Abstract
The geroprotective effects of rapamycin in mitigating frailty and cognitive complications in the perioperative period remains unknown. Of 39 C57BL/6 mice tested, 19 were young (16 weeks), and 20 were old (80 weeks). The interventional group (10 old, 10 young) received daily oral rapamycin for 8 weeks pre-op compared to controls (10 old, 9 young). Sham laparotomy was performed at week 9. Perioperative frailty was assessed using a murine clinical frailty scale, preoperatively and at 1, 4 and 8 weeks postoperatively. Spatial memory was assessed using the Barnes maze preoperatively, and at weeks 1 and 4 post-op. Rapamycin treatment is associated with significantly less decline in postoperative clinical frailty(p < 0.05). Subgroup analysis revealed similar findings for old and young mice. The rapamycin group demonstrated improved cognitive performance at 1-week postoperatively (β 40.18, 95%C.I. 8.70–71.67, p = 0.012), but only in older mice (β 54.51, 95%C.I. 6.77–102.25, p = 0.025). In a pre-clinical animal model of anesthesia and surgery, rapamycin supplementation protected against surgery-induced frailty and short-term postoperative cognitive dysfunction.
Similar content being viewed by others
Introduction
Aging is a significant risk factor for peri- and post-operative morbidity such as delirium, physical frailty, and poor functional outcomes1,2,3,4. Indeed, older surgical patients display greater susceptibility to physical frailty, and the cognitive sequelae related to the physiological stressors of anesthesia and surgery2,5,6. Therefore, effective therapeutic targets to modify the trajectory of aging, frailty and cognitive dysfunction in the perioperative period in aged patients are needed to improve clinical outcomes in at-risk subjects.
Preclinical animal models are well poised for the investigation of the knowledge gap wherein the mitigation of perioperative complications related to aging and disease are not yet fully elucidated. Furthermore, geroprotectors are intriguing drug candidates that have not been tested in this context. Rapamycin is a mammalian target of Rapamycin (mTOR) inhibitor and a widely studied geroprotector in preclinical models of aging and disease7,8,9, promotes longevity and mitigates dysfunction in several hallmarks and pillars of aging. Indeed, previous non-surgical studies have demonstrated the protective role of rapamycin in extending lifespan, reducing frailty, and enhancing resilience to physiological stress10,11,12,13. However, current literature within the perioperative setting remains comparatively limited, with several small studies suggesting a protective effect of rapamycin on mitigating short term postoperative cognitive dysfunction7,14,15,16,17,21. Therefore, the utility of rapamycin supplementation to modify the perioperative trajectory of aging, which predisposes to at-risk subjects to physical frailty and cognitive dysfunction, warrants further exploration1.
The aim of this study was to test the effect of rapamycin given orally preoperatively for 8 weeks on perioperative clinical frailty and cognitive performance in a preclinical murine model of anesthetic and surgical intervention. Both young and old mice were studied to determine if the geroprotective effect of Rapamycin is age-specific. We hypothesized that rapamycin supplementation would be associated with improved perioperative outcomes of clinical frailty, and cognitive performance.
Methods
Animals
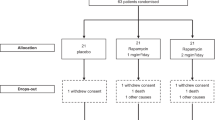
A total of 39 C57BL/6 male mice were included in the study and comprised young (n = 19, 16 weeks), and old (n = 20, 80 weeks) mice (The Jackson Laboratory, CA, USA). Mice were housed in a specific pathogen free (SPF) facility with room temperature controlled at 21–24 °C with free access to standardized food and water and a 12-h light/dark cycle. This study was approved by Institutional Animal Care and Use Committee (IACUC) of the National University of Singapore (protocol number R21-0307). All methods were performed in accordance with the relevant guidelines and regulations, and follow the ARRIVE guidelines. An overview of the study is presented in Fig. 1.
