Abstract
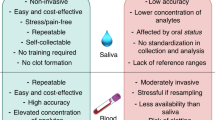
Myeloperoxidase (MPO) is a key element of host defense against pathogens but is also implicated in disease. To explore whether MPO contributes to the postulated relationship between oral inflammation and obesity, the concentration of MPO and its activity were studied in saliva of obese and non-obese individuals. Whole mixed unstimulated saliva was obtained from 44 apparently healthy women without (n = 25) and with (n = 19) simple obesity. MPO concentration in saliva was measured by immunoassay; salivary peroxidation and chlorination activities were assessed with tetramethylbenzidine- and aminophenyl-fluorescein-based assays, respectively. Salivary MPO concentrations were found to be significantly higher in obese than in non-obese women and could distinguish these two populations. However, it did not correlate with total salivary peroxidation activity (TSPA), which was lower in obese women. MPO chlorinating activity was not detected in pure saliva in neither of the groups. The subjects’ body weight, waist-to-hip ratio and the concentration of pro-inflammatory cytokines in saliva correlated positively with MPO concentration, but negatively with TSPA. In conclusion, MPO concentration in saliva is significantly increased in obesity but does not correlate with salivary peroxidation activity, which is lower in the obese. It may indicate that obesity impairs the ability of saliva to mitigate oxidative stress associated with inflammation.
Similar content being viewed by others
Introduction
The oral mucosa and saliva constitute the first line of defense against potentially harmful environmental factors. The peroxidase system in saliva consists of enzymes with peroxidative activity, hydrogen peroxide (H2O2) and the thiocyanate ion (SCN−)1. Salivary peroxidases catalyze the oxidation of thiocyanate to hypothiocyanite, which has strong antimicrobial activity2. The reaction requires H2O2 that is produced primarily by salivary glands and neutrophils, but also some bacteria. Thus, peroxidases prevent bacterial overgrowth by generating hypothiocyanite and remove excess bacterial H2O2, which can be toxic for tissues at high concentrations3,4. Other potential substrates for peroxidases include chloride, bromide, or iodide, which give rise to hypochlorite, hypobromite and hypoiodite, respectively5.
Sialoperoxidase (SPO) and myeloperoxidase (MPO) are the two main peroxidases found in the oral cavity. SPO is secreted by salivary glands and MPO is released by neutrophils entering the oral cavity with the gingival fluid. The proportions of both peroxidases are variable and depend on age, diet, smoking, and the presence of inflammation in the oral cavity2,6,7,8.
MPO is a high molecular weight protein produced by neutrophils and stored in their azurophilic granules until required9. Upon neutrophil activation, MPO is sequestered to phagolysosomes and becomes involved in the killing of phagocytosed bacteria. During this process, however, some of MPO may leak into adjacent tissues and adversely modify tissue proteins5,10,11. Thus, increased levels of MPO in serum and other bodily fluids usually reflect an underlying inflammatory condition, and as such have been detected in a number of inflammatory pathologies12,13,14,15. These include low-grade inflammation associated with obesity16,17,18. It has been found that visceral adipose tissue of obese individuals contains increased numbers of neutrophils that cause an imbalance between po-inflammatory and immunoregulatory T cells and fuel sustained inflammation19. Increased systemic levels of uncontained MPO may lead to unfavorable effects through MPO downstream products. In this respect, MPO is heavily implicated in oxidation of LDL and the resultant involvement in endothelial dysfunction and atherosclerosis14.
We have previously observed that MPO concentration in saliva correlated significantly with the body mass index (BMI) and salivary levels of pro-inflammatory cytokines IL-6 and TNFα20. We also found that even in the absence of typical obesity-associated diseases, the saliva from apparently healthy obese individuals contained increased concentrations of many inflammatory mediators21. The most notable increases were seen in the levels of adipose-tissue derived serpin A12 (Vaspin) and cytokines of the TNFα family, which reflected probably evolving insulin resistance and smoldering systemic inflammation, respectively. Moreover, although obese and non-obese individuals analyzed had similar and seemingly adequate oral hygiene practices, the levels of pro-inflammatory cytokines in saliva in the obese correlated positively with the magnitude of plaque build-up21.
