Abstract
The uneven distribution of human resources for health (HRH) in China, particularly within the realm of traditional Chinese medicine (TCM), has long posed a significant challenge. Although prior studies have examined regional disparities in overall HRH, limited research has specifically addressed the spatial and temporal dynamics of HRH in TCM and their underlying determinants. This study employs a multiscale geographically weighted regression (MGWR) model to explore the spatial and temporal dynamics of HRH in TCM across 31 Chinese provinces from 2008 to 2021. MGWR allows each explanatory variable to operate at its optimal spatial scale, capturing localized patterns of spatial heterogeneity. The results reveal that although HRH in TCM has generally increased over time, substantial disparities persist, with eastern and central regions exhibiting a higher degree of resource agglomeration while western regions continue to lag behind. Economic factors such as wage income, the number of TCM institutions, and education funding emerge as the most significant and spatially heterogeneous determinants. These localized effects suggest that region-specific policy interventions are needed—such as financial incentives and infrastructure support for underserved western regions, and institutional integration and quality standardization in eastern areas—reflecting the differentiated roles and development contexts of TCM across regions. By leveraging the advantages of MGWR in capturing multiscale spatial patterns, this study provides empirical evidence to support more targeted and sustainable planning for HRH in TCM development. Enhancing the accessibility of TCM services not only addresses current regional imbalances but also strengthens the healthcare system’s capacity to respond to the needs of an aging population and future public health emergencies. The findings offer valuable insights for policymakers aiming to improve health equity in China and may inform similar efforts in other countries facing spatial disparities in traditional medicine resources.
Similar content being viewed by others
Introduction
The uneven distribution of global human resources for health (HRH) has long posed a significant challenge within the field of public health1,2. High-income countries often enjoy far greater access to healthcare professionals than low- and middle-income countries, and even within countries, urban-rural inequalities in HRH can severely restrict access to quality care and undermine health equity3,4,5,6,7,8,9. In response to such challenges, WHO have increasingly emphasized the role of traditional medicine in advancing global health equity. The “WHO Traditional Medicine Strategy 2014–2023” advocates for the systematic integration of traditional medicine into national health systems. China, which has long integrated Traditional Chinese Medicine (TCM) into its national health system, offers a valuable case for understanding how traditional medicine can function within modern health governance. Studying the distribution and development of HRH in TCM may therefore provide valuable policy insights for countries aiming to strengthen or integrate traditional medical systems within their broader health governance frameworks. However, while China offers a compelling model of traditional medicine integration, its TCM human resources remain unevenly distributed across regions, limiting the full realization of health equity objectives domestically.
In China, as global aging intensifies and public health emergencies become increasingly frequent in the post-pandemic era, HRH in TCM have emerged as a crucial force in mitigating the impacts of population aging and addressing public health emergencies10,11,12. Since the latest round of healthcare reforms, the Chinese government has introduced strategic plans for the development of TCM and proposed a ‘Chinese solution,’ which has positively contributed to economic adjustments13,14. Particularly since the outbreak of the COVID-19 pandemic in 2019, TCM has played an effective role in fighting the epidemic, largely due to its cost-effectiveness15. Human capital of TCM, as a key driver of scientific pandemic response and disease prevention, has garnered widespread attention from society.
Over the past 15 years, despite relatively limited advancements in TCM, there has been significant growth in its HRH, particularly in enhancing capabilities of primary healthcare services. In 2020, the total number of TCM technicians in China reached about 830,627, with about 579,847 of these individuals serving as TCM practitioners, thus constituting the majority of the TCM workforce. By 2021, China had approximately 192 higher education institutions offering clinical medicine education, marking a significant increase in their number. Additionally, China boasts the world’s largest workforce of practicing physicians. However, it is important to note that mere economic investment cannot effectively improve healthcare service accessibility16. There is still a significant gap in healthcare service accessibility when compared to developed countries.
Health resources of TCM in China are distinctive for their distribution and arrangement significantly influenced by both macroeconomic reforms and micro-level factors such as urban-rural population mobility17,18,19. Furthermore, the natural geographical differences across regions, particularly the locations of medicinal herb production areas, confer unique advantages to certain regions, thereby exacerbating regional disparities in health resources20. These disparity not only underscore the imbalance in resource allocation but also presents challenges in achieving healthcare accessibility and equity21,22. As a vital complement to healthcare services, the HRH in TCM play a crucial role in enhancing the overall quality of healthcare delivery. While research focusing on the education and standardized training of medical students is important, it is equally essential to study the regional disparities among TCM practitioners. Developing effective policies to address the geographical disparities in the distribution of TCM practitioners is necessary to improve regional inequalities in healthcare resources23,24,25.
Due to population mobility, HRH in TCM may exhibit significant location-based spatial effects, including spatial dependency and heterogeneity. Traditional regression model assumptions can lead to considerable estimation biases and may be inadequate for accurately explaining the geographic heterogeneity of HRH in TCM26,27. Most studies28,29,30 demonstrate the broader applicability of spatial models in uncovering localized relationships within complex systems—an approach that resonates with the challenges of studying TCM health workforce distribution. While some research has addressed the spatial distribution characteristics of HRH in China, there is a significant lack of in-depth studies and analyses specifically focusing on the spatial heterogeneity in the TCM field31. Moreover, most existing studies have focused on the overall distribution of HRH, with limited attention to the spatial heterogeneity and multiscale drivers specific to TCM human resources across regions. In view of the limitations in existing studies, the present research aims to advance the understanding of spatial disparities in HRH by focusing on their distinct institutional frameworks and regional development characteristics. Unlike the broader literature on general HRH distribution, the spatial configuration of TCM practitioners is influenced by unique policy arrangements, historical legacies, and healthcare governance models21,22. To effectively capture these geographically differentiated patterns, this study employs a multi-scale Geographically Weighted Regression (MGWR) model. Compared with conventional models such as Ordinary Least Squares (OLS) and standard Geographically Weighted Regression (GWR), MGWR allows for the detection of spatially varying relationships across multiple scales, thereby offering improved explanatory power and policy relevance. To the best of our knowledge, this is the first study to apply MGWR to the analysis of TCM-specific HRH in China, providing both methodological innovation and empirical insights for regionally adaptive health workforce planning.
Furthermore, the application of visual map analysis based on geographic information systems (GIS) can significantly provide further support for refinement of healthcare services accessibility32. Against this backdrop, this study employs provincial-level data from China to build a comprehensive spatial econometric model. By employing models to identify the spatial-temporal characteristics of influencing factors, this study analyzes the development trends and spatial-temporal change of HRH in TCM across different regions. The findings of this study will provide empirical evidence for policy-making, assisting in the reduction of disparities in healthcare services between regions. Local governments should develop and implement strategies tailored to their specific regional contexts to address the challenges posed by an aging population and optimize the allocation of healthcare resources. Specifically, this study will focus on the following key issues: First, it will utilize geography research methods to deconstruct the geographical distribution characteristics and contributing causes of TCM practitioners, clarifying the development and changes within TCM. Second, by examining the spatial-temporal characteristics of various influencing factors, the study will explore optimization strategies for the allocation of HRH in TCM across different regions, aiming to provide scientific guidance for achieving balanced regional healthcare development. Finally, the study aims to offer new perspectives and strategies for the rational planning and effective management of human resources in TCM.
Study area and dataset
Study area
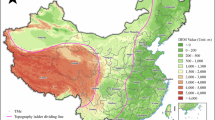
China is located in the eastern part of Asia, along the western coast of the Pacific Ocean, extending from 73°33’ to 135°05’ East and from 3°51’ to 53°33’ North. Its territory stretches from the Uzbel Pass in the Pamirs in the west (Wuqia County) to the confluence of the Heilongjiang and Ussuri rivers in the east, and from the northern end of the main channel of the Heilongjiang River in the north to the Zengmu Ansha in the south. The total area is approximately 9.6 million square kilometers, as illustrated in (Fig. 1). China encompasses a vast and diverse territory, featuring a range of terrains, including plains and hills in the east, basins and plateaus in the central region, and mountains and plateaus in the west. The climate is equally varied: the eastern regions experience temperate and subtropical monsoon climates with abundant rainfall, which is conducive to the cultivation of various traditional Chinese medicinal herbs; the central regions have a relatively dry temperate continental climate, ideal for drought-resistant herbs; and the western regions, characterized by arid plateaus and temperate continental climates, present harsher conditions yet support unique plateau herbs33,34,35. In this complex and diverse geographic and climatic environment, the levels of economic development, population distribution, and policy support vary across different regions of China. These factors collectively contribute to significant disparities in the distribution of TCM healthcare resources nationwide21,36.
Location of the study area. This map was generated by ArcGIS 22.0 (https://www.esri.com/).
This study covers 31 provinces, autonomous regions, and municipalities in China (except Hong Kong Special Administrative Region, the Macau Special Administrative Region, and Taiwan Province). The 31 provincial-level administrative divisions are selected as the basic spatial units for analysis.
Dataset and ethics statement
The data utilized in this study were obtained from the national bureau of statistics (NBS) and the State Administration of Traditional Chinese Medicine, both of which are responsible for monitoring data at the provincial level throughout China. All data are publicly available and aggregated, and the dataset used in this study is complete, with no missing values. As these are secondary data without any personal or identifiable information, informed consent was not required. This study does not involve human participants and uses only publicly available aggregated data; therefore, no ethics approval was necessary. We compiled data on coefficients spanning the years 2008 to 2021 and calculated the agglomeration degree of various resources at the provincial level.
