Abstract
The exact cause for no pain, local pain and referred pain groups according to the upper cervical palpation test (UPT) and whether neck pain in migraine patients is caused due to pain sensitization or influenced by perceived neck-related disability, is not fully understood. The aim was to determine whether upper cervical spine sensitivity tested by the UPT is associated with neck-related disability or increased pain sensitization in patients with migraine. Forty-two patients with episodic migraine were examined regarding mechanical and pressure pain thresholds, central sensitization (CSI), allodynia (ASC-12) and neck-related disability (NDI), and sub-grouped according to the UPT. An ANOVA analysis was performed for group differences. Exploratory regression and correlation analyses were performed with NDI and CSI as dependent variables to understand which factors are related and contribute to either subgroup allocation. No significant differences were found in UPT subgroups regarding CSI and NDI. The UPT subgroups could not be determined by any evaluated variable. The NDI was explained in 43.6% by the CSI and neck pain intensity. CSI results were explained to 49.4% by a model including ASC-12 and NDI. In conclusion, UPT subgroups were neither explained by differences in CSI, mechanical or pressure threshold testing or NDI.
Similar content being viewed by others
Introduction
Migraine is one of the diseases with the greatest global burden. In women and young adult men, headache disorders, especially migraine, are ranked among the top 10 diseases leading to disability in daily life1. Migraine is assumed to have a neurobiological cause originating in the central nervous system2. The biological cascade associated with a migraine attack is proposed to result in sensitization of trigeminal nociceptors, potentially explaining hyperalgesia and allodynia3. Pain perceived during a migraine attack is mainly located within the innervation area of the trigeminal nervous system4.
Migraine is characterized by attacks lasting 4 to 72 h, moderate to severe pain intensity, unilateral localization, and pulsatile pain. It is further associated with photophobia and phonophobia, nausea, and often worsens with physical activity5. Another highly prevalent yet often neglected and much-discussed manifestation of migraine is neck pain6,7. Up to 77% of migraineurs have neck pain, making it as frequent as all associated symptoms mentioned above. Compared to headache-free people, patients with migraine are 12 times more likely to have neck pain8. Nevertheless, neck pain is not part of the migraine diagnostic criteria5.
Neck pain in patients with migraine is related to a more severe clinical presentation of migraine attacks and worse migraine-related disability9. It is seen as a potential trigger for migraine attacks, correlates with a higher attack frequency, and is associated with a higher risk of chronicity10,11,12. Hence, the clinical relevance of neck pain and the need for a standard evaluation of the cervical spine of patients is evident. In addition, patients with migraine have a significantly higher presence of cervical musculoskeletal dysfunctions7. Further, there is an ongoing scientific debate as to whether neck pain should be considered a migraine symptom or whether, if it is due to a neck dysfunction, and if it may be a cause of or contributing factor to migraine.
A collection of standard headache assessment tests (HATs) for evaluating musculoskeletal neck dysfunctions in patients with migraine has been presented by Luedtke et al.13. Another commonly used and highly validated tool for assessing neck-related disability is the Neck Disability Index (NDI)14. Of all tests of the HATs, particularly manual joint palpation and trigger point palpation, had the highest prevalence of findings in migraine patients7. Luedtke and May continued investigating these findings by palpation of the upper cervical segments. With the upper cervical palpation test (UPT), patients can be stratified into three groups of neck pain perception, which may have high clinical relevance for future treatment of migraine: no pain, local pain, and referred pain during sustained palpation6.
Manual examination via the UPT requires pressure through suboccipital structures (joints, ligaments, suboccipital muscles). Hence, pain provocation during palpation could indicate either muscle or joint changes6. The trigeminocervical convergence theory represents a possible interaction between the musculoskeletal upper cervical and trigeminal nerve systems, as these are closely connected anatomically4,15. Considering this, the UPT may provide a mechanical explanation for local and referred pain sensitivity during the examination, as palpation is performed directly at the atlantooccipital and atlantoaxial joints6. These findings of different pain sensations in the upper cervical spine may indicate the presence of cervical musculoskeletal changes in migraine patients. However, it is not clear yet whether the neck pain in migraine patients is caused by a generally more sensitized system due to peripheral or central sensitization or by muscle or joint-related neck-related disability.
