Abstract
Pedicle screw fixation (PSF) has been extensively utilized in lumbar fusion surgeries to assist in stabilization. However, inappropriate implantation could accelerate the progression of adjacent segment degeneration (ASD). Current finite element studies are predominantly confined to single-segment fixation under conditions of normal bone mineral density and mechanical analyses of unidirectional adjacent vertebrae, failing to fully represent the diversity of clinical conditions. This study aimed to compare the biomechanical effects of long-segment unilateral pedicle screw fixation (UPSF) and bilateral pedicle screw fixation (BPSF) on ASD under normal and osteoporotic bone mineral density conditions. A finite element (FE) comparative study. METHODS Six distinct types of spinal models with L2–L5 fixation were constructed and categorized into two groups according to the different bone mineral density conditions: Group 1 (Model A: bilateral fixation, Model B: left lateral fixation, Model C: right lateral fixation) and Group 2 (Model D: bilateral fixation with osteoporosis, Model E: left lateral fixation with osteoporosis; Model F: right lateral fixation with osteoporosis). Six distinct motions were simulated for each model. These simulations were conducted to analyze the alterations in the range of motion (ROM), intervertebral disc pressure (IDP), articular cartilage stress in the adjacent upper and lower vertebrae, and stress experienced by the screw‒rod system. The ROM of the fused segment decreased significantly after internal fixation, and all values were less than 5°, meeting the stability criteria for surgery. Conversely, the adjacent vertebrae exhibited varying degrees of increased ROM during rotation, with the lower adjacent vertebrae in the osteoporotic model being particularly prominent. In addition, BPSF was more likely to cause IDP and articular cartilage stress than UPSF; the IDP in L1/L2 and L5/S1 was significantly greater in BPSF than in UPSF (difference range: 13.65-16.44%). The stress in the L1/L2 and L5/S1 adjacent vertebral articular cartilages was also greater in BPSF than in UPSF (difference range: 20.19-27.07%). The peak stress of the screw‒rod system was 197.88 MPa, which was significantly lower than its yield stress (825–895 MPa). Both UPSF and BPSF can meet the stability criteria necessary for spinal fusion surgery. The UPSF has relatively little biomechanical influence on adjacent segments, reducing the incidence of ASD. For patients requiring PSF, opting for the UPSF method may be more beneficial, irrespective of the bone mineral density. When treating osteoporosis patients, a critical assessment of bone density is needed, and personalized treatment should be adopted to avoid excessive adjacent vertebral activity and the risk of screw–rod breakage. This study provides strong biomechanical support for the clinical selection of PSF types for patients with different bone mineral density conditions.
Similar content being viewed by others
Introduction
Pedicle screw fixation (PSF) is a widely utilized spinal auxiliary fixation technique in clinical practice; it is often utilized in conjunction with oblique lumbar interbody fusion (OLIF) for the treatment of spinal degenerative diseases1,2. This approach effectively restores the intervertebral space height, enhances the sagittal balance of the lumbar spine, and maintains its stability. Notably, the clinical efficacy rate can be as high as 90–95%3. This internal fixation technique benefits mechanical transfer from the posterior column to the anterior column4, effectively preserving the three-dimensional structure of the spine and significantly reducing the risk of nerve damage5. Furthermore, precise screw channel positioning and rational design of the internal fixation system can significantly improve the efficiency of surgery and reduce the risk of recurrence. Compared with stand-alone cage fusion, PSF has been shown to markedly decrease the incidence of cage subsidence and has emerged as the gold standard for lumbar fusion surgery6.
Conventional PSF employs bilateral pedicle screw fixation (BPSF). While providing sufficient stability, BPSF has disadvantages, such as significant surgical trauma, excessive bleeding, and a long postoperative recovery time. Moreover, BPSF may also cause excessive stability of the vertebral body and increase the stress of the intervertebral disc in the adjacent vertebra, causing adjacent segment degeneration (ASD). Levy et al.7,8,9 proposed that the excessive stiffness of the BPSF is suspected to be the cause of ASD. With the development of minimally invasive techniques, the fixation method of unilateral pedicle screw fixation (UPSF) has gradually gained attention. Researchers have reported that the unilateral approach not only reduces surgical trauma and recovery time but also, in some cases, is comparable in stability to BPSF10. Nonetheless, the clinical application of UPSF remains controversial, especially in terms of long-term efficacy and a potential risk of adjacent segmental degeneration. In addition, there is a lack of compelling biomechanical evidence.