Currently, there is no consensus within the academic community regarding the factors that influence the spatial distribution of HRH in TCM, and the field remains in an exploratory stage. Research indicates that HRH are affected by multiple factors, including economic levels, public service capacity, and healthcare service capabilities2,16,18,19,21,36,37. Consequently, this study selects the following variables and indicators, informed by existing research, relevant theories, and data availability, to dissect driving mechanisms of spatial distribution in HRH. For instance, education funding is used as a proxy for regional public investment in human capital. Based on the New Economics of Labor Migration (NELM) theory, long-term investment in education may enhance a region’s capacity to attract and retain skilled labor, including health professionals. In the context of TCM, where practitioners typically require formal training, such investment is expected to influence the availability and distribution of HRH in TCM. The indicator for “TCM institutions” refers specifically to officially registered facilities, excluding informal or unlicensed private clinics.
Detailed descriptions of the selected variables and their explanations are presented in (Tables 1 and 2).
Methods
The method used in this paper was structured as shown in (Fig. 2). All the maps exhibited in this study were generated by ArcGIS 22.0 (https://www.esri.com/).
Calculation of the agglomeration degree of HRH
Health technicians, also known as medical personnel, refer to professionals engaged in professional and technical work in health institutions, including licensed physicians, registered nurses, occupational pharmacists and other primary health technicians. Human resources for health are defined as health technicians in this study. As the most commonly used index, HRH per thousand population has been widely used in related research to indicate the level of its resource allocation38. Geographical density can also be used to describe the level of allocation of human resources23,38. However, Population per thousand and geographic density indexes cannot present the dynamics of indicators across regions, which affects the credibility of the assessment. Therefore, the agglomeration degree of HRH can take into account the relative levels and dynamic changes in different regions.
The calculation of HRH per thousand population is as follows:
Where \(\:{K}_{i}\) is the HRH of 1,000 people in Province \(\:i\); \(\:Pi\) is the number of HRH in province \(\:i\); \(\:{C}_{i}\) is the number of resident populations in province \(\:i\).
Geographical density can well explain the change of the absolute value of the index. The calculation formula is as follows:
Where \(\:{H}_{i}\) is the HRH of geographic density in Province \(\:i\); \(\:Pi\) is the number of HRHs in province \(\:i\); \(\:{S}_{i}\) is the Geographical area in province \(\:i\).
The agglomeration degree of HRH refers to the degree of HRH population agglomeration in a region relative to all study regions. The specific calculation method is as follows:
Where \(\:{J}_{i}\) is the agglomeration degree of HRH in Province \(\:i\); \(\:Pi\) is the number of HRHs in province \(\:i\); \(\:{C}_{i}\) is the number of resident population in province \(\:i\). \(\:{\complement\:}_{n}\:\)is the total national HRH; \(\:{\text{P}}_{\text{n}}\) is the total population of China.
Indeed, to further confirm the accuracy and consistency of the different models, we compared the degree of change in HRH over the years by normalizing the three models. It is calculated as follows:
Where \(\:\varDelta\:{V}_{im}\) is the total degree of change in HRH over the years in different models respectively; \(\:{V}_{i2020}\) is the value of \(\:{K}_{i}\), \(\:{H}_{i}\), and \(\:{\text{J}}_{\text{I}}\) in 2020; \(\:{V}_{i2008}\) is the value of \(\:{K}_{i}\), \(\:{H}_{i}\), and \(\:{\text{J}}_{\text{I}}\) in 2008;
Spatial autocorrelation test
According to the first law of geography, spatial dependence generally exists among various elements, and its strength tends to change gradually with the spatial distance between them39. Spatial dependence is typically measured using indicators such as Moran’s I index and the Empirical Bayes Ratio. However, the construction of a spatial weight matrix has a high degree of endogeneity, and different matrices can lead to variations in spatial autocorrelation results. Therefore, this study uses the commonly applied contiguity-based spatial weight matrix to calculate Moran’s I40.
Global Moran’s I is employed to analyze the spatial autocorrelation of HRH in TCM across provinces in China, aiming to identify the overall distribution patterns and regional disparities. This method facilitates the revelation of macro-level trends, the quantification of spatial clustering effects, and provides a scientific basis for optimizing resource allocation.
Previous studies41 have demonstrated that local Moran’s I can further identify localized spatial clustering characteristics, thereby aiding in the delineation the spatial relationships between high-resource and low-resource clusters. However, as this study primarily focuses on overall spatial trends, we utilize global Moran’s I for analysis, while considering the application of local Moran’s I in future research to further refine the analysis of regional disparities.
A value near 1 denotes a significant positive spatial autocorrelation, whereas a value near − 1 denotes a strong negative spatial autocorrelation, with the index ranging from − 1 to 1. The formula is as follows:
Where \(\:n\) is the number of provincial-level cities in China; \(\:{\omega\:}_{ij}\) represents the constructed spatial weight matrix; \(\:{\mathcal{X}}_{\text{i}}\)(\(\:{\mathcal{X}}_{\text{j}}\)) denotes the unit elements for regions \(\:i\) and \(\:j\); \(\:\stackrel{-}{\mathcal{X}}\) is the mean value of the elements.
Spatial clusterization kernel density
Kernel density visualizes spatial clustering by measuring the density of features within their surrounding neighborhoods42. A smooth surface is placed over the element points, where the value decreases gradually with increasing distance from the point, reaching zero at the search radius. This is based on a quartic kernel function. The predicted density for an element at (X, Y) is calculated as follows:
For \(\:{dist}_{i}<radius\)
Where \(\:i\:\) represents the feature point of a province; hrh is the feature value of human resources for health. The \(\:{\text{d}\text{i}\text{s}\text{t}}_{i}\) denotes the distance between feature point \(\:i\:\:\)and the location (X, Y).
To determine the search radius, the kernel density bandwidth must be calculated. Considering China’s extensive transportation network that enhances mobility, the Euclidean distance is used for weighting. The calculation formula is as follows:
Where \(\:{D}_{m}\) represents the median distance from the weighted mean center. \(\:SD\) is the standard distance; \(\:{\omega\:}_{i}\) is the weight of feature \(\:i\); \(\:{\overline{\mathcal{X}}}_{\omega\:}\), \(\:{\overline{Y}}_{\omega\:}\:\)and \(\:{\overline{Z}}_{\omega\:}\) represent the weighted mean centers.
Spatial standard deviation ellipse
The standard deviation ellipse (SDE) is a spatial statistical technique proposed by Lefever in 1926 to measure the distribution of geographical elements43. We can summarize the spatiotemporal distribution characteristics of HRH at the provincial level in China by creating SDE: central trend, discrete and directional trend. The distance standard deviation of the HRH point data is calculated based on the theory of survey adjustment theory44:
SDE can compensate for the limitation of the direction of the data that cannot be identified from the standard deviation. We tried to calculate the distribution direction of the HRH dataset by defining a SDE with the following formula:
Firstly, The mean centers \(\:\overline{X}\) and \(\:\overline{Y}\) of the point dataset are calculated. And then, We calculated the orientation angle of the major axis of the ellipse, the formulas as follow:
Finally, Calculate the standard deviation of the long and short semi-axes using the matrix solution method of the coordinate axis rotation, the formulas as follow:
Local regression modeling
Traditional linear regression models are based on the assumption of independence, presuming that features are uniformly distributed across the study area45. However, spatial data often exhibit spatial autocorrelation, and the relationships between variables can vary significantly across different spatial contexts. GWR extends the OLS regression model by incorporating spatial relationships between features, thereby mitigating the effects of improper partitioning inherent in traditional regression models46. Nevertheless, in GWR models, the bandwidth for each variable is calculated as an average of all variable bandwidths, potentially leading to estimation bias when the model is constrained to a uniform spatial scale47. The multiscale geographically weighted regression (MGWR) model advances the GWR approach by incorporating multiple bandwidths, enabling each independent variable to have its unique level of spatial smoothing48. This refinement allows the MGWR model to more accurately capture the spatial positioning and stratified heterogeneity of research subjects arising from spatial segregation.
In this study, MGWR was selected for this study due to its ability to address the spatial heterogeneity of influencing factors in a more refined manner. In the context of HRH distribution, the effects of explanatory variables do not occur uniformly across space. For instance, the impact of average wages may be more locally concentrated, while indicators such as education expenditure or the number of TCM institutions may reflect broader, regionally structured patterns. Traditional GWR applies a single bandwidth to all variables, which may obscure such scale differences. By allowing each variable to have its own optimal bandwidth, MGWR better captures the multiscale spatial variations and offers more accurate and policy-relevant interpretations of how different factors shape the distribution of TCM human resources.
Although MGWR builds upon the GWR framework, its inferential process remains influenced by bandwidth selection and local regression coefficient estimation errors. Based on empirical findings from existing studies, this study employs AICC as the bandwidth selection criterion to achieve an optimal balance between model fit and complexity, thereby enhancing the robustness of the inference results49.
Moreover, compared to other spatial models, such as SEM and SLM, MGWR focuses more on spatial heterogeneity rather than merely addressing spatial autocorrelation. While SEM and SLM assume that spatial effects are global, MGWR allows regression coefficients to vary across locations, making it more suitable for analyzing the regional characteristics of resource distribution.
