Abstract
This study aims to elucidate the relationship between social jetlag and depressive symptoms in college students, with a focus on identifying specific cut points that significantly heighten the risk of depression. A cross-sectional study was conducted among 2,006 students from Jiangsu College of Nursing between October and November 2024. Social jetlag was calculated based on the difference between the midpoints of sleep on workdays and weekends. Depressive symptoms were assessed using the Patient Health Questionnaire-9 (PHQ-9). Multivariate logistic regression was applied to examine the relationship between social jetlag and depressive symptoms, adjusting for potential confounders. The prevalence of depressive symptoms (PHQ-9 ≥ 10) among participants was 10.1%. A non-linear relationship was observed between social jetlag and depressive symptoms, with the risk of depression increasing significantly beyond a threshold of 1.2 h of social jetlag. Specifically, individuals with social jetlag ≥ 1.2 h had 72% higher odds of depressive symptoms compared to those with lower levels (OR = 1.72, 95% CI: 1.24–2.38). Subgroup analyses revealed that this association was consistent across both grade and gender. Sensitivity analyses further affirmed the robustness of these findings. This study suggests a non-linear association between social jetlag and depressive symptoms in college students, with a marked increase in depression risk for those with social jetlag ≥ 1.2 h. Longitudinal studies are needed to clarify the causal pathways and identify modifiable factors for targeted interventions.
Similar content being viewed by others
Introduction
Depression represents a significant and growing global health challenge, affecting approximately 3.8% of the population worldwide. It is estimated that over 280 million people are currently living with depression, a mental health disorder that is now considered one of the leading causes of disability and a major contributor to the global disease burden. Tragically, depression is also responsible for more than 700,000 deaths annually due to suicide, which has become the fourth leading cause of death among individuals aged 15 to 29 years1.
University students, who are squarely situated within this high-risk age group, face a unique set of challenges that heighten their vulnerability to mental health disorders. The prevalence of depressive symptoms among college students is alarmingly high, with estimates suggesting that 33.6% of students experience some form of depressive distress2. The transition to university life often brings with it increased academic stress, new social dynamics, and the need to develop personal independence, all of which can place considerable strain on mental well-being3. Amid these stressors, sleep health emerges as a critical yet frequently underestimated factor in overall mental well-being4. Disturbed sleep is common among university students, with over 60% classified as poor-quality sleepers. These sleep disturbances are often exacerbated by delayed bedtimes and risetimes, particularly during weekends5. Such irregular sleep patterns contribute to disruptions in sleep-wake cycles, culminating in a phenomenon known as social jetlag6. This occurs when there is a misalignment between an individual’s internal biological clock and the externally imposed social schedules, especially the discrepancy between weekday and weekend routines7.
Social jetlag has emerged as a critical issue in addressing the sleep-health challenges commonly faced by college students, particularly those transitioning to university life8,9. Characterized by the misalignment between weekday and weekend sleep patterns, social jetlag disrupts circadian rhythms, resulting in a cascade of adverse physiological and psychological outcomes. These include fatigue10, impaired cognitive performance11, and metabolic dysfunction12. Of particular concern is the potential long-term impact of chronic social jetlag, which has been linked to an increased risk of mental health disorders, including depression13,14.
Despite the increasing recognition of social jetlag as a potential contributor to depressive symptoms in college students15, findings remain inconsistent16,17. Research examining its association with depression among college students-particularly freshman-remains limited. Furthermore, existing studies have yet to establish specific thresholds or “cut points” for social jetlag in this population, beyond which the risk of developing depressive symptoms significantly escalates. Identifying such thresholds is critical for the development of evidence-based interventions and preventive strategies aimed at alleviating the mental health burden associated with social jetlag in this population. Therefore, the present study seeks to address these gaps by exploring the relationship between social jetlag and depressive symptoms among college students.
Methods
Study design and participants
This cross-sectional study employed a cluster sampling method to recruit participants from Jiangsu College of Nursing, China. The target population included full-time, on-campus students aged 18 years or older, while commuting students and those engaged in off-campus internships were excluded.
The minimum required sample size was calculated to ensure adequate statistical power. Based on a total student population of 20,000, a margin of error of 5%, and a confidence level corresponding to a Z-score of 1.96, the estimated sample size was 377 participants18. To account for a potential 20% non-response rate, the required sample size was increased to approximately 452 participants.
