Abstract
C-reactive protein (CRP) is a well-established marker of inflammation in neonates. Recent studies have shown the potential of CRP velocity as an early indicator of infection disorders in children and adults. However, data on CRP dynamics in the neonatal population remain limited. Our objective was to assess the dynamics of CRP levels and determine their clinical relevance in newborns admitted to the nursery. This is a retrospective review of medical records of neonates ≥ 35 weeks of gestation with a birth weight of ≥ 2000 g, who underwent partial sepsis work-up with at least 2 consecutive CRP measurements within the first 48-h of life, between January and December 2020. CRP dynamics were analyzed using CRP velocity (CRPv, mg/L/h), calculated by dividing the interval between the first two consecutive CRP measurements by the corresponding interval time. A total of 212 neonates were included in the study. Neonates admitted to the neonatal intensive care unit (NICU) presented with higher levels of CRPv (p = 0.047), and were more likely to experience hypoglycemia (p = 0.023) and respiratory distress (p = 0.023). Lower CRPv levels were associated with elective cesarean surgery (p = 0.043). Among neonates with CRPv ≥ 2 mg/L/h, female infants exhibited even higher CRPv values (p = 0.018). Only two cases of blood culture-confirmed neonatal sepsis were identified, with CRPv values of 3.22 and 0.02 mg/L/h., Neither case required NICU admission. Regression analyses revealed that higher gestational age was significantly associated with elevated CRPv levels (p = 0.004) whereas hypothermia was linked to lower CRPv values (p = 0.031). In neonates, CRP dynamics generally corresponded to their overall clinical condition but were also influenced by various non-infectious factors, including GA, mode of delivery and gender. Additionally, neonatologists should consider the recent finding that neonatal hypothermia was associated with decreased CRP levels when assessing ill-appearing newborns with low CRP measurements.
Similar content being viewed by others
Introduction
C-reactive protein (CRP) is an inflammatory biomarker and is one of the downstream mediators of the acute-phase response1,2. It stands out as a simple, rapid, and cost-efficient laboratory test (2). Elevated CRP levels have been consistently correlated with acute bacterial diseases, and are commonly used by clinicians to guide antibiotic decisions2,3. As CRP is produced by the liver and does not cross the placenta, any increase in neonatal CRP levels reflects endogenous synthesis1,2.
Early onset of neonatal sepsis (EOS), a serious blood infection in newborns occurring within the first 72 h of life, exhibits varying mortality rates, ranging from 11 to 19%4. Prompt diagnosis and treatment of neonates with suspected sepsis are crucial to prevent severe and potentially life-threatening complications. However, this is complicated by the condition’s variable and non-specific clinical signs, such as respiratory distress and fever2,5,6. The diagnosis of neonatal sepsis typically involves a combination of methods, the EOS multivariate risk assessment calculator, and clinical evaluation of the newborn7. The sensitivity and specificity of CRP for diagnosing EOS show significant variability2,3,6,8. CRP has low sensitivity in the early stages of infection1,2,9 and can exhibit a physiological increase after birth or in non-infection-related condition2,10,11,12. As a result, antibiotics are often initiated in many newborns with a high suspicion of sepsis, even in the absence of a confirmed infection9. The calculated CRP velocity (CRPv), defined as the rate of change in CRP levels over time, has been reported as a valuable diagnostic tool for distinguishing acute bacterial from viral infections, and for early detection of acute infections in adults. It has also been used to differentiate postoperative fever secondary to bacterial infection from fever secondary to noninfectious origins in children13,14,15. Although CRP has been extensively studied in neonatology, research specifically examining CRPv or CRP dynamics in the neonatal population remains limited. Therefore, our objective was to assess the CRP dynamics and determine its clinical relevance in newborns admitted to the nursery.
Methods
Participants
We designed this retrospective observational study to analyze data collected on neonates born between 01 January 2020 and 31 December 2020 who were admitted to the nursery and underwent a partial sepsis workup within the first 48 h of life. Neonates with only a single CRP measurement were excluded. According to our local guidelines, healthy neonates with a gestational age (GA) ≥ 35 weeks and a birth weight (BW) ≥ 2000 g are admitted to the nursery rather than the Neonatal Intensive Care Unit (NICU). The study was carried out in accordance with Good Clinical Practice guidelines and the Declaration of Helsinki. Informed consent was waived by our local committee No. 0272–21-TLV, May 09, 2021.