Based on the above considerations, the study developed an optimal MGWR model to examine the spatial heterogeneity of factors influencing the distribution of HRH. By allowing for variable-specific bandwidths, the MGWR model provides a more nuanced understanding of spatial variations and enhances the precision of spatial analyses. The MGWR model is calculated as follows:
where \(\:{y}_{i}\) denotes the concentration of HRH in the province \(\:i\); \(\:\beta\:\) represents the regression coefficients of the explanatory variables; \(\:bwj\) refers to the bandwidths applied to estimate the regression coefficient of the \(\:j\) variable, \(\:\left({u}_{i},{v}_{i}\right)\) indicates the geographical coordinates of province \(\:i\); \(\:{\epsilon\:}_{i}\) corresponds to the random error term.
Results
The variation trend of HRH in TCM at provincial level in China
Analysis of the health resource aggregation
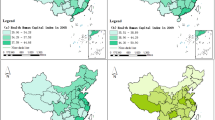
To investigate the spatial concentration of HRH in TCM, this study employs the agglomeration degree to evaluate the allocation of HRH, as illustrated in (Fig. 3). Overall, from 2008 to 2021, the distribution of HRH in TCM has been markedly uneven, with significant disparities observed among provinces. Beijing exhibits the highest agglomeration degree of HRH in TCM in the country, with an average value of 2.3, significantly exceeding the national average. As the capital of China, Beijing benefits from a strategic location that positions it as a central hub for resource allocation, thereby attracting a substantial number of TCM professionals. In contrast, the agglomeration degree of HRH in TCM in the central and western regions, including Chongqing, Sichuan, Inner Mongolia, Gansu, Tibet, and Qinghai, averages around 1.5, indicating a relatively high ranking. This can be largely attributed to the abundance of ethnic medical resources and a comparatively lower population in the Midwest region. In 2021, the agglomeration degree of HRH in TCM in 17 provinces, including Liaoning, Heilongjiang, Shanghai, and Jiangsu, fell below 1, signaling an insufficient supply of TCM resources relative to their populations. Among these, Hainan recorded the lowest agglomeration degree at 0.71, remaining below the national average for HRH in TCM. Additionally, we observed some improvement of HRH in TCM in certain previously uneven provinces. From 2008 to 2021, the agglomeration degree of HRH in TCM in regions such as Shanghai, Guangxi, Anhui, and Guizhou have increased annually, approaching a more balanced state near 1.
However, it is noteworthy that the agglomeration degree of HRH in TCM in developed central regions such as Beijing and Tianjin, as well as in coastal eastern regions like Zhejiang, Fujian, and Guangdong, and in northeastern industrial areas including Heilongjiang, Jilin, and Liaoning, has been declining annually. This trend indicates a significant loss of HRH in TCM in these areas. In summary, there is considerable variation in the concentration and distribution patterns of HRH in TCM across Chinese provinces. The key factors contributing to these disparities warrant further investigation.
Analysis of HRH per thousand population
This study employs the number of TCM practitioners per 1000 people from 2008 to 2021 to create a trend chart that illustrates the changes in HRH across Chinese provinces, as depicted in (Fig. 4). The total number of HRH in China increased from 253,200 in 2008 to 731,700 in 2021, reflecting a growth of 188.9%. Over this period, the overall trend in HRH across Chinese provinces has demonstrated a steady annual increase. In 2021, there were 0.52 TCM practitioners per 1,000 people in China, which remains below the 2025 target of 0.62 practitioners per 1,000 people established by the 14th Five-Year Plan of China. Figure 4 illustrates that the growth rate of HRH in TCM per 1000 people varies significantly across provinces in China, underscoring considerable regional disparities in both the total number of HRH in TCM and the number of TCM practitioners per 1000 people.
Analysis of geographical density of HRH
The measurement of Fig. 5 reflects the degree of change in HRH in each province over the years through geographic density. It should be noted that this comparison method may exaggerate the degree of imbalance between provinces due to ignoring the objective laws followed by the flow of talents. This discovery showed that the number of HRH is increasing year by year, meanwhile the relative level difference in the allocation of health resources has decreased but not obvious.
Comparisons of different HRH results
There are some similarities and differences in the overall changes of the provinces. The degree of change in HRH in different provinces is basically the same in the three models. While maintaining the growth in the number of HRH, the agglomeration of Beijing and Shanghai have the most obvious decline. Interestingly, the HRH growth rate in Guizhou is the fastest among the provinces. There is a wide gap between these three models, which is shown in (Fig. 6). by comparing the total degree of change. The results demonstrated that agglomeration density performed well in dynamic changes of HRH in provincial level of China.
Temporal and spatial changes of HRH in TCM
To further investigate the spatial distribution and evolution of HRH in China, this study utilizes cross-sectional data from 2008, along with average data from three distinct periods: 2009–2013, 2014–2018, and 2019–2021. These datasets are employed to create maps that depict the spatial distribution of HRH in TCM across the country. Figure 7 illustrates a significant imbalance in the distribution pattern of these resources, which are predominantly concentrated in the North China region, particularly around Beijing and Tianjin, the eastern coastal region, including Shanghai and Zhejiang, and the southwestern region, primarily comprising Tibet and Sichuan. Conversely, areas with limited resources are mainly found in the central region, a distribution pattern closely associated with the availability of medicinal resources and levels of economic development. In 2008, only Beijing and Tianjin were classified as high-density areas for HRH. However, during the period from 2019 to 2021, despite a notable increase in HRH throughout China, the number of high-density areas further declined, with only Beijing remaining classified as such, and its agglomeration degree experiencing a decrease of 18.82% compared to 2008. From 2008 to 2021, Inner Mongolia and Sichuan consistently ranked among the semi-dense areas. In contrast, Anhui and Yunnan remained in the sparse resource areas, with their agglomeration degree consistently below 1. Additionally, neighboring provinces such as Guizhou, Guangxi, Jiangxi, and Hunan fluctuated between the sparse and secondary sparse areas. In comparison, provinces like Qinghai, Guizhou, and Guangxi experienced the most significant increases in agglomeration degree of HRH; however, they still fell within the balanced and secondary sparse areas.
Spatial distribution maps of agglomeration degree of HRH between 2008 and 2021. Panels A to D illustrate the agglomeration degree in different periods, including 2008 (A), 2008–2013 (B), 2014–2018 (C), and 2020–2021 (D). Darker green shading indicates a higher degree of agglomeration, with value ranges classified by natural breaks. Provinces with no available data are marked with gray hatching. Maps were generated by ArcGIS 22.0 (https://www.esri.com/).
Although Beijing, Tianjin, and Chongqing have experienced the most significant declines in agglomeration degree of HRH, these regions remain classified as dense or semi-dense areas. This disparity highlights a pronounced ‘Matthew Effect’ in the distribution of HRH across China. Economically advanced regions exhibit a stronger ‘siphoning effect’ for TCM resources, enabling them to continue attracting high-quality TCM professionals despite rapid population growth. In contrast, economically less developed regions are becoming increasingly less appealing for TCM resources. This polarized distribution of HRH in TCM has a substantial impact on the accessibility and equity of healthcare services.
Moran’s I spatial autocorrelation analysis
Through extensive Monte Carlo simulations, the Moran’s I index for health technicians per 10,00 people in 2008 was calculated to be 0.254 (p = 0.02), indicating a significant spatial agglomeration effect. In 2018, the index increased to 0.257 (p = 0.03), demonstrating continued significant clustering. By 2021, the index rose further to 0.382 (p = 0.007), reflecting a highly significant spatial agglomeration effect. This data illustrates a notable and increasing trend in the spatial clustering of HRH in China. To explore regional spatial effects, scatter plots of the Moran’s I index for 2008, 2018, and 2021 were generated (Fig. 8). In these years, most provinces were positioned in the upper right and lower left quadrants. Notably, Tianjin, Beijing, and Inner Mongolia consistently appeared in the upper-right quadrant, indicating that these provinces possess high levels of HRH and are surrounded by provinces with dense distributions.
Spatial-temporal clustering characteristics of HRH in TCM
Using the kernel density analysis tool in ArcGIS 10.2, kernel density estimates for HRH in TCM were conducted for the representative years 2008, 2018, and 2021, resulting in the generation of a HRH density plot, as shown in (Fig. 9). The overall trend in kernel density distribution from 2008 to 2021 remained consistent, indicating the formation of a relatively stable spatial pattern of HRH in TCM. The kernel density of HRH in TCM varied across different regions, generally exhibiting a pattern characterized by ‘higher in the east and lower in the west’. The highest density centers of HRH in TCM were concentrated in areas such as Beijing, Tianjin, and Hebei, which served as central points from which density spread outward in layers. This pattern is closely associated with the coordinated development policy of TCM health resources in the Beijing-Tianjin-Hebei region. Additionally, these areas experienced a spillover effect, contributing to the concentration of HRH in TCM in neighboring provinces such as Shanxi, Henan, and Shandong. High density was also observed at the borders of Jiangsu and Zhejiang, as well as Sichuan and Chongqing, where a siphoning effect inhibited the concentration of HRH in TCM in adjacent provinces. This indicates a gradual concentration of HRH in TCM in economically developed regions.