Participants were recruited during evening self-study sessions via online promotion using a WeChat QR code. A total of 2,006 students were invited to participate in the study between October and November 2024. Of these, 1,764 students completed the questionnaire, which exceeded the minimum sample size requirement. Ethical approval for the study was obtained from the Jiangsu College of Nursing Ethics Committee (approval number: JSCN-ME-2024093002). Written informed consent was obtained from all participants prior to their inclusion in the study.
Data collection was conducted using a structured questionnaire designed to capture sociodemographic characteristics, medical history, lifestyle behaviors, and depressive symptoms. The survey was distributed via the “Questionnaire Star” platform. Students from 45 classes across 10 academic majors were invited to complete the questionnaire by scanning a QR code with their smartphones. To ensure data quality, trained quality control personnel were present on-site throughout the data collection process to address participant queries and verify the accuracy and completeness of completed questionnaires.
Social jetlag
Social jetlag was assessed using structured questionnaire that collected information on participants’ sleep and wake times on both workdays and weekends over the past month. The midpoint of sleep was calculated as the midpoint between sleep onset and wake-up time, using the formula: midpoint of sleep = sleep onset + (sleep duration ÷ 2). Social jetlag was defined as the absolute difference between the midpoint of sleep on workdays and weekends, calculated as: social jetlag = |midpoint of sleep on weekends-midpoint of sleep on workdays| 7.
Depressive symptoms
In this study, depressive symptoms were assessed using the Patient Health Questionnaire-9 (PHQ-9), a validated screening tool widely used for the assessment of depressive disorders in both clinical and research settings. The PHQ-9 consists of nine items, each corresponding to the diagnostic criteria for major depressive disorder outlined in the DSM-IV. Participants were asked to report the frequency of depressive symptoms experienced over the past two weeks. Each item was rated on a four-point Likert scale: “not at all” (0 points), “several days” (1 point), “more than half the days” (2 points), and “nearly every day” (3 points). The total PHQ-9 score ranges from 0 to 27, with higher scores indicating greater severity of depressive symptoms. A cutoff score of ≥ 10 was used to define the presence of clinically significant depressive symptoms, which aligns with established thresholds in previous validation studies. This threshold has demonstrated good diagnostic performance, with a sensitivity of 85% and a specificity of 85% for detecting major depressive disorder19.
Other variables
Age (years), gender (male/female), and grade level (freshman/sophomore) were recorded as basic demographic information. Anthropometric measurements included self-reported height (cm) and weight (kg), which were used to calculate body mass index (BMI) as weight (kg) divided by height (m²). BMI was categorized into three groups based on the Working Group on Obesity in China’s criteria: underweight (< 18.5 kg/m²), normal weight (18.5–24 kg/m²), and overweight/obese (≥ 24 kg/m²)20. Lifestyle factors included smoking status and alcohol consumption. Smoking status was classified into three categories: current smoker, former smoker, and never smoker. Alcohol consumption frequency was categorized as > 1 time per month or ≤ 1 time per month. Health-related factors included a self-reported history of clinically diagnosed hypertension (yes/no), diabetes (yes/no), and cardiovascular diseases (yes/no).
Statistical analysis
Multivariate logistic regression models were employed to evaluate the associations between social jetlag and depressive symptoms, with results expressed as odds ratios (ORs) and 95% confidence intervals (CIs). Three models were constructed to account for potential confounding factors: Model 1, a crude model without any covariate adjustments; Model 2, adjusted for age, gender, and grade level; and Model 3, further adjusted for BMI, smoking status, alcohol consumption, and sleep duration.
In the logistic regression models, depression was treated as the dependent variable, while social jetlag was modeled as the primary independent variable. To further investigate potential non-linear exposure–response relationships, restricted cubic spline regression with two degrees of freedom was applied. The exposure–response curves derived from the splines were used to determine a cutoff value for social jetlag, enabling the classification of participants into low and high social jetlag groups, with the low social jetlag group serving as the reference category.