Since neck pain and disability in migraine patients have been physically assessed with the UPT6, there needs to be further clarification of what the test truly evaluates. Therefore, the aim of the study was to assess the differences of the UPT subgroups regarding sensitization and neck pain/related disability. Besides, to determine whether upper cervical spine sensitivity tested by the UPT is associated with neck-related disability or increased pain sensitization in migraine patients. The first hypothesis is that the UPT may be explained by neck pain and/or neck-related disability. The second hypothesis is that the UPT may be explained by central sensitization.
Methods
The study protocol was preregistered on the Open Science Framework Platform (https://doi.org/10.17605/OSF.IO/CTKHM) and performed in accordance with relevant guidelines/regulations. The study was approved by the ethics committee of the University of Luebeck. All participants provided written informed consent prior to the data collection.
Participants
This study is part of the “MigrainePREDICT” study, in which at least 38 patients with migraine were required. Participants were recruited by convenience sampling from the campus of the University of Luebeck and social networks and the inclusion criteria were age between 18 and 73 years old, episodic migraine with or without aura with at least two headache days per month, fulfilling the diagnostic criteria of the third International Classification of Headache Disorders (ICHD-3)5. Participants were excluded from the study if they had a headache on the day of the examination, took pain medication on the day of the examination, or had any additional chronic systemic, neurological, or psychiatric illness. Further exclusion criteria were diagnosed acute neck pathologies or neck injuries such as rear-end collision or whiplash injuries in the last ten years.
Measurements
All participants filled out a questionnaire on demographic data and migraine- and neck-specific characteristics. Questions included age, migraine pain intensity, migraine attacks per month, and migraine diagnosis confirming associated symptoms such as an increase of the symptoms with activity, light, or noise. The presence of neck pain, its intensity and frequency were also recorded.
Upper cervical palpation test
Upper cervical spine sensitivity was tested using the UPT, described by Luedtke and May6 (Fig. 1). Oscillating and sustained palpation for about 30 s was performed on both sides of the transverse process of C1 (testing the left and right atlantooccipital joint number 1 on Fig. 1), and on both sides of the transverse process of C2, testing the left and right atlantoaxial joint (number 2 on Fig. 1). Patients were positioned in prone with their hands supporting their forehead. Pain intensity was verbally reported on a numerical pain scale from 0 to 10. Pain location was assessed as “no pain” if they did not feel any pain perception, “local pain” for pain in the neck area, and “referred pain” for pain referring to the head or back. The examiner further documented whether hypomobility was present in the tested joints (binary outcome).
Neck disability and intensity
For measuring neck-related disability, all participants completed the German version of the Neck Disability Index (NDI), which is a valid and reliable 10-item questionnaire on self-reported disability due to neck pain, with each question scored from 0 to 5 and a total score ranging from 0 to 5014,16,17. The NDI was implemented and validated for neck pain associated with various cervical musculoskeletal conditions14,16,18,19,20 Neck pain intensity was additionally self-evaluated in the demographic and symptom questionnaire using a numerical pain rating (NPRS) scale from 0 to 1021.
Central sensitization
For measuring central sensitization, all participants completed the Central Sensitization Inventory (CSI)22 part A. Part A is a questionnaire assessing 25 symptoms, on a scale from 1 to 4, associated with central sensitization syndrome with a total score ranging from 0 to 100. Part B was not used for this study as it focuses on additional diagnoses (e.g. Fibromyalgia, Chronic Fatigue Syndrome) related to central sensitization, which were exclusion criteria for this study23. In addition, the Allodynia Symptom Checklist (ASC-12)24 was evaluated, a 12-item questionnaire with total scores ranging from 0 to 24 that asks about the presence and frequency of allodynia symptoms during a migraine attack and thus measures cutaneous allodynia.