Given the complex relationship between inflammation, obesity and oral health22, in the present study we measured the level and activity of MPO in the saliva of obese individuals, testing the hypothesis that obesity per se modifies these parameters.
Methods
Materials
Unless stated otherwise, all reagents were from Merck (Darmstadt, Germany).
Study subjects
This retrospective study involving human participants was performed in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Bioethics Committee of Poznań University of Medical Science approved this study (No 189/14). Informed consent was obtained from all individual participants included in the study.
The analyzed saliva samples were those collected previously21 from consenting healthy volunteers. These were 19 women with simple obesity (as defined by BMI ≥ 30 kg/m2)and 25 women without obesity matched for age. The obese individuals were selected from a cohort of 50 candidates screened initially for eligibility. The reasons for exclusion were co-morbidities (most often hypertension, diabetes, hypothyroidism, and allergies) and/or taking medication known to affect the output of saliva23. Because only a few of the remaining candidates were men, the study group was limited to women to maintain homogeneity. Detailed demographic and anthropometric characteristics of the subjects as well as parameters of their oral health were presented previously21. Selected data pertinent to the present study is presented in Table 1. Importantly, the subjects did not differ significantly in terms of dental status, oral hygiene habits, and salivary pH. However, obese people tended to have reduced salivary flow after stimulation, as well as increased plaque formation and slightly diminished gingival condition.
Saliva collection
The samples of were collected, processed, and stored as recommended24,25,26. Briefly, the samples of whole mixed saliva were collected by passive unstimulated drooling over 20 min, as detailed before27. The samples were centrifuged (10,000 µg for 5 min at 4 °C), batched, stored at – 80 °C, and freshly thawed for each assay.
Saliva analysis
All patients’ samples were assessed in duplicates. Salivary concentrations of MPO protein were measured using a DuoSet Elisa Development System (R&D Systems, Bio-Techne, Minneapolis, MN, USA). To ensure accurate performance of the immunoassay in the salivary matrix, the representative samples of saliva were first tested for dilution and recovery. The optimal dilutions of saliva were determined so that the measurements were performed in the dynamic range of the assay. We found that the analyte recovery under these conditions was > 87% and the assay sensitivity and inter-assay variability were 37 pg/mL and 9.2%, respectively.
Total salivary peroxidation activity (TSPA) was measured according to Suzuki et al.28 and Pulli et al.29. Briefly, 10 µL of saliva was mixed with 80 µL of 0.75 mM H2O2 and 110 µL of a solution containing 2.9 mM 3,3’,5,5’-tetramethylbenzidine (TMB), 14.5% (v/v) dimethyl sulfoxide (DMSO) and 150 mM sodium phosphate, pH 5.4. After 5 min of incubation at 37 °C, the reaction was stopped by adding 50 µL of 2 M sulfuric acid, and the optical density was measured at 450 nm.
Salivary chlorination activity was measured using a method modified from the methods described by Pulli et al.29 and Setsukinai et al.30. To this end, the sample of saliva was diluted 1:120 in PBS and then 20 µL of it was mixed with 20 µL of MPO (1000 ng/mL) in a 0.1 M sodium phosphate/150 mM NaCl buffer (pH 7.4) and 40 µL of 20 µM 3’-(p-aminophenyl)-fluorescein (APF) in 0.1% DMSO. The mixture was incubated for 5 min at room temperature, and then 40 µL of 200 µM hydrogen peroxide in a 0.1 M sodium phosphate/150 mM NaCl buffer (pH 7.4) was added. The fluorescence was measured at baseline and after 20 min of incubation at 37 °C using wavelengths of 490 nm and 515 nm for excitation and emission, respectively, and the data were expressed as relative fluorescence units (RFU).