Rapamycin treatment and drug preparation
The intervention group (n = 10 young, n = 10 old mice) received daily rapamycin in their drinking water for 8 weeks preoperatively until laparotomy, while the control (n = 9 young, n = 10 old) group received vehicles (water). Rapamycin was added to the water to a final concentration of 0.08 mg/ml. As mice were expected to consume approximately 10% of body mass in water daily, a rapamycin dilution of 0.08 mg/ml was employed to achieve a target rapamycin dose of 8 mg/kg/day in accordance with previously published approaches14,15,16. This aligned with previously reported rapamycin concentrations (0.015–2.5 mg/ml), which are expected to induce significant concentration within the mice serum17,18. The amount of water drank by the mice was measured every two days, recorded and replaced with new rapamycin-containing water. The mice were weighed weekly. The treatment was conducted continuously for 8 weeks till prior to laparotomy. Assessors were blinded to the assigned treatment groups.
Anesthesia, surgery, and postsurgical care
Sham laparotomy was performed under standardized anesthesia and aseptic technique during the 9th week by blinded operators. In brief, mice were anesthetised by inhalation anaesthetic isoflurane. An approximate 2 cm incision was made on the abdomen through the skin layer and subcutaneous tissue. This was followed by wound closure with absorbable suture 4/0 with continuous suturing followed by simple interrupted skin sutures using non-absorbable 4/0 suture. Anesthesia and surgery time was standardised in both groups to be 1 h. Mice were placed in a cage for recovery from anaesthesia for 1 h, with sutures removed 2 weeks after laparotomy. Post-surgical care was received in a standardised fashion for the next 5 days, comprising daily monitoring and injections of Baytril or Carprofen for analgesia. All mice were euthanized at post-op week 8 by carbon dioxide overdose, at the end of the study.
Perioperative clinical frailty assessments
Preoperative and postoperative clinical frailty was assessed using a previously validated murine clinical frailty scale, as previously described19. In brief, the murine clinical frailty scale comprised a 31-point frailty index based on the Rockwood deficit accumulation model20, scored on multisystemic domains including integument, musculoskeletal, vestibulocochlear, ocular-nasal, digestive-urogenital, respiratory, and discomfort scores19.
Clinical frailty assessments were performed at baseline (week 0), immediately pre-operatively (at 8 weeks), 1 week post-operatively, 4 weeks post-operatively, and 8 weeks post-operatively. Clinical frailty assessments were performed by two trained assessors blinded to murine treatment status in a standardized fashion. Any disputes in clinical frailty scale assessment scores were resolved through consensus by the two assessors.
Perioperative cognitive tests of spatial memory using Barnes maze
Cognitive tests for the assessment of spatial memory was performed using the Barnes Maze in a standardized fashion at 3 timepoints: preoperatively, 1 week postoperatively, and 4 weeks postoperatively by trained assessors blinded to the treatment groups.
The Barnes Maze was employed as a cognitive test of murine spatial memory as previously described21,22. In brief, spatial cues were first located around the maze and kept constant throughout the study. On the first day of testing, the mouse was placed in the escape box for one minute, following which the animal was placed in the center of the maze inside a black chamber. As in all subsequent sessions, the chamber was removed after 10 s, whereupon a buzzer (80 dB) and a light (400 lx) were turned on, and the mouse was free to explore the maze for 3 min or until it entered the escape tunnel. The tunnel was always located underneath the same hole, which was randomly determined for each mouse. The platform was moved every day by 90° to avoid any odor cues, but the spatial cues and the tunnel position remained the same. Mice were tested once daily for 4 days. Learning was determined by a measurement of latency to the target hole on each day. On the 5th day, a probe trial was conducted to determine the long-term memory of the mice. The escape tunnel was removed, and the mouse was allowed to freely explore the maze for 3 min, where its spatial memory was assessed. Path length and error rate data were collected but not utilized for analysis. In the probe trial where the target hole was blocked, the time spent in the target quadrant and the other quadrants were scored and expressed in seconds for subsequent analysis, as an indicator of retention memory, as the primary outcome measure.
Statistical analysis
Statistical analysis was performed using Stata version 18 (StataCorp, 2023), R version 4.3.1 (R Core Team. 2023. R Foundation for Statistical Computing, Vienna, Austria) and GraphPad Prism (v 9.5). All statistical tests were conducted at a significance level of p < 0.05.
