Abstract
This study examines trends in application and match rates for the United States Hospice and Palliative Care Fellowship Match, focusing on demographic variations, competitiveness, and match success across applicant types. This retrospective study analyzed data from the National Resident Matching Program for Hospice and Palliative Care fellowships from 2016 to 2024, including applicant demographics and match outcomes. Chi-square tests were used to assess differences and temporal trends were evaluated with Mann–Kendall tests, and statistical significance was set at p < 0.05. Our results were that the number of fellowship programs increased from 122 in 2016 to 185 in 2024 (51.6% increase), with positions rising from 280 to 451 (61.1% increase). Applicants grew by 75.2%, from 259 to 454. US MDs had significantly higher match rates than non-US MDs (86.1% vs. 79.8%, p < 0.001). Female applicants were significantly overrepresented in Hospice and Palliative Care fellowships compared to all fellowships (64.9% vs. 47.0%, p < 0.001), while males were underrepresented (33.4% vs. 51.4%, p < 0.001). A higher proportion of matched applicants were from rural areas compared to all fellowships (16.0% vs. 13.1%, p = 0.040). In conclusion, the number of Hospice and Palliative Care fellowship programs, positions, and applicants has increased. Female applicants, compared to males, and White applicants, relative to their representation in all fellowships, accounted for a larger proportion of applications and had higher match rates. Heterosexual applicants were less likely to pursue Hospice and Palliative Care fellowships compared to all specialties.
Similar content being viewed by others
Introduction
Hospice and Palliative Care fellowships are specialized training programs within the broader field of medicine, designed to equip physicians with advanced expertise in delivering compassionate care to patients with serious, life-limiting illnesses. These programs are accredited by the Accreditation Council for Graduate Medical Education (ACGME) and have gained prominence due to the increasing demand for skilled hospice and palliative care practitioners, driven by an aging population and evolving healthcare needs1.
The National Resident Matching Program (NRMP) provides annual data on match outcomes, offering insights into the competitiveness and trends within various medical specialties, including Hospice and Palliative Care2. Over the past decade, the Hospice and Palliative Care fellowship match has experienced fluctuations in both the number of available positions and the number of applicants. As the demand for hospice and palliative care specialists continues to grow, it is critical to examine how demographic factors, such as race, sex, and international medical graduate (IMG) status, impact applicants’ chances of securing fellowship positions3.
This study seeks to address gaps in the literature by analyzing demographic variations and temporal trends in the United States Hospice and Palliative Care fellowship match from 2016 to 2024. The objectives are to evaluate the overall competitiveness of the fellowship, examine changes in applicant characteristics—including sex, race, ethnicity, and medical school location (US medical graduate versus IMG)—over time, and determine the association of these factors with match rates.
We hypothesize that while the total number of palliative care fellowship positions has increased, the number of applicants has fluctuated, likely influenced by demographic and geographical factors. By analyzing these trends in match outcomes, this study aims to inform strategies to improve recruitment efforts and enhance the inclusivity and accessibility of Hospice and Palliative Care training programs in the United States.
Methodology
This retrospective study analyzed publicly accessible data from the NRMP database on Hospice and Palliative Care fellowship match outcomes for the years 2016 through 20244,5. Previous studies have leveraged similar data to explore match results across various specialties6,7,8. As the data was anonymized and publicly available, no institutional review board (IRB) approval was necessary.
To examine trends over an 8-year period, we collected yearly data on Hospice and Palliative Care applicants, matches, ranked positions, and filled positions. The dataset provided figures for U.S. allopathic (MD) graduates, which allowed us to estimate match rates for non-U.S. allopathic (MD) graduates. Non-U.S. MD graduates include U.S. osteopathic (DO) graduates, U.S. IMGs, non-U.S. IMGs, 5th pathway graduates, and Canadian medical graduates. In addition to examining trends, we used a two-tailed Chi-square test to determine the association between IMG status and successful match throughout the study period.
