Abstract
Beals-Hecht (BH) syndrome is a rare autosomal dominant disorder caused by a mutation of the FBN-2 gene that codifies for fibrillin-2 (FBN-2). Its nosology includes congenital contractural arachnodactyly. The aim of this study was to evaluate the possible breakdown of redox homeostasis in the thoracic aortic aneurysm (TAA) from patients with BH. We determined OS markers such as malondialdehyde (MDA), total antioxidant capacity (TAC), carbonyl groups, glutathione (GSH), thiols the nitrate/nitrite ratio (NO3−/NO2−) and super oxide radical (O2–) by spectrophotometry in homogenized TAA from BH and the ascending fragment of the thoracic aorta (AFTA) from control subjects (CS). We also measured the activities of some of antioxidant enzymes such as GST, GPx, GR and TrxR. The super oxide dismutase (SOD) isoforms, catalase and peroxidase activities were evaluated by native polyacrylamide gels. The activities of the antioxidant enzymes GPx, TrxR, SOD isoforms, catalase and peroxidases were decreased in the TAA from patients with BH (p ≤ 0.04) and the OS markers NO3−/NO2−, TAC and thiols were decreased(p ≤ 0.04). In addition, O2– was increased in patients with BH (p = 0.02). The results suggest a possible loss of redox homeostasis; this loss could be due to the decrease of some of the enzymatic antioxidant system´s enzymes and some antioxidants of the non-enzymatic system. In addition, the decrease in TrxR activity and the concentration of thiol groups could contribute to the alteration and instability of the FBN-2 protein.
Similar content being viewed by others
Introduction
The Beals-Hecht (BH) syndrome is a rare pathology with an incidence of less than 1 case per 10,000 people, and it is manifested by congenital contractural arachnodactyly (CCA)1. It is an autosomal dominant disorder caused by a pathogenic variant of the fibrillin-2 (FBN-2) gene, that is located in chromosome 5q23.31. The fibrillin-2 (FBN-2) protein consists of five domains including a calcium binding site, an epidermal growth factor (cbEGF) binding site, an EGF-like structural domain, a glycine-rich region, a hybrid (hyb) domain, and an 8-cysteine repeat region2.
Fibrillins are major constituents of the extracellular matrix (ECM) and provide connective tissue elasticity and mechanical force. They help in the communication between cells through integrin receptors, and modulate the concentration, presentation, activation and bioavailability of transforming growth factor (TGFβ) and bone morphogenetic protein (BMP) complexes3. Fibrillin’s are extensively located in organs and tissues and serve as templates for the deposition of elastin during formation of elastic fibers (EF). They are essential for maintaining the integrity of tissues such as skin, blood vessels, lungs and the ocular ligament4. The nosology caused by the FBN-2 mutation in patients with BH syndrome is characterized by flexion contractures of multiple joints including elbows, knees, hips, ankles, and with long spider-like fingers, CCA, camptodactyly, contracture of major joints, scoliosis, pectus deformities and crumpled ears. Occasionally, there may exist cardiovascular signs similar to those present in Marfan syndrome (MFS) and, rarely, aortic dissection5. The mutation in the FBN-2 gene is the only one associated with CCA.
The nosology, the mutations of the FNB-2 gene in BH and the consequences present in patients who suffer from this disease have been described in the literature. However, to date, no basic research has addressed whether these patients may have oxidative stress (OS), even if this condition is present in other diseases with disrupted fibrillin’s such as MFS and Loeys-Dietz syndrome. Patients with these diseases show increased reactive oxygen species (ROS) and depletion in the antioxidant enzymatic system6,7.
On the other hand, the redox homeostasis is of vital importance to maintain the balance between ROS and the enzymatic and non-enzymatic antioxidant systems in humans. A disturbance in any of these systems causes alterations of the redox homeostasis leading to OS. OS is characterized by an increase in ROS such as super oxide anion (O2–), hydrogen peroxide (H2O2), and hydroxyl groups (OH–)8. In this sense, the disturbance of redox homeostasis could favor a chronic systemic oxidative background in patients with BH leading to a positive feedback circuit, and fibrillin instability, thus contributing to the anatomical alterations present in patients. Therefore, the objective of this preliminary study was to evaluate the possible break-down of redox homeostasis in the TAA from BH syndrome patients.
Materials and methods
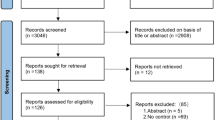
Recruitment of the BH patients and control subjects
This was an observational and comparative study. Three BH patients and six control subjects (CS) that were attended in the aorta clinic of the National Institute of Cardiology Ignacio Chávez were included. The patients were classified with BH by the Ghent criteria. The research protocol was approved by the research and ethics committee of the National Institute of Cardiology Ignacio Chávez (protocol number 23-1366). Each BH and CS patient signed an informed consent form in accordance with the Helsinki Declaration, as amended by the Congress of Tokyo, Japan9.
