Abstract
The collar of a cementless stem in total hip arthroplasty (THA) improves fixation and stability by connecting with the femoral calcar. Proper attachment is essential for reducing micromotion and preventing periprosthetic fractures of the femur. However, gaps between the femoral calcar and stem collar can occur during surgery, and it is unclear what degree of gap can be tolerated. This study evaluated 156 patients who received primary THA with the CORAIL stem. Medial and lateral gap distance were measured by frontal X-ray of the hip joint at 1 week and 1, 3, 6, 12, 24, and 36 months after THA. Clinical outcomes were assessed using Japanese Orthopaedic Association hip scores, and radiographic assessments included femoral morphology and stem subsidence. Gaps were initially observed in 55 patients, with 42 showing complete gap disappearance within 36 months. On logistic regression analysis, lateral gap distance was shown to significantly influence gap disappearance, with an optimal cut-off of 5.5 mm by receiver operating characteristic curve analysis. A smaller lateral gap was correlated with quicker closure. Our findings suggest that a lateral gap ≤ 5.5 mm allows postoperative bone remodeling to close the gap, contributing to long-term implant stability in THA using the CORAIL stem.
Similar content being viewed by others
Introduction
The cementless stem collar design provides better outcomes in total hip arthroplasty (THA). Attaching the stem collar directly to the cut calcar neck offers improved fixation, protection against subsidence, positive dispersion of vertical force into the calcar and resistance to stem rotation in relation to the femoral canal1,2,3,4. Both basic and clinical research indicate that the implementation of collared stems is associated with decreased risk of periprosthetic fracture of the femur4,5,6.
In practical surgical scenarios, however, inability to properly attach the stem collar to the cut calcar neck occasionally occurs. A recent study using finite element analysis indicated that micromotion in the contact model between the stem collar and cut calcar neck was notably reduced compared to non-contact models under both flat-surface walking and stair climbing conditions7. In such cases, the stem collar may not fulfill its essential role. Thus, precise placement of the stem collar is important to optimizing outcomes in THA.
A number of types of fully hydroxyapatite (HA)-coated stem with collar is available8,9,10. Several studies have reported the occurrence of bone remodeling in the calcar region when the stem collar is not in contact in the region of the femoral calcar8,10. This suggest that even if a gap occurs intraoperatively, post-operative bone remodeling can eliminate it and allow the collar to fulfil its role. However, the maximally acceptable gap distance between the collar of a fully HA-coated stem and the femoral calcar is unclear. Accordingly, an understanding of the distance of bone remodeling after THA will provide valuable intraoperative guidance for surgeons.
In this study, we investigated the relationship between the gap distance occurring between the calcar and collar during fully HA-coated stem insertion and subsequent bone remodeling after primary THA.
Materials and methods
Participants
We enrolled 156 consecutive patients (156 hips) who underwent primary THA with a G7® cup (Zimmer Biomet, Warsaw, IN) and CORAIL® stem (DePuy Synthes, Warsaw, IN, USA) at a single center. All operations were performed using a minimally invasive antero-lateral supine approach. The CORAIL stem is a forged titanium stem with a double-tapered geometry that is plasma-coated with 155 µm of HA. HA is also coated on the back of the stem collar. Collar length increases with stem size, namely 6 mm with sizes 8 to 11, 7 mm with sizes 12 to 15, and 9 mm with sizes 16 and above. Collar thickness is 3.5 mm for all sizes. Patients in this study all received stems sizes 8 to 12. In this study, stem size was determined based primarily on the fixation stability of the broach within the femoral canal, rather than whether the collar was seated on the femoral neck osteotomy surface. We prioritized achieving stable fixation in the canal, even if the collar did not fully contact the osteotomy surface. In some cases, such as when the femoral neck osteotomy was slightly over-resected or due to anatomical variations in the patient, a gap could occur.