ASD, a common complication following lumbar fusion, encompasses a spectrum of issues, such as lumbar spondylolisthesis, nucleus pulposus prolapse, lumbar spinal stenosis, loss of intervertebral height, and microarthropathy11. The presence of ASD may cause new symptoms and even require surgical repair12,13, imposing a considerable financial burden on patients and is considered a critical factor affecting patients’ quality of life. Consequently, the prevention and treatment of ASD following internal fixation has become an unavoidable problem for clinicians14,15,16. It is widely accepted that the occurrence of ASD is closely related to biomechanical alterations in the lumbar spine segment17. Dujic et al.18 found through retrospective imaging studies that the probability of early disc degeneration induced by UPSF is lower than that by BPSF, and they suspected that the increased stiffness caused by BPSF may play a role in increasing the stress of adjacent segments, further aggravating the induction of ASD. Kim et al.19 reported similar results. However, the specific biomechanical effects of UPSF and BPFS on adjacent vertebrae remain unclear.
In recent years, finite element (FE) simulation technology has been widely used in spinal biomechanics research. This technique provides detailed information on the stress distribution and displacement of the study subjects, helps in understanding the mechanical behavior of various parts of the spine under normal and pathological conditions, and shows great potential for predicting the risk of postoperative ASD and the failure of internal fixation. Chen et al.20 and Yu et al.21 also found through finite element analysis (FEA) that, in some cases, BPSF leads to excessive activity of adjacent vertebrae, thus aggravating the occurrence of ASD. These studies might have demonstrated the superiority of UPSF over BPSF in reducing the incidence of ASD. However, most studies are limited to normal bone mineral conditions and ignore the effect of osteoporosis on ASD. Researchers22,23,24 have reported that osteoporotic vertebrae, due to their lower bone density and strength, may negatively impact the outcomes of internal fixation surgeries. The failure of pedicle screws, displacement of fusion cages, subsequent spinal fractures, and pseudarthrosis following internal fixation surgery are associated with osteoporosis, and the risk of kyphosis at the fusion junction increases with decreasing bone density. In some cases, osteoporosis can also cause an increase in stress in the screw‒rod system, which may affect the stress distribution of adjacent vertebrae, thereby aggravating ASD. Therefore, the effect of bone mineral density on ASD should receive increased attention.
Most existing studies are predominantly confined to single-segment fixation and mechanical analyses of vertebral discs in unidirectional adjacent vertebrae, hindering a thorough understanding of the biomechanical impact of long-segment fusion and the interaction between other lumbar spine structures. Li et al.25 reported using FE comparisons that long-segment fixation was more likely to increase the stress on the intervertebral disc of the upper adjacent vertebra. Since more spinal segments are involved, long-segment fusion may result in an uneven stiffness distribution of the spine, which in turn affects the movement pattern and stress distribution of the entire spine. However, the study did not specify the stress distribution characteristics of the lower adjacent vertebra, which differs from the phenomena observed clinically. The stress distribution of the lower adjacent vertebrae is equally crucial for comprehending the biomechanical properties of the lumbar spine. Furthermore, studies have shown that mechanical changes in the articular cartilage are also important factors that aggravate the degeneration of adjacent vertebral joints. The clinical failure rate of revision surgeries due to pseudoarthrosis is as high as 40–70%22. These findings suggest that the condition of the articular cartilage significantly affects the postoperative outcomes of internal fixation surgery. Understanding the biomechanical effects of long-segmental internal fixation on upper and lower articular cartilage is also crucial for evaluating surgical efficacy and predicting postoperative complications.
The purpose of this study was to compare the biomechanical effects of long-segment UPSF and BPSF on ASD under normal and osteoporotic BMD conditions. The results of this study reveal the advantages and disadvantages of these two surgical methods, providing scientific evidence-based guidance for the clinical selection of lumbar internal fixation methods and postoperative evaluation.
Materials and methods
Construction of an intact lumbar spine model
A healthy adult male volunteer (28 years old, height 176 cm, weight 63 kg) was recruited for this research. Images from L1-S5 were obtained using a GE Light Speed VCT 64-slice spiral CT scanner (layer thickness: 0.625 mm; scanning conditions: 140 kV, 200 mA) and stored in Digital Imaging and Communications in Medicine (DICOM) format. This study was approved by the Ethics Committee of Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine (Ethics Approval number: 2024-1446-029-01). This study was conducted in compliance with the Declaration of Helsinki and all applicable ethical guidelines. All participants provided Written informed consent prior to the study.