Kernel density spatial distribution of HRH in TCM across China in 2008 (A), 2018 (B), and 2021 (C). High-density clusters are consistently observed in eastern and central regions. Maps were generated by ArcGIS 22.0 (https://www.esri.com/).
Spatial-temporal variation characteristics of HRH in TCM
The standard deviation ellipse was utilized to illustrate the center of distribution and the diffusion trend of HRH in China from 2008 to 2021, as depicted in (Fig. 10). This figure indicates that the spatial distribution of these resources follows a pattern extending from the east (slightly north) to the west (slightly south). The standard deviation ellipse encompasses regions primarily in eastern and central China, including Beijing, Tianjin, Hebei, Henan, Shandong, Shanxi, Shanghai, Sichuan, Chongqing, Hunan, Hubei, Anhui, Jiangsu, and Shaanxi. Compared to 2008, the ellipse in 2021 has shifted southwestward and decreased in size. In 2021, the centripetal force of the spatial distribution of HRH in China became increasingly evident, accompanied by a rise in the degree of dispersion. This suggests that while HRH have expanded across regions, the spatial agglomeration effect has intensified. The changes in HRH are increasingly correlated with the economic development of each region. The central positions of the spatial standard deviation ellipses for 2008 and 2021 are relatively consistent, indicating that the mean distribution across regions has remained stable, while the overall distribution pattern of HRH in China has become more stable.
Spatial distribution in the standard deviation ellipse of HRH in China in 2008 and 2021. This map was generated by ArcGIS 22.0 (https://www.esri.com/).
Model fitting
Evaluating and comparing the model fit and performance, a corrected Akaike Information Criterion (AICC) was used to select the optimal bandwidth. We evaluated the performance of the OLS, GWR, and MGWR models across four stages, with results consistently demonstrating that the MGWR model achieved the highest accuracy, as illustrated in (Table 3). In each of the four stages, the goodness-of-fit (R²) and adjusted R² values for the MGWR model exceeded those of the OLS and GWR models. The best model fit is indicating by a larger adjusted R and a smaller AIC value. Consequently, the MGWR model is deemed the most appropriate for investigating the spatial heterogeneity of factors influencing HRH in TCM.
Spatial heterogeneity analysis of influencing factors of HRH based on the MGWR model
The analysis results in 2008
In 2008, the primary factors influencing the distribution of HRH in TCM included the unemployment rate (p < 0.05), average wages (p < 0.05), education funding (p < 0.01), the number of TCM institutions (p < 0.01), and per-capita healthcare expenditure (p < 0.05). Among these factors, average wage had the most significant impact, followed by per-capita healthcare expenditure. Detailed results are presented in (Table 4). The regression coefficient for unemployment demonstrated a notable decrease from northern to southern regions, indicating a more substantial negative impact in the north compared to the south. Similarly, the regression coefficient for average wage exhibited a significant decline from northeast to southwest, suggesting a considerably stronger positive impact in the northeast relative to the southwest. The coefficient for education funding revealed a significant decrease from west to east, indicating a greater negative impact in the western regions compared to the eastern regions. Furthermore, the coefficient for the number of TCM institutions also decreased from west to east, implying that the positive impact of these institutions was much stronger in the western regions than in the eastern regions. High-value areas for the coefficient of per-capita healthcare expenditure were identified in North China and Northeast China, while low-value areas were found in Xinjiang and Tibet. This suggests that the negative impact of per-capita healthcare expenditure was more pronounced in high-value areas and less so in low-value areas. For further details, please refer to (Fig. 11).
Spatial distribution of the regression coefficients of the influential factors in the MGWR model in 2008: (A) spatial distribution of regression coefficients for unemployment rate; (B) spatial distribution of regression coefficients for average wage; (C) spatial distribution of regression coefficients for education funding; (D) spatial distribution of regression coefficients for number of TCM institution; (E) spatial distribution of regression coefficients for per-capita healthcare expenditure. Maps were generated by ArcGIS 22.0 (https://www.esri.com/).
The analysis results from 2009 to 2013
From 2009 to 2013, the number of TCM institutions was the only significant factor influencing the distribution of HRH in TCM. This finding suggests that regions with a higher density of TCM institution were more likely to see an increase in HRH. Detailed results can be found in (Table 5). Figure 12 illustrates that the coefficient for the number of TCM institutions displays a spatial distribution pattern that gradually decreases from northwest to southeast. Compared to 2008, areas of high value have shifted toward the northeast, while areas of low value have migrated toward the southwest. During this period, Xinjiang demonstrated particular sensitivity to the number of TCM institutions, whereas the eastern coastal regions, including Zhejiang, Fujian, and Guangdong, exhibited lower sensitivity, likely reflecting the relatively abundant health resources available in these areas at that time.
Spatial distribution of the regression coefficients of the influential factors in the MGWR model from 2009 to 2013: (A) spatial distribution of regression coefficients for number of TCM institutions; (B) spatial distribution of regression coefficients for per-capita healthcare expenditure. Maps were generated by ArcGIS 22.0 (https://www.esri.com/).
The analysis results from 2014 to 2018
From 2014 to 2018, average wage of healthcare personnel (p < 0.01), education funding (p < 0.1), the number of TCM institutions (p < 0.001), and per-capita healthcare expenditure (p < 0.1) significantly influenced the number of HRH in TCM (Table 6). Average wage of healthcare personnel had a significant positive impact on the number of HRH, indicating that regions with higher wages were more likely to experience an increase in HRH. High-value areas for medical wages were primarily located in the northeastern regions, including Heilongjiang, Jilin, and Liaoning, while low-value areas were found in parts of the southwest (Tibet, Yunnan, Guizhou) and South China (Guangxi, Guangdong, Hainan). This suggests that the quantity of HRH in TCM in high-value areas was more responsive to wage fluctuations, whereas low-value areas exhibited less sensitivity. Conversely, education funding had a significant negative impact on the number of HRH in TCM, indicating that higher local education funding corresponded with a less pronounced increase in HRH. The spatial distribution of education funding coefficients revealed a general pattern low east high west, with high-value areas concentrated in Xinjiang and low-value areas in Shanghai, Zhejiang, and Fujian. This indicates that the negative impact of education funding was considerably greater in high-value areas compared to low-value areas. Compared to 2008, both high-value and low-value areas saw a decrease, while the number of average-value areas increased. The coefficients for the number of TCM institutions exhibited a significant spatial pattern, gradually decreasing from northwest to southeast, consistent with the spatial pattern observed during the 2009–2013 period. The positive impact of TCM institutions was greater in the northwest than in the southeast.
The coefficients for per-capita healthcare expenditure shifted from a significant negative impact in 2008 to a significant positive impact, indicating that during this period, per-capita healthcare expenditure was aligned with the growth of HRH in TCM. However, the spatial distribution pattern of these coefficients remained consistent with that of 2008, demonstrating a significant decrease from the northeast to the southwest. This suggests that per-capita healthcare expenditure had a considerably greater positive impact in northeastern regions compared to southwestern regions, as shown in (Fig. 13).
Spatial distribution of the regression coefficients of the influential factors in the MGWR model from 2014 to 2018: (A) spatial distribution of regression coefficients for average wage of healthcare personnel; (B) spatial distribution of regression coefficients for education funding; (C) spatial distribution of regression coefficients for number of TCM institutions; (D) spatial distribution of regression coefficients for per-capita healthcare expenditure. Maps were generated by ArcGIS 22.0 (https://www.esri.com/).
The analysis results from 2019 to 2021
From 2019 to 2021, the primary factors influencing HRH in TCM remained consistent with those identified in the previous period. These factors included average wage of healthcare personnel (p < 0.05), education funding (p < 0.001), the number of TCM institutions (p < 0.001), and per-capita healthcare expenditure (p < 0.05). The specific effects of these factors are detailed in (Table 7). However, the spatial distribution of regression coefficients for these factors changed significantly compared to the previous period. High-value areas for average wage of healthcare personnel shifted from the three northeastern provinces to Xinjiang, while low-value areas transitioned to parts of the southeastern coastal regions, including Guangxi, Guangdong, Fujian, and Hainan. During this period, the positive impact of average wage of healthcare personnel on HRH was more pronounced in high-value areas. Education funding continued to exert a significant negative impact on the number of HRH in TCM, indicating that regions with higher education spending experienced less noticeable increases in HRH. The high-value areas for education funding were concentrated in the western regions, gradually decreasing towards the east. Low-value areas shifted from the eastern coastal regions of Shanghai, Zhejiang, and Fujian to the northeastern regions of Heilongjiang, Liaoning, and Jilin. Throughout this period, the number of TCM institutions continued to have a significant positive impact on the number of HRH in TCM.
The spatial distribution pattern of the coefficients for the number of TCM institutions has remained largely consistent with the previous period, with high-value areas concentrated in the western regions, particularly in Xinjiang. In contrast, low-value areas have shown a slight shift to the southwest. The coefficients for per-capita healthcare expenditure exhibit a significant positive distribution from north to south, characterized by an increase in high-value areas and a decrease in low-value areas compared to the previous period. This indicates that HRH in northern regions have become increasingly responsive to per-capita healthcare expenditure. For further details, please refer to (Fig. 14).
