Abstract
This study aimed to assess the knowledge, attitude, and practice (KAP) of caregivers managing rehabilitation for pediatric hemiplegia patients. Conducted at our hospital from January 25 to July 20, 2024, self-developed questionnaires were used to evaluate KAP scores among caregivers and compare demographic factors. Spearman correlation analysis explored relationships between variables, and structural equation modeling (SEM) examined direct effects. A total of 547 valid questionnaires were analyzed, with 71.48% female respondents and 90.86% parents of pediatric patients. The mean KAP scores were 6.63 ± 0.66 (range: 0–7), 23.50 ± 2.26 (range: 6–30), and 42.63 ± 5.32 (range: 10–50), respectively. Spearman correlation analysis revealed positive correlations between knowledge and attitude (r = 0.0889, P = 0.0377), and between attitude and practice (r = 0.5550, P < 0.001). SEM confirmed direct associations between monthly income and knowledge (path coefficient = 0.09, P = 0.002), knowledge and attitude (path coefficient = 0.28, P = 0.048), and education level and attitude (path coefficient = 0.46, P = 0.001). Additionally, attitude (path coefficient = 1.27, P < 0.001) and the dominant hand of pediatric patients (path coefficient = 1.34, P < 0.001) were directly associated with practice. Knowledge (path coefficient = 0.35, P = 0.049) and education level (path coefficient = 0.58, P = 0.001) were indirectly linked to practice. Caregivers of pediatric patients with hemiplegia displayed adequate knowledge, positive attitudes, and proactive practices in rehabilitation management. Educational interventions and support programs are suggested, especially for caregivers with lower income and education levels.
Similar content being viewed by others
Introduction
Characterized by unilateral paralysis, pediatric hemiplegia typically arises from congenital or acquired brain injuries, such as perinatal stroke, cerebral palsy, or traumatic brain injury1. Compared to children with diplegic or quadriplegic cerebral palsy, patients with pediatric hemiplegia typically exhibit unilateral motor impairments, highlighting unique functional rehabilitation healthcare2. A systematic analysis indicated that cerebral palsy, the most common cause of hemiplegia in children, affects 1.5 to 3.4 per 1,000 live births3. The pooled prevalence of cerebral palsy in China was estimated to 2.07 per 1000 population of children and adolescents4. In one study conducted in a hospital setting in Shanghai, hemiplegic cerebral palsy represented 23.4% of the total cases of cerebral palsy among children5. The neurological disorder can cause significant impairments in motor function, coordination, and muscle strength, which profoundly influences a child’s ability to perform daily activities and participate in social and educational environments6,7,8. The clinical implications of pediatric hemiplegia extend beyond physical disabilities, often including cognitive, behavioral, and emotional challenges that can persist into adulthood9.
The management of pediatric hemiplegia often requires long-term rehabilitation, in which caregivers play a pivotal role10. Caregivers, typically parents or family members, are responsible for supporting the child’s daily activities, facilitating therapy, and ensuring adherence to rehabilitation protocols. A comprehensive understanding of the nature of hemiplegia, its potential complications, and the strategies available for its management empowers caregivers to make informed decisions, seek professional support, and provide consistent therapy at home. Also, a positive attitude towards therapy can significantly enhance a caregiver’s commitment to the rehabilitation, thereby improving the child’s adherence to prescribed interventions. In addition to knowledge and attitude, caregivers’ practices in managing pediatric hemiplegia are a crucial determinant of rehabilitation success. Facilitating mobility exercises, encouraging adaptive activities, and integrating therapeutic interventions into daily routines, are essential for improving functional outcomes11,12. Caregivers who actively participate in therapy by following professional guidance, adjusting home environments, and providing emotional and physical support contribute significantly to the child’s recovery13. Furthermore, caregivers’ involvement in social support networks can enhance their ability to manage challenges, reduce stress, and maintain consistent care14. Understanding caregivers’ knowledge, attitudes, and practices (KAP) can help guide targeted educational interventions, and enhance the care provided to children with hemiplegia.