A preliminary and complete geometrical lumbar structure was constructed from the DICOM images using Mimics 21.0 (Materialise Inc., Leuven, Belgium) and saved in the STL format. Subsequently, we segmented the lumbar vertebrae into cortical bone and cancellous bone in the three-dimensional computer-assisted software Geomagic Wrap 2021 (Geomagic Inc., NC, USA). The articular cartilages and intervertebral discs were constructed and assembled in SolidWorks 2023 (SolidWorks Corp., Waltham, MA, USA) and stored as STP format. The intervertebral disc is composed of an endplate, annulus fibrosis (AF) and nucleus pulposus (NP). We defined the volume of the NP as 43% of the entire disc and the thickness of the endplate as 1 mm26. We set the contact relationship between the articular cartilage and the upper vertebral body to “no separation”, and the remaining components were set to be bound. After assembly, the model was stored in “step” format and imported into the FEA ANSYS 2024 R2 software (ANSYS, Inc., Canonsburg, PA, USA). In the Workbench module of the software, six intervertebral ligaments, including the anterior longitudinal ligament (ALL), posterior longitudinal ligament (PLL), supraspinous ligament (SSL), interspinous ligament (ISL), ligament flavum (LF) and intertransverse ligament (IL), were constructed based on true human anatomical characteristics. Next, we proceeded with material definition and parameter assignment for all the structures according to previous finite element data21,27,28. The materials and parameters are shown in Table 1. The vertebrae geometry was meshed to 6-node hexagonal solid finite elements, which could be increased to 8-node wedge elements in the discs and cartilages. To improve the accuracy of the simulation as much as possible, we ensured that each plane had at least two meshes.
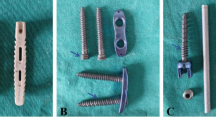
Simulation of internal fixation surgery
Six different internal fixation models were constructed to analyze the biomechanical effects of PSF methods based on the intact model and actual parameters: Group 1 (Model A: bilateral fixation, Model B: left lateral fixation, Model C: right lateral fixation) and Group 2 (Model D: bilateral fixation with osteoporosis, Model E: left lateral fixation with osteoporosis, Model F: right lateral fixation with osteoporosis; Fig. 1). To simulate internal fixation surgery, we removed the nucleus pulposus, annulus fibrosus, facet joints and articular cartilages from L2-L5 while preserving the upper and lower endplates of the corresponding segments. After that, three cages measuring 50 mm in length, 18 mm in width and 10 mm in height were implanted into the gaps. The angle between the front edge and back edge of the cage is 8°. The pedicle screw was 6 mm in diameter and 50 mm in length, whereas the rod was 5 mm in diameter. Next, the screws were placed parallel to the endplates and inserted into the vertebral bodies, ensuring that no damage to the cortical bone, after which they were assigned and analyzed according to the properties of the elastic materials. The osteoporosis Models D, E and F were obtained by changing the parameters of the cortical bone and cancellous bone29. To make the model conditions more consistent with the surgical state, we adjusted the shape and parameters of the annulus fibrosus and nucleus pulposus so that the discs were in a moderate state of degeneration (Table 1).
Boundary and load conditions
We established a contact relationship with reference to the published literature30,31; there was no sliding between the vertebral body and the fusion organ or pedicle surfaces. The freedom of the S1 lower vertebral body surface in six directions was constrained, and a vertical downward force of 500 N was applied to the upper surface of L1 to simulate the self-weight of the human body in the standing position, whereafter a pure moment of 10 N·m was applied to the same position to simulate the lumbar spine movements of flexion (FLEX), extension (EXT), left bending (LB), right bending (RB), left rotation (LR) and right rotation (RR).
Convergence test
Before the formal experiment, we conducted a grid convergence test on the model. We chose Model A as an example, roughened and refined the model respectively, and compared L1/L2 and L5/S1 disc stresses under different mesh densities. It is found that the disc stresses increased in the Coarsened model, but tended to balance in current model and the refined mode (with an error of 1.03% for L1/L2 and 4.65% for L5/S1 after refinement). The errors of the models after refinement are all less than 5%, indicating that the necessary refinement of the models is reasonable. In this study, the number the number of meshes s between Bold Model and Refined model, which takes into account the efficiency and accuracy, and is considered as a reasonable choice(As shown in Supplementary file).
Results
Model validation
The intact model was composed of 2,791,533 elements and 4,220,288 nodes. After performing simulations of three-dimensional movements, we compared the ROM results with the experimental data obtained from previous in vivo and in vitro studies32,33,34,35. The ROM value of each segment in the intact model was within the range of reference values. This strongly supported that the constructed model was valid and effective. It is worth noting that the range of motion obtained in this study differs significantly from the results of Chen, primarily characterized by smaller lumbar range of motion reported by Chen. The reason is that in the study of Chen, the lumbar spine model constructed was L1-L5, and did not include the sacrum. During validation, the lower surface of L5 was constrained, which may lead to the point of torque applied closer to the model center of gravity, resulting in less motion in all directions of the lumbar spine. In contrast, the lumbar segments constructed in this study were L1-S5, and the surface constrained was the upper surface of S1. The site applied by the torque was relatively close to the center of gravity of the model, resulting in a relative increase in motion conditions. In any case, our study has cited previous in vivo and in vitro research results and ensured that the range of motion is within the effective reference range, meeting the requirements for finite element validation. (Fig. 2).
