Abstract
With the increasing prevalence of hypertension, studying the relationship between hypertension and metabolism-related diseases has become particularly important. However, no research has yet investigated the association between metabolic scores in hypertensive patients and cardiometabolic multimorbidity. This article explores the relationship between the Metabolic Score for Visceral Fat (METS-VF), the Metabolic Score for Insulin Resistance (METS-IR), the Cardiometabolic Index (CMI), and the risk of Cardiometabolic Multimorbidity (CMM) in hypertensive patients, providing a theoretical basis for their health management. Using cluster random sampling, 16,303 workers aged 18 to 70 with a working duration of ≥ 1 year from 6 oilfield bases in Karamay City were selected to collect general data. The relationship between metabolic scores and the risk of CMM in hypertensive patients was analyzed using a Logistic regression model combined with restricted cubic spline curves, and further subgroup interaction analysis was conducted to identify potential influencing factors. In addition, the predictive value for CMM was assessed using covariate-adjusted receiver operating characteristic (ROC)curves.Finally, three sensitivity analyses were performed. (1) The study included a total of 16,303 patients with hypertension, among whom 5,988 had CMM, with a prevalence rate of 36.7%. Compared to the non-CMM group, the CMM group showed statistically significant differences in gender, age, smoking, alcohol consumption, BMI, waist circumference, FPG, TC, TG, LDL-C, UA, BUN, ALT, AST, and HDL levels (all P < 0.05). (2) Logistic regression and dose-response relationship: After controlling for confounding factors, the results showed that higher METS-VF, METS-IR, and CMI were all risk factors for CMM, with odds ratios of 3.11 (95% CI: 2.78 ~ 3.49), 7.89 (95% CI: 6.76 ~ 9.22), and 11.51 (95% CI: 9.97 ~ 13.29), respectively (all P for trend < 0.05). Notably, there was a non-linear dose-response relationship between METS-VF, METS-IR, CMI, and the risk of CMM (all P for non-linearity < 0.001). (3) The subgroup interaction analysis results showed a consistent relationship between the three metabolic scores and CMM patients with different stratification variables. It was also found that there were interactions between these three scores and gender, age, smoking, alcohol consumption, and BMI. (4) The adjusted ROC curve results showed that the AUCs for METS-VF, METS-IR, and CMI were 0.803, 0.840, and 0.821, respectively (all P < 0.05), indicating that these indices have good predictive value in identifying the risk of cardiometabolic comorbidities. METS-VF, METS-IR, and CMI exhibit complex interactions with the prevalence of CMM in hypertensive patients, leading to an increased risk of CMM and demonstrating good predictive ability for cardiometabolic comorbidities, which suggests their potential utility in the early prevention and intervention of cardiometabolic comorbidities.
Similar content being viewed by others
Introduction
Co-morbidities are becoming one of the global public health problems with the changing global demographics and increasing disease burden1. Cardiometabolic multimorbidity (CMM), which refers to the coexistence of two or more cardiometabolic diseases, including hypertension, coronary heart disease, stroke, and diabetes, is one of the most common and severe forms of multimorbidity2–3. As the prevalence of hypertension continues to rise4–5, studying the relationship between hypertension and metabolism-related diseases has become particularly important. Hypertension is not only an independent risk factor for cardiovascular diseases6, but also frequently coexists with metabolic abnormalities such as insulin resistance, obesity, hyperglycemia, and dyslipidemia7–8. These metabolic abnormalities collectively increase the risk of cardiovascular diseases. In recent years, studies have shown that insulin resistance (IR) is closely related to the pathophysiological processes of the occurrence and development of hypertension9. However, the assessment of IR is cumbersome, with poor patient compliance and limited measurement accuracy. Numerous studies have confirmed that METS-IR and METS-VF are reliable indicators of insulin resistance10,11,12. CMI is closely associated with metabolic-associated fatty liver disease, atherosclerosis, type 2 diabetes, and other cardiovascular diseases13,14. These indicators are comprehensive metrics that can be derived through simple routine biochemical calculations, addressing the shortcomings of traditional methods for assessing insulin resistance. They aid in identifying individuals with metabolic abnormalities, not only evaluating the quality of adipose tissue but also reflecting its dysfunction.