Current research has primarily focused on the clinical management of hemiplegia, with insufficient attention given to the caregiver’s role in rehabilitation15,16. KAP studies are more common in brain injuries during adulthood, such as hemiplegia17 and cerebral infarction18. Reportedly, the KAP regarding home-based care were positively associated among family caregivers of patients with cerebral infarction19. To our knowledge, only one KAP research from Saudi Arabia focused on pediatric hemiplegia20. The findings showed that the caregivers had favorable KAP scores towards cerebral palsy, but lacked understandings in handling emergency situations20. To date, no KAP studies regarding caregivers’ KAP towards pediatric hemiplegia have been available in China. The gap impedes the development of targeted interventions that can enhance caregiver engagement and improve rehabilitation effectiveness.
The study aimed to explore the KAP of caregivers responsible for the rehabilitation management of pediatric patients with hemiplegia. Moreover, the influential demographic factors of KAP were identified to inform targeted educational and support programs.
Methods
Study design and objects
This cross-sectional study was conducted at the X Institute of our hospital from January 25 to July 20, 2024. Participants included pediatric patients diagnosed with central hemiplegia at our hospital since 2016. The study received approval from the Institutional Review Board (ethics review batch number: (2024) Lun Review (Research) No. (5)), and informed consent was obtained from all participants.
Inclusion criteria: (1) Age under 18 years; (2) Diagnosis of central hemiplegia according to the criteria established by the 6th National Conference on Pediatric Rehabilitation and International Academic Exchange.
Exclusion criteria: (1) Movement disorders due to peripheral nerve injury, intracranial infection, or trauma; (2) Genetic metabolic diseases.
Sample size calculation
The calculation of sample size was based on the following formula employed in the cross-sectional study21:
where n denotes the sample size. Besides, p value was assumed to be 0.5 to achieve the maximum sample size. α refers to the type I error, which was set to 0.05 in this case. Subsequently, \({Z}_{1-\frac{\alpha}{2}}\) was yielded 1.96. \(\:\delta\:\) represents the effect sizes between groups, which was determined as 0.05, and at least 384 participants should be required. As regards the 20% of non-response rate, a total of 480 participants are required to be involved.
Questionnaire design
The questionnaire was designed following established guidelines and literature22,23,24. In the initial pre-test, 30 family caregivers of hospitalized children with central hemiplegia were recruited. A total of 28 valid questionnaires were collected. The overall Cronbach’s α coefficient was 0.807, with − 0.434 for knowledge, 0.490 for attitude, and 0.853 for practice. While the scale showed good internal consistency overall, the knowledge and attitude dimensions exhibited poor consistency. Following these findings, the questionnaire was revised, and a second round of pre-testing was conducted. This round included 30 valid questionnaires, yielding an overall Cronbach’s α coefficient of 0.745.
The final questionnaire, written in Chinese, consisted of 43 items across four dimensions. These included 18 items for basic information, 9 for knowledge, 6 for attitude, and 10 for practice. In the statistical analysis, scores were assigned based on the number of items. In the knowledge dimension (K1-K9), K1 and K9 were trap questions used to exclude invalid responses, and K2-K8 awarded 1 point for correct answers and 0 points for incorrect ones. The total score in the dimension ranged from 0 to 7 points.
In the attitude dimension, a five-point Likert scale was used. Positive attitude questions (A1-A4 and A6) were scored from 5 points for “Strongly agree” to 1 point for “Strongly disagree.” The negative attitude question (A5) was scored in reverse, from 1 point for “Strongly agree” to 5 points for “Strongly disagree”. The total score in the dimension ranged from 6 to 30 points.
The practice dimension also utilized a five-point Likert scale, with scores assigned from 5 points for “Strongly consistent” to 1 point for “Strongly inconsistent”. The total score for this dimension ranged from 10 to 50 points. A scoring threshold of > 70% was set for each dimension to define adequate knowledge, positive attitudes, and proactive practices25 (Supplementary Questionnaire).
Data collection
Caregivers of hospitalized children were invited to participate and complete the questionnaire on-site by scanning a QR code provided by the researchers. For outpatient caregivers, contact was made via phone, and the questionnaire link was sent through SMS or WeChat. To enhance participation and response rates, we emphasized the study’s purpose and its relevance to rehabilitation management. Caregivers who completed the questionnaire received personalized family rehabilitation guidance as an incentive. The questionnaire was simplified by using multiple-choice questions, making it easier and quicker to complete. To ensure data quality, each IP address was restricted to a single submission, and all items were made mandatory. The research team reviewed all completed questionnaires for accuracy, consistency, and internal coherence.