For inclusion, all patients were required to be available for follow-up for 36 months after surgery, and to be ambulatory with advanced or end-stage hip osteoarthritis (HOA) or idiopathic osteonecrosis of the femoral head (ION). We excluded patients with no evidence of a gap on frontal X-ray of the hip joint one week after surgery. We also excluded patients with a history of hip surgery ipsilateral to the THA, intraoperative periprosthetic femoral fracture, subsidence of the stem by more than 2 mm, or reoperation due to aseptic loosening.
This study was approved by the Institutional Review Board of Kitasato University Hospital (Approval Number: B22-089). The study was conducted in accordance with the principles of the Declaration of Helsinki, and written informed consent was obtained from all participants.
Clinical assessment
Clinical outcomes were evaluated in accordance with the Japanese Orthopaedic Association (JOA) hip scores at 1 month before and 36 months after surgery. This scoring system consists of four elements, namely pain (0–40 points), range of motion (0–20 points), gait ability (0–20 points), and performance in activities of daily living (0–20 points), and is widely used to investigate hip joint conditions in Japan11. A higher score indicates a better condition of the post-operative hip joint.
Radiographic assessment
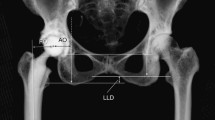
We assessed the gap between the femoral calcar and collar of the stem using postoperative frontal X-ray of the hip joint. X-rays were assessed at 1 week and 3, 6, 12, 24, and 36 months after THA. To assess gap distance between the femoral calcar and collar, medial and lateral gap distances were investigated with a 1-mm pitch at all time points (Fig. 1). Measurement of gap distance relied on an X-ray taken one week post-surgery, which served as the initial reference point. We then assessed bone remodeling-induced disappearance of the gap over 36 months post-surgery, and determined the time until complete disappearance. Cases in which the gap disappeared within 36 months were classified as the contact group, and those in which the gap did not disappear as the non-contact group. A flowchart of the study is presented in Fig. 2.
Subsidence was measured in 1-mm increments, with measurements taken from the initial postoperative radiograph as the baseline reference and reassessed at the final follow-up. Cases with subsidence up to 2 mm were included in the study, as this was considered within the acceptable range for clinical stability12. Therefore, the degree of subsidence in this study was categorized into 0, 1, and 2 mm. In this study, the term ‘gap’ refers to the remaining gap between the femoral calcar and stem collar at each follow-up interval. This gap may be influenced by both bone remodeling and subsidence.
We also evaluated the proximal femoral morphology using the Dorr classification13 by measuring the calcar width at the mid-level of the lesser trochanter and the canal width at 10 cm below the lesser trochanter, and then calculating the calcar-to-canal ratio to determine bone type. As described elsewhere, femurs with a ratio of 0–0.5 were classified as Type A, 0.51–0.75 as Type B, and 0.76–1 as Type C14,15.
We investigated whether the medial and lateral gap distances between the femoral calcar and stem collar influenced gap disappearance within 36 months post-surgery. We also calculated the cut-off values for medial and lateral gap distances at which gap disappearance due to bone remodeling could be expected, and the relationship between medial and lateral gap distances and time to gap disappearance.
Statistical analyses
The results are reported as mean ± standard error unless noted otherwise. To compare patient characteristics between the Contact and Non-contact groups, we used Pearson’s chi-square test for categorical variables, parametric t-tests for continuous variables with a normal distribution, and the Mann–Whitney U-test for variables not following a normal distribution. We employed the Mann–Whitney U test to compare lateral and medial gap sizes between the Contact and Non-contact groups at each follow-up interval (1 week, 3, 6, 12, 24, and 36 months). Logistic regression analysis was conducted to investigate the impact of medial and lateral gap distances on disappearance within 36 months post-surgery. Independent variables included age, gender, BMI, Dorr type, and medial and lateral gap distance, while the dependent variable was disappearance of the gap within 36 months. We applied receiver operating characteristic (ROC) curve analysis to determine cut-off values for the medial and lateral gaps, aiming to predict gap disappearance within the specified post-surgery timeframe. Additionally, we used Spearman’s rank correlation coefficient to assess correlations between gap distance and time to gap disappearance. Two observers independently analysed all radiographic images and resolved any disagreements through consensus. All statistical analyses were conducted with SPSS software (v.26.0; IBM, NY, USA), with statistical significance set at p < 0.05.