The data also included percentages of matched allopathic, osteopathic, U.S. IMGs, and non-U.S. IMGs, expressed as a proportion of all Hospice and Palliative Care fellows. We investigated how applicants matched their first, second, third, or subsequent choice of Hospice and Palliative Care program. Temporal changes were analyzed using the Mann–Kendall trend test, with Kendall’s Tau used to quantify the strength and direction of the trends, and p-values < 0.05 determining statistical significance.
Demographic data for the 2023 and 2024 application years were also available, as the NRMP began publicly reporting demographic information in 2023. Key demographic variables included sex, race, ethnicity, urban versus rural status, and first-generation status for college or medical school. These demographics were analyzed for both Hospice and Palliative Care applicants and those who matched, and were also compared to applicants and those who matched across all fellowships combined. Match rates were calculated and analyzed by these demographic categories. Potential disparities between applicants and matched individuals were evaluated using a two-tailed Chi-square test. Statistical significance was defined by a p-value of less than 0.05. All statistical analyses were conducted using XLSTAT software (RRID:SCR_016299).
Results
Number of programs, positions, applicants, and percentage of positions filled
The total number of training programs rose from 122 in 2016 to 185 in 2024, a 51.6% increase (τ = 0.944, p < 0.001), with available fellowship positions also increasing from 280 to 451 a 61.07% increase, (τ = 0.944, p < 0.001). The number of fellowship applicants also increased from 259 in 2016 to 454 in 2024, a 75.2% increase, (τ = 0.944, p < 0.001). There was no significant difference in the percentage of filled positions, 80.7% in 2016 and 83.1% in 2024 (τ = 0.056, p = 0.910) (Fig. 1; Table 1).
Demographic and urbanization status variations
In 2023 and 2024, 423 female applicants (64.9%) and 218 male applicants (33.4%) applied for the Palliative Care fellowship, with the remainder not identifying as male or female, or preferring not to answer. Females were more likely to apply for Hospice and Palliative care compared to females applying to all fellowships (64.9% vs. 47.0%, p < 0.001) and constituted a significantly greater proportion of matched applicants than all fellowships combined (65.1% vs. 48.7%, p < 0.001). Conversely, males were less likely to apply to Hospice and Palliative Care fellowship (33.4% vs. 51.4%, p < 0.001) and were significantly underrepresented in Hospice and Palliative Care compared to matched applicants of all fellowships (33.1% vs. 49.8%, p < 0.001). Females were also significantly more likely to apply and match to Palliative Care fellowship than males of the same category (p < 0.001 for both comparisons).
Asian applicants were less likely to apply to Hospice and Palliative Care compared to all fellowships (25.9% vs. 32.4%, p < 0.001), while White applicants were more likely to apply to Hospice and Palliative Care than to all fellowships (58.7% vs. 49.8%, p < 0.001). Similar trends for seen those actually matched into Hospice and Palliative Care fellowship (Asian applicants that matched in Hospice and Palliative Care fellowship versus all fellowships: 26.7% vs. 31.3%, p < 0.001; White applicants that matched in Hospice and Palliative Care fellowship versus all fellowships: 58% vs. 51.7%, p < 0.001).
There was no statistical difference in the proportion of applicants from rural areas applying to Hospice and Palliative Care versus to all fellowships (16.0% vs. 13.3%, p = 0.055). In contrast, applicants from urban areas were less likely to apply to Hospice and Palliative Care than all fellowships (22.7% vs. 26.7%, p = 0.024) (Table 2). Trends were also calculated among those from rural (16.0% vs. 13.1%, p = 0.040) versus urban (23.0% vs. 25.5%, p = 0.148) areas who ultimately matched.
Heterosexual applicants were significantly less likely to apply to Hospice and Palliative Care than all fellowships (79.1% vs. 87.2%, p < 0.001), while gay/lesbian and bisexual applicants applied to Hospice and Palliative Care at significantly higher rates than all other fellowships (p = 0.045 and p < 0.001 respectively). Similarly, matched heterosexual applicants were significantly underrepresented compared to all fellowships (79.2% vs. 87.1%, p < 0.001), while matched applicants identifying as bisexual made up a significantly higher proportion of the matched demographic than all fellowships (5.4% vs. 2.3%, p < 0.001). Matched gay/lesbian applicants also trended towards a higher representation in the Hospice and Palliative Care match, although this finding was not statistically significant (3.5% vs. 4.9%, p = 0.075). These demographic details are highlighted in Table 2.