Statistical methods
Continuous variables were expressed as mean ± standard deviation (SD), while categorical variables were reported as frequencies and percentages. Comparisons between two groups were performed using Student’s t-test, and ANOVA was used for continuous variables across three or more groups. Spearman correlation analysis explored associations between KAP scores. A structural equation model (SEM) was developed to test the following hypotheses: (1) caregivers’ knowledge directly affects their attitudes towards rehabilitation management of pediatric hemiplegia; (2) caregivers’ attitudes directly influence their practices; and (3) caregivers’ knowledge directly impacts their practices. Model fit was assessed using root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR), Tucker-Lewis index (TLI), and comparative fit index (CFI). Statistical analysis was conducted using STATA 17.0 (Stata Corp LP, College Station, TX, USA) and AMOS 26.0 (IBM Corp., Armonk, NY, USA). All statistical tests were two-tailed, with a significance level set at P < 0.05.
Results
A total of 716 questionnaires were collected. Of these, 17 cases were excluded due to pre-birth hemiplegia diagnoses, and 3 cases were excluded as the patients were over 18 years old. Additionally, 151 cases with consistent responses to trap questions were removed, resulting in 547 valid cases for analysis.
The majority of respondents were female (71.48%), aged 31–40 years (54.48%), parents of pediatric patients (90.86%), living in urban areas (61.79%), and either retired or unemployed (50.46%). Furthermore, 45.16% held a bachelor’s degree or higher, and 37.84% reported a monthly income between 2,000 and 5,000 yuan. Pediatric patients had a mean age of 5.53 ± 3.42 years and an average illness duration of 2,207.63 ± 1,240.56 days. Among the patients, 51.92% had right-side hemiplegia, and 53.2% were right-handed. Only 45.16% attended school, 35.89% were accompanied by a parent or caregiver, and 11.38% required caregiver accompaniment (Table 1).
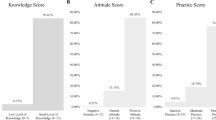
Caregivers’ knowledge, attitude, and practice scores for rehabilitation management were 6.63 ± 0.66, 23.50 ± 2.26, and 42.63 ± 5.32, respectively. Higher knowledge scores were observed among patients with urban residence (P = 0.027) and a monthly income exceeding 10,000 yuan (P = 0.006) (Table S1). Higher attitude scores were observed among urban residents (P = 0.004), caregivers with a bachelor’s degree or higher (P < 0.001), full-time or part-time employees (P = 0.006), and those with a monthly income of 5,000–10,000 yuan (P < 0.001) (Table S2). Higher practice scores were noted among right-handed pediatric patients (P = 0.004) (Table S3).
Accuracy rates in the knowledge dimension ranged from 84.10 to 99.27%. The highest accuracy (99.27%) was for the statement that physical therapy is a standard treatment for pediatric hemiplegia (K5). The lowest accuracy (84.10%) was related to caregivers’ management of sleeping positions, eating, and other daily activities, which are critical to the condition of pediatric patients (K8) (Table 2).
Positivity rates in the attitudes dimension ranged from 1.64 to 96.90%. The highest positivity rate (96.90%) was for the belief in the importance of rehabilitation management in improving pediatric patient outcomes (A2). In contrast, only 1.64% of caregivers reported not feeling anxious about the pediatric patient’s illness (A5) (Table 3).
Practice adherence rates varied between 63.44% and 93.60%. The highest adherence (93.60%) was for actively encouraging the pediatric patient during rehabilitation sessions (P9). The lowest adherence (63.44%) was for seeking support to manage negative emotions through conversations with relatives, friends, or psychologists (P10). Additionally, 78.25% of caregivers reported focusing on helping the pediatric patient change positions and correct abnormal posture while sleeping (Table 4).