Results
Classification of contact and non-contact groups
In this study, gaps between the femoral calcar and collar of the stem were observed in the baseline X-rays of 55 cases. Among these, gaps disappeared within 36 months post-surgery in 42 cases (76.4%). Consequently, 42 cases were classified into the Contact group and 13 cases into the Non-contact group. The two groups did not significantly differ with regard to patient characteristics, including age, gender, BMI, clinical diagnosis, or Dorr type. Additionally, they did not differ with regard to clinical data, including pre- and postoperative JOA hip scores. Details of patient characteristic and clinical data comparisons are shown in Table 1.
Lateral and medial gap measurements at each follow-up interval
The data for lateral gap measurements are presented in Table 2, and the data for medial gap measurements are shown in Table 3. The lateral gap in the Contact group decreased from 3.0 mm [interquartile ranges (IQR) 2.0–5.0] to 0.0 mm (IQR 0.0–0.0) by 24 months, while the Non-contact group’s gap only reduced from 6.0 mm (IQR 5.0–7.0) to 3.0 mm (IQR 3.0–4.0) at 36 months. Similarly, the medial gap in the Contact group dropped from 2.0 mm (IQR 1.0–3.0) to 0.0 mm, but in the Non-contact group, it reduced from 3.0 mm (IQR 2.0–4.0) to 1.0 mm by 36 months. Mann–Whitney U tests showed significant differences at all intervals.
Factors influencing gap disappearance
The only factor influencing disappearance of the gap within 36 months post-surgery was lateral gap distance (p = 0.013, Odds ratio = 3.21). There were no significant differences in other independent variables, including age, gender, BMI, Dorr type, stem subsidence, or medial gap distance (Table 4).
ROC curve analyses for gap disappearance prediction
ROC curve analyses were conducted to determine cut-off values for the medial and lateral gap distances in predicting gap disappearance within 36 months post-surgery (Fig. 3). AUC for the lateral gap distance was found to be 0.90, indicating good predictive accuracy. Optimal cut-off value for lateral gap distance was 5.5 mm, with a sensitivity of 0.85 and specificity of 0.86. For medial gap distance, the AUC was 0.74, suggesting moderate predictive accuracy, and the optimal cut-off value was 2.5 mm, with a sensitivity of 0.69 and specificity of 0.71.
Receiver operating characteristics curve for medial and lateral gap distance at one week post-operatively in predicting gap disappearance within 36 months post-surgery. Cut-off value of the lateral gap distance for gap disappearance was 5.5 mm, with asensitivity of 0.85 and specificity of 0.86 (red line). Cut-off value of medial gap distance for gap disappearance was 2.5 mm, with sensitivity of 0.69 and specificity of 0.71 (blue line).
Correlation between gap distance and time until gap disappearance
We analyzed correlations between medial and lateral gap distances and time until gap disappearance in patients with the Contact group (Fig. 4). Spearman’s rank correlation analysis revealed a weak significant positive correlation between the lateral gap and duration to gap disappearance (ρ = 0.315, p = 0.042). The lateral gap had a median of 6.0 mm (IQR 5.0–7.0 mm), and the duration to gap disappearance had a median of 24 months (IQR 12–24 months), suggesting that larger initial gaps required longer to close. In contrast, the medial gap had a median of 3.0 mm (IQR 2.0–5.0 mm), but no significant correlation was observed between the medial gap and duration to gap disappearance (ρ = 0.249, p = 0.112).
