrick, D. L. & Raghu, G. Assessment of health-related quality of life in patients with interstitial lung disease. Chest 116 (5), 1175–1182 (1999).
Campbell, M. J. & Swinscow, T. D. V. Statistics at Square One 11 edn (eds Chichester) (Wiley-Blackwell/BMJ Books, 2009).
Leung, S. K. et al. American thoracic society/European respiratory society 2005 standardization of DLCO measurement: impact on performance. Respirol 13 (5), 728–730 (2008).
Singh, S. et al. Survival predictors of interstitial lung disease in India: follow-up of interstitial lung disease India registry. Lung India. 38 (1), 5 (2021).
Singh, S. & Singh, N. Current trends of management of respiratory diseases by pulmonologists: results of National conference of pulmonary Disease-2015 survey. Lung India. 34 (1), 13. https://doi.org/10.4103/0970-2113.197093 (2017).
Alsumrain, M. et al. Combined pulmonary fibrosis and emphysema as a clinicoradiologic entity: characterization of presenting lung fibrosis and implications for survival. Respir Med. 146, 106–112. https://doi.org/10.1016/j.rmed.2018.12.003 (2019).
Jacob, J. et al. Functional and prognostic effects when emphysema complicates idiopathic pulmonary fibrosis. Eur. Respir J. 50 (1). https://doi.org/10.1183/13993003.00379-2017 (2017).
American Thoracic Society. Idiopathic pulmonary fibrosis: diagnosis and treatment: international consensus statement. Am. J. Respir Crit. Care Med. 161, 646–664 (2000).
Martinez, T. Y. et al. Evaluation of the short-form 36-item questionnaire to measure health-related quality of life in patients with idiopathic pulmonary fibrosis. Chest 117 (6), 1627–1632. https://doi.org/10.1378/chest.117.6.1627 (2000).
Noble, P. W. et al. Pirfenidone in patients with idiopathic pulmonary fibrosis (CAPACITY): two randomised trials. Lancet 377 (9779), 1760–1769. https://doi.org/10.1016/S0140-6736(11)60405-4 (2011).
King, T. E. Jr et al. BUILD-1: a randomized placebo-controlled trial of Bosentan in idiopathic pulmonary fibrosis. Am. J. Respir Crit. Care Med. 177 (1), 75–81. https://doi.org/10.1164/rccm.200705-732OC (2008).
King, T. E. Jr et al. BUILD-3: a randomized, controlled trial of Bosentan in idiopathic pulmonary fibrosis. Am. J. Respir Crit. Care Med. 184 (1), 92–99. https://doi.org/10.1164/rccm.201011-1874OC (2011).
Idiopathic Pulmonary Fibrosis Clinical Research Network. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl. J. Med. 366 (21), 1968–1977 (2012).
Egan, J. J., Martinez, F. J., Wells, A. U. & Williams, T. Lung function estimates in idiopathic pulmonary fibrosis: the potential for a simple classification. Thorax 60 (4), 270–273. https://doi.org/10.1136/thx.2004.035436 (2005).
Collard, H. R. et al. Changes in clinical and physiologic variables predict survival in idiopathic pulmonary fibrosis. Am. J. Respir Crit. Care Med. 168 (5), 538–542. https://doi.org/10.1164/rccm.200211-1311OC (2003).
Hanada, M. et al. Aerobic and breathing exercises improve dyspnea, exercise capacity and quality of life in idiopathic pulmonary fibrosis patients: systematic review and meta-analysis. J. Thorac. Dis. 12 (3), 1041 (2020).
Richeldi, L. et al. Efficacy of a tyrosine kinase inhibitor in idiopathic pulmonary fibrosis. N Engl. J. Med. 365 (12), 1079–1087. https://doi.org/10.1056/NEJMoa1103690 (2011).
Richeldi, L. et al. INPULSIS trial investigators. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl. J. Med. 370 (22), 2071–2082. https://doi.org/10.1056/NEJMoa1402584 (2014).
Xaubet, A. et al. Pulmonary function tests and CT scan in the management of idiopathic pulmonary fibrosis. Am. J. Respir Crit. Care Med. 158 (2), 431–436. https://doi.org/10.1164/ajrccm.158.2.9709008 (1998).
Horton, M. R. et al. Thalidomide for the treatment of cough in idiopathic pulmonary fibrosis: a randomized trial. Ann. Intern. Med. 157 (6), 398–406. https://doi.org/10.7326/0003-4819-157-6-201209180-00003 (2012).
Furukawa, T. et al. The St. George’s respiratory questionnaire as a prognostic factor in IPF. Respir Res. 18 (1), 1–6. https://doi.org/10.1186/s12931-017-0503-3 (2017).
Beretta, L., Santaniello, A., Lemos, A., Masciocchi, M. & Scorza, R. Validity of the saint George’s respiratory questionnaire in the evaluation of the health-related quality of life in patients with interstitial lung disease secondary to systemic sclerosis. Rheumatology 46 (2), 296–301 (2007).
Berry, C. E. et al. Relationship between lung function impairment and health-related quality of life in COPD and interstitial lung disease. Chest 142 (3), 704–711 (2012).
LoRusso, T. J., Belman, M. J., Elashoff, J. D. & Koerner, S. K. Prediction of maximal exercise capacity in obstructive and restrictive pulmonary disease. Chest 104 (6), 1748–1754 (1993).
Acknowledgements
We would like to thank the Indian Council of Medical Research (ICMR), New Delhi for assistance in in the execution of the study (Grant number: 5/8-4/19/Env/2020-NCD-II).
Funding
Open access funding provided by Manipal Academy of Higher Education, Manipal.
Author information
Authors and Affiliations
Contributions
Conceptualization: K. V., Patient recruitment and assessment: K. V., R. A., Data analysis and interpretation of findings: K. V., R. A., Writing the original manuscript: K. V., R. A., Review and editing the manuscript: G. A. M., A. K. M., V. A., M. T. D. and J. A. A.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Amin, R., Vaishali, K., Maiya, G.A. et al. Relationships between disease severity and measures of health status in people with interstitial lung disease in India: an observational study. Sci Rep 15, 16985 (2025). https://doi.org/10.1038/s41598-025-01877-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01877-4