Mechanical pain threshold and pressure pain threshold
The mechanical pain threshold (MPT) and pressure pain threshold (PPT) of the standardised and validated quantitative sensory testing (QST) protocol25 were assessed bilaterally to further quantify sensitivity. MPT and PPT were used at four sites: the neck (spinous process of C2), a receptive field of the first branch of the trigeminal nerve (V1) (above left and right eyebrow), and at a remote site (outside the neck or the receptive field of the trigeminal nerves (arm).
At all sites, MPT was measured with standardised PinPrick stimulators weighted from 8 to 512 mN (MRI Compatible Pinprick Stimulator Set; MRC Systems GmbH, Heidelberg, Germany). At each site, three series of threshold determination were performed, using ascending and descending stimuli until the participant reported a “sharp” or “blunt” sensation. There was no fixed time interval between the repetitions, but a brief pause was allowed to reposition the equipment and ensure consistency. MPT values were transformed logarithmically and calculated as the geometric mean. A higher mean value is associated with lower mechanical sensitivity.
PPTs were obtained with a standardised mechanical pressure algometer with a 1 cm2 contact surface and a 1–10 kg/cm2 scale (Force Dial FDK/FDN 20 algometer, Wagner Instruments, Greenwich, USA). At each site, threshold determination was performed three times by increasing the pressure by 0.5 k/s until participants reported the first sensation of pain. There was no fixed time interval between the repetitions, but a brief pause was allowed to reposition the equipment and ensure consistency and to avoid temporal summation of pain. PPT values were transformed logarithmically and calculated as the geometric mean. A higher mean value is associated with lower pressure sensitivity.
Procedures
All eligible and included participants (n = 42) first completed a series of questionnaires. Participants who were included were subsequently assigned to UPT and quantitative sensory testing for the MPT and PPT in a randomized order. All examiners were blinded toward migraine diagnosis, as the examination was part of a larger study, which also recruited healthy control participants. After all tests, the participants were stratified into three groups according to the results of the UPT (no pain, local pain, referred pain)6.
The examiner to the UPT test was a licensed physiotherapist with over seven years of clinical experience, and in the past six years, has been treating patients with headaches. Additionally, prior to data collection, all examiners underwent training and practice toward all assessments to ensure consistency. All participants were assessed using the same procedures to minimize potential bias.
Statistical analysis
Statistical analyses were performed with JAMOVI with a significance level of 5%. Demographic data and questionnaires for headache and neck pain characteristics were presented for each pain group as mean values, standard deviations, and percentages. To assess the normality of the data, Shapiro–Wilk test was performed. MPT and PPT results were transformed logarithmically prior to statistical analysis and are presented as mean values and standard deviations. Differences between UPT subgroups, regarding all test results, were assessed by Kruskal–Wallis-Test and chi-square test to account for the small sample sizes in each subgroup. Multinominal logistic regression model was performed with UPT groups (no pain, local pain and referred pain) and multilinear regression models with the NDI and CSI total scores as dependent variable, considering the variables that had significant associations with the dependent variable (p < 0.200) to explain which factors contribute to each score. To further explore correlations between the variables, Pearson’s correlation test was used for interval-scaled data and Spearman’s rho for ordinal-scaled data.
Results
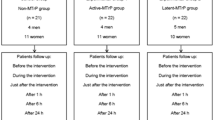
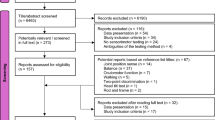
A total of 52 migraine patients were recruited for the study. Ten individuals were excluded as they did not fulfil the inclusion criteria. The 42 eligible participants were included in the analysis and were stratified into three UPT subgroups (Fig. 2).
Demographic data, headache, and neck pain characteristics of the participants for each subgroup of the UPT, are represented in Table 1. No statistically significant differences were found among the subgroups considering all measurements of neck-related disability and central sensitization (Tables 1 and 2).
There were no significant correlations among the CSI and all MPT and PPT results (p > 0.05). Therefore, these variables were not used for further statistical analysis (Table 3).
For the logistic regression considering the UPT subgroups as the dependent variable, the reference category was the no pain group (0), number 1.00 was the local pain group, and number 2.00 was the referred pain group. The model was not significant (X2 = 10.540(8); p = 0.229), therefore even though the CSI was a significant predictor, this result cannot be considered (Table 4).