Discussion
In this retrospective observational study, we evaluated patients who received primary THA with the CORAIL stem, focusing on the impact of gap distance between the femoral calcar and collar on gap disappearance within 36 months after surgery. Radiographic assessments at multiple post-surgery intervals revealed gaps in 55 cases, of which 42 gaps disappeared and 13 did not. The gap measurements showed significant differences between the Contact and Non-contact groups throughout the follow-up. In the Contact group, both the lateral and medial gaps steadily decreased and closed completely by 36 months. In contrast, the Non-contact group showed slower and incomplete closure over the same period, with significant differences between the groups observed at all time points. Logistic regression analysis confirmed that stem subsidence did not significantly influence gap disappearance, reaffirming that lateral gap distance was the only significant predictor. Lateral gap distance was the primary factor influencing gap disappearance, with an optimal cut-off value of 5.5 mm showing high predictive accuracy, whereas medial gap distance with a cut-off value of 2.5 mm showed moderate accuracy. A weak correlation was found between a smaller lateral gap and quicker gap disappearance, underscoring the importance of precise stem collar placement for successful bone remodeling and gap closure.
We found no difference in JOA hip score at 36 months after surgery between the two groups. Further, no participant experienced periprosthetic femoral fracture or aseptic loosening of the stem after surgery. Recent evidence also indicated that the presence or absence of contact between the collar of a fully hydroxyapatite-coated stem and the femoral neck did not affect clinical outcomes during the first postoperative year16. However, several previous studies have indicated that use of a collared stem decreases risk of periprosthetic femur fractures5,6,17. In their recent multivariate logistic analysis with adjustment for age, sex, and BMI, Rodriguez et al. reported that non-collared cementless stems were associated with an approximately threefold increased risk of periprosthetic femoral fracture compared to fully HA coated and collared cementless stems in patients aged over 65 years who underwent primary THA6. Considering that the absence of contact between the collar and femoral calcar is equivalent to the use of a collarless stem, these findings emphasize the importance of precise placement of the stem collar in optimizing outcomes in THA.
Although several studies have suggested the occurrence of bone remodeling between femoral calcar and stem collar, details have remained unclear. Vidalain reported the occurrence of bone remodeling in the calcar region with the CORAIL stem, and that on multivariate analysis femoral remodeling was not influenced to any significant extent by either patient- or prosthesis-related factors8. Our results are consistent with the findings of these studies. We revealed that the disappearance of the gap due to bone remodeling was not influenced by age, gender, BMI, Dorr type, or stem subsidence; rather, lateral gap distance was the only significant factor. These findings suggest that in clinical practice, achieving close proximity between the collar and calcar, particularly reducing the lateral gap, is crucial for facilitating postoperative bone remodeling and maintaining long-term implant stability.
Previous studies on bone remodeling in the stem collar and calcar gap did not consider gap distance8,10,18. In the present study, we found that the optimal cut-off value for lateral gap distance between the calcar and stem collar for gap disappearance was 5.5 mm (2.5 mm for medial gap distance). Additionally, we identified a positive weak correlation between lateral gap distance and time to gap disappearance. From a surgical perspective, this emphasizes the importance of minimizing the lateral gap during stem insertion, as ensuring a gap within 5.5 mm may enhance the likelihood of gap closure through postoperative bone remodeling, thereby optimizing implant stability.
Two basic studies have investigated risks associated with the femoral calcar-collar gap7,19. Watanabe et al. indicated that micromotion in the collar contact model was notably reduced compared to the non-contact model under both flat walking and stair climbing conditions7. In their study of the use of a composite femur in the CORAIL stem, Lamb et al. suggested that fracture torque and torsional stiffness were greater in the calcar-collar contact group than in the non-contact group19. They also reported that odds ratio for not achieving collar contact increased 3.8-fold for each mm of separation in the regression model19. These biomechanical findings support our clinical observations, reinforcing the significance of optimizing collar placement to reduce micromotion and improve implant stability. Given the variability in anatomical morphology, achieving complete collar-calcar contact may not always be feasible. However, our results indicate that maintaining a lateral gap within 5.5 mm allows for sufficient bone remodeling, contributing to long-term implant stability. As the collar designs of fully HA-coated stems vary in angle and size20, careful preoperative assessment and intraoperative adjustments are necessary to achieve optimal load distribution and implant longevity.