Associations of preoperative rapamycin supplementation on perioperative clinical frailty and cognitive performance were evaluated using linear mixed effects models with random intercepts and random slopes. The model adjusted for the interaction term of timing of assessment × rapamycin use. Trajectories of perioperative frailty by rapamycin use was visualized as estimated marginal means plots, alongside 95% confidence intervals. To evaluate if the effect of preoperative rapamycin on perioperative cognition and clinical frailty differed with time, regression coefficients, 95% confidence intervals and p-values derived from the interaction term of rapamycin × timing of assessmentwere reported, with time modelled as a discrete variable. Subgroup analysis stratified by murine age was performed to evaluate if the effect of preoperative rapamycin on perioperative clinical frailty and cognition was age-specific. To evaluate if there were age-specific effects of rapamycin on the outcomes, we performed additional analyses adjusted for the 3-way interaction term of age × rapamycin use × timing of assessment, which are presented in the Supplementary. The area under the curve derived from the change in frailty index scores was reported.
Results
Of 39 mice included, the intervention group comprised 10 old and 10 young mice, while the control group comprised 10 old and 9 young mice. The intervention group who received oral rapamycin treatment for 8 weeks pre-operatively and were compared to vehicle controls. No significant differences were found in the total amount of rapamycin consumed by the young mice (9.97 ± 1.26 mg/kg/day) and old mice (9.55 ± 1.84 mg/kg/day, p = 0.72). No significant differences were found in the volume of water consumed between the rapamycin (121.93±18.43 ml/kg/day) and control groups (35.57±41.86 ml/kg/day, p = 0.42). There was no mortality during the study period for both aged and young mice.
Effect of rapamycin treatment on perioperative clinical frailty
Perioperative clinical frailty was assessed using the murine clinical frailty scale comprising a 31-point frailty index based on the Rockwood deficit accumulation model20 and scored on multisystemic domains19.
The association between rapamycin administration and perioperative clinical frailty scores are presented in Table 1. Trajectories of perioperative clinical frailty by rapamycin use for all mice, and then with stratification by age are presented as estimated marginal means plots and standard errors derived from linear mixed effects models with random slopes and random intercepts, adjusted for the interaction term of time × rapamycin use (Fig. 2A–C). When compared with controls, preoperative rapamycin treatment was associated with significantly less decline in clinical frailty at postoperative week 1 (β −1.10, 95% C.I. −1.65, −0.55, p < 0.001), postoperative week 4 (β −1.29, 95% C.I. −1.85, −0.74, p < 0.001), and postoperative week 8 (β −1.31, 95% C.I. −2.03, −0.59, p < 0.001, Table 1). The rapamycin group (AUC 0.079) additionally demonstrated a four-fold decrease in AUC as compared with the control group (AUC 0.025).
On subgroup analysis by age, preoperative rapamycin treatment was associated with improved clinical frailty scores at all postoperative timepoints within the older mice (p < 0.05, Table 1; Fig. 2B). Within the young mice, rapamycin was associated with improved clinical frailty scores at postoperative week 1 and 4 (Table 1; Fig. 2C). The protective effect of rapamycin on clinical frailty was larger in older mice (AUC-difference 0.166) than younger mice (AUC-difference 0.017). Sensitivity analysis performed adjusted for the 3-way interaction term of age × rapamycin × timing of assessment are presented in Supplementary Table 1. Sensitivity analysis demonstrated statistically significant interactions of age at preoperative week 1 (β −1.69, 95% C.I. −2.66, −0.73 p = 0.001), postoperative week 4 (β −1.93, 95% C.I. −2.91, −0.96, p < 0.001) and postoperative week 8 (β −2.20, 95% C.I. −3.47, −0.94, p = 0.001, Supplemental Table S1).
Effect of rapamycin on perioperative cognition (Barnes maze)
Associations of rapamycin supplementation with perioperative cognitive performance in tests of spatial memory (Barnes maze) are presented in Table 2.