A segment of the ascending thoracic aorta aneurysm (TAA) was taken during the procedure of Bentall and De Bono from BH patients and stored at 4 °C10. This surgical technique consists of the replacement of the aortic valve root and ascending aorta with a Dacron tube, to which also both coronary arteries are anastomosed on the lateral faces and a valvular prosthesis10. Patients were considered candidates for surgery when they had ≥ 5 cm dilation and had been previously presented and discussed in a medical-surgical session or when they had attended the Institute for the first time with dilation and/or aortic dissection.
Inclusion criteria for BH patients included:
-
Patients who met the Ghent criteria evaluated by a rheumatology expert and that required surgical intervention of the TAA. Also, patients with another type of cardiovascular surgery such as David type 5 techniques, which was agreed upon consensus in a medical-surgical session were included.
-
Patients with and age of 18 years old or older.
-
Patients belonging to any gender.
The exclusion criteria were:
-
Patients that did not agree to sign the informed consent form.
-
Patients who did not suspend oral nitrates, NSAIDs, statins, calcium antagonist.
-
Patients with β-blocker intake for 7 days prior to obtaining the samples.
-
Patients with neoplastic disease and/or associated infection.
-
Subjects with a smoking history in the last 4 years.
-
Patients with different phenotypic variants or phenotypes related to such as Shiprintzen–Goldberg, Ehler–Danlos, Alagille, Weill–Marchesani, Turner, Noonan, Marfan, MASS, and Loeys–Dietz (all its variants) syndromes.
-
Patients with bicuspid aortic valve.
-
Patients with autosomal dominant polycystic, kidney disease.
Control subjects (CS)
The CS were 18 years old or more and were previously evaluated by a cardiologist and a rheumatologist to verify that they did not have a connective tissue disease. They met the diagnostic criteria for severe aortic valve dysfunction, and there was a recommendation to consider surgical intervention because of dilation of the ascending aorta according to the image studies. Therefore, all patients underwent an echocardiogram, CT scan, or MRI to determine valvular and aortic damage before presenting the case to the cardiac team, who ultimately decided on the most appropriate surgical technique to use, and the type of valve to be implanted for valve replacement, which could be a biological or mechanical prosthesis. Therefore, the ascending fragment of the thoracic aorta (AFTA) used was obtained from patients that did not have aortic damage and did not undergo surgery for aortic stenosis, having had no connective tissue syndrome pathology diagnosed. In these patients, there was no suspicion of inflammatory disease or the presence of a degenerative disorders such as thyroid and autoimmune diseases, hypertension or diabetes mellitus. Also, the drugs that could interfere with the outcome of the study such as NSAIDs or lipid-lowering agents, were suspended in the perioperative period. Cases were dealt cautiously, to avoid including patients undertaking treatment with allopurinol, antioxidants, or probable inhibitors of ROS production. Warfarin, aspirin, clopidogrel, anticoagulant, antiplatelet medications, and other similar drugs were suspended.
The TAA segment from patients with BH and the AFTA in CS, that were obtained during surgery were sectioned into two portions, placed in tubes and transported under Liquid nitrogen and frozen at -70 °C until study. The studies requested during hospitalization for both BH patients and CS included the determination of triglycerides (TG), HDL, LDL, total cholesterol (CT), creatinine, and glucose. All assays on serum biochemical variables were made in duplicate.
Thoracis aorta homogenization
The segment from the TAA and the AFTA of the BH and CS respectively, was homogenized under liquid nitrogen after adding KH2PO4 (2 mL) pH 7.3 in presence of 20 µL antiprotease inhibitors (1 mM PMSF, 2 µM pepstatin A, 2 µM leupeptin, and 0.1% aprotinin), and the preparation was kept in ice. The Bradford method was utilized to determine the protein concentration in the homogenates11.
Oxidative stress markers
Determination of malondialdehyde
Malondialdehyde (MDA) was read spectrophotometrically at 532 nm. A quantity of 100 µg of homogenized tissue from the TAA of BH patients and the AFTA in CS were used. Methanol with BHT at 4% (100 µL) plus KH2PO4 buffer pH 7.4 (1 mL) was added to the sample and it was then incubated at 37 °C for 30 min. Then, 2-thiobarbituric acid at 0.8 M (1.5 mL) was added. After that, the sample was incubated at 90 °C for 1 h. Then, KCL at 5% (1mL) plus n-butanol (4 mL) were added and shaken for 30 s, and the sample was centrifuged at 4000 rpm (2 min). The butanol phase was extracted, and the absorbance was measured6.
Evaluation of the total antioxidant capacity
The total antioxidant capacity (TAC) was detected spectrophotometrically at 593 nm. 100 µg of homogenized tissue from the TAA and the AFTA of the BH and CS respectively, were incubated in the presence of a mixture that contained C2H3O2 at 300 mM, FeCl3·6H2O at 20 mM, 2,4,6-tris-2pyridyl-s-triazine at 10 mM, HCL at 40 mM, at pH 3.6 (1.5 mL, at ratio of 10:1:1 v/v, ). The samples were incubated at 37 °C for 15 min and the absorbance was measured6.