Spatial distribution of the regression coefficients of the influential factors in the MGWR model from 2019 to 2021: (A) spatial distribution of regression coefficients for average wage of healthcare personnel; (B) spatial distribution of regression coefficients for education funding; (C) spatial distribution of regression coefficients for number of TCM institutions; (D) spatial distribution of regression coefficients for per-capita healthcare expenditure. Maps were generated by ArcGIS 22.0 (https://www.esri.com/).
Discussion
This study utilizes provincial-level data from China spanning the years 2008 to 2021 to investigate the spatial distribution and evolutionary characteristics of HRH in TCM through longitudinally examining its spatial dynamic changes across provinces. Additionally, the study employs the MGWR model to examine the spatial-temporal heterogeneity of key factors influencing the distribution of HRH in TCM. By dissecting the spatial variations and underlying drivers of HRH distribution, it offers insights into the evolution of TCM policies in China. The study reveals that HRH in TCM across Chinese provinces has generally shown a yearly increase, with a spatial distribution exhibiting a decreasing trend from east to west. The agglomeration degree of resources is higher in the eastern and central regions, while the western regions exhibit relatively lower levels of resources. As the capital of China, Beijing consistently maintained the highest agglomeration degree of HRH in TCM throughout the study period. Overall, the distribution of HRH in TCM has stabilized, exhibiting a characteristic pattern of ‘higher in the east and lower in the west’. These findings are consistent with previous research results23,24.
Since 2008, the number of TCM practitioners per thousand population has seen significant increases across all provinces. However, the growth rate has varied by region, influenced by national policies. In this context, the Chinese government’s initiatives to strengthen public health institutions and secure funding for public health services have facilitated the equalization of basic public health services, which has provided valuable support to regions with relatively scarce human resources for health50,51,52.
Nonetheless, the analysis of agglomeration degree reveals significant disparities in HRH among provinces. Changes in the agglomeration degree of HRH in TCM reflect the overall optimization of HRH allocation in China since the 2009 healthcare reform. Literature53 suggests that the 2009 healthcare reform initiated a second phase of rapid narrowing in regional disparities in the supply of HRH. Regions such as Guizhou and Guangxi have experienced an increase in agglomeration degree due to government policies that improved local healthcare infrastructure, provided incentives for TCM practitioners to work in these regions, and enhanced access to TCM education and training. However, these regions still fluctuate between sparse and semi-sparse zones. In contrast, despite a decline in the agglomeration degree of HRH in TCM in cities such as Beijing, Tianjin, and Chongqing, these areas remain classified as dense or semi-dense areas in terms of the spatial distribution of TCM practitioners. The decline in agglomeration degree may be attributed to the outflow of human resources or rapid population growth, where the increase in health personnel has failed to meet the growing demand, ultimately leading to a reduction in the agglomeration degree of TCM practitioners54.
Kernel density and standard deviation ellipse analyses reveal that HRH in TCM is still predominantly concentrated in the North China region, particularly around Beijing and Tianjin, consistent with previous research findings23,24. This concentration reflects the “siphoning effect”, where economically developed regions attract more human resources due to better salaries, working conditions, and professional opportunities. Although some regions benefit from spillover and catch-up effects, the flow of HRH remains largely concentrated in economically more prosperous areas. The typical “siphoning effect” observed in economic development continues to exacerbate regional disparities55,56,57. Despite the significant development of TCM and the preferential resource allocation policies for central and western regions following the healthcare reform—which have increased overall resources and somewhat alleviated regional inequalities—the increase in human resources does not necessarily lead to a reduction in inequality, as evidenced in other countries58. The spatial distribution of HRH in TCM exhibits significant regional disparities, characterized by a pronounced Matthew effect59. The government should consider implementing more effective resource allocation strategies and incentive mechanisms to promote the equitable distribution and mobility of HRH nationwide. This could include targeted financial incentives, further investments in education and infrastructure in underserved regions, and policies designed to retain TCM professionals in regions with the greatest need.
This study, through a comprehensive analysis of key factors across different periods, reveals that the determinants of HRH distribution in TCM varied significantly over time, influenced by broader socio-economic and policy factors.
For example, average wage had the strongest positive impact in 2008, while unemployment rate was also identified as a significant factor affecting the distribution of HRH in TCM during this period, although it did not exert a notable influence in other stages. This phenomenon may be related to the effects of the 2008 financial crisis on China’s economy, which led to an increase in unemployment rate60. In 2008, during the global financial crisis, China experienced an economic slowdown, leading to rising unemployment. In response, the Chinese government implemented a 4-trillion-yuan economic stimulus package, primarily directed toward infrastructure and industrial investment. Although the healthcare sector was not a major beneficiary, increased public funding for basic healthcare played a role in expanding employment opportunities in public health and TCM sectors. During this period, the unemployment rate emerged as a significant factor influencing HRH distribution, as more individuals sought stable employment in healthcare professions. These findings suggest that short-term economic fluctuations, such as a financial crisis, may temporarily influence HRH distribution through employment security concerns.
Per-capita health expenditure serves as an indicator of regional financial support for the provision and development of health services, reflecting, to some extent, the quality and accessibility of medical services. Previous studies23,61 have identified a positive correlation between per-capita health expenditure and the availability of HRH. However, this study reveals that, in 2008, per-capita healthcare expenditure negatively impacted the distribution of HRH in TCM. This phenomenon may be attributed to the prevailing social perceptions and demands of that era. With the advancement of modern Western medicine, characterized by its significant effectiveness and well-defined mechanisms, Western medicine rapidly gained acceptance in China and became the mainstream medicine62. Consequently, medical resource allocation primarily prioritized modern Western medicine, with substantial investments directed toward urban hospitals, advanced medical equipment, and Western medical training programs. Additionally, the public may have exhibited a stronger preference for Western medical treatments, thereby constraining the development of TCM infrastructure and limiting workforce expansion63. This trend resulted in TCM being less accessible and, in certain regions, not fully recognized as an essential healthcare resource36.
From the analysis of the number of TCM institutions, these findings align with the above trends. Throughout the study period, in addition to economic factors, the number of TCM institutions consistently exerted a positive influence on the distribution of HRH in TCM. Regions with high aggregation coefficients of TCM institutions were primarily located in the western areas, such as Xinjiang, where TCM has played a crucial role in healthcare due to the limited availability of Western medical resources. In contrast, in the economically developed eastern coastal regions like Zhejiang and Fujian, where Western medical resources are abundant and the basic public health service system is well-established, TCM institutions had relatively less influence on HRH distribution25. The disparity suggests that, while primary healthcare institutions are crucial in less developed regions, they hold less appeal in economically advanced areas, where Western medical services dominate. In the western regions, however, cost-effectiveness and accessibility of TCM have made it an essential component of healthcare, contributing to its higher sensitivity to the number of TCM institutions, which in turn positively affects HRH distribution.
The 2009 healthcare reform marked a turning point, introducing policies aimed at strengthening primary healthcare infrastructure and explicitly incorporating TCM into the national healthcare framework64. Concurrently, the implementation of the National Basic Public Health Service Plan reinforced the role of TCM in preventive care, particularly in regions where Western medical resources were limited50. As a result, per-capita health expenditure began to exert a positive influence, with its high coefficients gradually shifting westward and exhibiting a distinct north-to-south spatial distribution pattern over time. Compared to 2008, the coefficient for the number of TCM institutions have shifted toward the northeast. These results indicates that China has made significant strides in healthcare system reform, optimizing resource allocation through health policies and medical systems.
Despite these advancements, challenges persist. An earlier study reported that, in 2018, financial allocations for TCM medical institutions constituted only 2.90% of the total funding for all medical institutions65. By 2020, TCM health resources and services still accounted for less than a quarter of those provided by Western medicine36. Furthermore, literature66 indicates that in 2021, 84.2% of the healthcare burden in Chinese hospitals was borne by public hospitals, while 15.8% was borne by private hospitals; 60% of this burden was attributed to tertiary hospitals, 34% to secondary hospitals, and only 6% to primary hospitals67. This distribution is nearly the reverse of the data observed in the United States. Therefore, the government should continue to enhance the service capacity and resource allocation of TCM medical institutions to mitigate the disparity with Western medical resources. Simultaneously, the TCM service system should be optimized to increase its coverage and accessibility within primary healthcare institutions. Moreover, coordination and collaboration between TCM and Western medicine should be strengthened to address healthcare demands and improve the overall quality of medical services.
Although prior studies68,69 have suggested that increased education funding can promote a more balanced distribution of HRH, our findings reveal a contrasting pattern in western China. Specifically, during the years 2019 and 2021, education funding was found to have a significant negative effect on the spatial distribution of HRH in TCM, with the strongest adverse impact observed in Xinjiang. This apparent inconsistency may be attributed to several underlying factors. On one hand, the effectiveness of educational investment may be insufficient: although funding has increased, it may not effectively translate into improved educational quality and talent development, it becomes difficult to significantly enhance HRH in TCM70. On the other hand, regional disparities must be acknowledged: the educational infrastructure in the western regions is relatively underdeveloped, and short-term increases in educational spending may not sufficiently address deficiencies in infrastructure and teaching staff71. Under such circumstances, the marginal effect of educational investment is low, making it difficult to attract and train a sufficient number of TCM professionals. Additionally, another challenge lies in talent migration: even if education funding increases and TCM professionals are trained in western regions, these individuals may still opt to work in the economically more prosperous eastern and central regions, resulting in limited actual growth in HRH in the west59. To address these issues, the government should concentrate on targeted investments in key aspects of TCM education, improve educational infrastructure, enhance teacher training and recruitment, implement targeted training and employment incentive mechanisms, and promote inter-regional educational cooperation and resource sharing69. Furthermore, this study found that the spatial distribution of medical wage coefficients has shifted, with high-value areas transitioning from the three northeastern provinces to Xinjiang. This change may be attributed to the Chinese government’s heightened investment in TCM healthcare in economically disadvantaged regions during the COVID-19 pandemic. Empirical results suggest that economic factors are the primary drivers of talent migration72,73.