Estimated marginal means plots derived from linear mixed effects models with random slopes and random intercepts, adjusted for the interaction term of rapamycin × time are presented in Fig. 3A–C. The rapamycin group was found to have improved cognitive performance at week 1 postoperatively (β 40.18, 95% C.I. 8.70–71.67, p = 0.012). Upon stratification by age, rapamycin treatment was found to significantly improve postoperative cognitive performance at week 1 postoperatively in the old mice (β 54.51, 95% C.I. 6.77–102.25, p = 0.025), but not in young mice (β 23.24, 95% C.I. −16.87, 63.36, p = 0.256). At postoperative week 4, the control group had returned to baseline cognitive function, and there was no difference between the rapamycin and control groups across both subgroups of age (all p > 0.05). Sensitivity analysis performed adjusted for the 3-way interaction term of age × rapamycin × timing of assessment are presented in Supplementary Tables 2 and did not yield statistically significant interactions at postoperative 1 week (β 31.27, 95% C.I. −31.60, 94.14, p = 0.330) or postoperative week 4 (12.92, −48.10, 73.95, p = 0.678).
Discussion
Preoperative rapamycin supplementation was associated with an improved trajectory of perioperative clinical frailty in young and old mice, with larger effects observed in the more susceptible, older cohort. Rapamycin also suppressed short-term deficits in postoperative cognitive function, as assessed by Barnes maze testing. These anti-aging effects of rapamycin were the most prominent in elderly mice within the postoperative period. Taken together, our findings suggest the potential utility of preoperative rapamycin supplementation as a geroprotector, for modifying the trajectory of frailty and cognitive dysfunction in the perioperative period.
Our findings of improved perioperative frailty with rapamycin use are consistent with the current literature highlighting its role as a geroprotector, enhancing resilience through autophagy modulation, thereby improving healthspan10,23. Geroprotectors have been hypothesized to mitigate physical frailty, and enhance recovery from physiological insult through the improvement of deficits across multiple systems12,23,24,25. While studies evaluating the role of rapamycin in mitigating perioperative frailty are limited, our findings are aligned with previous studies conducted in non-surgical murine models, which have shown that rapamycin enhances resilience to physiological stress, extends lifespan, reduces frailty, and improves tissue architecture10,11,12,13. Our findings are also consistent in demonstrating a protective effect of rapamycin on the trajectory of clinical frailty. Interestingly, in the perioperative model, rapamycin mitigated the decline in frailty in both young and old mice, although the effect size was bigger in the aged mice. This suggests that its benefits may be broader than we expected and that its benefits may extend to physiologic stress imposed by anesthesia and surgery in a wider context. Our findings are, however, of particular relevance in preclinical perioperative of aging and disease, as aging increases vulnerability to the complications of anesthesia and surgery—representing an at-risk group which could benefit from targeted therapy1.
We additionally found that rapamycin supplementation suppressed short-term deficits in postoperative cognitive function at 1 week, but not at postoperative 4 weeks. Our findings are aligned with previous studies which have reported the protective effect of rapamycin against acute postoperative cognitive dysfunction in aged mouse models, assessed within 24 h to 7 days postoperatively7,14,15,16,17,21. These studies postulated that this phenomenon occurred since reducing mTOR activity led to enhanced autophagy, as well as reduced levels of alpha-synuclein and phosphorylated Tau26,27,28,29,30. Our study addresses an important knowledge gap—as preclinical studies evaluating the effect of rapamycin on postoperative cognition are comparatively limited. Our results suggest that the protective effect of preoperative rapamycin is only on short-term postoperative cognitive function, and may more selectively benefit aged disease models31,32. The observed early benefits of rapamycin may not have persisted in the longer term due to several mechanisms. The observed early cognitive benefits of rapamycin may not have persisted in the longer term due to several potential mechanisms. First, rapamycin was administered solely during the preoperative period and not continued postoperatively. Additionally, transient changes in neuroinflammation associated with anesthesia and surgery may contribute to reversible cognitive deficits, similar to those seen in delirium33. Therefore, it is plausible that the short-term benefits of rapamycin in response to acute neuroinflammatory insults and transient changes in synaptic plasticity may not be sustained without continued postoperative supplementation33,34. However, these preliminary findings should be interpreted with caution due to the small effect sizes and limited cohort size in our study. Future studies involving larger preclinical and clinical disease cohorts are necessary to validate these results. The effect of rapamycin on biomarkers of hippocampal neuroinflammation during the acute postoperative period, when cognitive deficits were attenuated, is also worthy of future study.