Spearman correlation analysis revealed significantly positive correlations between knowledge and attitude (r = 0.0889, P = 0.0377) and between attitude and practice (r = 0.5550, P < 0.001) (Table S4). SEM showed favorable goodness-of-fit indices (RMSEA = 0.024, SRMR = 0.025, TLI = 0.978, CFI = 0.990) (Table S5). The SEM identified significantly positive associations between monthly income and knowledge (path coefficient = 0.09, P = 0.002). It also showed positive relationships of knowledge (path coefficient = 0.28, P = 0.048) and education level (path coefficient = 0.46, P = 0.001) with attitude. Additionally, attitude (path coefficient = 1.27, P < 0.001) and the dominant hand of pediatric patients (path coefficient = 1.34, P < 0.001) were positively associated with practice (Fig. 1, Table S6).
Structural equation model showing the associations between KAP scores. All variables are observed variables. Direction of causality is indicated by single-headed arrows. The standardized path coefficients are presented alongside the arrows.
Dominant hand of pediatric patients, Residence, Education levels, Occupational type, Monthly income.
Further SEM analysis confirmed direct associations between monthly income and knowledge (path coefficient = 0.09, 95% CI: 0.03, 0.15, P = 0.002). Knowledge (path coefficient = 0.28, 95% CI: 0.00, 0.56, P = 0.048) and education level (path coefficient = 0.46, 95% CI: 0.19, 0.72, P = 0.001) were directly associated with attitude. Furthermore, attitude (path coefficient = 1.27, 95% CI: 1.10, 1.43, P < 0.001) and the dominant hand of pediatric patients (path coefficient = 1.34, 95% CI: 0.60, 2.08, P < 0.001) showed direct associations with practice. Knowledge (path coefficient = 0.35, 95% CI: 0.00, 0.71, P = 0.049) and education level (path coefficient = 0.58, 95% CI: 0.24, 0.92, P = 0.001) were also indirectly linked to practice (Table 5).
Discussion
This study showed that caregivers of pediatric patients with hemiplegia demonstrated adequate knowledge, positive attitudes, and proactive practices towards rehabilitation management. Positive and direct correlations were observed between knowledge and attitude, and between attitude and practice. Besides, indirect associations were determined between knowledge and practice.
The KAP levels in our study underscored the essential role of informed and engaged caregivers in the rehabilitation of children with hemiplegia. In alignment with our findings, one study from Saudi Arabia reported favorable KAP scores among caregivers of children with cerebral palsy20. Similarly, a Chinese study highlighted high KAP levels towards home-based care among family caregivers of cerebral infarction patients18. In contrast, an Egyptian study found that most caregivers of hemiplegic adults demonstrated only moderate knowledge and struggled to implement effective care practices17. Also, Hamed and Abd Elaleam26 reported caregivers’ unsatisfactory knowledge and inadequate practices regarding cerebral palsy of their children. These disparities in KAP levels emphasized the need for targeted educational interventions. Such initiatives should focus on providing accessible information, training programs, and support networks tailored to caregivers’ specific needs in diverse settings.
The highest accuracy (99.27%) in the knowledge dimension was related to recognizing physical therapy as a standard treatment for pediatric hemiplegia. Physical therapy is widely regarded as a cornerstone in hemiplegia management, both in clinical practice and caregiver education27. Similar to findings on caregivers’ perceptions of post-acute home healthcare28, our study indicated that caregivers were well-informed about physical therapy’s role in enhancing mobility, strength, and functional independence in children with hemiplegia. Conversely, the lowest accuracy (84.10%) was observed in caregivers’ understanding of the importance of managing sleeping positions, eating, and daily activities for pediatric patients’ condition. Inappropriate sleeping positions can lead to musculoskeletal complications29, while inadequate assistance with eating and other activities may hinder the child’s development and independence30. Future educational interventions should place greater emphasis on the holistic nature of rehabilitation, ensuring that caregivers are equally well-informed about the importance of daily activities and positioning in the management of pediatric hemiplegia.
Most caregivers (96.90%) held positive attitudes towards the roles of rehabilitation management in improving pediatric patient outcomes. Such high positivity indicates that caregivers are highly motivated to engage in rehabilitation practices, as they recognize the potential benefits for their child’s functional improvement and overall well-being. However, only 1.64% of caregivers reporting that they did not feel anxious due to the pediatric patient’s illness. The chronic nature of hemiplegia, coupled with concerns about the child’s future independence and quality of life, can lead to considerable stress for caregivers31,32. Additionally, the pressure of managing rehabilitation routines can contribute to heightened anxiety levels31. Taken together, while caregivers may be committed to supporting their child’s rehabilitation, the emotional burden they carry can impede their well-being. Programs aimed at caregiver well-being, including counseling, stress management training, and peer support networks, can thus be valuable in reducing anxiety and improving mental health.