Throughout the 21st century, the Chinese government has cultivated a supportive policy environment for the advancement of TCM64. Especially since the 18th National Congress of the Communist Party in 2012, approximately 30 policies and measures have been implemented to promote TCM. The holistic approach and comprehensive treatment methods inherent in TCM have shown significant advantages in managing chronic diseases, addressing suboptimal health conditions, and in preventive medicine74,75. Moreover, its low-cost and high-efficiency characteristics in addressing specific health issues offer a cost-effectiveness that is clearly superior to that of modern medicine76,77. TCM not only complements the limitations of modern medicine but also provides broader health coverage through holistic care and preventive healthcare. A study conducted in China revealed that an increase in proportion of 1% of TCM physicians was associated with a decrease of 5.097 excess deaths, a 17.52-day increase of life expectancy and a decrease of 0.082% of health expenses among rural residents78. China is harnessing the growth of TCM to address health inequalities and establish a nationwide network of basic healthcare services.
The COVID-19 pandemic exposed the deficiencies of global healthcare systems in their response to public health emergencies79,80. However, TCM showcased significant potential in addressing major public health crises. According to the National Health Commission of China, during the COVID-19 pandemic, TCM not only treated COVID-19 independently but also integrated with modern medicine, with 92% of confirmed cases receiving combined therapies81,82. Moreover, a systematic review confirmed the substantial efficacy of TCM during the pandemic, particularly in alleviating symptoms, reducing hospital stays, and decreasing the incidence of severe cases83. Notably, TCM had already demonstrated its effectiveness in previous public health emergencies. During outbreaks such as SARS, highly pathogenic avian influenza, hand-foot-and-mouth disease, and H1N1 influenza, TCM proved highly effective in controlling the spread of infections and alleviating patient suffering84,85. For instance, traditional TCM remedies such as Qingkailing, Shuanghuanglian, and Lianhua Qingwen capsules exhibited unique advantages in the prevention and treatment of viral infectious diseases83. The strengths of TCM are evident not only in its therapeutic effectiveness but also in its ability to enhance the resilience and flexibility of healthcare systems.
TCM emphasizes the importance of “preventing disease before it occurs” through preventive treatments and immunity enhancement to reduce the risk of infection83,86. This proactive strategy can significantly reduce the societal impact of public health crises before an outbreak occurs87. TCM not only provides treatment during the acute phase but also offers comprehensive care during the recovery phase, thereby promoting the restoration of patient health. This approach strengthens the healthcare system’s capacity to respond to ongoing public health challenges, making it more resilient and adaptable. Furthermore, TCM resources are relatively abundant and easily accessible, facilitating rapid medical support during public health emergencies and thereby enhancing the healthcare system’ ability to respond quickly and adapt effectively. While the role of traditional medicine is gaining recognition globally, significant differences exist in how such systems are integrated into national health strategies. While traditional medicine systems such as Ayurveda in India and traditional African medicine are widely practiced, they are often administered separately from mainstream healthcare88,89. In contrast, China has institutionalized TCM through national education, licensing, and integration into public health services. This systematic incorporation allows TCM to play a more proactive role in strengthening health system resilience. The Chinese experience may offer policy-relevant insights for other countries seeking to formalize traditional medicine within their healthcare frameworks.
The COVID-19 pandemic has highlighted the vulnerabilities in global healthcare systems. As the world transitions to the post-pandemic era and confronts an aging population, developing countries and rural areas in developed nations are struggling to address future public health challenges and demand for primary healthcare, against the backdrop of social and economic repercussions of the pandemic1,90. A growing number of countries are now focusing on TCM and exploring ways to integrate it into their public health policies and treatment strategies91,92. TCM has shown distinct advantages in responding to public health emergencies, providing substantial support in addressing forthcoming public health challenges. Additionally, due to its affordability and accessibility, TCM plays a critical role in managing both common and chronic diseases. Consequently, TCM holds significant potential in resource-limited countries and in efforts aimed at enhancing global health equity. The WHO has emphasized the importance of TCM in its “WHO Traditional Medicine Strategy 2002–2005” and the revised “WHO Traditional Medicine Strategy 2014–2023” advocating for the global adoption of appropriate policies to promote the development of TCM93.
The widespread application of TCM is poised to significantly influence the future distribution of global health resources. TCM provides low-cost and easily accessible preventive and therapeutic methods that can greatly enhance primary healthcare services, strengthen the resilience and flexibility of health systems, and contribute to the achievement of the WHO’s Sustainable Development Goals. This is particularly relevant in addressing health inequities in developing countries and in rural areas of developed nations. In the post-pandemic era, the integration of TCM with Western medicine, coupled with the widespread promotion of TCM treatment practices, can better safeguard global health and strengthen public health security. The comprehensive application of TCM not only has the potential to boost public health emergency response capabilities but also to improve the long-term sustainability and equity of global health systems.
Limitations
In this study, through the aforementioned analysis, we have made some important findings, nevertheless, our study still suffers from some limitations. First, due to data availability, some variables, such as the scale of TCM hospitals, work environment, and others, were not included in our analysis. Furthermore, this study only performed the research from dimensions of provincial-level cities. If more granular data, such as prefecture-level or institutional-level information, become available in the future, they could enable more detailed investigation. In particular, the application of multilevel spatial regression models would allow researchers to account for nested data structures and cross-scale influences, thereby improving the precision and policy relevance of HRH distribution analysis. Second, though the data used in this study primarily comes from provincial-level data provided by the NBS and the National Administration of TCM, some data may suffer from lag or inaccurate reporting, which could affect the accuracy of the results. Third, considering that relevant data from the government is difficult to obtain, this study employs the local government’s investment in public services, such as Education funding, as an indirect proxy variable to assess the level of government support for the healthcare system. In the future, research should incorporate more detailed fiscal expenditure data or policy text analysis to directly assess the impact of government support.
Conclusions and implications
This study represents, to the best of our knowledge, the first systematic analysis of the development and changes in TCM from the perspective of HRH. By applying a MGWR model, the study identifies pronounced spatial heterogeneity in the influence of economic, institutional, and policy factors on HRH allocation—heterogeneities that are frequently obscured in conventional modeling approaches. The use of MGWR not only improves model performance but also facilitates localized interpretations, thereby offering a methodological advancement in spatial health resource research.
Empirically, the findings demonstrate that policy-driven initiatives, particularly national healthcare reforms, have contributed to a sustained increase in HRH over time. However, the spatial distribution of these resources remains highly imbalanced, with persistent concentration in the eastern and central provinces. This enduring disparity reflects a complex interplay of structural determinants, including income levels, institutional density, education investment, and broader policy environments. Taken together, the results enhance the theoretical understanding of health resource inequalities and provide a robust empirical foundation for designing geographically tailored, equity-oriented strategies for HRH planning within the traditional medicine sector.
Based on these findings, we recommend that the government implement region-specific policies to achieve more equitable distribution of HRH and healthcare outcomes. These policies should respond to local needs and ensure the long-term sustainability of TCM resources and workforce development.
In resource-scarce western regions—where TCM plays a critical role due to the limited availability of Western medical infrastructure—central-to-local fiscal transfer mechanisms should be strengthened. The central government could introduce performance-based subsidies or earmarked grants to support local governments in expanding and retaining TCM HRH. Targeted measures may include salary top-ups, bonded scholarships linked to rural service obligations, housing allowances, and subsidized continuing education programs for both students and practitioners. Additionally, policies should focus on expanding the geographic coverage of TCM services by increasing the number of institutions and upgrading their infrastructure, particularly in rural and remote areas. To enhance primary care delivery and accessibility, vertical integration of TCM services should be institutionalized by promoting inter-hospital collaboration across provincial, county, and primary healthcare levels and establishing digital referral and supervision systems. Emerging digital health technologies—such as telemedicine and AI-assisted diagnostics—offer promising avenues for addressing HRH shortages in remote areas. Future policies should consider integrating these tools into TCM service delivery frameworks, particularly in regions where the physical deployment of healthcare professionals remains limited.
In contrast, in economically developed eastern regions, where Western medical resources are abundant, it is essential to integrate TCM into the primary healthcare system. This integration should be supported by policies that ensure the equitable distribution of TCM resources relative to the population’s needs. Collaborative training programs should be established to foster cooperation between TCM and Western medicine practitioners. Additionally, the standardization of TCM practices is necessary to ensure consistent quality across regions, which will contribute to improving the overall healthcare system. Promoting TCM-Western medicine collaboration at the primary care level will enhance the comprehensiveness of healthcare services, improve patient outcomes, and reduce inefficiencies within the healthcare system.
Though healthcare reform has made progress, TCM remains underfunded relative to Western medicine. We recommend that a ring-fenced budget line be allocated to TCM in regional health expenditure frameworks, with performance-linked funding criteria. A long-term financing model should be developed, including capital investments in infrastructure, research, and human capital, to ensure TCM’s ability to meet evolving health demands and serve as a complementary pillar in national health strategy.