The protective effects of rapamycin on clinical frailty, and short-term postoperative cognition may be underpinned by several mechanisms. Firstly, rapamycin is an mTOR inhibitor, which exerts anti-aging effects through the activation of autophagy—a process by which cells recycle their proteins and organelles, allowing for the effective clearance of damaged proteins and subcellular organelles7. This could be explained by the increase in autophagic flux incurred with rapamycin-induced mTOR inhibition, leading to downstream P62 depletion, and the downregulation of P62 phosphorylation35,36,37,38. Taken together, the resultant activation of autophagy mechanisms conferred by rapamycin supplementation, a molecular hallmark underpinning biological aging, may contribute to increased physical and cognitive resilience in the perioperative period39.
Limitations
Our study has several limitations. Serial blood and tissue sampling was not performed longitudinally. Therefore, future studies are required to ascertain the temporal trajectory of autophagy-related and neuroinflammatory proteins within the perioperative period, or their correlations with the clinical phenotype (frailty or cognition) observed. Further study is also needed to determine the optimal dose, and duration of rapamycin supplementation, and whether it should be continued postoperatively, with considerations of the risks of perioperative complications related to rapamycin use. Preclinical reports have highlighted the potential for rapamycin to contribute to delayed wound healing, possibly through its anti-inflammatory effects40,41. In the clinical setting, similar observations were noted in a cohort of bladder cancer patients, reporting that rapamycin mitigated surgery induced T-cell exhaustion but increased wound site complications42. It is therefore unclear if prolonged rapamycin supplementation may predispose to complications unique to the perioperative period, which would not otherwise be encountered in non-surgical settings. Also, our study only included male mice to minimize gender-specific variations conferred by estrous cycles in female mice43. As such, rapamycin’s perioperative anti-aging effects on female mice should be studied, given that female mice may be more sensitive to the increase in lifespan mediated by rapamycin44. Nonetheless, previous studies have demonstrated rapamycin’s significant anti-aging effects in both male and female mice44,45. Lastly, the postoperative effects of rapamycin on expression of proteins reflective of mechanisms underpinning postoperative cognitive dysfunction, such as neuroinflammatory proteins (IL-6, TNF-α), amyloid, and phosphorylated-Tau isoforms should be studied at both early and late postoperative timepoints, as surrogate markers of perioperative neuropathological insult30,46,47. Nonetheless, our study demonstrates early proof-of-concept of the Gero protective effect of rapamycin in modifying the perioperative trajectory of physical frailty.
Conclusions
In a preclinical murine model undergoing anesthesia and surgery, rapamycin treatment may mitigate postoperative decline in clinical frailty decline, particularly in older mice. Rapamycin was also found to mitigate short-term postoperative cognitive decline at 1 week, however, this was not sustained in the longer term postoperatively. Further studies are required to validate these findings in preclinical and clinical perioperative models of aging and disease.
Data availability
Data utilized in the preparation of this manuscript is available from the corresponding author, upon reasonable request.
References
Schuetze, S., Manig, A., Ribes, S. & Nau, R. Aged mice show an increased mortality after anesthesia with a standard dose of ketamine/xylazine. Lab. Anim. Res. 35, 8. https://doi.org/10.1186/s42826-019-0008-y (2019).
Lin, H. S., McBride, R. L. & Hubbard, R. E. Frailty and anesthesia—risks during and post-surgery. Local. Reg. Anesth. 11, 61–73. https://doi.org/10.2147/lra.S142996 (2018).