Data collection
Blood analyses were performed according to our nursery’s standard of care. Indications for a sepsis workup were maternal or neonatal fever, amnionitis, neonatal grunting, distress, desaturation, hypothermia, or hypoglycemia. Broad-spectrum antibiotics were administered for 48 h until blood culture returned negative, with treatment decisions made at the neonatologist’s discretion. The Neonatal Early Onset Sepsis calculator was incorporated into routine care for neonates with a GA ≥ 35 weeks in 2021, after the study period. CRP velocity (CRPv) was calculated using the first two consecutive CRP measurements. This was done by dividing the difference between the two CRP values (CRP-2 at time T2 minus CRP-1 at time T1) by the time interval between measurements (T2—T1). Collected demographic and clinical data of the neonates included GA, gender, BW, mode of delivery, 1-min and 5-min Apgar scores, morbidities, weight for gestational age (small for gestational age [SGA], appropriate GA [AGA] and large GA [LGA])16, medications and partial sepsis workup (CRP, complete blood count [CBC] and blood culture). Maternal data included age, prenatal medication and conditions. The dynamics of CRP were evaluated in relation to both maternal and neonatal variables.
Statistical analysis
Categorical variables are reported as frequencies and percentages. Descriptive statistics (means and standard deviations, for normally distributed variables, or median and interquartile range) were calculated for demographic data. Normality was assessed by Shapiro–Wilk tests. Independent T-test or Mann–Whitney U test or Kruskal–Wallis test (adjusted by the Bonferroni correction for multiple tests) was applied to compare continuous variables when appropriate. Chi-square tests or Fisher’s exact tests were applied to compare categorical variables. Due to the irregular distribution of CRP (1 and 2) and CRPv concentrations, we applied a logarithmic transformation (base 10) to reduce skewness and kurtosis and stabilize the variance of the residuals. The LOG10 values of CRPv were used in regression analyses. We employed linear regression (enter mode) or stepwise linear regression to assess the impact of various factors on CRP measurements and CRPv. IBM SPSS Statistics for Windows, Version 29.0.2.0 Armonk, NY, was used for statistical data analyses and p-values < 0.05 were considered statistically significant.
Results
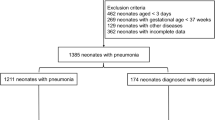
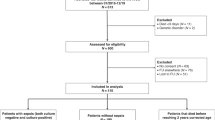
Among the 9,859 deliveries between January and December 2020 admitted to the nursery, 230 neonates underwent a sepsis workup within the first 48 h of life. Of these 212 had at least two consecutive CRP measurements, allowing for CRPv calculation (Fig. 1). During this period, two cases of confirmed EOS with positive blood cultures were identified, resulting in a rate of 0.2 per 1,000 live births. One case was caused by Escherichia coli (E. coli) bacteremia and the other by Group B Streptococcus (GBS) bacteremia. Descriptive characteristics of the mothers and neonates are presented in Table 1. The average maternal age was 32.4 years, while neonates had a mean GA of 39 weeks (range 35 to 42 weeks). The male-to-female ratio was not significantly different (56.1% vs 43.9%, p = 0.074). The NICU admission rate for these neonates was 10%. None of the EOS cases required NICU admission. All neonates survived to discharge. The first CRP measurements (CRP-1) were taken between 1 and 29 h of life, with a median value of 7 h. The second measurements (CRP-2) were taken between 7 and 48 h of life, with a median value of 22 h. The median interval time between CRP measurements was 12.5 h.
CRP measurements were influenced by the neonatal gender, with female neonates having higher CRP-1 and CRP-2) measurements than males (median [mg/L], 2.5 vs 0.4, p = 0.002 and 13.7 vs 6.7, p = 0.009, respectively). However, this difference was not observed for CRPv (median [mg/L/h], 0.3 vs 0.2, p = 0.333). Both CRPv and CRP measurements, were impacted by the mode of delivery. Neonates born via elective cesarean section had significantly lower CRPv compared to those born via vaginal delivery (median [mg/L/h], 0.06 vs 0.33, adjusted p = 0.043). CRP levels were also significantly lower in neonates delivered by elective cesarean section than in those born via vaginal delivery or emergency C-section (all p < 0.050). Neonates admitted to the NICU had a significantly higher CRPv than those kept at the nursery (median [IQR, mg/L/h] 0.7 [0.1–2.7] vs 0.2 [0.02–1], p = 0.047) along with significantly more comorbidities such as hypoglycemia (14.3% vs 2.1%, p = 0.023) and respiratory distress (90.5% vs 69.8%, p = 0.044). The overall rate of hypothermia was 17.5%, with all affected neonates managed in the nursery. Median CRPv levels were significantly lower in neonates with hypothermia compared to those without (0.1 vs 0.3 mg/L/h, p = 0.043).