ROMs of adjacent vertebrae
Figure 3 shows that for the fusion segments, Group 1 experienced ROM decreases of 98.45%, 92.51% and 91.43%, respectively, and the decline in Model A was greater than that in Models B and C. Group 2 experienced decreases of 96.52%, 91.56% and 90.91%, respectively, and the decline in Model D was greater than that in Models E and F. The maximum ROM was 0.98°, and the minimum ROM was 0°.
Compared with those of the Intact model, the ROMs of the upper and lower adjacent segments showed varying degrees of decrease in FLEX, EXT and lateral bending movements; However, they showed varying degrees of increase in rotation movement: L1/L2 increased by 7.45%, 5.42% and 4.52% in Group 1 and 10.84%, 10.3% and 9.03% in Group 2, respectively. L5/S1 increased by 33.33%, 32.13% and 30.52% in Group 1 and by 45.38%, 44.58% and 42.17% in Group 2, respectively. The increases in the osteoporotic model were significantly greater than those in the normal bone model; the increases in the lower adjacent vertebrae were significantly greater than those in the upper adjacent vertebrae; and there was no significant difference between the increases in the UPSF and BPSF.
Adjacent vertebral disc pressure
As shown in Figs. 4, 5 and 6, after PSF, the IDP of all models increased compared with that of the normal models. The IDP values of L1/L2 in Group 1 were 3.62 MPa, 3.11 MPa, and 3.09 MPa, respectively, and those in Group 2 were 3.59 MPa, 3.10 MPa and 3.09 MPa, respectively. The IDP of L1/L2 in BPSF was significantly greater than that in UPSF (difference range: 13.65–14.64%). There was little difference in the L1/L2 IDPs between the two groups under the same PSF pattern and motion conditions (difference range: 0.32–0.84%). The IDP values of L5/S1 in Group 1 were 2.19 MPa, 1.86 MPa, and 1.83 MPa, respectively, and those in Group 2 were 2.19 MPa, 1.84 MPa, and 1.83 MPa, respectively. The IDP of L5/S1 was greater in BPSF than in UPSF (difference range: 15.07–16.44%). There was little difference in the L5/S1 IDP between the two groups under the same PSF pattern and movement conditions (difference range: 1.08–1.09%). With the same PSF method, the pressure of the L1/L2 disc was generally greater than that of the L5/S1 disc (difference range: 30.08–30.12%). Notably, the IDP of L1/L2 in BPSF was smaller than that in UPSF under EXT conditions.
Adjacent articular cartilage stress
As shown in Fig. 7; Table 2, after PSF, the stress of the articular cartilage in all models increased compared with that of the normal models. The stress values of the L1/L2 articular cartilage in Group 1 were 14.90 MPa、10.82MPa和10.79 MPa, respectively, and those in Group 2 were15.08 MPa, 10.94 MPa and 10.83 MPa, respectively. L1/L2 articular cartilage stress was significantly greater in BPSF than in UPSF (difference range: 24.35–27.07%), and the stress in L1–L2 cartilage in Group 2 was greater than that in Group 1 under the same PSF method and the same movement conditions (difference range:5.35–7.88%). The stress values of the L5/S1 articular cartilage in Group 1 were 12.88 MPa, 10.23 MPa, and 10.28 MPa, respectively, whereas those in Group 2 were 12.82 MPa, 10.12 MPa, and 10.14 MPa, respectively. The articular cartilage stress of L5/S1 in BPSF was significantly greater than that in UPSF (difference range: 20.19–21.06%). The L5/S1 cartilage stress of the two groups was not significantly different under the same PSF pattern or the same movement conditions (difference range: 0.47–1.36%). In the same group, the IDP of the same adjacent vertebra did not differ significantly between the left and right PSF modes (difference range: 0.20–0.49%).
Screw-rod system stress
To further assess the stability and feasibility of different PSF, we also analyzed the stress on the screw‒rod system, as shown in Figs. 8 and 9. In Group 1, the screw‒rod stress values were 69.35 MPa, 80.31 MPa, and 79.91 MPa, respectively, and in Group 2, they were 71.63 MPa, 86.84 MPa, and 86.97 MPa, respectively. The stress of the screw‒rod system in UPSF was significantly greater than that in BPSF (difference range: 15.23–21.42%). In the two groups of models, the maximum stress in the screw‒rod system occurred during EXT with right lateral fixation, with values of 21.94 MPa for Model C and 23.84 MPa for Model F, followed by EXT with left lateral fixation, with values of 21.65 MPa for Model B and 22.77 MPa for Model E. Moreover, the minimum stress occurred in the FLEX condition, which was 4.74 MPa for Model A and 5.19 MPa for Model C. In general, the stress of the screw‒rod system in the UPSF mode was much greater than that in the BPSF mode in both models. Under the same PSF method and the same movement conditions, the stress in the screw‒rod system of Group 2 was greater than that of Group 1 (difference range: 3.29–8.83%).