Ou-Young, J. et al. Identifying risk factors for poor multidimensional recovery after major surgery: a systematic review. Acta Anaesthesiol. Scand. 67, 1294–1305. https://doi.org/10.1111/aas.14302 (2023).
An, Z. et al. Analysis of risk factors for postoperative delirium in middle-aged and elderly fracture patients in the perioperative period. Sci. Rep. 13, 13019. https://doi.org/10.1038/s41598-023-40090-z (2023).
Schulte, P. J. et al. Association between exposure to anaesthesia and surgery and long-term cognitive trajectories in older adults: report from the Mayo clinic study of aging. Br. J. Anaesth. 121, 398–405. https://doi.org/10.1016/j.bja.2018.05.060 (2018).
Jin, Z., Rismany, J., Gidicsin, C. & Bergese, S. D. Frailty: the perioperative and anesthesia challenges of an emerging pandemic. J. Anesth. 37, 624–640. https://doi.org/10.1007/s00540-023-03206-3 (2023).
Mannick, J. B. & Lamming, D. W. Targeting the biology of aging with mTOR inhibitors. Nat. Aging. 3, 642–660. https://doi.org/10.1038/s43587-023-00416-y (2023).
Lee, D. J. W., Kuerec, H., Maier, A. B. & A. & Targeting ageing with rapamycin and its derivatives in humans: a systematic review. Lancet Healthy Longev. 5, e152–e162. https://doi.org/10.1016/s2666-7568(23)00258-1 (2024).
Wong, M. Mammalian target of rapamycin (mTOR) pathways in neurological diseases. Biomed. J. 36, 40–50. https://doi.org/10.4103/2319-4170.110365 (2013).
Trendelenburg, A. U. et al. A role in the treatment of frailty. Mech. Ageing Dev. 180, 11–20. https://doi.org/10.1016/j.mad.2019.03.002 (2019).
Correia-Melo, C. et al. Rapamycin improves healthspan but not inflammaging in nfκb1(-/-) mice. Aging Cell. 18, e12882. https://doi.org/10.1111/acel.12882 (2019).
Phillips, E. J. & Simons, M. J. P. Rapamycin not dietary restriction improves resilience against pathogens: a meta-analysis. Geroscience 45, 1263–1270. https://doi.org/10.1007/s11357-022-00691-4 (2023).
Jiang, Z., He, Q., Wezeman, J., Darvas, M. & Ladiges, W. A cocktail of rapamycin, acarbose, and phenylbutyrate prevents age-related cognitive decline in mice by targeting multiple aging pathways. GeroScience https://doi.org/10.1007/s11357-024-01198-w (2024).
Kaeberlein, M. Rapamycin and ageing: when, for how long, and how much? J. Genet. Genomics. 41, 459–463. https://doi.org/10.1016/j.jgg.2014.06.009 (2014).
Selvarani, R., Mohammed, S. & Richardson, A. Effect of rapamycin on aging and age-related diseases-past and future. Geroscience 43, 1135–1158. https://doi.org/10.1007/s11357-020-00274-1 (2021).
Bishu, K. et al. Anti-remodeling effects of rapamycin in experimental heart failure: dose response and interaction with angiotensin receptor blockade. PLoS One. 8, e81325. https://doi.org/10.1371/journal.pone.0081325 (2013).
Del Grosso, A. et al. Chronic rapamycin administration via drinking water mitigates the pathological phenotype in a Krabbe disease mouse model through autophagy activation. Biomed. Pharmacother. 173, 116351. https://doi.org/10.1016/j.biopha.2024.116351 (2024).
Houssaini, A. et al. mTOR pathway activation drives lung cell senescence and emphysema. JCI Insight. 3 https://doi.org/10.1172/jci.insight.93203 (2018).
Whitehead, J. C. et al. A clinical frailty index in aging mice: comparisons with frailty index data in humans. J. Gerontol. Biol. Sci. Med. Sci. 69, 621–632. https://doi.org/10.1093/gerona/glt136 (2014).