To assess potential effect modification, stratified analyses were conducted according to grade level, gender, and BMI categories. Additionally, sensitivity analyses were performed to examine the robustness of the findings. Specifically, these analyses excluded participants with a history of clinically diagnosed hypertension, diabetes, or cardiovascular diseases, as well as those exhibiting advanced sleep timing on weekends (defined as the midpoint of sleep on rest days being earlier than on workdays). All statistical analyses were conducted using R software (version 4.4.2). Statistical significance was defined as a two-tailed p-value of < 0.05.
Results
Study sample characteristics
A total of 2,006 college students were invited to participate in the study, of whom 1,764 completed the questionnaire, yielding a response rate of 87.9%. Table 1 summarizes the general characteristics of the participants. The median (IQR) age of the respondents was 19 (19–20) years, and the majority were female (83.3%). Most participants were freshmen (63.1%), with BMI predominantly within the normal range (18.5–24 kg/m², 56.3%). Current smokers accounted for only 2.4% of the sample, while the vast majority were either former smokers or had never smoked (97.6%). Alcohol consumption was infrequent, with 97.1% of participants reporting drinking alcohol ≤ 1 time/month. The prevalence of hypertension, diabetes, and cardiovascular diseases was low, at 0.8%, 0.2%, and 0.6%, respectively. Depressive symptoms (PHQ-9 ≥ 10) were reported by 10.1% of participants. The median (IQR) sleep duration was 8.87 (8.21–9.61) hours, while the median (IQR) social jetlag was 1.13 (0.58–1.75) hours.
Non-linear association between social jetlag and depressive symptoms
Figure 1 depicts the dose-response relationship between social jetlag and the OR of depressive symptoms, adjusted for potential confounders. The analysis revealed a significant non-linear association (P-overall < 0.0001; P-non-linear = 0.0001). The OR remained stable when social jetlag was below approximately 1.2 h, indicating minimal risk. However, beyond this threshold, the OR increased sharply, peaking at around 5 h of social jetlag, with the highest risk observed. At higher levels of social jetlag, the OR began to decline, though it remained elevated compared to lower levels of social jetlag. Consequently, 1.2 h was selected as the cut-off value to categorize social jetlag in subsequent analyses. The distribution of participants with social jetlag < 1.2 h and ≥ 1.2 h is summarized in Table S1. Of the 1,764 students, 53.3% exhibited social jetlag < 1.2 h, while 46.7% had ≥ 1.2 h. No significant differences were observed in age or sex distribution between the groups. However, students with social jetlag ≥ 1.2 h were significantly more likely to be freshmen and current smokers. This group also exhibited longer sleep durations and a higher prevalence of depressive symptoms.
The associations between social jetlag and depressive symptoms are summarized in Table 2. In the unadjusted model (Model 1), individuals with social jetlag ≥ 1.2 h had significantly higher odds of depressive symptoms compared to those with social jetlag < 1.2 h (OR = 1.62, 95% CI: 1.19–2.22, P = 0.002). After adjusting for age, sex, and grade (Model 2), the association remained robust, with an OR of 1.64 (95% CI: 1.19–2.26, P = 0.002). Further adjustments in Model 3 yielded similar results, with individuals experiencing ≥ 1.2 h of social jetlag having 72% higher odds of depressive symptoms compared to their counterparts with < 1.2 h of social jetlag (OR = 1.72, 95% CI: 1.24–2.38, P = 0.001).
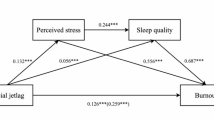
The results of subgroup analyses for the association between social jetlag and depressive symptoms across different demographic characteristics are presented in Fig. 2 and Table S2. Among freshmen, those with social jetlag ≥ 1.2 h had significantly higher odds of depressive symptoms compared to their counterparts with social jetlag < 1.2 h (OR = 2.09, 95% CI: 1.05–5.18, P = 0.036). A similar association was observed among sophomores (OR = 1.61, 95% CI: 1.11–2.33, P = 0.012). Gender-stratified analysis revealed that the odds of depressive symptoms were elevated in both females (OR = 1.64, 95% CI: 1.15–2.34, P = 0.006) and males (OR = 2.42, 95% CI: 0.99–5.88, P = 0.052), though the association in males approached but did not reach statistical significance. When stratified by BMI, individuals with a BMI of 18.5 to 24 kg/m² showed the strongest association between social jetlag ≥ 1.2 h and depressive symptoms (OR = 1.91, 95% CI: 1.22–3.01, P = 0.005). This association was also significant in those with a BMI > 24 kg/m² (OR = 1.84, 95% CI: 1.01–3.34, P = 0.045) but not in participants with a BMI < 18.5 kg/m² (P = 0.364). Notably, no statistically significant interactions were observed between social jetlag and age, gender, grade, BMI, or sleep duration in relation to depressive symptoms (all P for interaction > 0.05).