The peroxidation and chlorination assays were validated by measuring these reactions in response to a serious of known doses of exogenous leukocyte-derived MPO.
Statistical analysis
Statistical analysis was performed using GraphPad Prism, version 10.3.0 (GraphPad Software, San Diego, CA, USA). Data were analyzed for normality of distribution using the Shapiro-Wilk test and then analyzed using either Student’s t-test with Welch correction or Mann-Whitney U test, for normally and non-normally distributed data, respectively. If required, ANOVA was used. Correlations were analyzed by non-parametric Spearman correlation. A P value < 0.05 was considered statistically significant.
Results
Salivary MPO concentrations in obesity
Compared to non-obese women (BMI < 30 kg/m2), women with BMI-defined obesity (BMI ≥ 30 kg/m2) had significantly higher MPO concentrations in saliva (Fig. 1A). Although there was some overlap between MPO levels in both groups, the mean MPO level in the saliva of obese women was almost 60% higher than that in non-obese women. The effect size expressed as Cohen’s d was 1.246, which is considered large31. Moreover, MPO levels in the saliva could discriminate between the two groups of subjects, which, with a cut-off value of 355 ng/mL, resulted in a reasonable sensitivity of 65% and high specificity of 92% (Fig. 1B).
Salivary MPO concentration in obesity. (A) The concentration of MPO in whole mixed unstimulated saliva from obese and non-obese subjects. The data were compared with the Mann-Whitney test and presented as median and interquartile ranges with individuals values indicated; (B) Receiver operating characteristic (ROC) for MPO concentration in individuals with and without obesity. The cut-off point that discriminated the groups was estimated to be 350 ng/mL. Abbreviation: MPO myeloperoxidase.
To ensure that the difference in MPO concentration was not caused by changes in salivary output, the MPO levels were normalized per saliva flow (Table 1). These were found to be (median; interquartile range, ng/mL/min): 1163 (864–1782) and 751 (312–1096) in obese and non-obese individuals, respectively. This difference was still highly significant (p = 0.0076).
Salivary peroxidation and chlorination activity
Since MPO exerts both peroxidation and chlorinating effects, we then measured these activities in the exemplary samples of saliva. We found that neat saliva exhibited considerable peroxidative activity, which decreased with serial saliva dilutions down to the level seen in the plain buffer (Fig. 2A).
MPO activity in saliva. Total salivary peroxidation activity (A) and chlorinating activity (B) was measured in neat and serially diluted example saliva from 4 healthy individuals and compared to those in control buffer. The data were analyzed with the Browne-Forsythe and Welch ANOVA and expressed as means ± SD. (C) Comparison of chlorination activity in samples of saliva at different dilutions spiked with excess MPO (final concentration 1000 ng/mL). Example saliva was from 4 healthy individuals. The data were analyzed with multiple t-tests and expressed as means ± SD. Abbreviations: MPO myeloperoxidase, OD optical density, RFU relative fluorescence units.
In contrast, the chlorination activity in samples of pure saliva was significantly lower than in the MPO-containing control buffer (Fig. 2B). However, it increased with serial dilutions of saliva and reached the control level only at 128-fold dilution. These data indicated that saliva components might have interfered with chlorination activity and hypochlorite formation under the assay conditions. To test this possibility, we added a known amount of bacterial MPO to a series of diluted saliva (to give a final MPO concentration of 1000 ng/mL) and then measured the chlorination activity (Fig. 2C) These experiments demonstrated that, in contrast to the strong chlorinating effect of MPO added to the control buffer, MPO showed no chlorinating activity when added to pure saliva, and only partially regained this activity when the saliva was diluted at least 128 times. Therefore, in subsequent analyses we focused on the peroxidative effect of saliva.