However, oil workers constitute a unique occupational group. Due to the fact that oil operations are predominantly located in Gobi desert areas, far from urban centers, and operate on a shift system, the prevalence of unhealthy behaviors such as alcohol consumption and smoking is notably high15,16,17, leading to a significant increase in the prevalence of hypertension18. Identifying reliable biomarkers can aid in better predicting CMM, assessing treatment efficacy, and formulating new prevention and treatment strategies. By evaluating the metabolic scores of hypertensive patients, healthcare professionals can more effectively identify patients at high risk of cardiometabolic comorbidities, thereby enabling the development of personalized intervention and treatment plans to reduce the incidence of cardiovascular events and improve the overall health status of patients. We believe that METS-VF, METS-IR, and CMI may be associated with the risk of CMM in hypertensive patients and may have certain predictive value for the risk of CMM in hypertensive patients, but the specific correlations and strengths need further verification. To our knowledge, there have been no studies reported so far that evaluate the associations of METS-VF, METS-IR, and CMI with the risk of CMM in hypertensive patients. Therefore, this study aims to assess the relationships between these metabolic scores and the risk of developing CMM in hypertensive patients.
Materials & methods
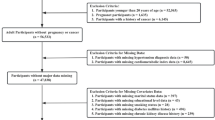
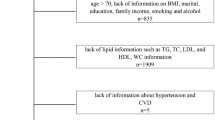
Study Subjects. Using whole cluster random sampling method, a total of 16,303 workers aged 18–70 years old who participated in health checkups were randomly selected from 4 districts in Kelamayi City, Xinjiang, with operating units as clusters and 6 oilfield enterprises and service units. Inclusion criteria: (1) aged 18–70 years with ≥ 1 year of service (2) blood pressure ≥ 140/90 mmHg, or those who have been diagnosed and treated for hypertension (3) complete physical examination data related to this study. Exclusion criteria: (1) patients with severe organic lesions, psychiatric disorders, and genetic disorders; (2) those with a history of liver disease (hepatitis, cirrhosis, and hepatocellular carcinoma); and (3) those with incomplete physical examination data. The study was approved by the Ethics Review Committee of the First Affiliated Hospital of Xinjiang Medical University (Ethics No. XJYKDXR20230303026), with adherence to the Declaration of Helsinki’s ethical guidelines. All participants provided signed informed consent.
Methods
data collection.The staff of the Physical Examination Department at Karamay Central Hospital collected data on general information and physical examinations. General information primarily included age, gender, alcohol consumption, smoking, and medical history. Smoking19 was defined as an average of ≥ 1 cigarette per day for more than six months. Alcohol consumption20 was defined as an average of ≥ 1 time per week, ≥ 50 g per time, for more than six consecutive months. Physical examination data mainly included measurements of height, weight, waist circumference, blood pressure, blood glucose, and blood lipids. Height and weight were measured without shoes at a standard position using an automatic recorder (RGZ-120). After the examinee rested for five minutes, blood pressure was measured in a seated arm position using an Omron (HEM-7211) electronic blood pressure monitor, with the average of three measurements taken as the blood pressure value. The research subjects did not eat or drink water after 10 pm the night before, and before 9 am, 4 ml of peripheral venous blood was collected by a professional occupational disease doctor and analyzed using a fully automated biochemical analyzer (Beckman Coulter AU5800) to detect Triglycerides (TG), Total cholesterol (TC), High-density lipoprotein cholesterol (HDL-C), Low-density lipoprotein cholesterol (LDL-C), and Fasting plasma glucose (FPG).
quality control. (1) Personnel Training and Instrument Calibration: The staff of the Physical Examination Department at Karamay Central Hospital collected the data. All personnel involved in data collection received standardized training on physical measurement methods, instrument operation procedures, etc.All physical examination equipment (such as height and weight measuring instruments, blood pressure monitors, biochemical analyzers, etc.) was calibrated according to standard procedures before use to ensure the consistency and accuracy of data collection. (2) Data Validation: Preliminary validation of the collected data was conducted to ensure its completeness and accuracy. For example, checking whether numerical variables such as age and blood pressure were within reasonable ranges. (3) Data Cleaning: The data is cleaned by removing duplicate records and erroneous data. For a small amount of completely random missing data, we employ the Complete Case Analysis method.