Sensitivity analyses
The results of the sensitivity analyses are summarized in Table S3. In the first sensitivity analysis, which excluded participants with hypertension, diabetes, or cardiovascular diseases (n = 23), the association between social jetlag and depressive symptoms remained robust and statistically significant (OR = 1.75, 95% CI: 1.26–2.43, P = 0.001). In the second sensitivity analysis, which excluded 131 participants who exhibited weekend advanced sleep timing, the association also persisted with a slightly higher effect size (OR = 1.84, 95% CI: 1.30–2.60, P = 0.001).
Discussion
In our study, the prevalence of depressive symptoms among college students was 10.1%, which is notably lower than the 28.4% prevalence rate reported in a recent meta-analysis of depression among Chinese university students. This discrepancy is partly due to the considerable variation in prevalence rates across different studies, which range from 2.4 to 80.6%. These differences are influenced by factors such as the study population and the tools used for screening21. Even when the same screening tool is applied, variations in the cutoff scores can lead to significant differences in reported prevalence22. In the present study, we used the PHQ-9 with a cutoff score of 10, which is typically used to identify moderate to severe depressive symptoms22. The prevalence of depressive symptoms in our study falls within the range of 7.8–12.6%, as reported in Chinese college students that also applied the PHQ-9 ≥ 10 cutoff23. This indicates that our findings are consistent with the general trend observed in similar populations. The use of this higher threshold likely contributed to the lower prevalence observed in our sample, as it may have excluded individuals with mild depressive symptoms.
This study examined the relationship between social jetlag and depressive symptoms among college students, revealing a significant non-linear association. Our results indicate that social jetlag ≥ 1.2 h is associated with a higher likelihood of depressive symptoms. Notably, this association remained robust after adjusting for various potential confounders, suggesting that social jetlag may function as an independent risk factor for depression in this population. Subgroup analyses further affirmed the consistency of this relationship across demographic groups, including freshmen, sophomores, and both genders, thus reinforcing the generalizability of our findings. These results align with previous research. For instance, a study conducted in the United States also found a positive association between social jetlag and depressive symptoms among college students15. Conversely, studies conducted in Korea and China found no significant association between social jetlag and depressive symptoms among college students16,17. While these studies typically employed linear models, our study used restricted cubic splines to model the dose-response relationship, allowing us to capture the non-linear nature of the association. Previous studies have suggested that the relationship between social jetlag and depressive symptoms is significantly non-linear among adolescents24,25. For instance, depressive symptoms initially showed a slight decrease at lower levels of social jetlag, reaching the lowest risk at around 51 min, after which the risk increased progressively25. Similarly, our study identified a threshold of social jetlag at 72 min, beyond which the risk of depressive symptoms increased markedly. There is no consensus on the optimal cut-off values for social jetlag in predicting depressive symptoms. Previous studies have typically categorized social jetlag into hourly segments (e.g., 0 to < 1 h, 1 to < 2 h, and ≥ 2 h)26,27. While our study supports this general approach, we utilized restricted cubic splines to more precisely capture the non-linear nature of the relationship between social jetlag and depressive symptoms, providing a more nuanced understanding of the dose-response relationship.
The precise mechanisms underlying the relationship between social jetlag and depressive symptoms remain poorly understood. Existing research has indicated that disturbances in the circadian rhythm can lead to metabolic imbalances, especially affecting glucose and lipid metabolism28, which may in turn increase susceptibility to depressive symptoms29. Moreover, interactions between the circadian system and the sleep homeostatic system—responsible for regulating sleep duration and intensity—are also of significant interest30. Previous study has highlighted that sleep duration is independently linked to the onset of depressive symptoms31. In our study, we observed that the association between social jetlag and depressive symptoms remained significant even after controlling for sleep duration. This suggests that the effects of circadian rhythm disturbances on depressive symptoms may operate independently of the sleep homeostasis system. A recent study shows that social jetlag is associated with reduced melatonin production, as evidenced by lower urinary excretion of 6-sulfatoximelatonin in night workers compared to day workers32. Since melatonin plays a crucial role in regulating mood, its dysregulation due to social jetlag may disrupt these processes, thereby increasing the risk of depressive symptoms33. Additionally, other potential mechanisms, including the roles of cortisol and epigenetic factors, warrant further investigation to deepen our understanding of this complex relationship.