Carbonylation
To evaluate the amount of carbonyl groups, 100 µg of homogenized tissue from the TAA and the AFTA of the BH and CS respectively were used. The sample was mixed with HCL 2.5 M (500 µL) and in parallel, another sample was mixed with 2,4-dinitrophenylhydrazine (500 µL) and incubated in the dark at room temperature for one hour. At the end of the incubation, C2HCL3O2 at 20% was added (500 µL) and the samples were centrifuged at 15,000× g for 5 min. The bottom was recuperated, and it was washed two time, adding C2H5OH/C4H8O2 (1 mL). Then, the samples were incubated for 10 min and centrifuged at 15,000× g for 10 min. Finally, CH6CLN3 at 6 M in KH2PO4 at 20 mM and pH 2.3 (1 mL) was added and the mixture was incubated at 37 °C for 30 min. The absorbance was read spectrophotometrically at 370 nm6.
GSH and thiols
For the GSH determination, 100 µg of homogenized tissue were used and its presence was detected spectrophotometrically at 412 nm, according to the Ellman’s method. Thiol groups were read spectrophotometrically at 415 nm. 50 µg of homogenized tissue form the cardiac valve of BH patients and CS were used according to Erel and Neselioglu’s method7.
NO3 −/NO2 − ratio determination
To evaluate the NO3−/NO2− ratio, 100 µg of homogenized tissue from the TAA and the AFTA of the BH and CS respectively, previously deproteinized with 0.5 N, NaOH and 10%, ZnSO4 (100 µL) were used. Then, 10 µL of the cytochrome c reductase (NADPH) (Sigma Aldrich Cat# 24479) were added and the samples were incubated for 30 min at 37 °C. Sulfanilamide 1% and N-naphthyl-ethyldiamine 0.1% (200 µL respectively) were added and the total volume was adjusted with distilled water to 1 mL. The absorbance was measured at 5407.
Detection of the super oxide anion
The O2– was determined in the homogenized tissue from the TAA and the AFTA of the BH and CS respectively. Briefly, 50 µg of the homogenized tissue were added to glycine buffer 2 mL (50 mM, ) at pH 10.2 plus epinephrine 50 µL (60 mM) and incubated at 30 °C for 8 min. The indirect detection of the O2– by irreversible oxidation of epinephrine to adrenochrome occurs at 1 to 5 mmol/min–1 and was monitored spactrophotometrically at 480 nm with an extinction coefficient of 4.0 mM− 1 cm− 1.in the homogenated of the TAA and the AFTA of the patients with BH and CS respectively.
Determinations of antioxidant enzymes that employ GSH as a substrate
To evaluate the activities of GST, GPx, GR and TrxR, 100 µg of homogenized tissue from the TAA and the AFTA of the BH and CS respectively, were used and treated as previously described10. The GR activity was expressed as µmol of reduced GSSG/min/mg of protein, with an extinction coefficient of 6220 M− 1 cm− 1. The GST activity was expressed as units of GS-TNB mol/min/mg of protein, with an extinction coefficient of 14,150 M− 1 cm− 1. The GPx activity was expressed as nmol of NADPH oxidized/min/mg of protein, with an extinction coefficient of 6220 M− 1 cm− 1 at 340 nm for NADPH. The samples were incubated and monitored at 340 nm for 6 min at 37 °C. The activity TrxR was determined after incubation and monitoring at 412 nm for 6 min at 37 °C. The TrxR activity was expressed as TNB nmol/min/mL of the serum, with an extinction coefficient of 13,600 M− 1 cm− 18.
Determinations of super oxide dismutase isoforms, catalase and peroxidases activities
The super oxide dismutase (SOD) isoform, catalase and peroxidase activities were determined through non-denaturing gel electrophoresis10. 100 µg of homogenized tissue from the TAA and the AFTA of the BH and CS respectively, were applied directly in non-denaturing 10% polyacrylamide gels. The electrophoresis was carried out at 120 volts for 4 h. For SOD isoform’s activity, the gel was incubated with nitro blue tetrazolium at 2.45 mM for 20 min, then incubated with buffer of the KH2PO4 at 36 mM, EDTA at 28 mM, and riboflavin at 28 mM pH 7.8 (20 mL) and exposed for 10 min to UV light. For catalase activity the gel was incubated with a mixture of 1% K3Fe (CN)6 and 1% of FeCl3 6H2O for 10 min in the dark and then washed with distilled water to stop the reaction12. Purified SOD from bovine erythrocytes with a specific activity of 112 U/mg of protein (Sigma-Aldrich, St. Louis, MO, USA) and purified CAT from a bovine liver having a specific activity of 60 U/mg (Sigma-Aldrich) were used as positive control to calculate the activity of these enzymes. For the peroxidase activity, the gel was washed with distilled water three times, for 5 min, after being incubated with 3 mg/mL 3,3,5,5-tetramethylbenzidine dissolved in CH3-OH/CH3COOH/H2O (1:1:1 v/v) with H2O2 (300 µL) total volume 20 mL, for 10 min. A quantity of 35 µL of horseradish peroxidase was loaded to a final concentration of 178.5 µg as a standard. The activities of the SOD isoforms, catalase and peroxidase gels were analyzed using densitometry with a Kodak Image® 3.5 system. The samples were placed in a separate lane of the gel and run in parallel with the biological samples. The intensity of the signal from the control lanes was used as a reference to measure the enzymatic activity in the tissue samples. Therefore, the results are expressed as U of activity per mg of protein. The gels were analyzed by densitometry with image Sigma Scan Pro 5.1 software (Systat Software, Inc., San Jose, CA, USA).