Subsequently, it was evaluated which of the variables influenced neck disability and central sensitization, respectively. In Table 5, considering the NDI score as the dependent variable, the results showed that model 3 was statistically significant [F = 16.870; p = 0.000; R2 adjusted = 0.436] and that NDI, was explained to 43.6% by the CSI questionnaire (p = 0.000) and neck pain intensity (p = 0.032).
Considering the CSI score as the dependent variable, the results demonstrated that model 2 was statistically significant [F = 14.328; p = 0.000; R2 adjusted = 0.494]. CSI was explained in 49.4% by the ASC-12 (p = 0.006) and the NDI (p = 0.000). The UPT did not significantly explain the CSI (p = 0.056), as shown in Table 6.
Discussion
The purpose of this study was to disentangle neck-related disability or pain sensitivity as explanations for UPT results in patients with migraine.
In the sample, 83% percent of migraine patients perceived local or referred neck pain during the UPT. Seventeen percent had no pain during the examination, and 43% perceived referred pain to the head. These results corroborate the UPT findings of Luedtke et al.6, who reported that 80% of migraineurs perceived pain on upper cervical spine palpation, with half of these also reporting referred pain. It, however, shows a different proportion of Watson and Drummond26 who observed higher rates of head pain referral in both migraine and tension-type headache populations or Liang et al.27 that showed much lower number of cervical musculoskeletal findings in patients with migraine, compared with tension type headache. Differences between these reports can only be hypothesized and are most likely based on either the population characteristics, the purpose of the studies or individual differences across examiners.
The subgroup stratification according to the UPT may indicate clinically relevant migraine subtypes: migraine patients without UPT neck findings may experience neck pain as a migraine symptom without any ongoing nociception from the upper cervical spine. In contrast, migraine patients with UPT findings might have upper cervical spine dysfunctions, which could be contributing to migraine-associated disability6.
Considering that the UPT requires pressure on suboccipital structures and assesses the patient’s pain response, results may either indicate local muscle or joint changes6 or evaluate general pain sensitivity, potentially influenced by central sensitization processes.
In this current sample, UPT subgroups did not differ significantly regarding neck disability or neck pain intensity, CSI, ASC-12, and MPT and PPT measures. This is line with the results of the observational study by Schwarz et al. (2021), in which no statistically significant subgroup differences were found regarding neck-related disability or allodynia (NDI and ASC-12). This raises the question of how the different pain perceptions, leading to the subgroup allocation, can be explained.
The most obvious hypothesis is that the UPT assesses musculoskeletal neck dysfunction and that subgroup allocations could, hence, also be explained by NDI, and neck pain intensity. However, this hypothesis could not be confirmed. In fact, the “no pain” group of the UPT reported higher levels of average neck pain intensity than the “local and referred pain” groups. There are several ways to explain these results: The overall prevalence of neck pain in this current sample was very high (82%) and highest in the “no pain” UPT group.
The UPT assesses the upper cervical spine (C1 and C2), as these cervical segments are assumed to influence the trigeminal nervous system through proximity of spinal and trigeminal afferents within the brainstem4. Schwarz et al. further elaborated that only the upper two cervical segments may contribute to pain provocation in patients with migraine28.
The literature on neck pain, however, reports that the majority of neck pain and disability are caused by mid and lower cervical segments29. It, therefore, seems likely that the neck pain and disability reported by this current sample are independent phenomena alongside migraine, affecting lower parts of the cervical spine, which were not assessed during the UPT. This explanation aligns with Liang et al., who postulated that the NDI–when used in migraine populations–is more influenced by allodynia or central sensitization than by musculoskeletal dysfunction since, in their study, a correlation between NDI and cervical dysfunction could not be found. This suggestion is potentially confirmed by the results of this study, in which the NDI was explained by 43.6% for the CSI questionnaire and neck pain intensity.
The second hypothesis, that UPT subgroups are determined by the level of central sensitization, was also not confirmed. Even for the highest CSI values in the “referred pain” group and lowest in the “no pain” group, the ANOVA analyses did not provide statistically significant differences between subgroups regarding indicators for central sensitization (CSI, ASC-12, and mechanical and pressure pain thresholds).