In the practice dimension, most caregivers (93.60%) actively encouraged the pediatric patients during rehabilitation training. Encouragement and positive reinforcement are critical elements in rehabilitation, which are essential for achieving long-term improvements in motor function and independence33. Contrastingly, the lowest adherence rate (63.44%) was reported for seeking help to relieve negative emotions by talking to relatives, friends, or psychologists. Several reasons may account for the finding. First, caregivers may prioritize the physical aspects of care over their emotional well-being, focusing more on their child’s rehabilitation needs rather than addressing their own mental health challenges34. Second, cultural or societal factors may discourage caregivers from seeking external support, particularly psychological services. The gaps can be due to stigmatization or a lack of awareness about the availability and benefits of such resources35. Research also reported that high levels of caregiver stress and emotional strain can negatively impact caregiving practices, potentially reducing the effectiveness of rehabilitation efforts for the child36. Introducing psychological support services as a routine part of the rehabilitation can make it easier for caregivers to reduce any stigma associated with seeking help. Besides, peer support groups where caregivers can share their experiences with others in similar situations may serve as an accessible form of emotional relief.
Compared to the correlation between attitude and practice, the correlation between knowledge and attitude was much weaker. Caregivers may possess sufficient knowledge, but their attitudes may be affected by personal experiences, social support, or perceived barriers to caregiving. Therefore, while improving knowledge is crucial, fostering positive attitudes may also require addressing emotional, psychological, or societal factors. Further SEM analysis confirmed the indirect associations between knowledge and practice. Knowledge alone may not directly drive caregiving behaviors; instead, it works by shaping caregivers’ attitudes, which in turn influence their practices. Educational interventions should focus on enhancing attitudes by emphasizing the effectiveness and importance of rehabilitation, fostering confidence in caregiving skills, and addressing emotional barriers. Several influential factors of KAP were also determined. First, caregivers from higher-income households were more likely to possess greater knowledge. The association can be explained by the better access to educational resources, healthcare services, and rehabilitation programs related to the higher income37. Providing cost-effective resources to improve their knowledge of rehabilitation are suggested, such as community outreach programs and online platforms offering educational materials. Second, a high level of education was associated with improved attitude scores, possibly due to the understanding of rehabilitation effectiveness. Educational support should be developed for caregivers with lower income, including visual aids, step-by-step guides, and interactive media for easy understandings. Third, caregivers of right-handed pediatric patients exhibited higher practice scores. This may be attributed to the stronger motor connectivity in right-handed individuals, which allows caregivers to more easily engage in exercises that utilize the dominant hand, thereby enhancing the effectiveness of caregiving practices38.
This study has several limitations. First, its cross-sectional design and single-region focus may limit the generalizability and causal interpretation of the findings. Second, the reliance on self-reported data through questionnaires can introduce the potential for social desirability bias and inaccurate measurement, which may cause inflated or skewed responses39. More objective measures are recommended, such as direct observation of caregiving data from healthcare professionals, to complement self-reported questionnaires. Additionally, triangulating the data with qualitative interviews could provide a more comprehensive understanding of caregivers’ attitudes and behaviors. Third, despite efforts were made to ensure a representative sample by including both hospitalized and outpatient caregivers, selection bias may still exist to impact the generalizability of our findings.
In conclusion, caregivers of pediatric patients with hemiplegia exhibited adequate knowledge, positive attitudes, and proactive rehabilitation practices. Targeted educational interventions and support programs are necessary, especially for those with lower income and education levels.
Data availability
All data generated or analysed during this study are included in this published article.
References
Varma, A. et al., Pediatric Patients With Hemiplegia: A Systematic Review of a Randomized Controlled Trial. Cureus. 15, (2023).
Damiano, D. et al. Comparing functional profiles of children with hemiplegic and diplegic cerebral palsy in GMFCS levels I and II: are separate classifications needed? Dev. Med. Child. Neurol. 48, 797–803 (2006).