Diagnostic Criteria and Definitions.Cardiometabolic Multimorbidity is usually considered as the coexistence of two or more cardiometabolic diseases. However, in this study, CMM was defined as the occurrence of ≥ 1 of the following diseases in hypertensive patients: coronary heart disease (myocardial infarction or angina), stroke (ischemic stroke, cerebral hemorrhage, or subarachnoid hemorrhage), diabetes mellitus, and dyslipidemia.
①Metabolic Insulin Resistance Score(METS-IR)10=(Ln[(2*FPG) + TG])*BMI)/(Ln[HDL])
②Visceral fat metabolic score(METS-VF)11=4.466 + 0.011*[(Ln(METS-IR))3] + 3.239*.
[(Ln(WHTR))3+0.319(Gender) + 0.594*(Ln(age))]{male = 1,female = 0}.
③ Cardiometabolic index (CMI) 13= [TG (mmol L-1 )/HDL-C(mmol L-1 )]×WtHR.
Statistical analysis. Use SPSS 27.0 software and R4.3.2 software to analyze and process the data. Data that follows a normal distribution are represented as mean ± standard deviation, and t-test is used for comparison between two groups; Non normally distributed data are represented by M (P25, P75) and Mann Whitney U test is used. Count data is described as percentages and analyzed for inter group differences using chi square test. In order to clearly distinguish the association between METS-IR, METS-VF, and CMI indices and cardiac metabolic comorbidities, we grouped them according to quartiles and used univariate and multivariate logistic regression models combined with restricted cubic spline curves to analyze the relationship between various metabolic scores and the risk of CMM in hypertensive patients. The study indicators were grouped according to the median, and further subgroup interaction analysis was conducted to identify potential influencing factors. And two sensitivity analyses were conducted to further evaluate the robustness of the association. Firstly, we use Propensity Score Matching (PSM) method and 1:1 nearest neighbor matching method for matching, and re run logistic regression analysis to control for potential confounding factors. Secondly, we incorporated metabolic score as a continuous variable into the model to determine whether the association between its specific value and cardiac metabolic comorbidities still has statistical significance, in order to exclude human information loss caused by classification. In the third sensitivity analysis, as age is a significant risk factor for cardiovascular metabolic diseases, we excluded any participants over the age of 50. In addition, the receiver operating characteristic (ROC) curve adjusted for covariates was used to evaluate its predictive value for CMM. Test level α = 0.05.
Results
Cardiometabolic Multimorbidity in oil workers and basic demographic characteristics.The study included a total of 16,303 patients with hypertension, among whom 5,988 had CMM, representing a prevalence rate of 36.7%. Compared to the non-CMM group, the CMM group showed statistically significant differences in gender, Age, Smoking, Alcohol consumption, BMI, WC, FPG, TC, TG, LDL-C, UA, BUN, ALT, AST, and HDL levels (all P < 0.05). (Table 1).
Correlation and dose-response relationship between metabolic score and risk of Cardiometabolic Multimorbidity in hypertensive patients.To ensure the reliability and stability of the results, three models were developed. After model 3 was corrected for confounders, the results showed that the Q4 group (OR = 3.11, 95% CI: 2.78 ~ 3.49) increased the risk of developing CMM compared to the Q1 group of the METS-VF (P < 0.05), the Q4 group (OR = 7.89, 95% CI: 6.76 ~ 9.22) compared to the Q1 group of the METS-IR, the Q1 group of the CMI group compared to Q4 group of CMI (OR = 11.51, 95% CI: 9.97 ~ 13.29) were risk factors for the development of CMM (all P for trend < 0.05). Table 2. results of the restricted cubic spline regression model showed a nonlinear dose-response relationship between METS-IR and METS-VF and CMI and the risk of developing CMM; hypertensive patients were more likely to develop CMM at METS-VF, METS-IR, and CMI levels of 6.62, 43.33, and 2.51, respectively (OR = 3.47, 95%CI:2.98 ~ 4.06), (OR = 1.14, 95% CI:1.13 ~ 1.15),and (OR = 4.12,95%CI:3.87 ~ 4.40).(P for overall trend < 0.001, P for nonlinearity < 0.001). Figure 1.