Discussion
ASD, a prevalent complication following lumbar spinal fusion surgery, has a multifaceted etiology. Various factors, such as patient age, bone health, the method of cage implantation, and the approach to internal fixation, can impact the development of ASD. This study investigated the mechanical behavior of different PSF methods from a biomechanical perspective, revealing the biomechanical impacts and underlying mechanisms of distinct bone conditions and PSF methods on the development of ASD. Six distinct internal fixation models were constructed, and the ROM, IDP, and stresses on the articular cartilage of the lumbar spine were nearly identical under both the left and right lateral fixation modes, further supporting the validity and efficacy of the model. These findings indicate that UPSF has potential benefits in alleviating intervertebral disc pressure and articular cartilage stress in adjacent vertebrae. The impact of osteoporosis on ASD may stem from the excessive activity induced by its low bone mineral density.
Generally, the ROM of lumbar segments less than 5° in all directions after internal fixation is deemed effective36. In the present study, the maximum ROM of the fused segment after PSF was 0.98°, reaching the standard criteria for the fusion rate37, which suggests that both the UPSF and the BPSF exhibit comparable efficacy in maintaining lumbar stability. However, BPSF appeared to have resulted in a more pronounced reduction in ROM, potentially leading to excessive stability of the lumbar spine, which might have been unnecessary for the patient. Interestingly, during rotational movement, both the upper and lower adjacent vertebrae showed excessive activity, and this increase in adjacent segment ROM is viewed as a compensatory overload phenomenon and is usually considered reasonable. However, Chen et al.20,38. suggested that excessive activity of the adjacent vertebrae may cause degeneration of the corresponding segments. In this study, The increase in adjacent segment ROM only occurs in axial rotation, while it decreases in flexion, extension, and lateral bending. This phenomenon is consistent with the findings of Yu et al.21. They noted that the decrease in adjacent segment ROM may be due to the fact that the experiment did not account for the influence of soft tissue stress. In addition, finite element simulation mainly models the immediate postoperative state, and the progressive changes of ROM in adjacent segments may not be immediately recognized, which may also have contributed to the reduction of ROM in adjacent vertebra during the simulation. Furthermore, we observed that the increase in total ROM in the osteoporotic model was significantly greater than that in the normal bone model and that the increase in ROM in the lower adjacent vertebrae was significantly greater than that in the upper segment. However, there was no significant difference in the increase in ROM between the UPSF group and the BPSF group. Consequently, we speculate that for long-segment fixation, the excessive activity of adjacent vertebrae is not strongly related to the PSF method itself but rather related to bone density and the alignment of the vertebrae. As bone density and strength decrease, the support and stability capabilities of osteoporotic vertebrae are reduced, leading to more passive motion after the implantation of internal fixation devices, and the lower vertebrae are also more likely to withstand the accumulation of loads and produce more movement. Therefore, for patients with osteoporosis, attention should be given to the implantation skills to avoid causing excessive activity in adjacent vertebrae. The choice between UPSF and BPSF does not have much differential effect on the ROM.
Furthermore, we observed that BPSF was more likely to lead to the enlargement of adjacent vertebral IDP (difference range: 13.65–16.44%). This observation aligns with the findings of Dujic et al.18. In particular, the increase in IDP resulting from BPSF was more pronounced in the upper adjacent segment than in the lower adjacent segment. We also found that the peak stress in the upper and lower adjacent discs occurred during FLEX, which is consistent with the observed phenomenon that the lumbar spine undergoes a greater ROM and experiences more concentrated forces during FLEX in everyday activities. In contrast, during EXT motion, the disc stress in UPSF was marginally greater than that in BPSF, which could also be attributed to the posterior positional characteristics of the rods or the existence of an anterior‒posterior tilt angle within the cage itself. The posterior positioning of the rod may offer supportive benefits during the EXT of the vertebral column, potentially alleviating some of the stress on the intervertebral discs. Conversely, the fusion device’s posteriorly lower design could lead to increased stress concentration on the intervertebral disc during FLEX. Furthermore, under identical bone quality and movement conditions, the stress values observed in the upper segment discs were greater than those in the lower discs. This finding aligns with clinical observations, indicating that the upper adjacent vertebrae are more susceptible to degeneration34,39,40,41, further suggesting that changes in IDP are an important factor in causing disc degeneration. Within the same PSF pattern and the same type of movement, the IDP under different bone conditions did not differ significantly (difference range: 0.32–1.09%), which indicates that osteoporosis does not contribute much to an additional increase in disc stress. In summary, in terms of the impact of stress magnitude in adjacent segment intervertebral discs on ASD, UPSF has the potential to prevent and delay the occurrence of ASD (especially in the upper adjacent vertebrae) in both osteoporotic and normal bone conditions.