While these recommendations offer a pathway to address current disparities, it is equally important to consider the conditions necessary for their successful implementation. In less-developed regions, limited fiscal capacity and administrative support may hinder the sustainability of TCM workforce investment, even with central funding. Coordination between departments and across administrative levels is often insufficient, which may reduce the effectiveness of cross-regional talent policies or digital service integration. Furthermore, despite increased training efforts, retaining qualified TCM professionals in rural areas remains difficult due to inadequate working conditions and limited career development opportunities. These issues deserve careful consideration when translating policy recommendations into practice.
In the future, as TCM assumes a more significant role in global healthcare systems, governments—particularly in resource-limited developing countries—should consider incorporating TCM into their public health policy frameworks. This integration has the potential to enhance the overall quality of healthcare services, strengthen system resilience, and promote global health equity and sustainable development. Encouraging international cooperation and exchange in TCM can facilitate the dissemination of China’s successful experiences in TCM development, thereby bolstering the capacity of the global health system to respond to challenges and enhancing its resilience, in alignment with the WHO’s Sustainable Development Goals. Actively promoting the global application of TCM can provide diverse options for prevention, treatment and rehabilitation, thereby offering effective solutions to global public health challenges.
Furthermore, given the growing international interest in incorporating traditional medicine into national health systems, the analytical framework employed in this study may offer broader applicability. In many low- and middle-income countries—such as India with Ayurveda and numerous African nations with diverse traditional healing systems—HRH for traditional medicine are similarly affected by regional disparities, insufficient public investment, and fragmented policy environments. The MGWR model, with its ability to detect variable-specific spatial heterogeneity, provides a flexible tool for examining such localized dynamics. Applying this approach across different national contexts could support comparative research and contribute to more tailored, evidence-based workforce planning in the traditional medicine sector globally.
Data availability
Citations for the data used in the study can be accessed in these official websites: http://www.natcm.gov.cn/ and https://www.stats.gov.cn/. Other data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Haakenstad, A. et al. Measuring the availability of human resources for health and its relationship to universal health coverage for 204 countries and territories from 1990 to 2019: a systematic analysis for the global burden of disease study 2019. Lancet 399 (10341), 2129–2154 (2022).
Yan, W. et al. Association between inequalities in human resources for health and all cause and cause specific mortality in 172 countries and territories, 1990–2019: observational study. BMJ 381, e073043 (2023).
Wang, H. et al. Left behind: widening disparities for males and females in US County life expectancy, 1985–2010. Popul. Health Metrics. 11 (1), 8 (2013).
World health statistics. monitoring health for the SDGs, sustainable development goals[EB/OL]. https://www.who.int/publications/i/item/9789240094703 (2024).
Liu, J. & Eggleston, K. The association between health workforce and health outcomes: A cross-country econometric study. Soc. Indic. Res. 163 (2), 609–632 (2022).
Ahmat, A. et al. The health workforce status in the WHO African region: findings of a cross-sectional study. BMJ Global Health. 7 (1), e008317 (2022).
Balogun, J. A. In The Nigerian Healthcare System: Pathway to Universal and High-Quality Health Care. A Comparative Analysis of the Health System of Nigeria and Six Selected Nations Around the World (eds Balogun, J. A.) 299–344 (Springer International Publishing, 2021).
Boniol, M. et al. The global health workforce stock and distribution in 2020 and 2030: a threat to equity and ‘universal’ health coverage? BMJ Global Health. 7 (6), e009316 (2022).
Simoens, S. & Hurst, J. The supply of physician services in OECD Countries[Z]. (2006).
Fang, L. et al. World health organization survey on the level of integration of traditional Chinese medicine in Chinese health system rehabilitation services. Integr. Med. Res. 12 (2), 100945 (2023).
Cao, Y. et al. Status and challenges of public health emergency management in China related to COVID-19. Front. Public. Health 8, 250 (2020).
Wang, L. et al. The development and reform of public health in China from 1949 to 2019. Globalization Health. 15 (1), 45 (2019).
Mucelli, A. & Spigarelli, F. Healthcare Policies and Systems in Europe and China: Comparisons and Synergies (World Scientific, 2017).
Li, Z. G. & Wei, H. A comprehensive evaluation of China’s TCM medical service system: an empirical research by integrated factor analysis and TOPSIS. Front. Public. Health. 8, 532420 (2020).
Hu, Z. COVID-19 Patients’ views and experiences of traditional chinese medicine treatment in South Africa. Alternative Ther. Health Med. 28. (2022).
Gordon, T., Booysen, F. & Mbonigaba, J. Socio-economic inequalities in the multiple dimensions of access to healthcare: the case of South Africa. BMC Public. Health 20 (1), 289 (2020).
Jiang, J. & Wang, P. Health status in a transitional society: urban-rural disparities from a dynamic perspective in China. Popul. Health Metr. 16 (1), 22 (2018).
Long, H. et al. The allocation and management of critical resources in rural China under restructuring: problems and prospects. J. Rural Stud. 47, 392–412 (2016).
Yang, D., Acharya, Y. & Liu, X. Social Health Insurance Consolidation and urban-rural Inequality in Utilization and Financial Risk Protection in China 308115200 (Social Science & Medicine, 2022).
Shan, Z. J. et al. Distribution patterns and industry planning of commonly used traditional Chinese medicinal plants in China. Plant. Divers. 44 (3), 255–261 (2022).
Zhou, M. Equity and prediction of health resource allocation of traditional Chinese medicine in China. PLoS One. 18 (8), e0290440 (2023).
Yu, H. et al. Equity analysis of Chinese physician allocation based on Gini coefficient and theil index. BMC Health Serv. Res. 21 (1), 1–8 (2021).
Yuan, L. et al. Regional disparities and influencing factors of high quality medical resources distribution in China. Int. J. Equity Health. 22 (1), 8 (2023).
Pan, J. & Shallcross, D. Geographic distribution of hospital beds throughout China: a county-level econometric analysis. Int. J. Equity Health. 15 (1), 179 (2016).
Hou, D. & Wang, X. Unveiling Spatial disparities in basic medical and health services: insights from China’s provincial analysis. BMC Health Serv. Res. 24 (1), 329 (2024).
Shabrina, Z., Buyuklieva, B. & Ng, M. K. M. Short-term rental platform in the urban tourism context: A geographically weighted regression (GWR) and a multiscale GWR (MGWR) approaches. Geographical Anal. 53 (4), 686–707 (2021).
Iyanda, A. E. et al. A retrospective cross-national examination of COVID-19 outbreak in 175 countries: a multiscale geographically weighted regression analysis. J. Infect. Public Health. 13 (10), 1438–1445 (2020).
Zaman, W. et al. Phylogenetic exploration of traditional Chinese medicinal plants: a case study on Lamiaceae (angiosperms). Pak. J. Bot. 54 (3). (2022).
Saqib, S. et al. Identifying conservation priority areas using Spatial phylogenetic approaches in West himalaya. Pak. J. Bot. 56 (3). (2024).
Saqib, S. et al. Identifying hotspots and climate drivers of alien plant species for conservation prioritization across the Pan-Himalaya. Biol. Conserv. 302, 110994 (2025).
Bai, Q. Finding flaws in the spatial distribution of health workforce and its influential factors: An empirical analysis based on Chinese provincial panel data, 2010–2019. Frontiers in Public Health.
Using spatial analysis. and GIS To Improve Planning and Resource Allocation in a Rural District of Bangladesh. BMJ Global Health.
Liu, W. et al. Influence of ecological factors on the production of active substances in the anti-cancer plant Sinopodophyllum hexandrum (Royle) T.S. Ying. PLoS One 10 (4), e0122981 (2015).
Liu, J. et al. Palynological evidence for late miocene Stepwise aridification on the Northeastern Tibetan plateau. Clim. Past. 12 (7), 1473–1484 (2016).
Li, J., Fan, G. & He, Y. Predicting the current and future distribution of three Coptis herbs in China under climate change conditions, using the maxent model and chemical analysis. Sci. Total Environ. 698, 134141 (2020).
Xu, R. et al. Trends in the disparities and equity of the distribution of traditional Chinese medicine health resources in China from 2010 to 2020. PLoS One 17 (10), e0275712 (2022).
Chen, J. et al. Ten years of China’s new healthcare reform: a longitudinal study on changes in health resources. BMC Public. Health 21, 2272 (2021).
Zhang, X. et al. Associations between measures of pediatric human resources and the under-five mortality rate: a nationwide study in China in 2014. World J. Pediatr. 17 (3), 317–325 (2021).
Lessani, M. N. & Li, Z. SGWR: similarity and geographically weighted regression. Int. J. Geogr. Inf. Sci. 38 (7), 1232–1255 (2024).
Chen, Y. Spatial autocorrelation equation based on Moran’s index. Sci. Rep. 13 (1), 19296 (2023).
Ghosh, P. & Cartone, A. A Spatio-temporal analysis of COVID‐19 outbreak in Italy. Reg. Sci. Policy Pract. 12 (6), 1047–1062 (2020).
Węglarczyk, S. Kernel density estimation and its application. ITM Web of Conferences 23, 00037 (2018).