Subgroup interaction analysis of the relationship between metabolic scores and Cardiometabolic Multimorbidity in hypertensive patients.Stratified analyses were used to explore the correlation between study indicators and CMM risk in different subgroups. We performed subgroup analyses of the correlations between study indicators and CMM, and when analyzing the correlation between an indicator and CMM, we did not include the indicator used to calculate the index as a stratified variable in the model. The results showed that the logistic regression model developed in this study was stable, and it can be assumed that the relationship between different metabolic score levels and CMM was not affected by stratification. (Fig. 2). The interaction results showed that there was a multiplicative interaction, antagonistic, between METS-VF and alcohol consumption; multiplicative interactions between METS-IR and CMI and gender, age and alcohol consumption, respectively; additive interactions between METS-IR and smoking; and additive interactions were found between CMI and gender and BMI.(Additional file: Table S1-S3). These findings suggest complex interactions between different metabolic scores and CMM that lead to an increased risk of CMM and emphasize the importance of addressing these factors in preventive health strategies.
ROC curve analysis of different metabolic scores to predict the risk of cardiometabolic multimorbidity in hypertensive patients.Adjusted ROC curve analysis showed that CMI had the highest AUC, followed by METS-IR and METS-VF (Fig. 3).CMI had the highest sensitivity (76.4%), whereas METS-VF had the highest specificity (80.8%). suggesting the importance of these metrics in identifying the risk of cardiometabolic multimorbidity.
sensitivity analysis.To verify the robustness of the findings, we performed three sensitivity analyses, reran the logistic regression model analysis with model 1 not controlling for any confounders and model 2 controlling for relevant confounders, and analyzed the correlation of a given index with the CMM with the index used to calculate that index excluded from being included as a covariate in the model adjustment. In the first sensitivity analysis, we matched baseline characteristics of hypertensive patients, using a propensity score matching method. The results showed no significant changes in the associations between METS-VF, METS-IR, CMI, and Cardiometabolic Multimorbidity, and after adjusting for confounders, the results showed an OR (95% CI) of 2.34 (2.01 ~ 2.71), 7.00 (5.74 ~ 8.53), and 8.30 (6.87 ~ 10.04) for the Q4 group, respectively, compared with the Q1 group. In addition, we performed a second sensitivity analysis with metabolic score as a continuous variable. The results showed that elevated metabolic score was associated with an increased risk of Cardiometabolic Multimorbidity with OR (95% CI) of 3.10 (2.79 ~ 3.44), 1.10 (1.10 ~ 1.12), and 1.26 (1.24 ~ 1.29), respectively. In the third sensitivity analysis, we also excluded any participants older than 50 years. The results after adjusting for confounders showed that the OR (95% CI) was 3.67 (3.00 ~ 4.48), 14.24 (11.25 ~ 18.03), and 35.98 (27.77 ~ 46.61), respectively, in group Q4 compared with group Q1, which revealed a significantly higher risk of CMM development in hypertensive patients younger than 50 years old compared with overall hypertensive patients, and also verified the robustness of the study findings. (Additional file: Table S4-S6).
Discussion
The findings of this study indicate that in the hypertensive population, higher levels of METS-IR, METS-VF, and CMI are associated with an increased risk of CMM. This relationship is particularly pronounced among male hypertensive patients. Our research not only validates the association between different metabolic scores and an elevated risk of CMM but also further reveals that METS-IR, METS-VF, and CMI have good predictive value for CMM. Notably, although previous studies have shown that cardiometabolic diseases are more common in the elderly population, our sensitivity analysis results indicate that even after excluding individuals over 50 years old, higher metabolic scores are still associated with an increased risk of CMM in hypertensive patients. The subgroup analysis revealed interactions between the three metabolic scores and gender, age, smoking, alcohol consumption, and BMI. Another significant finding was the nonlinear dose-response relationship between METS-VF, METS-IR, CMI, and the risk of CMM. These findings are consistent with previous research. The study by Cai21 demonstrated that the Cardiometabolic Index (CMI) was significantly associated with the risk of CMM in hypertensive patients. The study by Yang et al.22 also found that the Visceral Adiposity Metabolic Score (METS-VF) holds significant value in predicting future diabetes risk. Moreover, the study by Zhang et al.23 further substantiated the relationship between the metabolic score and the risk of CMM, highlighting the potential application value of the metabolic score in predicting CMM risk, indicating a close correlation between the metabolic score and CMM risk.