Salivary peroxidation activity in obesity
There was no significant correlation between salivary MPO concentration and TSPA in the individuals examined (Fig. 3A). Furthermore, TSPA was found to be significantly higher in non-obese women than in obese women (Fig. 3B). The effect size of this difference was considered medium-to-large (Cohen’s d = 0.672). Interestingly, based on the peroxidative activity produced by exogenous MPO at doses corresponding to those found in saliva, the fraction of TSPA that could be attributed to MPO was estimated to be lower in the non-obese than in the obese: (mean ± SD) 33 ± 23% vs. 61 ± 26%, respectively.
MPO concentration and total peroxidation activity in saliva. (A) Correlation between salivary concentration of MPO and TSPA in all individuals examined. The data were analyzed using the Spearman test; (B) TSPA in obese and non-obese subjects. The data were compared with the Mann-Whitney test and presented as median and interquartile ranges with individuals values indicated. Abbreviations: MPO myeloperoxidase, OD optical density.
Salivary peroxidation activity vs. MPO concentration
To clarify these seemingly contradictory results, MPO concentration and TSPA were related to other parameters (Fig. 4). Indeed, it turn out that anthropometric measures (weight, BMI, and waist-to-heap-ratio) correlated positively with MPO levels, but negatively with TSPA (Fig. 4A). Accordingly, the same pattern of correlation was found for salivary levels of several mediators previously identified as differentially expressed in obesity21. These included proinflammatory cytokines, adhesion molecules and adipokines (Fig. 4B and C).
Different pattern of correlations between salivary MPO and TSPA with other parameters. Salivary MPO and TSPA in all patients examined were correlated with anthropometric parameters (A) and with salivary concentrations of pro-inflammatory mediators (B), as well with adipokines and endothelial adhesion molecules (C). Spearman test was used to create heatmaps for the correlation matrix with the colors and numbers representing the coefficients of non-parametric Spearman correlation. Abbreviations: MPO myeloperoxidase, TSPA total salivary peroxidase activity, BMI body mass index, WHR waist-to-heap ratio, TNFα tumor necrosis factor α, TNFR1 tumor necrosis factor receptor 1, PTX-3 pentraxin-3; sICAM-1 soluble intercellular adhesion molecule-1, serpin A12 serine protease inhibitor A12 (alias Vaspin = Visceral adipose-specific serpin). All parameters used for correlation analysis with MPO and TSPA were measured in our study21.
Discussion
The main finding of the present study is that in women with simple obesity, without any comorbidities, MPO concentration in saliva is increased, but at the same time total salivary peroxidative activity (TSPA) is decreased. The increase in MPO concentration in saliva most likely reflects the systemic inflammation associated with obesity. The contribution of local inflammation is probably less significant, because compared to non-obese women, those with obesity had only slightly increased plaque accumulation and worse gingival condition, but no overt periodontal disease21.
The observed increase in MPO concentration corresponds to the previously reported increase in the level of other inflammatory mediators in the saliva of obese people21,32,33. However, the fact that it was not accompanied by an increase in TSPA is surprising. One could expect that the presence of increased amount of MPO in saliva would lead to a parallel increase in TSPA. There may a number of potential reasons for this discrepancy. First, it may be due to obesity-induced reduction in SPO production by the salivary glands. Although SPO levels were not directly measured in this study, it is well recognized that obesity is associated with reduced output of saliva, especially in response to stimulation21,34,35. It has previously been attempted to use dapsone, an inhibitor of MPO, to assess how much of the salivary peroxidation activity is contributed by SPO and MPO36. Interpretation of these experiments became difficult, however, when it turned out that SPO was even more sensitive to dapsone inhibition than MPO36.
Second, the differences in TSPA can be related to the availability of substrates for SPO and MPO, i.e. H2O2 and thiocyanate1. Their limiting effect on TSPA may depend not only on the amount of saliva released, but also on the diet, the composition of the oral microflora, and the activity of other enzymes such as catalase and superoxide dismutase (SOD), or the presence of ceruloplasmin37, which may act as a MPO inhibitor38. In the analyzed group, however, we did not detect significant differences in SOD levels and catalase activity between obese and non-obese people21.