The strengths of this study include the large sample size, which allowed for adjustments for potential confounders such as age, gender, and academic grade. Furthermore, the use of multiple stratified analyses provided valuable insights into the varying impact of social jetlag on depressive symptoms across different demographic subgroups. Notably, our findings emphasize the robust dose-response relationship between social jetlag and depressive symptoms, with a clear threshold effect. However, our study also has several limitations. First, the cross-sectional design of the study limits our ability to draw causal inferences between social jetlag and depressive symptoms. Second, although the study included a large sample of college students, it relied on a convenience sampling method, which may limit the generalizability of the findings to other populations or regions. However, it is important to note that this institution includes students from a wide variety of programs, such as Nursing, Health Management, Rehabilitation, and Public Health Management. As such, our study encompasses a diverse sample that can be considered somewhat representative of the broader college student population. Additionally, Jiangsu Nursing College is the only medical university in Huai’an, which further enhances the representativeness of the sample within this regional context. Third, although we controlled for key confounders, the possibility of residual confounding cannot be entirely ruled out. Thirdly, the study utilized self-reported questionnaires to assess social jetlag, which may be subject to reporting biases. Finally, our definition of social jetlag was based solely on sleep timing, specifically the difference in mid-sleep time between weekdays and weekends. This measure does not capture potential differences in daily activities, which are also important contributors to circadian misalignment. Further research with more objective sleep measures, such as actigraphy or polysomnography, would help to validate our findings and provide a more accurate assessment of sleep patterns.
Conclusions
In conclusion, this study demonstrates a significant association between social jetlag and depressive symptoms in college students, with a marked increase in risk for those experiencing social jetlag ≥ 1.2 h. The relationship remained robust after adjusting for key confounders, highlighting the potential impact of disrupted sleep patterns on mental health. Longitudinal studies are needed to better understand the temporal relationship between social jetlag and depressive symptoms in college student, as well as to explore the underlying mechanisms driving this association.
The exposure-response relationships between social jetlag and odd ratio of depressive symptoms among college students. The red solid line represents the odds ratio (OR) of depressive symptoms as a function of social jetlag, while the shaded area indicates the 95% confidence interval. The dashed red vertical line marks a social jetlag of 1.2 h, indicating an increased risk threshold. The black dashed horizontal line represents an odds ratio of 1, indicating no increased or decreased risk.
Subgroup analysis of the odds ratio for depressive symptoms among college students by body mass index (BMI), gender, and grade. BMI is categorized as < 18.5 kg/m², 18.5–24 kg/m², and ≥ 24 kg/m² (red markers). Gender is divided into female and male (green markers), while grade is categorized as freshman and sophomore (blue markers). The vertical dashed line represents an odd ratio of 1, indicating no difference in risk.
Data availability
The data supporting this study’s findings were available from the corresponding author upon reasonable request.
References
Institute of Health Metrics and Evaluation. Global Health Data Exchange (GHDx). https://vizhub.healthdata.org/gbd-results/ (Accessed 9 January 2025).
Li, W., Zhao, Z., Chen, D., Peng, Y. & Lu, Z. Prevalence and associated factors of depression and anxiety symptoms among college students: a systematic review and meta-analysis. J. Child. Psychol. Psychiatry. 63, 1222–1230. https://doi.org/10.1111/jcpp.13606 (2022).
Kumaraswamy, N. Academic stress, anxiety and depression among college students: A brief review. Int. Rev. Social Sci. Humanit. 5, 135–143 (2013).
Dinis, J. & Bragança, M. Quality of sleep and depression in college students: A systematic review. Sleep. Sci. 11, 290–301. https://doi.org/10.5935/1984-0063.20180045 (2018).