Cardiometabolic multimorbidity (CMM) is an increasingly concerning health issue24,25, particularly among the hypertensive population, as hypertension is the most common component of CMM26. Over 50% of hypertensive patients concurrently suffer from other cardiometabolic diseases such as diabetes and coronary heart disease27. A longitudinal cohort study involving millions of Chinese adults has shown that cardiometabolic multimorbidity significantly increases the risk of mortality28. Previous studies have indicated that hypertensive patients often exhibit higher metabolic scores29,30,31, and such metabolic abnormalities further elevate their risk of developing cardiometabolic multimorbidity32. The increased risk of comorbidity may stem from multiple mechanisms, including vascular dysfunction, oxidative stress, inflammatory responses, and lipid metabolism disorders33. In medical research and clinical practice, the presence of comorbidities has significant implications for patient diagnosis, treatment, and prognosis. Therefore, we included patients with hypertension as our study subjects to analyze the relationship between different metabolic scores and the risk of cardiometabolic comorbidities in hypertensive patients. The study results showed that the overall prevalence of CMM among hypertensive oil workers was 36.7%, higher than the 11.2% CMM prevalence reported in the study by Zheng Y et al.34 This discrepancy may be related to occupational specificity, regional environment, and differences in survey years. Shift work can disrupt circadian rhythms, affect dietary habits and sleep patterns, and consequently impact metabolic parameters35.Meanwhile, petroleum workers are often exposed to higher environmental pressures, which may lead to increased levels of psychological stress36, subsequently affecting metabolic status. Studies have shown37 that elevated stress levels are positively correlated with multiple components of metabolic syndrome, such as waist circumference, fasting blood glucose, and triglycerides. Additionally, the level of physical activity among petroleum workers may be influenced by the nature of their work. Although shift work does not significantly impact overall physical exercise, reduced physical activity during off-duty hours may affect metabolic health38. Moreover, the dietary habits in the Xinjiang region, characterized by high salt and fat intake and low consumption of fruits and vegetables, may further synergize with occupational factors to increase metabolic risks. In this study, the prevalence of CMM among women was 9.7%, lower than the 33.1% reported by Zhao Y et al.39 in their survey on the prevalence of cardiometabolic multimorbidity among Chinese women. The prevalence of CMM among men reached 34.3%, significantly higher than the 15.6% reported by Cheng et al.26 Trends in the Prevalence of Cardiometabolic Multimorbidity in the United States, 1999–2018. in their survey of the general male population in the United States. This discrepancy may be attributed to the predominance of male petroleum workers in this study (with males accounting for 86.69% of the study population), as men are more susceptible to accelerating cardiovascular pathologies by promoting insulin resistance and inflammatory responses, and thus typically exhibit higher visceral fat accumulation and cardiovascular risk40.
Furthermore, this study revealed significant multiplicative interactions between METS-VF, METS-IR, and CMI with alcohol consumption, and an antagonistic effect was observed between METS-VF and alcohol consumption. This phenomenon may be related to the complex regulatory effects of alcohol on lipid metabolism. The study by García-Villafranca et al.41 suggested that alcohol can inhibit AMPK-mediated lipolysis on one hand, and promote lipogenesis on the other. The research by Li Yuanyuan et al.42 indicated that alcohol has a dual regulatory role in lipid metabolism, promoting both triglyceride synthesis and fatty acid oxidation. This bidirectional regulatory effect may partially explain the antagonistic interaction observed between metabolic indicators and alcohol consumption in this study. METS-IR and CMI exhibited multiplicative interactions with gender and age, which may be related to Gender differences in hormonal regulation, fat distribution, and metabolic characteristics26. Males have higher levels of androgens, predisposing them to abdominal fat accumulation, whereas females benefit from the cardioprotective effects of estrogen before menopause. METS-IR showed an additive interaction with smoking. Smoking43, as a known risk factor for CMM, increases the risk of CMM through multiple pathways, including vascular endothelial damage, promotion of inflammatory responses, and disruption of lipid metabolism. As an indicator reflecting metabolism, the additive interaction between METS-IR and smoking suggests that elevated METS-IR levels further increase the risk of CMM in the smoking population.Similarly, the additive interaction between CMI and gender as well as BMI also suggests a similar risk accumulation effect. The age factor also exhibits a similar interaction, as the metabolic function of the human body gradually declines with age, and the relationship between metabolic scores and the risk of CMM may change with age. This finding is of significant importance for identifying high-risk populations and formulating targeted prevention strategies, indicating that these interaction factors should be comprehensively considered in clinical practice to more accurately assess an individual’s risk of CMM. CMI demonstrated the best performance in identifying CMM risk, with its higher AUC value and sensitivity (76.4%) being crucial for early screening and diagnosis of CMM, as early detection and intervention can effectively improve patient prognosis and reduce the incidence of complications. Although METS-IR and METS-VF showed better performance in AUC and specificity, they were slightly inferior to CMI in terms of sensitivity. Overall, the ROC curve analysis results of these indicators support our findings from the aforementioned interaction analysis: different metabolic scores play a significant role in identifying CMM risk, but their effects may be influenced by various subgroup factors such as gender, age, etc. Therefore, in clinical practice, it is necessary to combine multiple metabolic scoring indicators and clinical information for comprehensive evaluation to improve the accuracy of identifying CMM risk.