Third, the activity of MPO can be affected by variations in MPO expression levels dependent on polymorphisms in the MPO promoter region15. They can modulate the binding of transcription factors and the resultant rate of gene transcription39,40. Moreover, it has been reported that even certain polymorphisms located in the MPO gene non-coding regions could affect MPO activity41, possibly through changes in the final protein conformation.
Fourth, it has been suggested that salivary peroxidation activity may be affected by estrogen levels42,43. Although all subjects in the present study were of the same sex (young women), the study did not control for the potential influence of changes in estrogen levels related to the menstrual cycle or the use of contraceptives.
Finally, it may be that saliva does not provide the optimal pH for MPO activity. MPO appears to be most effective at pH 5–644, while the pH of unstimulated saliva in both non-obese and obese people is 6.7–7.1 and increases to 7.0–7.5 after stimulation21.
Moreover, with some surprise, we found that there was no significant MPO chlorination activity in the tested saliva samples. Although the concentration of chloride in saliva is high, thiocyanate appears to be a preferential substrate for MPO2. As we showed that serial dilution of saliva led to the gradual emergence of MPO chlorinating activity, it can be hypothesized that dilution resulted in a decrease in thiocyanate availability while chloride levels were still high, allowing MPO activity to occur. MPO has been implicated in promoting atherosclerosis as chlorotyrosine, a specific product of MPO-generated oxidation, was detected at increased levels in human atherosclerotic plaques45,46. Thus, the absence of MPO-dependent chlorinating activity in healthy individuals and in those with uncomplicated obesity may indicate that under these conditions saliva protects oral tissues from unfavorable modifications caused by MPO-generated halogenating oxidants. Consequently, the detection of MPO-dependent chlorinating activity in saliva may mean that the protective potential of saliva in this respect has been exhausted.
Once MPO was recognized as being at the intersection of immunity and disease, attempts were made to link salivary MPO to oral health (reviewed in2). Although no clear associations were found in this respect, this was not interpreted as a lack of significance of MPO, but rather as the complexity of the oral microenvironment in which multiple defense systems coexist. The present study adds to this complexity by showing that obesity may confound the relationship between salivary MPO concentration and salivary peroxidative activity. It also raises an interesting question of whether the relationship between obesity, inflammation, and oral health22 is related to increased MPO release or rather to insufficient rise in salivary peroxidative activity.
Obvious limitations of this study include the small number of obese patients, their relatively narrow age range, and the lack of men in this group. However, as explained previously21, this is related to the fact that the study aimed to recruit obese patients without apparent comorbidities, such as hypertension, diabetes, or hypothyroidism, and taking no medication that may affect salivary flow. While these features of the subjects could be viewed as advantages of the study, such patients constitute only the minority in the obese population. Furthermore, the subjects were recruited from individuals seeking weight-loss treatment for their obesity; which may suggest that they expressed a greater-than-average level of health consciousness and oral care. Nevertheless, our previous analysis showed that the profile of cytokines and adipokines identified in this small group of subjects was also present in an unselected cohort of obese individuals21. In summary (Fig. 5), our observations suggest that measuring MPO concentration alone, without simultaneous assessment of MPO activity, is incomplete and cannot provide a complete picture of the role of MPO in the oral cavity. Therefore, future studies should measure these two parameters in parallel, and preferably assess them sequentially, rather than only on the basis of a single-point measurement.
Data availability
Data generated are available on reasonable request (koryb@ump.edu.pl).
References
Tenovuo, J. & Pruitt, K. M. Relationship of the human salivary peroxidase system to oral health. J. Oral Pathol. 13, 573–584. https://doi.org/10.1111/j.1600-0714.1984.tb01459.x (1984).
Ihalin, R., Loimaranta, V. & Tenovuo, J. Origin, structure, and biological activities of peroxidases in human saliva. Arch. Biochem. Biophys. 445, 261–268. https://doi.org/10.1016/j.abb.2005.07.004 (2006).