In addition to IDP, the stress concentration on the articular cartilage caused by PSF surgery is also a significant contributor to ASD. In the present study, the stress in the articular cartilage was observed to follow a similar trend to that in the intervertebral discs; the stress in the BPSF group was greater than that in the UPSF group (difference range: 20.19–27.07%). Therefore, we believe that osteoporotic patients will undergo a similar process of ASD after PSF surgery as patients with normal bone quality. For patients requiring PSF surgery, the UPSF approach may be more reasonable regardless of their bone conditions.
Yu et al.21. and Tao et al.42 reported that although UPSF has a fusion effect similar to that of BPSF, it is more likely to lead to excessive stress on the screw‒rod system, increasing the risk of screw fracture. Similar results were obtained in this study in terms of stress changes with the screw‒rod system. In the UPSF mode, the stress of the screw‒rod system was greater than that in the BPSF mode under all working conditions (difference range: 15.23–21.42%). However, the peak stress value of the screw‒rod system (197.88 MPa) was significantly lower than the yield strength of the titanium alloy (825–895 MPa)43. Therefore, routine lumbar spine motion while under the UPSF mode is unlikely to result in a fracture of the screw‒rod system. Under osteoporotic conditions, the screw‒rod system is subject to greater stress, which may be related to insufficient vertebral support and the compensatory force of the screw‒rod after the bone mineral density decreases. Nevertheless, the peak stress experienced by the screw‒rod system is still within the tolerance range of the screw‒rod, and the tendency of the rod‒screw system to have higher stresses in the UPSF mode than in the BPSF mode remains unchanged. Consequently, the clinical selection of UPSF and BPSF is justified. However, for osteoporosis patients opting for UPSF, a thorough assessment of bone density should be conducted to ensure that the nail rod system will not break due to excessive stress.
There are several limitations in this study: (1) This study involved biomechanical analysis on different fixation methods for pedicle screws, but in clinical practice, cortical bone trajectory (CBT) screw (CBT) implantation can also be used for different clinical conditions and treatment strategies.(2) The study was purely a finite element simulation, which lacked clinical case follow-up as evidence to support it. Future research can investigate other methods of screw implantation, and long-term follow-up of clinical cases also can be considered to further explore the actual effects of different internal fixations on the neighboring vertebrae. (3) The study used CT data from a 28-year-old healthy male for modeling, which followed the single-sample validation model commonly used in finite element analysis. However, due to the anatomical individual differences in human bones (such as bone density distribution, geometric morphology variations, etc.), especially in the elderly, whose bone itself may have a certain degree of degeneration, hyperplasia, or osteoporosis, the model can only represent the lumbar spine condition at a similar age and with similar bone quality conditions. In addition, the construction of the pathology model is achieved by changing the model parameters, which may lead to some deviation of the simulation results from the real data. Therefore, future studies will consider using CT data from multiple groups of subjects of different age stages and different bone conditions for model construction, making the finite element simulation results more universal and representative.
Conclusion
In this study, FEA revealed that both UPSF and BPSF can meet the surgical stability standards. Compared with BPSF, UPSF has a weaker effect on the stress of adjacent vertebrae, reducing the incidence of ASD while effectively maintaining vertebral stability. The unilateral screw insertion method can preserve one normal segment for a future revision, greatly reducing surgical trauma and treatment costs. Consequently, for patients requiring PSF, opting for the UPSF method may be more beneficial, irrespective of the bone’s condition. Notably, when treating osteoporosis patients, a thorough assessment of bone density is needed, and personalized treatment should be adopted to avoid excessive adjacent vertebral activity and the risk of screw–rod breakage.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Cheng, C. et al. Spondylolisthesis with uncommon congenital deformity of L4-L5 vertebral fusion treated by oblique lumbar interbody fusion. World Neurosurg. 127, 222–226 (2019).
He, W. et al. Standalone oblique lateral interbody fusion vs. combined with percutaneous pedicle screw in spondylolisthesis. BMC Musculoskelet. Disord. 21 (1), 184 (2020).
Good, C. R. et al. Complications and revision rates in minimally invasive Robotic-Guided versus Fluoroscopic-Guided spinal fusions: the MIS refresh prospective comparative Study. Spine (Phila Pa. 1976). 46 (23), 1661–1668 (2021).
Kim, H., Chang, B. & Chang, S. Y. Pearls and pitfalls of oblique lateral interbody fusion: A comprehensive narrative Review. Neurospine 19 (1), 163–176 (2022).
Wang, W. et al. Oblique lateral interbody fusion stand-alone vs. combined with percutaneous pedicle screw fixation in the treatment of discogenic low back pain. Front. Surg. 9, 1013431 (2022).
Pierzchajlo, N. et al. Augmented reality in minimally invasive spinal surgery: A narrative review of available Technology. World Neurosurg. 176, 35–42 (2023).
Levy, H. A. et al. Answer to the letter to the editor of Z. Feng, et al. concerning "Unilateral versus bilateral pedicle screw fixation with anterior lumbar interbody fusion: a comparison of postoperative outcomes" by Levy HA, et al. (Eur Spine J [2024]: https://doi.org/10.1007/s00586-024-08412-5). Eur Spine J, 33(11), 4406–4407. (2024).