Jones, D. M., Song, X. & Rockwood, K. Operationalizing a frailty index from a standardized comprehensive geriatric assessment. J. Am. Geriatr. Soc. 52, 1929–1933. https://doi.org/10.1111/j.1532-5415.2004.52521.x (2004).
Bach, M. E., Hawkins, R. D., Osman, M., Kandel, E. R. & Mayford, M. Impairment of spatial but not contextual memory in camkii mutant mice with a selective loss of hippocampal LTP in the range of the theta frequency. Cell 81, 905–915. https://doi.org/10.1016/0092-8674(95)90010-1 (1995).
Li, X. et al. Cognitive dysfunction precedes the onset of motor symptoms in the mitopark mouse model of Parkinson’s disease. PLoS One. 8, e71341. https://doi.org/10.1371/journal.pone.0071341 (2013).
Bellantuono, I. Find drugs that delay many diseases of old age. Nature 554, 293–295. https://doi.org/10.1038/d41586-018-01668-0 (2018).
Jeon, O. H. et al. Local clearance of senescent cells attenuates the development of post-traumatic osteoarthritis and creates a pro-regenerative environment. Nat. Med. 23, 775–781. https://doi.org/10.1038/nm.4324 (2017).
Riera, C. E. & Dillin, A. Can aging be ‘drugged’? Nat. Med. 21, 1400–1405. https://doi.org/10.1038/nm.4005 (2015).
Yuan, H. et al. Melatonin and rapamycin attenuate isoflurane-induced cognitive impairment through Inhibition of neuroinflammation by suppressing the mTOR signaling in the hippocampus of aged mice. Front. Aging Neurosci. 11, 314. https://doi.org/10.3389/fnagi.2019.00314 (2019).
Gao, S. et al. Role of mTOR-regulated autophagy in synaptic plasticity related proteins downregulation and the reference memory deficits induced by anesthesia/surgery in aged mice. Front. Aging Neurosci. 13, 628541. https://doi.org/10.3389/fnagi.2021.628541 (2021).
Chen, X. et al. mTOR-mediated autophagy in the hippocampus is involved in perioperative neurocognitive disorders in diabetic rats. CNS Neurosci. Ther. 28, 540–553. https://doi.org/10.1111/cns.13762 (2022).
Zhang, X., Zhou, Y., Xu, M. & Chen, G. Autophagy is involved in the sevoflurane anesthesia-induced cognitive dysfunction of aged rats. PLoS One. 11, e0153505. https://doi.org/10.1371/journal.pone.0153505 (2016).
Yang, N. et al. Autophagy prevents hippocampal α-synuclein oligomerization and early cognitive dysfunction after anesthesia/surgery in aged rats. Aging (Albany NY). 12, 7262–7281. https://doi.org/10.18632/aging.103074 (2020).
Halloran, J. et al. Chronic inhibition of mammalian target of rapamycin by rapamycin modulates cognitive and non-cognitive components of behavior throughout lifespan in mice. Neuroscience 223, 102–113. https://doi.org/10.1016/j.neuroscience.2012.06.054 (2012).
Lu, J. et al. Anesthesia/surgery-induced learning and memory dysfunction by inhibiting mitophagy-mediated NLRP3 inflammasome inactivation in aged mice. Exp. Brain Res. 242, 417–427. https://doi.org/10.1007/s00221-023-06724-4 (2024).
Skelly, D. T. et al. Acute transient cognitive dysfunction and acute brain injury induced by systemic inflammation occur by dissociable IL-1-dependent mechanisms. Mol. Psychiatry. 24, 1533–1548. https://doi.org/10.1038/s41380-018-0075-8 (2019).
Chen, B. et al. Transient neuroinflammation following surgery contributes to long-lasting cognitive decline in elderly rats via dysfunction of synaptic NMDA receptor. J. Neuroinflamm.. 19, 181. https://doi.org/10.1186/s12974-022-02528-5 (2022).
J Klionsky, D. et al. Guidelines for the use and interpretation of assays for monitoring autophagy (3rd edition). Autophagy 12, 1–222. https://doi.org/10.1080/15548627.2015.1100356 (2016).