Hänström, L., Johansson, A. & Carlsson, J. Lactoperoxidase and thiocyanate protect cultured mammalian cells against hydrogen peroxide toxicity. Med. Biol. 61, 268–274 (1983).
Tenovuo, J. & Larjava, H. The protective effect of peroxidase and thiocyanate against hydrogen peroxide toxicity assessed by the uptake of [3 h]-thymidine by human gingival fibroblasts cultured in vitro. Arch. Oral Biol. 29, 445–451. https://doi.org/10.1016/0003-9969(84)90025-6 (1984).
Arnhold, J. & Malle, E. Halogenation activity of mammalian Heme peroxidases. Antioxid. (Basel). 11. https://doi.org/10.3390/antiox11050890 (2022).
Khan, A. A., Rahmani, A. H., Aldebasi, Y. H. & Aly, S. M. Biochemical and pathological studies on peroxidases—an updated review. Glob J. Health Sci. 6, 87–98. https://doi.org/10.5539/gjhs.v6n5p87 (2014).
de Oliveira, F. K., Santos, L. O. & Buffon, J. G. Mechanism of action, sources, and application of peroxidases. Food Res. Int. 143, 110266. https://doi.org/10.1016/j.foodres.2021.110266 (2021).
Courtois, P. Oral peroxidases: from antimicrobial agents to ecological actors (review). Mol. Med. Rep. 24, 12139. https://doi.org/10.3892/mmr.2021.12139 (2021).
Hansson, M., Olsson, I. & Nauseef, W. M. Biosynthesis, processing, and sorting of human myeloperoxidase. Arch. Biochem. Biophys. 445, 214–224. https://doi.org/10.1016/j.abb.2005.08.009 (2006).
Aratani, Y. Myeloperoxidase: its role for host defense, inflammation, and neutrophil function. Arch. Biochem. Biophys. 640, 47–52. https://doi.org/10.1016/j.abb.2018.01.004 (2018).
Kargapolova, Y. et al. The enzymatic and non-enzymatic function of myeloperoxidase (mpo) in inflammatory communication. Antioxid. (Basel). 10. https://doi.org/10.3390/antiox10040562 (2021).
Lockhart, J. S. & Sumagin, R. Non-canonical functions of myeloperoxidase in immune regulation, tissue inflammation and cancer. Int. J. Mol. Sci. 23 https://doi.org/10.3390/ijms232012250 (2022).
Siraki, A. G. The many roles of myeloperoxidase: from inflammation and immunity to biomarkers, drug metabolism and drug discovery. Redox Biol. https://doi.org/10.1016/j.redox.2021.102109 (2021). 46,102109.
Frangie, C. & Daher, J. Role of myeloperoxidase in inflammation and atherosclerosis (review). Biomed. Rep. 16, 53. https://doi.org/10.3892/br.2022.1536 (2022).
Strzepa, A., Pritchard, K. A., Dittel, B. N. Myeloperoxidase: a new player in autoimmunity. Cell. Immunol. 317, 1–8. https://doi.org/10.1016/j.cellimm.2017.05.002 (2017).
Olza, J. et al. Myeloperoxidase is an early biomarker of inflammation and cardiovascular risk in prepubertal obese children. Diabetes Care. 35, 2373–2376. https://doi.org/10.2337/dc12-0614 (2012).
Gómez García, A., Rivera Rodríguez, M., Gómez Alonso, C., Rodríguez Ochoa, D. Y. & Alvarez Aguilar, C. Myeloperoxidase is associated with insulin resistance and inflammation in overweight subjects with first-degree relatives with type 2 diabetes mellitus. Diabetes Metab. J. 39, 59–65. https://doi.org/10.4093/dmj.2015.39.1.59 (2015).
Qaddoumi, M. G. et al. Investigating the role of myeloperoxidase and angiopoietin-like protein 6 in obesity and diabetes. Sci. Rep. 10, 6170. https://doi.org/10.1038/s41598-020-63149-7 (2020).