Match rates of US MD versus non-US MD graduates
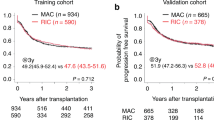
US MD graduates had a significantly higher match rate than non-US MD graduates over the study period (86.1% vs. 79.8%, p < 0.001). However, during the initial study period, 2016 and 2017 US MD had a lower match rate than non-US MD graduates (85.7% vs. 89.3% in 2016), (79.5 vs 80.7 in 2017). Over time, there was a slight increase in the annual match rate for US MD graduates (85.7% in 2016 to 88.8% in 2024, τ = 0.778, p = 0.002), while there was a decrease in the annual match rate for non-US MD graduates (89.3% to 79.8%) which was not statistically significant (τ = − 0.222, p = 0.477) (Fig. 2; Table 3).
Variations in the percentage of US MD, US DO, US IMG, and non-US IMG graduates
The number of US MD graduates in Hospice and Palliative care fellowship trended towards an increase from 55.8 to 63.7%, though this change was not statistically significant (τ = − 0.029, p = 0.915). Similarly, for non-US IMGs (τ = − 0.141, p = 0.600), and US DOs (τ = 0.167, p = 0.612) the trend remained unchanged. In contrast, the only statistically significant trend among medical training backgrounds was with US IMGs, with the percentage in Hospice and Palliative Care fellowship decreasing significantly from 15.9% to 10.7% over the study period (τ = − 0.611, p = 0.025) (Fig. 3; Table 4).
Applicant match data by choice of program
Over the 8-year study period, trends in the percentage of applicants matching to their first-choice program (τ = − 0.333, p = 0.260), second choice (τ = 0.222, p = 0.477), third choice (τ = 0.514, p = 0.058), or fourth or lower choice (τ = 0.310, p = 0.249) remained unchanged (Fig. 4; Table 5).
Unmatched applicants
The percentage of unmatched applicants showed a statistically significant decrease from 12.7% in 2016 to 8.4% in 2024 (τ = − 0.783, p = 0.004).
Discussion
This study provides the first comprehensive analysis of demographic variations and temporal trends in the United States Hospice and Hospice and Palliative Care fellowship match data from the NRMP. Over the study period, the number of Palliative Care fellowship training programs, positions, and applicants increased. Female applicants represented a larger proportion of applications and had significantly higher match rates than males. White applicants were more likely to apply for and match into Hospice and Palliative Care fellowships compared to their representation in all fellowships. Heterosexual applicants were less likely to pursue Hospice and Palliative Care fellowships compared to all fellowships. US MDs demonstrated higher match rates than non-US MDs. Lastly, the rate of applicants going unmatched has decreased over the study period.
Our study reveals that females are more likely to apply for and match into Hospice and Palliative Care fellowships compared to their representation in all fellowships. Moreover, significantly more females applied than males (423 vs. 219 applicants). This trend is noteworthy and aligns with prior research indicating that sex-specific factors, such as the perceived alignment of a specialty with personal values and professional aspirations, significantly influence subspecialty selection9. A survey by LeGrand and Heintz et al. (2012) investigating the demographics, motivations, and decision-making processes of residents pursuing palliative medicine fellowships found that a majority of respondents (61%) were women9. Female physicians often gravitate toward fields like Hospice and Palliative Care, which prioritize work-life balance and patient-centered care10. Moreover, this may stem from the fellowship’s potential to offer career transitions into less chaotic, procedure-intensive settings. Conversely, males demonstrate substantially lower interest in Hospice and Palliative Care, a pattern also observed in pediatric palliative care11. However, the match rates between females and males were similar, with only a small difference (94.6% vs. 93.1%), suggesting minimal clinical significance.