Lund, H. G., Reider, B. D., Whiting, A. B. & Prichard, J. R. Sleep patterns and predictors of disturbed sleep in a large population of college students. J. Adolesc. Health. 46, 124–132. https://doi.org/10.1016/j.jadohealth.2009.06.016 (2010).
Di, H. et al. Evaluation of sleep habits and disturbances among US adults, 2017–2020. JAMA Netw. Open. 5, e2240788. https://doi.org/10.1001/jamanetworkopen.2022.40788 (2022).
Wittmann, M., Dinich, J., Merrow, M. & Roenneberg, T. Social jetlag: misalignment of biological and social time. Chronobiol Int. 23, 497–509. https://doi.org/10.1080/07420520500545979 (2006).
Komada, Y. et al. Social jetlag and menstrual symptoms among female university students. Chronobiol Int. 36, 258–264. https://doi.org/10.1080/07420528.2018.1533561 (2019).
Hakimi, H., Hosseinkhani, Z., Taherkhani, O. & Momeni, M. Association between chronotype, social jetlag, sleep quality, and academic burnout among nursing students: A cross-sectional study. Chronobiol Int. 41, 1275–1286. https://doi.org/10.1080/07420528.2024.2397396 (2024).
Tamura, N., Komada, Y., Inoue, Y. & Tanaka, H. Social jetlag among Japanese adolescents: association with irritable mood, daytime sleepiness, fatigue, and poor academic performance. Chronobiol Int. 39, 311–322. https://doi.org/10.1080/07420528.2021.1996388 (2022).
Yang, F. N., Picchioni, D. & Duyn, J. H. Effects of sleep-corrected social jetlag on measures of mental health, cognitive ability, and brain functional connectivity in early adolescence. Sleep 46 https://doi.org/10.1093/sleep/zsad259 (2023).
Bouman, E. J. et al. The association between social jetlag and parameters of metabolic syndrome and type 2 diabetes: a systematic review and meta-analysis. J. Sleep. Res. 32, e13770. https://doi.org/10.1111/jsr.13770 (2023).
Min, J., Jang, T. W., Lee, H. E., Cho, S. S. & Kang, M. Y. Social jetlag and risk of depression: results from the Korea National health and nutrition examination survey. J. Affect. Disord. 323, 562–569. https://doi.org/10.1016/j.jad.2022.12.010 (2023).
Tamura, N. & Okamura, K. Longitudinal course and outcome of social jetlag in adolescents: A 1-year follow-up study of the adolescent sleep health epidemiological cohorts. J. Sleep. Res. 33, e14042. https://doi.org/10.1111/jsr.14042 (2024).
Weiss, C., Woods, K., Filipowicz, A. & Ingram, K. K. Sleep quality, sleep structure, and PER3 genotype mediate chronotype effects on depressive symptoms in young adults. Front. Psychol. 11, 2028. https://doi.org/10.3389/fpsyg.2020.02028 (2020).
Chang, S. J. & Jang, S. J. Social jetlag and quality of life among nursing students: A cross-sectional study. J. Adv. Nurs. 75, 1418–1426. https://doi.org/10.1111/jan.13857 (2019).
Qu, Y. et al. Association of chronotype, social jetlag, sleep duration and depressive symptoms in Chinese college students. J. Affect. Disord. 320, 735–741. https://doi.org/10.1016/j.jad.2022.10.014 (2023).
Wang, J. & Fang, S. The developmental trajectory of college students’ psychological flexibility: based on latent growth model. J. Context. Behav. Sci. 32, 100765 (2024).
Negeri, Z. F. et al. Accuracy of the patient health Questionnaire-9 for screening to detect major depression: updated systematic review and individual participant data meta-analysis. Bmj 375, n2183. https://doi.org/10.1136/bmj.n2183 (2021).
Ji, C. Y. Report on childhood obesity in China (1)--body mass index reference for screening overweight and obesity in Chinese school-age children. Biomed. Environ. Sci. 18, 390–400 (2005).
Gao, L., Xie, Y., Jia, C. & Wang, W. Prevalence of depression among Chinese university students: a systematic review and meta-analysis. Sci. Rep. 10, 15897. https://doi.org/10.1038/s41598-020-72998-1 (2020).