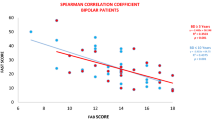
Statistical analysis
Continuous variables are expressed as median with minimum and maximum values. Categorical variables, such as frequencies and percentages, are reported. The results were normalized with a natural logarithm and the normality distribution was evaluated using the Shapiro-Wilk test. The Mann–Whitney test used according to the Gaussian distribution, was performed to detect significant independent variables The graphical results are shown as the median, first quartile, third quartile, and half dotted line. The Sigma Plot program (Systat Software Inc., SanJose, CA 95131, USA, EE. 191 UU, North First Street, Suite 360, Jandel Corporation, San Jose, CA, USA) was used for statistical analysis. The GraphPad-Prism 8 Software. Inc. (San Diego, CA, USA), 1995–2023, was used to generate the graphs. Differences were considered statistically significant when p ≤ 0.05.
Results
Table 1 describes the positive characteristics of the Ghent criteria in the three patients with the BH syndrome. The three cases included were men with an overall median age of 38 (min 30 – max 66).
Table 2 describes the clinical and symptomatic characteristics of the three patients with BH and the six control subjects.
Table 3 shows the demographic characteristics, comorbidities, serum biochemistry and general characteristics of the aorta in the three patients with BH and the six CS patients
OS markers of the non-enzymatic system are shown in (Fig. 1). In this study we determined NO3–/NO2– ratio, TAC, carbonylation, GSH and thiol groups which were decreased in patients with BH syndrome in comparison with CS (p ≤ 0.001 panel a and, p = 0.04 panel e, p = 0.01 panel f, respectively). The carbonyl groups and LPO-index were not significantly modified between groups.
Figure 2 shows that the GR, GPx and TxrR activities in the homogenized tissue from the TAA of HB patients was decreased in comparison with CS (p = 0.04 p = 0.01 and p < 0.001, panel a, b and d respectively). However, the activity of the GST did not change in BH in comparison with CS (panel c).
The activity of the SOD-1 and − 2 ware decrease (p = 0.02 and p = 0.01 Fig. 3A, b, respectively) in BH in comparison with CS (Fig. 3b).
The peroxidases and catalase activities showed a decrease in BH in comparison with CS (Fig. 4a, b, p = 0.01).
The Fig. 5 present the indirect detection of the O2– by irreversible oxidation of epinephrine to adrenochrome, showed an increase in the patients with BH in comparison to CS, *p = 0.02.
Discussion
The alteration of the redox homeostasis in the TAA from patients with MFS and in some of its variants such as the Loeys-Dietz syndrome has been previously demonstrated12,13,14. However, there is no information on the alteration of redox homeostasis linked to an increase in the oxidant background, in patients with the BH syndrome which might be associated with the FBN-2 gene mutation. Therefore, the aim of this study was to demonstrate whether there is an alteration of the redox homeostasis in patients with BH syndrome.
The clinical identification of MFS is accomplished through the Ghent criteria or genetic mapping; however, there are only clinical data that guide the physician to suspect the diagnosis of BH syndrome. In this series of cases, we were able to differentiate patients with MFS from those with BH syndrome through the scoring system proposed by Meerschaut et al.15. All three cases met the Ghent nosology and score for the diagnosis of BH and, although the gold standard test is genetic mapping, only the third case was confirmed by genetic testing of a positive FBN-2 mutation. The scoring method used allows for the classification and suspicion of the diagnosis with a sensitivity of 75% and specificity of 60%, when a genetic determination is not available15.