To the best of our knowledge, research on CMM is currently limited, although some have noted that dyslipidemia44, overweight, etc.45 are significantly associated with a gradually increasing risk of cardiometabolic multimorbidity. However, there is no research on the correlation between metabolic scores in hypertensive patients and the risk of CMM. Nevertheless, hyperlipidemia, hyperglycemia, and obesity are important and modifiable risk factors for hypertensive patients. By integrating these metabolic indicators to more accurately assess the risk of CMM, it can help better evaluate the risk of its onset and formulate new preventive strategies.
This study also has certain limitations. Firstly, it is a cross-sectional study that can only reflect the disease and exposure status of individuals at the time of the survey, and cannot determine causal relationships. Secondly, the sample of this study is from a single-center sample of occupational populations in Xinjiang, and its extrapolation has certain limitations. Thirdly, CMM was measured through self-reported chronic diseases, and thus may be underestimated or overestimated in this study. Future large-sample longitudinal epidemiological studies are still needed for different regions and populations. Therefore, prospective cohort studies will be conducted in the future to test etiological hypotheses, further verify the association between metabolic scores and CMM in hypertensive patients, and provide a scientific basis for early identification of high-risk CMM populations and the formulation of corresponding effective personalized prevention and intervention strategies.
Conclusions
In summary, this study reveals significant associations between METS-IR, METS-VF, and CMI with the risk of CMM in hypertensive oil workers, with a nonlinear dose-response relationship observed between these factors and CMM. Subgroup interaction analysis further indicates that these associations not only vary between genders but are also significantly influenced by age, BMI, and lifestyle factors such as alcohol consumption and smoking. This underscores the importance of individualized metabolic assessment for hypertensive patients in clinical practice, and the development of targeted strategies for the prevention and control of CMM to reduce the risk of CMM occurrence.
Data availability
Due to the data are not public but are available from the corresponding author on reasonable request.
References
World Health Organization. Ageing and health. (2024). https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
Xie, H. et al. Association between healthy lifestyle and the occurrence of cardiometabolic Multimorbidity in hypertensive patients: a prospective cohort study of UK biobank. Cardiovasc. Diabetol. 21, 199 (2022).
Sun, X., Li, X. & Editorial Aging and chronic disease: public health challenge and education reform. Front. Public. Health. 11, 1175898 (2023).
Zhang, M. et al. Prevalence, awareness, treatment, and control of hypertension in China, 2004-18: findings from six rounds of a National survey. BMJ 380, e071952 (2023).
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet Lond. Engl. 398, 957–980 (2021).
Li, Z. et al. Five-year changes in cardiovascular risk factors and treatment strategies among elderly community-dwelling adults in Shibei district. Qingdao Chin. J. Geriatr. Heart Brain Vessels. 25, 151–155 (2023).
Bloomgarden, Z. T. Insulin resistance, dyslipidemia, and cardiovascular disease. Diabetes Care. 30, 2164–2170 (2007).