Bjørkøy, G. et al. Methods in Enzymology, Vol. 452 181–197. (Academic Press, USA, 2009).
Pankiv, S. et al. p62/SQSTM1 binds directly to Atg8/LC3 to facilitate degradation of ubiquitinated protein aggregates by autophagy. J. Biol. Chem. 282, 24131–24145. https://doi.org/10.1074/jbc.M702824200 (2007).
Ichimura, Y. et al. Phosphorylation of p62 activates the Keap1-Nrf2 pathway during selective autophagy. Mol. Cell. 51, 618–631. https://doi.org/10.1016/j.molcel.2013.08.003 (2013). https://doi.org
López-Otín, C., Blasco, M. A., Partridge, L., Serrano, M. & Kroemer, G. Hallmarks of aging: an expanding universe. Cell 186, 243–278. https://doi.org/10.1016/j.cell.2022.11.001 (2023).
Mills, R. E., Taylor, K. R., Podshivalova, K., McKay, D. B. & Jameson, J. M. Defects in skin gamma delta T cell function contribute to delayed wound repair in rapamycin-treated mice. J. Immunol. 181, 3974–3983. https://doi.org/10.4049/jimmunol.181.6.3974 (2008).
Squarize, C. H., Castilho, R. M., Bugge, T. H. & Gutkind, J. S. Accelerated wound healing by mTOR activation in genetically defined mouse models. PLoS One. 5, e10643. https://doi.org/10.1371/journal.pone.0010643 (2010).
Svatek, R. S. et al. Rapamycin prevents surgery-induced immune dysfunction in patients with bladder Cancer. Cancer Immunol. Res. 7, 466–475. https://doi.org/10.1158/2326-6066.Cir-18-0336 (2019).
Tsao, C. H., Wu, K. Y., Su, N. C., Edwards, A. & Huang, G. J. The influence of sex difference on behavior and adult hippocampal neurogenesis in C57BL/6 mice. Sci. Rep. 13, 17297. https://doi.org/10.1038/s41598-023-44360-8 (2023).
Miller, R. A. et al. Rapamycin-mediated lifespan increase in mice is dose and sex dependent and metabolically distinct from dietary restriction. Aging Cell. 13, 468–477. https://doi.org/10.1111/acel.12194 (2014).
Shindyapina, A. V. et al. Rapamycin treatment during development extends life span and health span of male mice and aphnia magna. Sci. Adv. 8, eabo5482. https://doi.org/10.1126/sciadv.abo5482 (2022).
Geng, J. et al. Associations between Alzheimer’s disease biomarkers and postoperative delirium or cognitive dysfunction: a meta-analysis and trial sequential analysis of prospective clinical trials. Eur. J. Anaesthesiol. 41, 234–244. https://doi.org/10.1097/eja.0000000000001933 (2024).
Lyra e Silva, N. M. et al. Pro-inflammatory interleukin-6 signaling links cognitive impairments and peripheral metabolic alterations in Alzheimer’s disease. Translational Psychiatry. 11, 251. https://doi.org/10.1038/s41398-021-01349-z (2021).
Author information
Authors and Affiliations
Contributions
Author contributions to this work are as follows: MAS: data acquisition, analysis, interpretation, draft, revision. JG: conception, data interpretation, revision. JHT: data analysis, interpretation. JL: data analysis, conception, data acquisition, revision. FCKT: conception, data acquisition, analysis, CL: data acquisition, ESPW: conception, interpretation, revision, WNHL: conception, STHC: interpretation, drafting, revision. ABM: interpretation, drafting, revision. BKK: revision, drafting, conception, interpretation. LKT: conception, data acquisition, analysis, interpretation, drafting, revision. All authors approve the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sim, M.A., Goh, J., Lee, J. et al. Effect of preoperative rapamycin supplementation on perioperative clinical frailty and cognitive performance in a murine model undergoing anesthesia and surgery. Sci Rep 15, 19741 (2025). https://doi.org/10.1038/s41598-025-02707-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-02707-3