The overlap of several clinical conditions in MFS and BH syndromes can be explained because both conditions present mutations in two homologous genes, the FBN-1 and FBN-2, with similar functions. Nevertheless, the altered gene in MFS encodes for FBN-1 and is located chromosome 15q15-21.3 while the modified gene in patients with BH syndrome is in the 5q23-31 chromosome and encodes for FBN-215,16. Both mutations are related to skeletal, cardiovascular and aortic damage, and reports of cardiac abnormalities in BH syndrome have appeared for more than 4 decades. Mutations of both fibrillin’s have been found in a single patient and reported in the literature. This situation can synergistically worsen cardiovascular manifestations and these patients also present other comorbidities16.
In this sense, FBN-2 participates in the formation of the embryonic valve and is pointed out as a molecular factor involved in bicuspid aortic valve complexity15. The patients with BH in this series of cases also had severe dilatation of the roots of both great arteries with aortic insufficiency16.
Likewise, patients with only CCA, as in BH syndrome seem to have a favorable prognosis. Nevertheless, an association of the presence of aortic dilation and aortic dissection with some polymorphisms in the FBN-2 gene have been identified in some cases17. Timely clinical detection and imaging studies make possible the early detection of the possible aortic disease, and FBN-2 genetic testing could be useful to identify cases17.
Patients with BH have aortic root dilatation and the vast majority lack evidence of congenital heart disease. In addition, the FBN-2 gene spans more than 28 kb and 65 exons and is expressed early in development being constrained to bone and cartilage matrices. This gene is essential for the EF formation in adult tissues. Ten novel mutations have been identified in the FBN-2 protein in patients with BH, and 75% of them happen in the consensus region. Interestingly, none of these identified FBN-2 mutations alter amino acids in the calcium-binding sequence or in the EGF-like domains. The pathogenic variant causes a decrease in the amount of the FBN-2 protein available for the formation of microfibrils; hence, it reduces the EF, resulting in the symptoms exhibited in patients such as reduced strength and flexibility to the connective tissue that sustains the body’s joints and organs18. These findings have led to the search of a better understanding of the molecular basis of CCA and the mechanisms of damage that interact with the inflammatory status and oxidative dysregulation13.
On the other hand, EF assembly is a multistep process in which tropo-elastin (TE) monomers are secreted from elastogenic cells and then self-assemble/coacervate to form microaggregates that interact with fibulin-4 (Fbln) and − 5. This is a fundamental initial step for the generation of mature EF. In this process, the amino acids in TE could be susceptible to oxidative modifications and thus affect EF. Therefore, carbonyl formation by ROS on side chains of specific amino acids such as Lys, Arg, Pro, and Thr may occur, resulting in an alteration of protein structure and function. For example, oxidative modifications by O2– to collagen cause a change in the elasticity of the skin, as well as stiffer and more brittle cartilage19. The above supports the theory that each protein interaction during assembly could actively participate in the structural alteration observed in patients with aortic dilatation and dissection.
Our results only show a tendency to a decrease in the amount of carbonyl groups in the patients with BH. A possible explanation of this could be the small sample of patients studied. However, the amino acids in TE are susceptible to oxidative modifications and this may favor carbonylation which is associated with a decrease in TAC. In addition, FBN-2 contains two hyb domains composed of a TB/8-Cys-rich glycoprotein region with disulphide bridges between the Cys which are necessary for the temporal and hierarchical assembly of microfibrils that are indispensables to sequester TGFβ20. The formation of intermolecular disulphide bonds is not convenient between a conserved extra Cys in the hyb1 domain as an early part of the microfibril assembly process in cbEGF domains. This may result in reduced calcium affinity, and destabilization of the linkage of the cbEGF domain21,22,23.
The TrxR/Trx system is fundamental for the equilibrium of redox homeostasis and disulphide bond regeneration. TrxR reduces thioredoxin (Trx) through GSH oxidation in the presence of NADPH+. This results in reduction of disulfide bridges (thiol groups) between Cys. It contributes to reduce the protein dysfunction, inactivate cellular receptors, and the loss of enzyme activity24. Three TrxR isoforms (nuclear, mitochondrial and cytosolic) have been described in mammals. High and low expressions of Trx in the abdominal aorta aneurysms in the luminal and abluminal faces of arteries have been reported25. An efficient TrxR/Trx system contributes to decreases endothelial dysfunction and is associated with an anti-thrombotic and proinflammatory state. However, the alteration of the TrxR/Trx system contributes to OS resulting in disturbances in redox homeostasis7. Our results show a decrease in both the TrxR activity and in the concentration of thiol groups in the homogenized tissue from the TAA of arteries from BH patients. These results suggest that the TrxR/Trx system is highly compromised in this syndrome and might contribute to the decreased maturation of EF26. These changes could also be associated to the lack of disulphide bonds formed between TB/8-Cys-rich glycoprotein region of the FBN-227. In addition, the low TrxR activity could also contribute to OS which is favored, in part, by the increase in the ROS including H2O2.