Less surprisingly, CSI and ASC-12 showed a positive and statistically significant correlation- this indicates that the perceived unpleasantness of sensory stimuli in the face and neck during migraine attacks (as measured by the ASC-12) is related to an overall level of increased sensitivity and perceived unwellness (measured by the CSI).
The lack of correlation between the QST variables and CSI is more challenging to interpret, given that previous studies by Mibu et al. and Steinmetz et al. reported a high correlation between PPTs and CSI30,31,32. However, these studies were not performed in migraine populations but in chronic low-back pain, knee osteoarthritis, and musculoskeletal disorders30,31,32. Regarding migraine, our findings diverge from previous studies that have demonstrated significant associations between central sensitization and sensory processing in migraine33,34. A potential explanation for this discrepancy lies in our smaller sample size and in methodological differences, such as the stratification of the participants across different phases of the migraine cycle33. Furthermore, approximately one-third of the items on the CSI are typically reported associated symptoms of migraine attacks, such as headache, temporomandibular symptoms, nausea, sleep, cognition, and sensitivity to light35. Hence, the CSI results recorded in this current sample might reflect more typical migraine-associated symptoms than central sensitization.
One important limitation of the current study is that it was not systematically controlled for the migraine cycle phase at the time of the assessment, since the participants were assessed at a single time point without migraine phase classification, however, the purpose was not to differentiate between migraine phases but to assess the influences on UPT test results. Since pain sensitivity is expected to change with the migraine phases the association between sensitivity and UPT results should remain stable.
This study only investigated C1 and C2 and did not manually assess mid or lower cervical segments or use other tests. However, previous research showed that the NDI and manual palpation results are correlated24. It can, therefore, be postulated that the neck-related disability reported by this study population were explained by musculoskeletal dysfunction in the lower parts of the cervical spine.
No imaging or additional tests were performed to assess the upper cervical spine, which could confirm the UPT results. Hence, the results must be interpreted with caution and can only exclude the influence of central sensitization and perceived neck-related disability as driving factors for subgroup classification.
The sample sizes of the UPT subgroups were relatively small6,34. However, similar group sizes are used in other studies on the UPT subgrouping. Furthermore, Kruskal–Wallis testing is robust even in small sample sizes36.
Conclusion
The current results confirm the high prevalence of neck pain in migraineurs and of pain during UPT reported in previous studies within this population. Pain on UPT is not determined by central sensitization, as measured by CSI or by overall neck-related disability, as measured by the NDI. Hence, the NDI seems to be of limited use in detecting upper cervical musculoskeletal dysfunction in patients with migraine. Similarly, the CSI seems to provide limited information on central sensitization in migraine patients since one-third of the items describe migraine-related symptoms. The UPT, therefore, is believed to measure an independent construct, most likely upper cervical musculoskeletal dysfunction that should be confirmed in future studies.
Data availability
The data that support the findings of this study are available on request from the corresponding author, KL.
References
Steiner, T. J., Stovner, L. J., Jensen, R., Uluduz, D. & Katsarava, Z. Migraine remains second among the world’s causes of disability, and first among young women: Findings from GBD2019. J. Headache Pain 21(1), 137. https://doi.org/10.1186/s10194-020-01208-0 (2020).
Goadsby, P. J. Advances in the understanding of headache. Br. Med. Bull. 73–74(1), 83–92. https://doi.org/10.1093/bmb/ldh052 (2005).
Meents, J. E., Neeb, L. & Reuter, U. TRPV1 in migraine pathophysiology. Trends Mol. Med. 16(4), 153–159. https://doi.org/10.1016/j.molmed.2010.02.004 (2010).
Bartsch, T. & Goadsby, P. J. The trigeminocervical complex and migraine: Current concepts and synthesis. Curr. Pain Headache Rep. 7(5), 371–376. https://doi.org/10.1007/s11916-003-0036-y (2003).
Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 38(1):1–211. https://doi.org/10.1177/0333102417738202 (2018).
Luedtke, K. & May, A. Stratifying migraine patients based on dynamic pain provocation over the upper cervical spine. J. Headache Pain 18(1), 97. https://doi.org/10.1186/s10194-017-0808-0 (2017).