Racial disparities were evident in our analysis. Compared to all fellowships, Asian applicants were less likely to apply for or match into Hospice and Palliative Care fellowships, whereas White applicants showed the opposite trend. These findings align with research from other subspecialties, where factors such as mentorship availability, cultural influences, and the perceived emotional demands of the specialty play a significant role12. To effectively meet the diverse needs of patients, it is essential for the Hospice and Palliative Care workforce to become more inclusive and diverse. Although our study found no significant differences in application or match rates for Black individuals, this could be attributed to the underpowered nature of the outcome. Existing research highlights a severe lack of racial diversity in palliative medicine, with fewer than 5% of hospice and palliative medicine fellows identifying as Black. Research by Bell et al. underscores critical disparities in palliative care training among Black medical trainees, particularly at institutions with higher percentages of Black student enrollment13. Additionally, none of the historically Black colleges and universities with medical schools offer dedicated palliative care training, such as courses, clerkships, rotations, or affiliated hospice and palliative care fellowship programs13. Moreover, institutions with the highest Black student enrollment were less likely to provide palliative care training during internal or family medicine residencies compared to those with the lowest Black enrollment13. Addressing these racial gaps is crucial to fostering a more equitable and representative healthcare workforce. The fellowship, however, demonstrated notable diversity and inclusion within its workforce, with a higher number of bisexual applicants and a trend toward greater representation of gay and lesbian applicants compared to their representation in all fellowships.
Notable geographic trends were observed in match rates and fellowship applicants. Rural applicants were more likely than urban applicants to match into Hospice and Palliative Care fellowships, potentially reflecting a stronger commitment to addressing the high demand for Palliative Care services in underserved rural areas. This finding supports the hypothesis that rural programs often attract applicants driven by a dedication to bridging rural healthcare gaps, including the need for Palliative Care services. Conversely, applicants from metropolitan areas showed a preference for more technologically complex specializations14. This contrast underscores the diverse motivations and preferences influencing medical career trajectories, shaped by geographic and program-specific contexts.
Significant variations in match rates were observed based on educational backgrounds, with US MDs matching at significantly higher rates than non-US MDs, and this disparity increasing over time. Similar patterns have been documented in other subspecialties where US MD graduates typically have an advantage in the matching process15. This trend may be attributed to program preferences for applicants who do not require visa sponsorship. Lastly, compared to other applicants in our demographic dataset, those who were the first in their family to attend college had a slightly lower match rate of 90.3%. This disparity may be attributed to financial and resource-related challenges, limited familial exposure to higher education, and reduced access to relatable mentors and networking opportunities.
Limitations
This study has various limitations that must be noted. First, while it analyzes match outcomes from 2016 to 2024, the conclusions represent previous patterns and may not effectively forecast future trends. Second, the lack of statistics on the number of fellowship program applications and interview invites limits our knowledge of the matching process. Third, the demographic data, including race and ethnicity, were only accessible for the last two years, making it difficult to identify consistent long-term patterns. Fourth, it is unclear how residency program rankings and other training-related characteristics influence match success. Fifth, our study may be subject to biases inherent in the questionnaire-based format of the NRMP database. These include response bias, recall bias, and social desirability bias, which are common limitations of self-reported data. However, because the NRMP collects responses anonymously, these biases may be reduced to some extent. Nonetheless, the findings of our study should be interpreted with caution. Lastly, various confounding factors, such as geographic location, personal preferences, and training backgrounds are likely to influence match outcomes and should be investigated further.
Conclusion
In summary, the number of Hospice and Palliative Care fellowship training programs, positions, and applicants increased. Female applicants, compared to males, and White applicants, relative to their representation in all fellowships, accounted for a larger proportion of applications and had higher match rates. Heterosexual applicants were less likely to pursue Hospice and Palliative Care fellowships compared to all fellowships. US MDs consistently demonstrated higher match rates than non-US MDs. Future research should focus on initiatives to address challenges such as the underrepresentation of certain demographics in palliative care and the growing demand for trained professionals as the population ages. This will be crucial for developing a more diverse and resilient palliative care workforce capable of meeting future healthcare needs.
Data availability
All data can be requested by emailing the corresponding author with a reasonable request.
Abbreviations
- ACGME:
-
Accreditation council for graduate medical education
- NRMP:
-
National resident matching program
- IMG:
-
International medical graduate
- MD:
-
Doctor of medicine
- DO:
-
Doctor of osteopathic medicine
References
Roth, A. R. & Canedo, A. R. Introduction to hospice and palliative care. Prim Care 46(3), 287–302. https://doi.org/10.1016/j.pop.2019.04.001 (2019).