McIntyre, S. et al. Global prevalence of cerebral palsy: A systematic analysis. Dev. Med. Child. Neurol. 64, 1494–1506 (2022).
Yang, S., Xia, J., Gao, J. & Wang, L. Increasing prevalence of cerebral palsy among children and adolescents in China 1988–2020: A systematic review and meta-analysis. J. Rehabil Med. 53, jrm00195 (2021).
Gong, C. et al. Prevalence and related factors of epilepsy in children and adolescents with cerebral palsy: a systematic review and meta-analysis. Frontiers Pediatr. 11, 1189648 (2023).
Chiu, H. C., Ada, L., Cherng, R. J. & Chen, C. Asymmetry in sensory-motor function between the lower limbs in children with hemiplegic cerebral palsy: an observational study. J. Physiol. Invest. 66, 345–350 (2023).
Pashmdarfard, M., Richards, L. G. & Amini, M. Factors affecting participation of children with cerebral palsy in meaningful activities: systematic review. Occup. Therapy Health Care. 35, 442–479 (2021).
Said, R., Abd-Elmonem, A. M. & Aly, M. G. Correlation between selective motor control and upper extremity function in children with hemiparesis. Pakistan J. Med. Health Sci. 15, 1709–1712 (2021).
Jasien, J. M. et al. Cognitive, adaptive, and behavioral profiles and management of alternating hemiplegia of childhood. Dev. Med. Child. Neurol. 61, 547–554 (2019).
Papathanasiou, E., Chevignard, M., Vuillerot, C., Tiberghien, A. & Godard, I. Pediatric stroke rehabilitation: A review of techniques facilitating motor recovery. Ann. Phys. Rehabil. Med. 59, e2 (2016).
Atkinson, H. L., Greenham, M., Cooper, A. & Gordon, A. Intervention for Functional Motor Skills in Children with Strokep. 113–134 (Routledge, 2024).
Chan-Víquez, D. et al. Understanding a videogame home intervention for children with hemiplegia: a mixed methods multi-case study. Front. Med. Technol. 5, 1217797 (2023).
Massey, J., Tsianakas, V., Gordon, A. & Robert, G. Improving parent and therapist experiences of codelivering intensive upper limb interventions for children with hemiplegia: A qualitative study using the theoretical domains framework. Child Care Health Dev. 51, e70040 (2025).
Shoukat, N. & Khawar, R. The perceived social support, dysfunctional attitude, resilience and quality of life in hemiplegic paralyzed patients. Pakistan Armed Forces Med. J. 73, 1695 (2023).
Rissardo, J. P., Vora, N. M., Singh, Y., Kishore, S. & Caprara, A. L. F. Navigating the complexity of alternating hemiplegia in childhood: A comprehensive review. Rambam Maimonides Med. J. 15, e0015 (2024).
Samanta, D. Management of alternating hemiplegia of childhood: a review. Pediatr. Neurol. 103, 12–20 (2020).
Tony, M. I., Ragheb, S. G. & Ibrahim, W. K. Caregivers’ Awareness Regarding Hemiplegia among Adults. prevalence. 922, 100-000.
Chen, Z. et al. Knowledge, attitudes, and practices of family caregivers for patients with cerebral infarction toward home-based care. Front Public Health. 12, 1436423 (2024).
Chen, Z. et al. Knowledge, attitudes, and practices of family caregivers for patients with cerebral infarction toward home-based care. Front. Public. Health. 12, 1436423 (2024).
Almosallam, A. et al. Caregiver Knowledge, Attitude, and Behavior toward Care of Children with Cerebral Palsy: A Saudi Arabian Perspective. 12, 982 (2024).
Pourhoseingholi, M. A., Vahedi, M. & Rahimzadeh, M. Sample size calculation in medical studies. Gastroenterol. Hepatol. Bed Bench. 6, 14–17 (2013).
Chen, Y. et al. Quality of life and it’s influencing factors for caregivers of children with disabilities. Chin. Rehabilitation Theory Pract. 27, 1144–1151 (2021).
Guo, J. et al. Interventions to improve physical function for children and young people with cerebral palsy: interpretation by Chinese experts. Chin. J. Appl. Clin. Pediatr. 37, 502–509 (2023).