Shantaram, D. et al. Obesity-associated microbiomes instigate visceral adipose tissue inflammation by recruitment of distinct neutrophils. Nat. Commun. 15, 5434. https://doi.org/10.1038/s41467-024-48935-5 (2024).
Nijakowski, K. et al. Increased myeloperoxidase concentrations in saliva could reflect increased body mass and oral microinflammation. Front. Biosci. (Landmark Ed.) 28, 168. https://doi.org/10.31083/j.fbl2808168 (2023).
Lehmann-Kalata, A. et al. Salivary fingerprint of simple obesity. Cytokine 110, 174–180. https://doi.org/10.1016/j.cyto.2018.05.006 (2018).
Jepsen, S., Suvan, J. & Deschner, J. The association of periodontal diseases with metabolic syndrome and obesity. Periodontol 2000. 83 (125 – 53). https://doi.org/10.1111/prd.12326 (2020).
Villa, A. et al. World workshop on oral medicine VI: a systematic review of medication-induced salivary gland dysfunction. Oral Dis. 22, 365–382. https://doi.org/10.1111/odi.12402 (2016).
Veerman, E. C. I., Vissink, A., Wong, D. T. & van Amerongen, N. A. Processing and storage of saliva samples. In: (ed Wong, D. T.) Salivary Diagnostics. Ames: Wiley-Blackwell; 69–76. (2008).
Vissink, A., Wolff, A. & Veerman, E. C. I. Saliva collectors. In: (ed Wong, D. T.) Salivary Diagnostics. Ames: Wiley-Blackwell; 37–59. (2008).
Mortazavi, H., Yousefi-Koma, A. A. & Yousefi-Koma, H. Extensive comparison of salivary collection, transportation, preparation, and storage methods: a systematic review. BMC Oral Health. 24, 168. https://doi.org/10.1186/s12903-024-03902-w (2024).
Surdacka, A. et al. Relation of salivary antioxidant status and cytokine levels to clinical parameters of oral health in pregnant women with diabetes. Arch. Oral Biol. 56, 428–436 (2011).
Suzuki, K., Ota, H., Sasagawa, S., Sakatani, T. & Fujikura, T. Assay method for myeloperoxidase in human polymorphonuclear leukocytes. Anal. Biochem. 132, 345–352. https://doi.org/10.1016/0003-2697(83)90019-2 (1983).
Pulli, B. et al. Measuring myeloperoxidase activity in biological samples. PLoS One. 8, e67976. https://doi.org/10.1371/journal.pone.0067976 (2013).
Setsukinai, K., Urano, Y., Kakinuma, K., Majima, H. J. & Nagano, T. Development of novel fluorescence probes that can reliably detect reactive oxygen species and distinguish specific species. J. Biol. Chem. 278, 3170–3175. https://doi.org/10.1074/jbc.M209264200 (2003).
Sullivan, G. M. & Feinn, R. Using effect size-or why the P value is not enough. J. Grad Med. Educ. 4, 279–282. https://doi.org/10.4300/jgme-d-12-00156.1 (2012).
Lehmann, A. P. et al. Characteristics of salivary inflammation in obesity. Pol. Arch. Intern. Med. 130, 297–303. https://doi.org/10.20452/pamw.15186 (2020).
Ostrowska, L., Gornowicz, A., Pietraszewska, B., Bielawski, K. & Bielawska, A. Which salivary components can differentiate metabolic obesity? PLoS One. 15, e0235358. https://doi.org/10.1371/journal.pone.0235358 (2020).
Modéer, T., Blomberg, C. C., Wondimu, B., Julihn, A. & Marcus, C. Association between obesity, flow rate of whole saliva, and dental caries in adolescents. Obes. (Silver Spring). 18, 2367–2373. https://doi.org/10.1038/oby.2010.63 (2010).
Maruyama, K. et al. The impact of masticatory ability as evaluated by salivary flow rates on obesity in Japanese: the toon health study. Obes. (Silver Spring). 23, 1296–1302. https://doi.org/10.1002/oby.21071 (2015).