Luedtke, K., Starke, W. & May, A. Musculoskeletal dysfunction in migraine patients. Cephalalgia Int. J. Headache 38(5), 865–875. https://doi.org/10.1177/0333102417716934 (2018).
Al-Khazali, H. M. et al. Prevalence of neck pain in migraine: A systematic review and meta-analysis. Cephalalgia 42(7), 663–673. https://doi.org/10.1177/03331024211068073 (2022).
Bragatto, M. M. et al. Is the presence of neck pain associated with more severe clinical presentation in patients with migraine? A cross-sectional study. Cephalalgia Int. J. Headache 39(12), 1500–1508. https://doi.org/10.1177/0333102419854061 (2019).
Florencio, L. L. et al. Neck pain disability is related to the frequency of migraine attacks: A cross-sectional study. Headache 54(7), 1203–1210. https://doi.org/10.1111/head.12393 (2014).
Ferracini, G. N. et al. Myofascial trigger points and migraine-related disability in women with episodic and chronic migraine. Clin. J. Pain 33(2), 109. https://doi.org/10.1097/AJP.0000000000000387 (2017).
Vincent, M. B. Headache and Neck. Curr. Pain Headache Rep. 15(4), 324–331. https://doi.org/10.1007/s11916-011-0195-1 (2011).
Luedtke, K. et al. International consensus on the most useful physical examination tests used by physiotherapists for patients with headache: A Delphi study. Man Ther. 23, 17–24. https://doi.org/10.1016/j.math.2016.02.010 (2016).
Vernon, H. The Neck Disability Index: State-of-the-art, 1991–2008. J. Manipulat. Physiol. Ther. 31(7), 491–502. https://doi.org/10.1016/j.jmpt.2008.08.006 (2008).
Bartsch, T. Increased responses in trigeminocervical nociceptive neurons to cervical input after stimulation of the dura mater. Brain 126(8), 1801–1813. https://doi.org/10.1093/brain/awg190 (2003).
Vernon, H. & Mior, S. The Neck Disability Index: A study of reliability and validity. J. Manipulat. Physiol. Ther. 14(7), 409–415 (1991).
Cramer, H., Lauche, R., Langhorst, J., Dobos, G. J. & Michalsen, A. Validation of the German version of the Neck Disability Index (NDI). BMC Musculoskelet. Disord. 15, 91. https://doi.org/10.1186/1471-2474-15-91 (2014).
Young, B. A. et al. Responsiveness of the neck disability index in patients with mechanical neck disorders. Spine J. 9(10), 802–808. https://doi.org/10.1016/j.spinee.2009.06.002 (2009).
Pietrobon, R., Coeytaux, R. R., Carey, T. S., Richardson, W. J. & DeVellis, R. F. Standard scales for measurement of functional outcome for cervical pain or dysfunction: A systematic review. Spine 27(5), 515 (2002).
Figueirêdo, I. N. A. et al. Occurrence and severity of neck disability in individuals with different types of temporomandibular disorder. Oral. Maxillofac. Surg. 25(4), 471–476. https://doi.org/10.1007/s10006-021-00943-1 (2021).
Williamson, A. & Hoggart, B. Pain: A review of three commonly used pain rating scales. J. Clin. Nurs. 14(7), 798–804. https://doi.org/10.1111/j.1365-2702.2005.01121.x (2005).
Neblett, R., Hartzell, M. M., Mayer, T. G., Cohen, H. & Gatchel, R. J. Establishing clinically relevant severity levels for the central sensitization inventory. Pain Pract. Off. J. World Inst. Pain 17(2), 166–175. https://doi.org/10.1111/papr.12440 (2017).
Neblett, R. et al. The central sensitization inventory (CSI): Establishing clinically significant values for identifying central sensitivity syndromes in an outpatient chronic pain sample. J. Pain 14(5), 438–445. https://doi.org/10.1016/j.jpain.2012.11.012 (2013).
Lipton, R. B. et al. Cutaneous allodynia in the migraine population. Ann. Neurol. 63(2), 148–158. https://doi.org/10.1002/ana.21211 (2008).