Yuill, R. S. The standard deviational ellipse; an updated tool for Spatial description. Geogr. Annaler: Ser. B Hum. Geogr. 53 (1), 28–39 (1971).
Teunissen, P. J. G. Adjustment Theory: an introduction[M]//TU Delft OPEN Textbooks (TU Delft OPEN Textbooks, 2024).
Zdaniuk, B. Ordinary Least-Squares (OLS) Model[M]//Michalos A C. Encyclopedia of quality of life and well-being research. 4515–4517 (Springer, 2014).
Zhu, C. et al. Impacts of urbanization and landscape pattern on habitat quality using OLS and GWR models in Hangzhou, China. Ecol. Ind. 117, 106654 (2020).
Tasyurek, M., Celik, M. & RNN-GWR A geographically weighted regression approach for frequently updated data. Neurocomputing 399, 258–270 (2020).
Li, Z. & Fotheringham, A. S. Computational improvements to multi-scale geographically weighted regression. Int. J. Geogr. Inf. Sci. 34 (7), 1378–1397 (2020).
Harris, P. et al. The use of geographically weighted regression for Spatial prediction: an evaluation of models using simulated data sets. Math. Geosci. 42 (6), 657–680 (2010).
Tao, W. et al. Towards universal health coverage: lessons from 10 years of healthcare reform in China. BMJ Global Health. 5 (3), e002086 (2020).
Li, L. & Fu, H. China’s health care system reform: progress and prospects. Int. J. Health Plann. Manag. 32 (3), 240–253 (2017).
Meng, Q. & Xu, L. Monitoring and evaluating progress towards universal health coverage in China. PLoS Med. 11 (9), e1001694 (2014).
Cheng, J., Kuang, X. & Zeng, L. The impact of human resources for health on the health outcomes of Chinese people. BMC Health Serv. Res. 22 (1), 1213 (2022).
Liu, J. X. et al. Global health workforce labor market projections for 2030. Hum. Resour. Health 15 (1), 11 (2017).
Ma, Y. et al. Exploration of the role of human capital in China’s high-quality economic development and analysis of its Spatial characteristics. Sustainability 15 (5), 3900 (2023).
Wang, Y. et al. The disequilibrium in the distribution of the primary health workforce among eight economic regions and between rural and urban areas in China. Int. J. Equity Health 19 (1), 28 (2020).
Lin, X. et al. Evaluating the link between innovative human capital and regional sustainable development: empirical evidence from China. Environ. Sci. Pollut. Res. 30 (43), 97386–97403 (2023).
Kobayashi, Y. & Takaki, H. Geographic distribution of physicians in Japan. Lancet 340 (8832), 1391–1393 (1992).
Dong, E. et al. Differences in regional distribution and inequality in health-resource allocation on institutions, beds, and workforce: a longitudinal study in China. Archives Public. Health. 79 (1), 78 (2021).
Chang, S. S. et al. Impact of 2008 global economic crisis on suicide: time trend study in 54 countries. BMJ 347, f5239 (2013).
Sahoo, P. M., Rout, H. S. & Jakovljevic, M. Future health expenditure in the BRICS countries: a forecasting analysis for 2035. Globalization Health 19 (1), 1–17 (2023).
Jin, L. From mainstream to marginal? Trends in the use of Chinese medicine in China from 1991 to 2004. Soc. Sci. Med. 71 (6), 1063–1067 (2010).
Lam, T. P. & Sun, K. S. Dilemma of integration with Western medicine - views of traditional Chinese medicine practitioners in a predominant Western medical setting. Complement. Ther. Med. 21 (4), 300–305 (2013).
Wang, W. Y. et al. Current policies and measures on the development of traditional Chinese medicine in China. Pharmacol. Res. 163, 105187 (2021).
Zeng, L. et al. Equity and efficiency analysis of financial investment in traditional Chinese medicine in China. Soft Sci. Health 36 (2), 14–19 (2022).
Zhang, X. et al. Rapid Growth of Private Hospitals in China: Emerging Challenges and Opportunities To Health Sector Management 44 (The Lancet Regional Health, 2024).
National Health Commission of the People’s Republic of China. The 2022 China Health Statistics yearbook (China Union Medical University, 2022).
Dussault, G. & Franceschini, M. C. Not enough there, too many here: Understanding geographical imbalances in the distribution of the health workforce. Hum. Resour. Health. 4 (1), 12 (2006).
Frenk, J. et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet 376 (9756), 1923–1958 (2010).
Zhao, F. et al. Investing in human resources for health: the need for a paradigm shift. Bull. World Health Organ. 91 (11), 799–799A (2013).
Hu, S. et al. Identifying the uneven distribution of health and education services in China using open Geospatial data. Geogr. Sustain. 4 (2), 91–99 (2023).
Gu, H., Wang, J. & Ling, Y. Economic geography of talent migration and agglomeration in China: A dual-driver framework. China Econ. Rev. 86, 102180 (2024).
George, G., Rhodes, B. & Laptiste, C. What is the financial incentive to immigrate? An analysis of salary disparities between health workers working in the Caribbean and popular destination countries. BMC Health Serv. Res. 19 (1), 109 (2019).
Jiang, M. et al. The role of Chinese medicine in the treatment of chronic diseases in China. Planta Med. 77 (9), 873–881 (2011).
Zhang, A. et al. Future perspectives of personalized medicine in traditional Chinese medicine: A systems biology approach. Complement. Ther. Med. 20 (1), 93–99 (2012).
Chang, L. C. et al. Utilization patterns of Chinese medicine and Western medicine under the National health insurance program in Taiwan, a population-based study from 1997 to 2003. BMC Health Serv. Res. 8 (1), 170 (2008).
Xu, Q. et al. Cost-effectiveness analysis of combining traditional Chinese medicine in the treatment of hypertension: compound Apocynum tablets combined with Nifedipine sustained-release tablets vs Nifedipine sustained-release tablets alone. BMC Complement. Med. Ther. 20 (1), 330 (2020).
He, P. et al. Strengthening of traditional Chinese medicine in the health system reform: effect on health outcomes and financial protection. Evidence-Based Complement. Altern. Med. 2022 (1), 7226674 (2022).
Filip, R. et al. Global challenges to public health care systems during the COVID-19 pandemic: A review of pandemic measures and problems. J. Personalized Med. 12 (8), 1295 (2022).
Haldane, V. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat. Med. 27. (2021).
Huang, K. et al. Traditional Chinese medicine (TCM) in the treatment of COVID-19 and other vral infections: Efficacies and mechanisms. Pharmacol. Therapeut. 225107843 (2021).
Li, Q. et al. The role played by traditional Chinese medicine in preventing and treating COVID-19 in China. Front. Med. 14 (5), 681–688 (2020).
Yang, Y. et al. Traditional Chinese medicine in the treatment of patients infected with 2019-new coronavirus (SARS-CoV-2): A review and perspective. Int. J. Biol. Sci. 16 (10), 1708–1717 (2020).
Luo, Y. et al. Application of Chinese medicine in acute and critical medical conditions. Am. J. Chin. Med. 47 (06), 1223–1235 (2019).
Ma, Y. et al. Prevention and treatment of infectious diseases by traditional Chinese medicine: a commentary. APMIS 127 (5), 372–384 (2019).
An, X. et al. The direct evidence and mechanism of traditional Chinese medicine treatment of COVID-19. Biomed. Pharmacother. 137111267 (2021).
P Z, J G. Evaluation of China’s public health system response to COVID-19. J. Global Health 11. (2021).
Thyagarajan, S. Integration of Ayush within National health care systems: challenges and the way forward. J. Res. Ayurvedic Sci. 7, 59 (2023).
Ouoba, K., Fofana, S. & Semdé, R. Factors limiting traditional medicine integration into modern health systems in Africa: protocol for a systematic review of qualitative studies. Public. Health. 211, 62–65 (2022).
Hanson, K. et al. The lancet global health commission on financing primary health care: putting people at the centre. Lancet Global Health. 10 (5), e715–e772 (2022).
Kim, J. K. et al. Utilization of traditional medicine in primary health care in low- and middle-income countries: a systematic review. Health Policy Plann. 35 (8), 1070–1083 (2020).
Chung, V. C. H. et al. Traditional and complementary medicine for promoting healthy ageing in WHO Western Pacific region: policy implications from utilization patterns and current evidence. Integr. Med. Res. 10 (1), 100469 (2021).
Burton, A., Smith, M. & Falkenberg, T. Building who’s global strategy for traditional medicine. Eur. J. Integr. Med. 7 (1), 13–15 (2015).
Funding
This work was supported by the Soft Science Research Program of Zhejiang Province (2025C15011) and the Research Project of Zhejiang Chinese Medical University (2024RCZXSK05).
Author information
Authors and Affiliations
Contributions
Z.J.R and L.C.C contributed to the conception of the study and the study design and provided continual supervision. Z.S and F.Y.J contributed to the data curation and the statistical analyses. L.C.C and L.H.J contributed to the code check and the interpretation of the data. Z.J.R, Z.S and F.Y.J accessed and verified the data, wrote the initial version of the manuscript. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, J., Zhou, S., Feng, Y. et al. Spatiotemporal dynamics and driving factors of human resources for health in traditional Chinese medicine in China. Sci Rep 15, 18224 (2025). https://doi.org/10.1038/s41598-025-02615-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-02615-6