Thomas, E. L., Jefferson, M. M., Joyner, R. E., Cook, G. S. & King, C. C. Leukocyte myeloperoxidase and salivary lactoperoxidase: identification and quantitation in human mixed saliva. J. Dent. Res. 73, 544–555. https://doi.org/10.1177/00220345940730021001 (1994).
Delmonico, L. et al. Proteomic profile of saliva and plasma from women with impalpable breast lesions. Oncol. Lett. 12, 2145–2152. https://doi.org/10.3892/ol.2016.4828 (2016).
Chapman, A. L. et al. Ceruloplasmin is an endogenous inhibitor of myeloperoxidase. J. Biol. Chem. 288, 6465–6477. https://doi.org/10.1074/jbc.M112.418970 (2013).
Hoy, A. et al. Serum myeloperoxidase concentration in a healthy population: biological variations, familial resemblance and new genetic polymorphisms. Eur. J. Hum. Genet. 9, 780–786. https://doi.org/10.1038/sj.ejhg.5200702 (2001).
Piedrafita, F. J. et al. An Alu element in the myeloperoxidase promoter contains a composite sp1-thyroid hormone-retinoic acid response element. J. Biol. Chem. 271, 14412–14420. https://doi.org/10.1074/jbc.271.24.14412 (1996).
Chevrier, I., Tregouet, D. A., Massonnet-Castel, S., Beaune, P. & Loriot, M. A. Myeloperoxidase genetic polymorphisms modulate human neutrophil enzyme activity: genetic determinants for atherosclerosis? Atherosclerosis 188, 150–154. https://doi.org/10.1016/j.atherosclerosis.2005.10.012 (2006).
Pal, T. & Bhattacharyya, A. K. Cyclic changes in salivary lactate dehydrogenase, peroxidase and leucine aminopeptidase during menstrual cycle. Indian J. Exp. Biol. 27, 695–698 (1989).
Tenovuo, J., Laine, M., Söderling, E. & Irjala, K. Evaluation of salivary markers during the menstrual cycle: peroxidase, protein, and electrolytes. Biochem. Med. 25, 337–345. https://doi.org/10.1016/0006-2944(81)90092-2 (1981).
Arnhold, J. The dual role of myeloperoxidase in immune response. Int. J. Mol. Sci. 21, 8057. https://doi.org/10.3390/ijms21218057 (2020).
Hazen, S. L. & Heinecke, J. W. 3-chlorotyrosine, a specific marker of myeloperoxidase-catalyzed oxidation, is markedly elevated in low density lipoprotein isolated from human atherosclerotic intima. J. Clin. Invest. 99, 2075–2081. https://doi.org/10.1172/jci119379 (1997).
Nicholls, S. J. & Hazen, S. L. Myeloperoxidase and cardiovascular disease. Arterioscler. Thromb. Vasc Biol. 25, 1102–1111. https://doi.org/10.1161/01.ATV.0000163262.83456.6d (2005).
Acknowledgements
The authors wish to acknowledge the volunteers who participated in this study.
Funding
The authors did not receive support from any external organization for the submitted work.
Author information
Authors and Affiliations
Contributions
KK – conceptualization, data curation, methodology, validation, formal analysis, writing – review & editing, supervision; AS – methodology, resources; funding acquisition, supervision; AL – investigation, data curation, validation; JZS – investigation, formal analysis; J.W.- conceptualization, writing original draft, visualization.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study was approved by the Bioethics Committee of the Poznan University of Medical Sciences (decision #189/14) and was performed in accordance with the Helsinki Declaration. Informed consent was obtained from all individual participants included in the study.
Authors’ consent
All authors have read the manuscript and have agreed to submit it in its current form for consideration for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Korybalska, K., Surdacka, A., Lehmann, A. et al. Increased MPO concentration but decreased peroxidase activity in saliva of obese women. Sci Rep 15, 18716 (2025). https://doi.org/10.1038/s41598-025-03565-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-03565-9