Our study has several limitations. First, different stem designs may produce different results, so our findings may not be generalizable to all fully hydroxyapatite-coated stems. Second, factors such as activity level and the duration of weight-bearing may influence subsidence outcomes, but these were not fully controlled in our study. Third, the sample size for this observational study is small, which may limit both the statistical power and the generalizability of our results. Fourth, a prospective comparative study between collared and non-collared prostheses would provide a more robust evaluation of the clinical benefits of collared stems. Lastly, a longer follow-up period is needed to better assess long-term outcomes and potential complications. Despite these limitations, we hope our results will serve as an important intraoperative indicator for surgeons using this stem.
Conclusion
This retrospective observational study evaluated the impact of gap distance between the femoral calcar and stem collar on gap disappearance within 36 months post-surgery in patients undergoing primary THA with the CORAIL stem. Our findings indicate that lateral gap distance is a significant factor influencing gap disappearance, with an optimal cut-off value of 5.5 mm.
Data availability
The datasets supporting the conclusions of this article are included within the article. The raw data can be requested from the corresponding author, YO.
References
Demey, G., Fary, C., Lustig, S., Neyret, P. & Selmi, T. Does a collar improve the immediate stability of uncemented femoral hip stems in total hip arthroplasty? A bilateral comparative cadaver study. J. Arthroplasty 26, 1549–1555. https://doi.org/10.1016/j.arth.2011.03.030 (2011).
Panichkul, P., Bavonratanavech, S., Arirachakaran, A. & Kongtharvonskul, J. Comparative outcomes between collared versus collarless and short versus long stem of direct anterior approach total hip arthroplasty: A systematic review and indirect meta-analysis. Eur. J. Orthop. Surg. Traumatol. 29, 1693–1704. https://doi.org/10.1007/s00590-019-02516-1 (2019).
Cidambi, K. R. et al. Impact of femoral stem design on failure after anterior approach total hip arthroplasty. J. Arthroplasty 33, 800–804. https://doi.org/10.1016/j.arth.2017.10.023 (2018).
Johnson, A. J. et al. A calcar collar is protective against early torsional/spiral periprosthetic femoral fracture: A paired cadaveric biomechanical analysis. J. Bone Jt. Surg. Am. 102, 1427–1433. https://doi.org/10.2106/JBJS.19.01125 (2020).
Lamb, J. N. et al. A calcar collar is protective against early periprosthetic femoral fracture around cementless femoral components in primary total hip arthroplasty: A registry study with biomechanical validation. Bone Jt. J. 101, 779–786. https://doi.org/10.1302/0301-620X.101B7.BJJ-2018-1422.R1 (2019).
Rodriguez, S. et al. How much protection does a collar provide? Assessing risk of early periprosthetic femur fractures following total hip arthroplasty in elderly patients. J. Arthroplasty 39, 997-1000.e1. https://doi.org/10.1016/j.arth.2023.10.020 (2024).
Watanabe, R., Mishima, H., Totsuka, S., Nishino, T. & Yamazaki, M. Primary stability of collared and collarless cementless femoral stems—A finite element analysis study. Arthroplast Today 21, 101140. https://doi.org/10.1016/j.artd.2023.101140 (2023).
Vidalain, J. P. Twenty-year results of the cementless Corail stem. Int. Orthop. 35, 189–194. https://doi.org/10.1007/s00264-010-1117-2 (2011).