Kroenke, K., Spitzer, R. L. & Williams, J. B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x (2001).
Luo, W., Zhong, B. L. & Chiu, H. F. Prevalence of depressive symptoms among Chinese university students amid the COVID-19 pandemic: a systematic review and meta-analysis. Epidemiol. Psychiatr Sci. 30, e31. https://doi.org/10.1017/s2045796021000202 (2021).
Zhang, Y., Fan, Y., Ma, Z., Wang, D. & Fan, F. Associations of social jetlag and insomnia symptoms with depressive symptoms among Chinese adolescents: A large population-based study. Sleep. Med. 104, 98–104. https://doi.org/10.1016/j.sleep.2023.02.024 (2023).
Tamura, N. & Okamura, K. Social jetlag as a predictor of depressive symptoms among Japanese adolescents: evidence from the adolescent sleep health epidemiological cohort. Sleep. Health. 9, 638–644. https://doi.org/10.1016/j.sleh.2023.06.005 (2023).
Bouman, E. J. et al. Is the association between social jetlag and BMI mediated by lifestyle? A cross-sectional survey study in the Dutch general population. Prev. Med. 181, 107908. https://doi.org/10.1016/j.ypmed.2024.107908 (2024).
Jung, E. J. et al. Association between social jetlag and self-rated health: evidence from Korean representative working population. Sleep. Med. 114, 86–91. https://doi.org/10.1016/j.sleep.2023.12.019 (2024).
Panda, S. Circadian physiology of metabolism. Science 354, 1008–1015. https://doi.org/10.1126/science.aah4967 (2016).
Muhtz, C., Zyriax, B. C., Klähn, T., Windler, E. & Otte, C. Depressive symptoms and metabolic risk: effects of cortisol and gender. Psychoneuroendocrinology 34, 1004–1011. https://doi.org/10.1016/j.psyneuen.2009.01.016 (2009).
Logan, R. W. et al. Impact of sleep and circadian rhythms on addiction vulnerability in adolescents. Biol. Psychiatry. 83, 987–996. https://doi.org/10.1016/j.biopsych.2017.11.035 (2018).
Li, X. L., Wei, J., Zhang, X., Meng, Z. & Zhu, W. Relationship between night-sleep duration and risk for depression among middle-aged and older people: A dose-response meta-analysis. Front. Physiol. 14, 1085091. https://doi.org/10.3389/fphys.2023.1085091 (2023).
Vieira, R. P. O. et al. High social jetlag is correlated with nocturnal Inhibition of melatonin production among night workers. Chronobiol Int. 38, 1170–1176. https://doi.org/10.1080/07420528.2021.1912072 (2021).
Kholghi, G., Eskandari, M., Shokouhi Qare Saadlou, M. S., Zarrindast, M. R. & Vaseghi, S. Night shift hormone: how does melatonin affect depression? Physiol. Behav. 252, 113835. https://doi.org/10.1016/j.physbeh.2022.113835 (2022).
Funding
This work was supported by the General Research Project in Philosophy and Social Sciences at Jiangsu Higher Education Institutions (Grant No. 2024SJYB1446), the Research on the Construction of the ‘One-Stop’ Student Community Network Ideological and Political Education System in Higher Education Institutions under New Media (Grant No. 2024SHBZ29), and the Innovation and Entrepreneurship Program of Jiangsu Province (Grant No. JSSCBS20211625).
Author information
Authors and Affiliations
Contributions
J.L and S.L: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing-original draft, Writing-review & editing. J.Y: Data curation, Investigation, Supervision, Writing-review & editing. T.D, Z.J, S.W, L.Z, H.G, B.Y, Y.L, Y.Z, J.W, W.Y, Q.R: Investigation, Data curation, Writing-review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
Ethical approval for the study was obtained from the Jiangsu College of Nursing Ethics Committee (approval number: JSCN-ME-2024093002). Written informed consent was obtained from all participants prior to their inclusion in the study. All data procedures were carried out in accordance with relevant ethical guidelines and regulations associated with the declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Luo, J., Yang, J., Dai, T. et al. Non-linear relationship between social jetlag and depressive symptoms among Chinese college students. Sci Rep 15, 18317 (2025). https://doi.org/10.1038/s41598-025-03371-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-03371-3