Xue, H., Tu, Y. & Cai, M. Comparison of unilateral versus bilateral instrumented transforaminal lumbar interbody fusion in degenerative lumbar diseases. Spine J. 12 (3), 209–215 (2012).
Xu, L. et al. Is unilateral pedicle screw fixation as effective as bilateral pedicle screw fixation in transforaminal lumbar interbody fusion: a meta-analysis of randomized controlled trials. Eur. Spine J. 32 (2), 700–711 (2023).
Pan, C. et al. Comparative Biomechanical analysis of unilateral, bilateral, and lateral pedicle screw implantation in oblique lumbar interbody fusion: A finite element Study. Bioeng. (Basel), 10(11). (2023).
Helgeson, M. D., Bevevino, A. J. & Hilibrand, A. S. Update on the evidence for adjacent segment degeneration and disease. Spine J. 13 (3), 342–351 (2013).
Ouchida, J. et al. Adjacent segment degeneration after Short-Segment lateral lumbar interbody fusion (LLIF). Biomed. Res. Int. 2022, 5161503. (2022).
Wang, W. et al. Biomechanical comparative analysis of effects of dynamic and rigid fusion on lumbar motion with different sagittal parameters: an in vitro study. Front. Bioeng. Biotechnol. 10, 943092 (2022).
Maragkos, G. A. et al. Factors predictive of adjacent segment disease after lumbar spinal Fusion. World Neurosurg. 133, e690–e694 (2020).
Alentado, V. J. et al. Predisposing characteristics of adjacent segment disease after lumbar Fusion. Spine (Phila Pa. 1976). 41 (14), 1167–1172 (2016).
Ramirez-Villaescusa, J. et al. Risk factors related to adjacent segment degeneration: retrospective observational cohort study and survivorship analysis of adjacent unfused segments. Br. J. Neurosurg. 33 (1), 17–24 (2019).
Mannion, A. F. et al. ISSLS prize winner: Long-term follow-up suggests spinal fusion is associated with increased adjacent segment disc degeneration but without influence on clinical outcome: results of a combined follow-up from 4 randomized controlled trials. Spine (Phila Pa. 1976). 39 (17), 1373–1383 (2014).
Dujic, M. K. et al. MRI assessment of the early disc degeneration two levels above fused lumbar spine segment: A comparison after unilateral and bilateral transforaminal lumbar interbody fusion (TLIF) Procedure. J. Clin. Med. 11(14) (2022).
Kim, T. et al. Comparison of adjacent segment degeneration after successful posterolateral fusion with unilateral or bilateral pedicle screw instrumentation: a minimum 10-year follow-up. Spine J. 13 (10), 1208–1216 (2013).
Chen, X. L. et al. Interspinous dynamic stabilization adjacent to fusion versus double-segment fusion for treatment of lumbar degenerative disease with a minimum follow-up of three years. Int. Orthop. 40 (6), 1275–1283 (2016).
Yu, Q. et al. Finite element analysis of Biomechanical investigation on diverse internal fixation techniques in oblique lumbar interbody fusion. BMC Musculoskelet. Disord. 25 (1), 804 (2024).
Khalid, S. I. et al. Association of osteopenia and osteoporosis with higher rates of pseudarthrosis and revision surgery in adult patients undergoing single-level lumbar fusion. Neurosurg. Focus. 49 (2), E6 (2020).
Liu, C. et al. Biomechanical assessment of different transforaminal lumbar interbody fusion constructs in normal and osteoporotic condition: a finite element analysis. Spine J. 24 (6), 1121–1131 (2024).
Chen, J. W. et al. The association between bone mineral density and proximal junctional kyphosis in adult spinal deformity: a systematic review and meta-analysis. J. Neurosurg. Spine. 39 (1), 82–91 (2023).
Li, C. et al. Comparison of Biomechanical effects of polyetheretherketone (PEEK) rods and titanium rods in lumbar long-segment instrumentation: a finite element study. Front. Bioeng. Biotechnol. 12, 1416046 (2024).
Xue, F. et al. Effects of cervical rotatory manipulation on the cervical spinal cord complex with ossification of the posterior longitudinal ligament in the vertebral Canal: A finite element study. Front. Bioeng. Biotechnol. 11, 1095587 (2023).
Deng, Z. et al. A finite element study of traditional Chinese cervical manipulation. Eur. Spine J. 26 (9), 2308–2317 (2017).
Chayer, M. et al. Biomechanical modelling of indirect decompression in oblique lumbar intervertebral fusions: A finite element study. Clin Biomech (Bristol, Avon), 120,106352. (2024).
Pan, H. et al. Finite element analysis of precise puncture vertebral augmentation in the treatment of different types of osteoporotic vertebral compression fractures. BMC Musculoskelet. Disord. 25 (1), 599 (2024).