Appointment Year. (n.d.). Charting outcomes in the match. Nrmp.org. Retrieved November 9, 2024, from https://www.nrmp.org/wp-content/uploads/2021/08/2018-Charting-Outcomes-SMS.pdf
Lupu, D., Quigley, L., Mehfoud, N. & Salsberg, E. S. The growing demand for hospice and palliative medicine physicians: Will the supply keep up?. J. Pain Symptom Manage. 55(4), 1216–1223. https://doi.org/10.1016/j.jpainsymman.2018.01.011 (2018).
Match Data | NRMP. NRMP. August 20, 2024. https://www.nrmp.org/match-data/
Bartek S. Charting outcomesTM: Demographic characteristics of applicants in the specialties matching service® | NRMP. NRMP. August 27, 2024. https://www.nrmp.org/match-data/2024/04/charting-outcomes-demographic-characteristics-of-applicants-in-the-specialties-matching-service/
Silvestre, J., Brgdar, A. & DeLisser, H. M. Match outcomes for cardiovascular disease fellowship training: 2010 to 2021. J. Am. Heart Associat. 11(24), e028237. https://doi.org/10.1161/jaha.122.028237 (2022).
Goodman, C. R. et al. No longer a match: Trends in radiation oncology national resident matching program (NRMP) data from 2010–2020 and comparison across specialties. Int. J. Radiat. Oncol. Biol. Physics. 110(2), 278–287. https://doi.org/10.1016/j.ijrobp.2021.03.006 (2021).
Silvestre, J., Aakhus, E., Weldeslase, T. A. & DeLisser, H. M. A 15-year analysis of supply and demand for hematology and oncology training in the United States. JCO Oncol. Pract. 20(5), 717–724. https://doi.org/10.1200/op.23.00531 (2024).
Susan, B. et al. Palliative medicine fellowship: A study of resident choices LeGrand. J. Pain Symptom Manage. 43(35), 558–568 (2012).
Yin, K. et al. Gender differences and influencing factors in specialty choices: Findings from one medical school in China. Front. Public Health 9, 648612 (2021).
De Clercq, E. et al. The conceptual understanding of pediatric palliative care: A Swiss healthcare perspective. BMC Palliat. Care 18(1), 55. https://doi.org/10.1186/s12904-019-0438-1 (2019).
Gisselbaek, M. et al. Gender and Race/Ethnicity dynamics in anesthesiology mentorship: Results of a European survey. BMC Anesthesiol. 24(1), 311. https://doi.org/10.1186/s12871-024-02692-6 (2024).
Bell, L. F. et al. Lack of exposure to palliative care training for black residents: A study of schools with highest and lowest percentages of black enrollment. J. Pain Symptom Manage. 61(5), 1023–1027. https://doi.org/10.1016/j.jpainsymman.2020.11.010 (2021).
Longenecker, R. et al. A match made in rural: Interpreting match rates and exploring best practices. Fam. Med. 55(7), 426–432. https://doi.org/10.22454/FamMed.2023.106345 (2023).
Chandrakanth, et al. Trends in the match rate and composition of candidates matching into categorical general surgery residency positions in the United States Are. Am. J. Surg. 213(1), 187–194 (2017).
Author information
Authors and Affiliations
Contributions
All authors contributed to writing and reviewing the article. Additionally, Samuel Flesner and Aman Goyal did the statistical analysis and utilized software. Amir Sohail and Mohamed Daoud did validation and supervision. Aman Goyal and Amir Sohail did conceptualization. Urooj Shamim, Sonia Hurjkaliani, and Priya Goyal worked on figures, tables, and data curation.
Corresponding author
Ethics declarations
Competing interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Goyal, A., Flesner, S.L., Shamim, U. et al. Demographic variations and temporal trends in hospice and palliative care fellowship matches in the United States. Sci Rep 15, 29101 (2025). https://doi.org/10.1038/s41598-025-02332-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-02332-0