Tanaka, A. & Node, K. Associations of metabolic disorders with hypertension and cardiovascular disease: recent findings and therapeutic perspectives. Hypertens. Res. Off J. Jpn Soc. Hypertens. 47, 3338–3344 (2024).
Yuan, L. S. & Chen, M. L. Insulin resistance, hyperinsulinemia, and hypertension. Chin. J. Hypertens. 28, 616–620 (2020).
Bello-Chavolla, O. Y. et al. METS-IR, a novel score to evaluate insulin sensitivity, is predictive of visceral adiposity and incident type 2 diabetes. Eur. J. Endocrinol. 178, 533–544 (2018).
Bello-Chavolla, O. Y. et al. Metabolic score for visceral fat (METS-VF), a novel estimator of intra-abdominal fat content and cardio-metabolic health. Clin. Nutr. Edinb. Scotl. 39, 1613–1621 (2020).
Li, J. et al. Association between metabolic score for insulin resistance and hypertension: A cross-sectional study. Chongqing Med. 52, 2310–2314 (2023).
Duan, S. et al. Cardiometabolic index: A new predictor for metabolic associated fatty liver disease in Chinese adults. Front. Endocrinol. 13, 1004855 (2022).
Shi, W. R. et al. Estimate of prevalent diabetes from cardiometabolic index in general Chinese population: A community-based study. Lipids Health Dis. 17, 236 (2018).
An, H. Q. et al. Interaction between genes and occupational stress on hypertension risk in oil workers: a bayesian network analysis. China Occup. Med. 48, 39–45 (2021).
Yang, F. et al. Association between sleep disorders and hypertension among oil workers in Karamay. J. Hyg. Res. 50, 586–592 (2021).
Li, X. et al. Association between occupational stress and hypertension among oilfield workers in desert environments of Xinjiang. Mod. Prev. Med. 46, 25–29 (2019).
Tao, N. et al. Association of glucocorticoid receptor gene polymorphism and occupational stress with hypertension in desert petroleum workers in Xinjiang, China. Bmc Med. Genet. 19, 213 (2018).
Yang, G. H. et al. Prevalence of smoking and passive smoking among Chinese population in 2002. Chin. J. Epidemiol. 26, 5–11 (2005).
Wang, J. M. et al. Diet habits, alcohol drinking, tobacco smoking, green tea drinking, and the risk of esophageal squamous cell carcinoma in the Chinese population. Eur. J. Gastroenterol. Hepatol. 19, 171–176 (2007).
Cai, X. et al. Associations of the cardiometabolic index with the risk of cardiovascular disease in patients with hypertension and obstructive sleep apnea: Results of a longitudinal cohort study. Oxid. Med. Cell. Longev. 4914791 (2022). (2022).
Yang, R. et al. Assessing the usefulness of a newly proposed metabolic score for visceral fat in predicting future diabetes: results from the NAGALA cohort study. Front. Endocrinol. 14, 1172323 (2023).
Zhang, Z., Zhao, L., Lu, Y., Meng, X. & Zhou, X. Relationship of triglyceride-glucose index with cardiometabolic multi-morbidity in China: evidence from a National survey. Diabetol. Metab. Syndr. 15, 226 (2023).
Xiong, S., Hou, N., Tang, F., Li, J. & Deng, H. Association of cardiometabolic Multimorbidity and adherence to a healthy lifestyle with incident dementia: A large prospective cohort study. Diabetol. Metab. Syndr. 15, 208 (2023).
Han, Y. et al. Lifestyle, cardiometabolic disease, and Multimorbidity in a prospective Chinese study. Eur. Heart J. 42, 3374–3384 (2021).
Cheng, X., Ma, T., Ouyang, F., Zhang, G. & Bai, Y. Trends in the prevalence of cardiometabolic Multimorbidity in the united States, 1999–2018. Int. J. Environ. Res. Public. Health. 19, 4726 (2022).
Xu, S. et al. Epidemiological survey of cardiometabolic Multimorbidity and related risk factors in Chinese population: a cross-sectional study. Preprint at https://doi.org/ (2024). https://doi.org/10.21203/rs.3.rs-3896393/v1
Zhang, D. et al. Multimorbidity of cardiometabolic diseases: prevalence and risk for mortality from one million Chinese adults in a longitudinal cohort study. Bmj Open. 9, e024476 (2019).