Ohashi, Y. et al. Influence of broach surface design of a fully hydroxyapatite coated, double tapered stem on periprosthetic bone mineral density after total hip arthroplasty: A study based on the morphology of the proximal femur. Arch. Orthop. Trauma Surg. https://doi.org/10.1007/s00402-024-05430-2 (2024).
Hayashi, S. et al. Hydroxyapatite-coated compaction short stem represents a characteristic pattern of peri-prosthetic bone remodelling after total hip arthroplasty. Arch. Orthop. Trauma Surg. 142, 2903–2910. https://doi.org/10.1007/s00402-021-04140-3 (2022).
Kuribayashi, M. et al. Reliability and validity of the Japanese Orthopaedic Association hip score. J. Orthop. Sci. 15, 452–458. https://doi.org/10.1007/s00776-010-1490-0 (2010).
Ries, C., Boese, C. K., Dietrich, F., Miehlke, W. & Heisel, C. Femoral stem subsidence in cementless total hip arthroplasty: A retrospective single-centre study. Int. Orthop. 43, 307–314. https://doi.org/10.1007/s00264-018-4020-x (2019).
Dorr, L. D. et al. Structural and cellular assessment of bone quality of proximal femur. Bone 14, 231–242. https://doi.org/10.1016/8756-3282(93)90146-2 (1993).
Issa, K., Stroh, A. D., Mont, M. A. & Bonutti, P. M. Effect of bone type on clinical and radiographic outcomes of a proximally-coated cementless stem in primary total hip arthroplasties. J. Orthop. Res. 32, 1214–1220. https://doi.org/10.1002/jor.22648 (2014).
Park, C. W. et al. Femoral stem survivorship in dorr type a femurs after total hip arthroplasty using a cementless tapered wedge stem: A matched comparative study with type B femurs. J. Arthroplasty 34, 527–533. https://doi.org/10.1016/j.arth.2018.11.004 (2019).
Iwakiri, K. et al. No impact of contact between the medial collar of a hydroxyapatite-coated triple-tapered stem and the femoral neck on periprosthetic bone mineral density. J. Arthroplasty 39, 2082–2087. https://doi.org/10.1016/j.arth.2024.02.011 (2024).
Konow, T., Baetz, J., Melsheimer, O., Grimberg, A. & Morlock, M. Factors influencing periprosthetic femoral fracture risk. Bone Jt. J. 103-B, 650–658. https://doi.org/10.1302/0301-620X.103B4.BJJ-2020-1046.R2 (2021).
Jacquot, L. et al. Clinical and radiographic outcomes at 25–30 years of a hip stem fully coated with hydroxylapatite. J. Arthroplasty 33, 482–490. https://doi.org/10.1016/j.arth.2017.09.040 (2018).
Lamb, J. N., Coltart, O., Adekanmbi, I., Pandit, H. G. & Stewart, T. Calcar-collar contact during simulated periprosthetic femoral fractures increases resistance to fracture and depends on the initial separation on implantation: A composite femur in vitro study. Clin. Biomech. 87, 105411. https://doi.org/10.1016/j.clinbiomech.2021.105411 (2021).
Radaelli, M., Buchalter, D. B., Mont, M. A., Schwarzkopf, R. & Hepinstall, M. S. A new classification system for cementless femoral stems in total hip arthroplasty. J. Arthroplasty 38, 502–510. https://doi.org/10.1016/j.arth.2022.09.014 (2023).
Acknowledgements
We would like to thank Dmed for English language editing.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Study design: YoO, YuO, KF, and MasT. Data collection: YuO, MahT and HS. Data analysis: YoO, KaU and NT. Drafting manuscript: YoO, KF and KeU. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ohashi, Y., Fukushima, K., Osaki, Y. et al. Impact of stem collar to femoral calcar gap distance on postoperative bone remodeling in a fully hydroxyapatite-coated stem. Sci Rep 15, 18110 (2025). https://doi.org/10.1038/s41598-025-02970-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-02970-4