CRPv was similar among neonates regardless of whether their mothers received full, partial, or no antibiotic treatment (p = 0.994). Antibiotic treatment was started in 65.1% of the neonates, with 9.4% receiving prolonged treatment (≥ 48 h) due to clinical concern such as fever and elevated CRP levels. However, only 1% (2/212 cases) had confirmed EOS. After excluding the confirmed cases of EOS, median CRPv was significantly higher in neonates who received a full course of antibiotics compared to those who received prophylactic antibiotics or no treatment (3.3 vs 0.2 mg/L/h, adjusted p = 0.001, and 3.3 vs 0.3 mg/L/h, adjusted p = 0.018, respectively). Additionally, neonates who completed a full antibiotic course had significantly higher rates of fever (18.2% vs 2.5%, p = 0.045) and NICU admission (36.4% vs 8.5%, p = 0.016) compared to those who discontinued empiric treatment or were not treated.
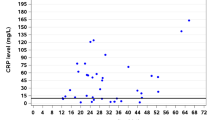
Linear regression analyses, on the complete cohort (N = 212), were conducted to explore the relationship between CRPv and CRP measurements and infectious as well as non-infectious variables such as GA, mode of delivery, gender, weight for gestational age and time intervals between CRP measurements. The model, although statistically significant (F(7, 211) = 6.8, p < 0.001), explained 18.8% of the variance (adjusted R2 = 0.160). CRPv levels were lower in neonates whose CRP assessment was initiated later in life (β = -0.008, p < 0.001) and in those who experienced hypothermia (β = -0.058, p = 0.031). Conversely, higher CRPv levels were associated with increasing GA (β = 0.003, p = 0.004), (Fig. 2). In addition, the first CRP measurement was influenced by neonate age in hours (β = 0.038, p < 0.001), female gender (β = 0.209, p = 0.001), maternal amnionitis (β = 0.330, p = 0.007), hypothermia (β = -0.233, p = 0.006) and GA (β = 0.006, p = 0.040), explaining 32.8% of the variance, whereas the second CRP measurement was influenced by GA (β = 0.015, p < 0.001) and hypothermia (β = -0.357, p < 0.001), explaining 19.5% of the variance. Furthermore, stepwise regression analysis among neonates exhibiting a CRPv ≥ 2mg/L/h (n = 32) showed that higher CRPv was associated with female gender (β = 0.070, p = 0.018) and not GA, mode of delivery, hypothermia, initiation of CRP assessment, weight for gestational age and time intervals between CRP measurements.
In our cohort, only two cases of blood culture-confirmed EOS were identified, leading to a significant class imbalance which hinders the evaluation of CRPv as a predictive tool for EOS. Furthermore, the CRPv values of these two cases were positioned at opposite extremes (3.22 and 0.02 mg/L/h), corresponding to the 20th percentile and at the 60th percentile of the CRPv distribution, respectively (Fig. 3). Both cases involved male neonates born at 38 weeks of gestation via vaginal delivery. However, the neonate with the lower CRPv value (0.02 mg/L/h) also presented with hypothermia.