Rycman, A., McLachlin, S. & Cronin, D. S. Comparison of numerical methods for cerebrospinal fluid representation and fluid-structure interaction during transverse impact of a finite element spinal cord model. Int. J. Numer. Method Biomed. Eng. 38 (3), e3570 (2022).
Ke, S. et al. The Biomechanical influence of facet joint parameters on corresponding segment in the lumbar spine: a new visualization method. Spine J. 21 (12), 2112–2121 (2021).
Chen, C. S. et al. Stress analysis of the disc adjacent to interbody fusion in lumbar spine. Med. Eng. Phys. 23 (7), 483–491 (2001).
Song, M. et al. Stress distribution of different lumbar posterior pedicle screw insertion techniques: a combination study of finite element analysis and Biomechanical test. Sci. Rep. 11 (1), 12968 (2021).
Bydon, M. et al. The incidence of adjacent segment disease after lumbar discectomy: A study of 751 patients. J. Clin. Neurosci. 35, 42–46 (2017).
Yamamoto, I. et al. Three-dimensional movements of the whole lumbar spine and lumbosacral joint. Spine (Phila Pa. 1976). 14 (11), 1256–1260 (1989).
Boustani, H. N. et al. Which postures are most suitable in assessing spinal fusion using radiostereometric analysis?. Clin Biomech (Bristol, Avon) 27(2), 111–116 (2012).
Wang, L. et al. Finite element analysis of polyethylene wear in total hip replacement: A literature review. Proc. Inst. Mech. Eng. H. 233 (11), 1067–1088 (2019).
Kamalanathan, V. et al. Lordosis recreation with PLIF Surgery-What is the influence on adjacent segment Lordosis? An observational study of radiological alignment Change. Spine (Phila Pa. 1976). 45 (17), 1178–1184 (2020).
Zhao, Y. et al. Adjacent segment disease after anterior cervical decompression and fusion: analysis of risk factors on X-ray and magnetic resonance imaging. Chin. Med. J. (Engl). 127 (22), 3867–3870 (2014).
Choi, K. C. et al. Changes in the adjacent segment 10 years after anterior lumbar interbody fusion for low-grade isthmic spondylolisthesis. Clin. Orthop. Relat. Res. 472 (6), 1845–1854 (2014).
Wang, W. et al. Effects of dynamic and rigid implantation on Biomechanical characteristics of different sagittal alignment lumbar after single- or double-level spinal fixations: a finite-element modeling study. Eur. J. Med. Res. 28 (1), 583 (2023).
Tao, E. et al. Biomechanical changes of oblique lumbar interbody fusion with different fixation techniques in degenerative spondylolisthesis lumbar spine: a finite element analysis. BMC Musculoskelet. Disord. 25 (1), 664 (2024).
Wu, J. et al. Application of dual-trajectory screws in revision surgery for lumbar adjacent segment disease: a finite element study. J. Orthop. Surg. Res. 17 (1), 427 (2022).
Funding
This research was funded by: the National Natural Science Foundation of China (No. 81973871, 31900942), Shanghai Clinical Research Center for Musculoskeletal Health (No. 20MC1920600), Clinical Research Plan of SHDC (SHDC2020 CR1051B), Boca Raton Regional Hospital Foundation and the Helene and Stephen Weicholz Foundation.
Author information
Authors and Affiliations
Contributions
Linling Zhang: Experimented, and wrote the main manuscript. Zhongxiang Yu: Conducted data collection and analysis. Xuanzong Zhang: Revised the manuscript. Kuan Wang: Provided technical support. Hongsheng Zhan and Yongfang Zhao: Provide experimental resources. Maohua Lin and Frank Vrionis: Supervise the experimental process and revised the manuscript. Huihao Wang: Designed the study, processed the experimental data, and revised the manuscript. Linling Zhang and Zhongxiang Yu contributed equally to this work. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This research protocol was reviewed and approved by the Ethics Committee of Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine (Ethics Approval number: 2024-1446-029-01).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, L., Yu, Z., Zhang, X. et al. Finite element analysis of pedicle screw fixation biomechanics and adjacent segment degeneration in varied bone conditions. Sci Rep 15, 19047 (2025). https://doi.org/10.1038/s41598-025-03377-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-03377-x
Keywords
This article is cited by
-
Comparative study by FEM of different liners of a transfemoral amputated lower limb
Scientific Reports (2025)
-
Cadmium-induced nucleus pulposus derived mesenchymal stem cells apoptosis via MAPK signaling pathway contributes to IVD degeneration
In Vitro Cellular & Developmental Biology - Animal (2025)
-
Biomechanical optimization of pedicle screw trajectories in osteoporotic lumbar fusion: finite element analysis and validation of robotic-assisted implementation
Journal of Robotic Surgery (2025)