Moreover, one of the enzymes that uses H2O2 as a substrate in the presence of GSH is GPx. Our results showed a decrease in the activity of this enzyme. This suggests that this decrease could be due to the high concentration of intracellular H2O2 (enzymatic activity inhibition by substrate)28. GPx regulates the H2O2 concentration, having a modulating effect on the TGF-β1 signaling pathways28, GPx is also capable of acting as a peroxinitrite (ONOO–) reductase. A decrease in its activity could cause the accumulation of RNS in the aortic smooth muscle cells of patients as has been described in MFS29,30. Furthermore, ONOO– affects the enzymatic activities by introducing tyrosine residues or oxidizing thiol groups thereby leading to 3-nitrotyrosine formation or formation of oxidized thiol groups in proteins. ONOO– is the result of the oxidation of the nitric oxide (NO) by O2–31. Our results show a decrease in the NO3–/NO2– ratio and this reduction could be due in part to the rapid oxidation of NO to ONOO–.
In addition, TE is susceptible to oxidative modifications by ONOO−, as is shown in an immunoblot analysis where TE is oxidized by the ONOO − and hypochlorous acid by activated monocytes and macrophages. In this sense, an in vitro study in an EF assembly model showed that oxidated modified TE failed to form EF through the cross-linking with other proteins required for EF assembly, including Fbln-4, -5, and FBN-232. This suggests that the ROS/RNS ratio can modify the TE and that these modifications may affect EF assembly. Therefore, OS influences structural and functional changes in EF under pathological conditions32. However, more studies are necessary for the confirmation of this hypothesis.
On the other hand, the tripeptide GSH inactivates ROS by itself and it is a major thiol-disulfide redox buffer and antioxidant molecule that protects from overproduction of ROS under pathological conditions33. In addition, TxrR, GPx and GST require GSH as cofactor for ROS detoxification. This detoxification reaction converts reduced GSH to oxidized GSSG34. Our results show that GSH is decrease in the TAA from BH patients, and they suggest that the increased oxidative background in patients with BH may deplete this antioxidant molecule, contributing to the loss of the activity of TrxR and GPx favoring the oxidative background.
The reduction of GSSG to GSH is catalyzed by GR. This enzyme acts as a control mechanism for the regeneration and re-establishment of the GSH concentration35,36. Our results show that the activity of GR tends to decrease in patients with BH syndrome. The non- significant tendency could be due to the small sample size. These results suggest that the chronic state of OS may favor the GSH oxidation through the loss of GR activity which may result in a decrease of the GSH regeneration37,38,39.
Regarding the isoforms of SOD, catalase and peroxidases, which are enzymes that participate in redox homeostasis, there are alterations in MFS syndrome that contribute to OS7,8. The results in this study show the presence of decrease activities in the native polyacrylamide gels of SOD-1 (the manganese isoform which predominates in the mitochondria and is very important in the muscular function to detoxicate ROS) and SOD-2, which is found in the cytoplasm (Cu-Zn isoform). Both enzymes are key in the detoxification process of O2–. The decrease in the activity of both isoforms in the patients with BH suggests that O2– contributes in an important manner to the oxidative background. It contributes to the generation of other ROS that have a longer half-life and are more aggressive in the oxidation process such as H2O2, OH– and ONOO–. In addition, the activities of the peroxidases and catalase (both responsible for detoxifying H2O2), showed a significant decrease. These results suggest that the patients with BH course with an increased oxidative background in the TAA7,8,12,13,14, and this contributes in part to instability of the FBN-2 protein and EF.
In this sense, the NADPH oxidase family in MFS is increased and it participates in the formation and progression of TAA, through the induction of inflammation, MMP activity, VSMC apoptosis and changes in ECM properties40. This oxidase family is one of the main sources of O2– production. Our results in this study showed an increase in this ROS specie in the patients with BH compared to CS. This suggests an oxidative background that is associated with the alteration of the enzymatic and non-enzymatic antioxidant system and could lead to the modification of redox homeostasis thus contributing to oxidative modifications in TE. In this sense, the oxidative modifications to TE by O2– could alter EF assembly. Modifications to the C-terminal domain of TE could affect deposition of TE aggregates into microfibrils. Removal of the C-terminal domain reduces the ability of TE to assemble into EF35.
Study limitations
Due to the fact that BH syndrome is a rare pathology where the prevalence is less than 1 in 10,000 cases, the recruitment of these patients is scarce, and it is very difficult to collect samples. This may seem a first limitation; however, this is really not so, because some of the results are clear as preliminary findings even if the number of cases is very low. Although several results did not reach a statistically significant difference, the trends are biologically relevant and important given the small “n” of cases. Furthermore, the low number of cases in this study indicates that the participation of OS is a mechanism that deserves attention for possible therapeutic targets. Therefore, since there exist no studies on this condition, and none have focused on elucidating the participation of OS or the presence of a state of the deregulation of redox homeostasis, this topic requires attention to further consider the adjuvant management of patients with antioxidant therapy in possible clinical trials. On the other hand, although the control subjects that were selected for comparison with BH patients were intervened for aortic valve replacement and were therefore not entirely healthy, they underwent the same procedures as the subjects with BH. These control subjects might present alterations in redox homeostasis; however, the point of comparison lies in the presence and absence of BH. Another study limitation was the lack of evaluation of nuclear factor erythroid 2-related factor 2-Keap1 signaling which is a master regulator of the antioxidant enzymatic system Therefore, the exploration of the participation of this system could provide interesting findings in patients with BH.