Rolke, R. et al. Quantitative sensory testing: A comprehensive protocol for clinical trials. Eur. J. Pain 10(1), 77–88. https://doi.org/10.1016/j.ejpain.2005.02.003 (2006).
Watson, D. H. & Drummond, P. D. Head pain referral during examination of the neck in migraine and tension-type headache. Headache 52(8), 1226–1235. https://doi.org/10.1111/j.1526-4610.2012.02169.x (2012).
Liang, Z., Galea, O., Thomas, L., Jull, G. & Treleaven, J. Cervical musculoskeletal impairments in migraine and tension type headache: A systematic review and meta-analysis. Musculoskelet. Sci. Pract. 42, 67–83. https://doi.org/10.1016/j.msksp.2019.04.007 (2019).
Schwarz, A., Luedtke, K. & Schöttker-Königer, T. Only cervical vertebrae C0–C2, not C3 are relevant for subgrouping migraine patients according to manual palpation and pain provocation: Secondary analysis of a cohort study. BMC Musculoskelet. Disord. 23(1), 379. https://doi.org/10.1186/s12891-022-05329-2 (2022).
Balcha, T. E., Getaneh, F. B. & Woldeyohannes, A. M. A Retrospective analysis on cervical spine magnetic resonance imaging findings in patients with neck pain in a tertiary hospital, Addis Ababa, Ethiopia. Ethiop. J. Health Sci. 31(5), 1025–1032. https://doi.org/10.4314/ejhs.v31i5.15 (2021).
Mibu, A., Nishigami, T., Tanaka, K., Manfuku, M. & Yono, S. Difference in the impact of central sensitization on pain-related symptoms between patients with chronic low back pain and knee osteoarthritis. J. Pain Res. 12, 1757–1765. https://doi.org/10.2147/JPR.S200723 (2019).
Steinmetz, A., Hacke, F. & Delank, K. S. Pressure pain thresholds and central sensitization in relation to psychosocial predictors of chronicity in low back pain. Diagn. Basel Switz. 13(4), 786. https://doi.org/10.3390/diagnostics13040786 (2023).
Mibu, A. et al. Does a combination of self-reported signs related to central sensitization and pressure pain threshold allow for a more detailed classification of pain-related characteristics in patients with chronic musculoskeletal pain?: A cross-sectional study. Pain Pract. Off. J. World Inst. Pain 22(6), 556–563. https://doi.org/10.1111/papr.13125 (2022).
Di Antonio, S. et al. Cervical musculoskeletal impairments in the 4 phases of the migraine cycle in episodic migraine patients. Cephalalgia 42(9), 827–845. https://doi.org/10.1177/03331024221082506 (2022).
Di Antonio, S. et al. Profiling migraine patients according to clinical and psychophysical characteristics: Clinical validity of distinct migraine clusters. Neurol. Sci. 45(3), 1185–1200. https://doi.org/10.1007/s10072-023-07118-8 (2024).
Suzuki, K., Suzuki, S., Shiina, T., Kobayashi, S. & Hirata, K. Central sensitization in migraine: A narrative review. J. Pain Res. 15, 2673–2682. https://doi.org/10.2147/JPR.S329280 (2022).
Schwarz, A., Ziegeler, C., Daneshkhah, S., May, A. & Luedtke, K. Predicting the outcome of the greater occipital nerve block—An observational study on migraine patients with and without musculoskeletal cervical impairment. Cephalalgia 41(1), 78–89. https://doi.org/10.1177/0333102420954518 (2021).
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
All authors had a substantial contribution to the conception and design of the project.; JP, MMO, EK, LJ, ND, KL were major contributors to data collection; JP, MMO, AV, KL discussed and analysed the main data of the manuscript; JP, MMO were major contributors to the manuscript writing and share the first authorship; All the authors read and approve of the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pradela, J., Otto, M.M., Kaske, E. et al. Results of upper cervical palpation test in migraine patients are not explained by pain sensitization. Sci Rep 15, 20276 (2025). https://doi.org/10.1038/s41598-025-03344-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-03344-6