Discussion
Our findings highlight the influence of non-infectious factors, such as GA, mode of delivery, gender and clinical parameters like neonatal hypothermia, on CRP measurements and dynamics within the first 48 h of life, emphasizing their role as potential early confounders. Due to the limited number of confirmed EOS cases (only two cases with positive blood cultures), we were unable to evaluate CRP dynamics in relation to EOS. While previous studies in adults and older children, have demonstrated the diagnostic value of CRP dynamics for infection13,15,17, this study explores its diagnostic significance and utility in neonates. Research has shown that obtaining consecutive CRP measurements during the initial 24–48 h after infection onset provides a more accurate and reliable diagnostic approach for early-onset sepsis2. However, CRP levels in neonates are influenced by various non-infectious parameters, such as GA, mode of delivery, neonatal age, or MASF10,11,12,18. Consistent with previous studies, our findings suggest that GA significantly impacts CRP levels2,10,12 with neonates born at later GA exhibiting higher CRPv values. Additionally, female neonates in our cohort tended to produce higher CRP levels within the first few hours of life, and at extreme CRPv values, higher CRPv levels were also associated with female gender. Sbarouni et al., reviewed literature on gender differences in biomarkers and noted that healthy women generally exhibited higher and more variable CRP levels than men19. Birth and early postnatal period are marked by physiological stress and complex adaptations in the newborn20. The significant association between higher CRP values and vaginal deliveries, compared to elective or even emergency cesarean sections, has been reported in previous studies as well10,11. Furthermore, our findings indicate that neonatal hypothermia negatively impacts CRP dynamics. A delay in the onset of the CRP response and peak CRP levels have been observed during therapeutic hypothermia in neonatal encephalopathy, suggesting a potential dampening effect on the inflammatory response21. Hypothermia has been shown to impair immune function in vitro by reducing the number of circulating polymorphonuclear granulocytes and diminishing their oxidative burst capacity. Additionally, in infants undergoing therapeutic hypothermia, cytokine expression is altered, including a delayed secondary peak in key inflammatory mediators such as interleukin-6 (IL-6). Since IL-6 is essential for the hepatic induction of CRP, this delayed cytokine response may contribute to a blunted or delayed CRP elevation in hypothermia-treated neonates22. To our knowledge, this is the first report highlighting the negative impact of hypothermia on CRP measurements and dynamics outside the context of therapeutic hypothermia. This finding warrants further investigation, as it may lead to the misinterpretation of low CRP values as false negatives, potentially resulting in adverse clinical outcomes, particularly in CRP-based sepsis evaluations. In our cohort, the decision to initiate and extend antibiotic treatment was primarily based on the clinical condition of the neonates, even in cases of negative blood cultures. CRP dynamics aligned with the clinical presentation, supporting the neonatologist’s decisions to treat and/or transfer neonates to the NICU.
Variability in CRP responses among neonates may be attributed to their unique characteristics, including immature organ function and an underdeveloped immune response12. We hypothesize that limited CRP production in younger neonates may be due to their smaller liver size, whereas higher CRP levels have been associated with greater liver maturity in older neonates2.
A key strength of our study is the use of data from a single tertiary hospital, minimizing heterogeneity related to routine practices and management of suspected neonatal sepsis. This report is the first to assess the variability and clinical significance of CRPv in neonates. However, our study has several limitations, including its retrospective design, which may introduce sampling bias and variability in medical records. The small cohort size and the inclusion of neonates whose mothers received antibiotics prior to delivery are additional limitations.
Conclusions
In neonates, CRP dynamics generally reflected their overall clinical condition but were also influenced by various non-infectious factors, including GA, mode of delivery and gender. Additionally, neonatologists should consider the recent finding that neonatal hypothermia is associated with decreased CRP levels when assessing ill-appearing newborns with low CRP measurements.
Data availability
The datasets used during the current study available from the corresponding author on reasonable request.
References
Pepys, M. B. & Hirschfield, G. M. C-reactive protein: a critical update. J Clin. Invest. 111(12), 1805–1812 (2003).
Hofer, N., Zacharias, E., Müller, W. & Resch, B. An update on the use of C-reactive protein in early-onset neonatal sepsis: current insights and new tasks. Neonatology 102(1), 25–36 (2012).
Benitz, W. E., Han, M. Y., Madan, A. & Ramachandra, P. Serial serum C-reactive protein levels in the diagnosis of neonatal infection. Pediatrics 102(4), E41 (1998).
Fleischmann-Struzek, C. et al. The global burden of paediatric and neonatal sepsis: a systematic review. Lancet Respir. Med. 6(3), 223–230 (2018).
Fleiss, N., Schwabenbauer, K., Randis, T. M. & Polin, R. A. What’s new in the management of neonatal early-onset sepsis?. Arch. Dis. Child Fetal. Neonatal Ed. 108(1), 10–14 (2023).