Conclusions
The results of this preliminary study in this series of three patients with BH suggest a possible loss of redox homeostasis. This loss could be due to the decrease of some enzymes of the enzymatic antioxidant system such as GPx, TrxR, SOD isoforms, peroxidases and catalase, and also to the loss of some antioxidants of the non-enzymatic system such as GSH, thiols, TAC and NO3–/NO2– ratio, associate to O2– increase. In addition, the decrease in TrxR activity and the concentration of thiol groups could contribute to the alteration and instability of the FBN-2 protein.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request and available from the María Elena Soto and Israel Pérez-Torres.
References
Li, A. L. et al. Case report: identification of novel fibrillin-2 variants impacting disulfide bond and causing congenital contractural arachnodactyly. Front. Genet. 14, 1035887 (2023).
Zhang, C. et al. A novel splice site mutation in the FBN2 gene in a Chinese family with congenital contractural arachnodactyly. Biochem. Genet. 62 (4), 2495–2503 (2024).
Smaldone, S. & Ramirez, F. Fibrillin microfibrils in bone physiology. Matrix Biol. 52–54, 191–197 (2016).
Zodanu, G. K. E. et al. High-throughput genomics identify novel FBN1/2 variants in severe neonatal Marfan syndrome and congenital heart defects. Int. J. Mol. Sci. 25 (10), 5469 (2024).
Yang, S. & Li, Z. FBN2 pathogenic variants in congenital contractural arachnodactyly with severe cardiovascular manifestations. Connect. Tissue Res. 65 (3), 214–225 (2024).
Zúñiga-Muñoz, A. M. et al. Glutathione system participation in thoracic aneurysms from patients with Marfan syndrome. Vasa 46 (3), 177–186 (2017).
Pérez-Torres, I. et al. & Guarner-Lans, V. Oxidative stress in plasma from patients with Marfan syndrome is modulated by deodorized garlic preliminary findings. Oxid. Med. Cell. Longev. 5492127 (2022).
Soto, M. E. et al. Reduced levels of selenium and thioredoxin reductase in the thoracic aorta could contribute to aneurysm formation in patients with Marfan syndrome. Int. J. Mol. Sci. 24 (13), 10429 (2023).
Ndebele, P. The declaration of Helsinki, 50 years later. JAMA 310 (20), 2145–2146 (2013).
Bentall, H. & De Bono A. A technique for complete replacement of the ascending aorta. Thorax 23 (4), 338–339 (1968).
Bradford, M. M. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal. Biochem. 72, 248–254 (1976).
Soto, M. E. et al. & Pérez-Torres, I. Analysis of oxidative stress enzymes and structural and functional proteins on human aortic tissue from different aortopathies. Oxid. Med. Cell. Longev. 760694 (2014).
Soto, M. E. et al. & Pérez-Torres, I. Oxidant/antioxidant profile in the thoracic aneurysm of patients with the Loeys-Dietz syndrome. Oxid. Med. Cell. Longev. 5392454 (2020).
Pérez-Torres, I., Roque, P., El-Hafidi, M., Diaz-Diaz, E. & Baños, G. Association of renal damage and oxidative stress in a rat model of metabolic syndrome. Influence of gender. Free Rad Res. 43 (8), 761–771 (2009).
Meerschaut, I. et al. Callewaert, B. A clinical scoring system for congenital contractural arachnodactyly. Genet. Med. 22 (1), 124–131 (2020).
Gupta, P. A. et al. Ten novel FBN2 mutations in congenital contractural arachnodactyly: delineation of the molecular pathogenesis and clinical phenotype. Hum. Mutat. 19 (1), 39–48 (2002).
Phokaew, C., Sittiwangkul, R., Suphapeetiporn, K. & Shotelersuk, V. Double heterozygous variants in FBN1 and FBN2 in a Thai woman with Marfan and beals syndromes. Eur. J. Med. Genet. 63 (9), 103982 (2020).
Rueda-Martínez, C. et al. Fibrillin 2 is upregulated in the ascending aorta of patients with bicuspid aortic valve. Eur. J. Cardiothorac. Surg. 51 (1), 104–111 (2017).
Bell, R. E. & Wheller, J. J. Cardiac defects in a patient with congenital contractural arachnodactyly. South. Med. J. 78 (6), 742–743 (1985).
Takeda, N. et al. Congenital contractural arachnodactyly complicated with aortic dilatation and dissection: case report and review of literature. Am. J. Med. Genet. A. 167A (10), 2382–2387 (2015).