Jackman, M. et al. Interventions to improve physical function for children and young people with cerebral palsy: international clinical practice guideline. Dev. Med. Child. Neurol. 64, 536–549 (2022).
He, J. et al. Chinese pregnant women’s knowledge, attitude, and practice of self-protection against coronavirus disease 2019 during the post-pandemic period: A structural equation modeling-based survey. Int. J. Disaster Risk Reduct. 87, 103559 (2023).
Hamed, A. & Abd Elaleam, N. A. Assessment caregiver’s knowledge and practice regarding care of their children with cerebral palsy. Helwan Int. J. Nurs. Res. Pract. 2, 206–218 (2023).
Huang, J. et al. Effects of physical therapy-based rehabilitation on recovery of upper limb motor function after stroke in adults: a systematic review and meta-analysis of randomized controlled trials. Annals Palliat. Med. 11, 52131–52531 (2022).
Chase, J. D. et al. Caregivers’ perceptions managing functional needs among older adults receiving Post-Acute home health care. Res. Gerontol. Nurs. 12, 174–183 (2019).
Noll, M. et al. High prevalence of inadequate sitting and sleeping postures: a three-year prospective study of adolescents. Sci. Rep. 7, 14929 (2017).
Masuke, R. et al. Effect of inappropriate complementary feeding practices on the nutritional status of children aged 6–24 months in urban Moshi, Northern Tanzania: cohort study. PloS One. 16, e0250562 (2021).
Dlamini, M. D., Chang, Y. J. & Nguyen, T. T. B. Caregivers’ experiences of having a child with cerebral palsy. A meta-synthesis. J. Pediatr. Nurs. 73, 157–168 (2023).
Fritz, H. & Sewell-Roberts, C. Family stress associated with cerebral palsy. In: Cerebral Palsy (515–545) (Springer, 2020).
Gangwani, R., Cain, A., Collins, A. & Cassidy, J. M. Leveraging factors of self-efficacy and motivation to optimize stroke recovery. Front. Neurol. 13, 823202 (2022).
Buka, S. L. et al. The family is the patient: promoting early childhood mental health in pediatric care. Pediatrics 149 (Supplement 5), e2021053509L (2022).
Zou, X., Fitzgerald, R. & Nie, J. B. Unworthy of care and treatment: cultural devaluation and structural constraints to Healthcare-Seeking for older people in rural China. Int. J. Environ. Res. Public Health. 17, 2132 (2020).
Cui, P. et al. The impact of caregiver burden on quality of life in family caregivers of patients with advanced cancer: a moderated mediation analysis of the role of psychological distress and family resilience. BMC Public. Health. 24, 817 (2024).
McMaughan, D. J., Oloruntoba, O. & Smith, M. L. Socioeconomic status and access to healthcare: interrelated drivers for healthy aging. Front. Public. Health. 8, 231 (2020).
Pool, E. M., Rehme, A. K., Fink, G. R., Eickhoff, S. B. & Grefkes, C. Handedness and effective connectivity of the motor system. Neuroimage 99, 451–460 (2014).
Bergen, N. & Labonté, R. Everything is perfect, and we have no problems: detecting and limiting social desirability bias in qualitative research. Qual. Health Res. 30, 783–792 (2020).
Author information
Authors and Affiliations
Contributions
Qi Liu and Xiaoyong Chen carried out the studies, participated in collecting data, and drafted the manuscript. Ya Guo, Xiaoli Li, Gongwei Jia, Jiahong Zhan, Zhongyu He, Guangshen Yuan, Chunyan Liu, Yuanyuan Lai read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been approved by the Institutional Review Board of Pediatric Patient’s Hospital of Chongqing Medical University (ethics review batch number: (2024) Lun Review (Research) No. (5)), and the written informed consent of the study subjects was obtained. I confirm that all methods were performed in accordance with the relevant guidelines. All procedures were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Guo, Y., Li, X., Jia, G. et al. Knowledge, attitude and practice of rehabilitation management of the caregivers of pediatric patients with hemiplegia. Sci Rep 15, 18756 (2025). https://doi.org/10.1038/s41598-025-03223-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-03223-0