Chiesa, C. et al. C-reactive protein, interleukin-6, and procalcitonin in the immediate postnatal period: influence of illness severity, risk status, antenatal and perinatal complications, and infection. Clin. Chem. 49(1), 60–68 (2003).
Puopolo KM, Lynfield R, Cummings JJ, Committee on fetus and newborn, committee on infectious diseases. Management of infants at risk for group B streptococcal disease. Pediatrics. https://doi.org/10.1542/peds.2019-2350, (2019).
Friedman, N., Yochpaz, S., Zirkin, S., Herzlich, J. & Marom, R. C-reactive protein and the neonatal early-onset sepsis calculator for the diagnosis of neonatal sepsis. Eur. J. Clin. Microbiol. Infect Dis. 40(6), 1227–1234 (2021).
Eichberger, J., Resch, E. & Resch, B. Diagnosis of neonatal sepsis: the role of inflammatory markers. Front Pediatr. 8(10), 840288 (2022).
Perrone, S. et al. C reactive protein in healthy term newborns during the first 48 hours of life. Arch. Dis. Child Fetal. Neonatal. Ed. 103(2), F163–F166 (2018).
Kozlovski, T., Yochpaz, S., Shachar, I., Friedman, N. & Marom, R. Does the delivery mode affect post-birth neonatal serum C-reactive protein levels? A causal effect analysis. J. Paediatr. Child Health. 58(8), 1330–1336 (2022).
Chiesa, C. et al. C reactive protein and procalcitonin: reference intervals for preterm and term newborns during the early neonatal period. Clin. Chim. Acta. 412(11–12), 1053–1059 (2011).
Paran, Y. et al. C-reactive protein velocity to distinguish febrile bacterial infections from non-bacterial febrile illnesses in the emergency department. Crit. Care. 13(2), R50 (2009).
Coster, D. et al. Using the kinetics of C-reactive protein response to improve the differential diagnosis between acute bacterial and viral infections. Infection 48(2), 241–248 (2020).
Nahum, E. et al. Role of C-reactive protein velocity in the diagnosis of early bacterial infections in children after cardiac surgery. J. Intensive Care Med. 27(3), 191–196 (2012).
Dollberg, S., Haklai, Z., Mimouni, F. B., Gorfein, I. & Gordon, E.-S. Birth weight standards in the live-born population in Israel. Isr. Med. Assoc. J. 7(5), 311–314 (2005).
Wasserman, A. et al. Septic patients presenting with apparently normal C-reactive protein: A point of caution for the ER physician. Medicine 98(2), e13989 (2019).
Tiozzo, C. & Mukhopadhyay, S. Noninfectious influencers of early-onset sepsis biomarkers. Pediatr. Res. 91(2), 425–431 (2022).
Sbarouni, E., Georgiadou, P. & Voudris, V. Gender-specific differences in biomarkers responses to acute coronary syndromes and revascularization procedures. Biomarkers 16(6), 457–465 (2011).
Hillman, N. H., Kallapur, S. G. & Jobe, A. H. Physiology of transition from intrauterine to extrauterine life. Clin. Perinatol. 39(4), 769–783 (2012).
Chakkarapani, E., Davis, J. & Thoresen, M. Therapeutic hypothermia delays the C-reactive protein response and suppresses white blood cell and platelet count in infants with neonatal encephalopathy. Arch. Dis. Child Fetal. Neonatal Ed. 99(6), F458–F463 (2014).
Russwurm, S. et al. Direct influence of mild hypothermia on cytokine expression and release in cultures of human peripheral blood mononuclear cells. J. Interferon. Cytokine Res. 22, 215–221 (2002).
Author information
Authors and Affiliations
Contributions
J.H., D.M. and L.M conceptualized the study. Methodology and data acquisition, J.H., Y.W. and L.M. Validation, R.M. Data analysis, L.M. Original draft preparation, J.H. and L.M. Review and editing, D.M., Y.W., R.M. and S.B. All authors reviewed the manuscript. Original draft preparation, J.H. and L.M. Review and editing, D.M., Y.W., R.M. and S.B. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Herzlich, J., Waksman, Y., Marom, R. et al. Determinants of CRP measurements and CRP dynamics during early neonatal sepsis work up. Sci Rep 15, 18031 (2025). https://doi.org/10.1038/s41598-025-02337-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-02337-9