Xiong, F. et al. [associations between insulin resistance indexes and hyperuricemia in hypertensive population]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 45, 390–398 (2023).
Liu, X. Z., Fan, J. & Pan, S. J. METS-IR, a novel simple insulin resistance indexes, is associated with hypertension in normal-weight Chinese adults. J. Clin. Hypertens. Greenwich Conn. 21, 1075–1081 (2019).
Soleimani, M. Insulin resistance and hypertension: new insights. Kidney Int. 87, 497–499 (2015).
Feng, L. et al. Prevalence and correlates of cardiometabolic Multimorbidity among hypertensive individuals: A cross-sectional study in rural South asia-bangladesh, Pakistan and Sri Lanka. Bmj Open. 9, e030584 (2019).
Glass, C. K. & Olefsky, J. M. Inflammation and lipid signaling in the etiology of insulin resistance. Cell. Metab. 15, 635–645 (2012).
Zheng, Y. et al. Association between composite lifestyle factors and cardiometabolic Multimorbidity in Chongqing, China: A cross-sectional exploratory study in people over 45 years and older. Front. Public. Health. 11, 1118628 (2023).
Wan, X. et al. Shift work promotes adipogenesis via cortisol-dependent downregulation of EGR3-HDAC6 pathway. Cell. Death Discov. 10, 129 (2024).
Yang, F. et al. Interaction between sleep status and occupational stress on hypertension among oilfield workers. Chin. Occup. Med. 48, 386–391 (2021).
Liu, H. R. et al. The relationship between occupational psychological stress and metabolic syndrome. Chin. J. Occup. Med. 88, 92–92 (2015).
Zhao, Y. et al. The prevalence of cardiometabolic Multimorbidity and its associations with health outcomes among women in China. Front. Cardiovasc. Med. 10, 922932 (2023).
Zhou, X. L. et al. Study on the relationship between body constitution and lipid metabolism abnormalities in patients with coronary heart disease of different genders. Shizhen Guo Yi Guo Yao. 31, 2804–2806 (2020).
García-Villafranca, J., Guillén, A. & Castro, J. Ethanol consumption impairs regulation of fatty acid metabolism by decreasing the activity of AMP-activated protein kinase in rat liver. Biochimie 90, 460–466 (2008).
Li, Y. Y. & Zhou, J. Y. The role of Lipin-1 in the pathogenesis of alcoholic fatty liver disease. Chin. J. Hepatol. 24, 237–240 (2016).
Flor, L. S. et al. Health effects associated with exposure to secondhand smoke: A burden of proof study. Nat. Med. 30, 149–167 (2024).
Zhao, Y. et al. Elevated blood remnant cholesterol and triglycerides are causally related to the risks of cardiometabolic Multimorbidity. Nat. Commun. 15, 2451 (2024).
Zhao, F. et al. Weight changes from early to middle adulthood and cardiometabolic Multimorbidity later in life among middle-aged and older adults: A retrospective cohort study from the NHANES 1999–2018. Front. Endocrinol. 15, 1306551 (2024).
Acknowledgements
The authors thank all participants and investigators.
Funding
Xinjiang Uygur Autonomous Region Youth Science and Technology Top Talents Project (2022TSYCCX0097) and Xinjiang Uygur Autonomous Region Key Laboratory Construction Project (Grant No. 2025D04023).
Author information
Authors and Affiliations
Contributions
The authors of the submission meet all of the following criteria: GM: Participate in thesis topic selection and design, data collection, data analysis and interpretation, writing - original manuscript. JQW: Participate in paper topic selection and design, data collection, methodology. XYC and XG: Participate in paper topic selection and design, data collection, validation, and editing. NT and HQA: Supervision, answer academic questions, Writing - Review and Editing, Funding Acquisition, Project Management.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Review Committee of the First Affiliated Hospital of Xinjiang Medical University (Ethics No. XJYKDXR20230303026), and the study subjects gave informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Muheiyati, G., Wang, J., Chen, X. et al. The correlation between different metabolic scores and the risk of cardiometabolic comorbidities in hypertensive patients. Sci Rep 15, 33793 (2025). https://doi.org/10.1038/s41598-025-01963-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-01963-7