Xu, P. et al. Gao. A novel splicing mutation in the FBN2 gene in a family with congenital contractural arachnodactyly. Front. Genet. 11, 143 (2020).
Deslee, G. et al. Elastin expression in very severe human COPD. Eur. Respir J. 34 (2), 324–331 (2009).
Ramirez, F. & Sakai, L. Y. Biogenesis and function of fibrillin assemblies. Cell. Tissue Res. 339 (1), 71–82 (2010).
Reinhardt, D. P., Gambee, J. E., Ono, R. N., Bachinger, H. P. & Sakai, L. Y. Initial steps in assembly of microfibrils. Formation of disulfide-cross-linked multimers containing fibrillin-1. J. Biol. Chem. 275 (3), 2205–2210 (2000).
Downing, A. K. et al. Solution structure of a pair of calcium-binding epidermal growth factor-like domains: implications for the Marfan syndrome and other genetic disorders. Cell 85 (4), 597–605 (1996).
Chupakhin, E. & Krasavin, M. Thioredoxin reductase inhibitors: updated patent review (2017–present). Expert Opin. Ther. Pat. 31 (8), 745–775 (2021).
Lu, J. & Holmgren, A. The thioredoxin antioxidant system. Free Radic Biol. Med. 66, 75–87 (2014).
Kirsch, J. et al. Endothelial dysfunction, and a prothrombotic, Proinflammatory phenotype is caused by loss of mitochondrial thioredoxin reductase in endothelium. Arterioscler. Throm Vasc Biol. 36 (9), 1891–1899 (2016).
Sakai, L. Y., Keene, D. R. & Engvall, E. Fibrillin, a new 350-kD glycoprotein, is a component of extracellular microfibrils. J. Cell. Biol. 103 (6 Pt 1), 2499–2509 (1986).
Talot, T., Conconi, M. T. & Di Liddo, R. Structural and functional failure of fibrillin-1 in human diseases (review). Int. J Mol. Med. 41 (3), 1213–1223 (2018).
Lubos, E., Loscalzo, J. & Handy, D. E. Glutathione peroxidase-1 in health and disease: from molecular mechanisms to therapeutic opportunities. Ant Red Sig. 15 (7), 1957–1997 (2011).
Soto, M. E. et al. Pérez-Torres, I. Participation of oleic acid in the formation of the aortic aneurysm in Marfan syndrome patients. Prost Other Lipid Mediat. 123, 46–55 (2016).
Bellinger, F. P., Raman, A. V., Reeves, M. A. & Berry, M. J. Regulation and function of selenoproteins in human disease. Biochem. J. 422 (1), 11–22 (2009).
Degendorfer, G. et al. Exposure of Tropoelastin to peroxynitrous acid gives high yields of nitrated tyrosine residues, di-tyrosine cross-links and altered protein structure and function. Free Radic Biol. Med. 15, 219–231 (2018).
Akhtar, K. et al. Oxidative and nitrosative modifications of Tropoelastin prevent elastic fiber assembly in vitro. J. Biol. Chem. 285 (48), 37396–37404 (2010).
Lu, S. C. Regulation of glutathione synthesis. Mol. Aspects Med. 30 (1–2), 42–59 (2009).
Deponte, M. Glutathione catalysis and the reaction mechanisms of glutathione-dependent enzymes. Biochim. Biophys. Acta. 1830 (5), 3217–3266 (2013).
Meister, A. Glutathione metabolism and its selective modification. J. Biol. Chem. 263 (33), 17205–17208 (1988).
Enns, G. M. et al. Degree of glutathione deficiency and redox imbalance depend on subtype of mitochondrial disease and clinical status. PLoS One. 9 (6), e100001 (2014).
Jiménez-Altayó, F. et al. Redox stress in Marfan syndrome: dissecting the role of the NADPH oxidase NOX4 in aortic aneurysm. Free Radic Biol. Med. 118, 44–58 (2018).
Acknowledgements
Payment of open access publication was financed by Instituto Nacional de Cardiología Ignacio Chávez.
Author information
Authors and Affiliations
Contributions
M.E.S. and I.P.-T. Conceptualization, writing, methodology.; L. M.-P. Methodology.; V. G.-L., Writing, review and editing. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics declarations
Each BH patient signed an informed consent form in accordance with the Helsinki Declaration, as amended by the Congress of Tokyo. Informed consent has been obtained from the patient(s) to publish this paper.
Institutional review board statement
The research protocol was approved by the research and ethics committee of the National Institute of Cardiology Ignacio Chávez (protocol number 23-1366).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Soto, M.E., Manzano-Pech, L., Guarner-Lans, V. et al. Possible break-down of redox homeostasis in Beals-Hecht syndrome. Sci Rep 15, 18668 (2025). https://doi.org/10.1038/s41598-025-03135-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-03135-z