Abstract
HIV-positive patients often experience increased oral and dental health challenges due to compromised immunity, long-term antiretroviral therapy (ART), stigma, and discrimination. These factors can lead to reduced access to oral care, delayed treatment, and exacerbation of oral diseases, which may further contribute to disease transmission among close contacts and healthcare providers. This study aimed to assess the prevalence of oral health issues, evaluate the decayed, missing, and filled teeth (DMFT) index, and identify factors associated with poor oral health outcomes among HIV-positive patients in Tabriz, Iran, in 2024. This cross-sectional study included 134 HIV-positive patients referred to a counseling center. Demographic and clinical information was obtained from the counseling center’s software. Oral examinations were performed by trained professionals, and a structured questionnaire was completed for each participant after obtaining informed consent. Data on DMFT index and the prevalence of periodontal diseases, mucosal lesions, and other oral health issues were collected and analyzed using SPSS 26 software. Statistical correlations were explored between DMFT index and variables such as smoking, drug use, education level, and CD4 count. Among the 134 participants (96 men and 38 women) with a mean age of 44 years, the average duration of HIV infection was 106 months. The DMFT index averaged 16.7 and was significantly associated with smoking, drug use, education level, and CD4 count (p < 0.05). Periodontal disease was the most prevalent condition (69%), followed by angular cheilitis (17.9%) and aphthous ulcers (16.4%). Mucosal lesions such as candidiasis, hairy leukoplakia, and cancer had a prevalence of less than 5%. Financial constraints (66%) and stigma or discrimination (27%) were identified as the primary barriers to accessing dental services. A high DMFT index and periodontal disease prevalence were observed. Smoking, drug use, lower education, and CD4 count were significantly associated with worse outcomes (p < 0.05). Financial barriers and stigma hindered access to care. This approach can improve oral health outcomes and reduce barriers to care for this vulnerable population.
Similar content being viewed by others
Introduction
Oral health is integral to overall health and quality of life, significantly influencing one’s ability to eat, speak, and socialize without pain or discomfort. The World Health Organization (WHO) defines oral health as a state in which individuals are free from chronic pain, mouth sores, periodontal (gum) disease, tooth decay, tooth loss, and other diseases that limit their capacity for daily function and social interaction1. In HIV-positive populations, oral health issues are particularly prevalent due to immune system degradation and the adverse effects of ART2. Oral manifestations can serve as critical indicators of disease progression in HIV-positive patients and include conditions such as candidiasis, hairy leukoplakia, and periodontal diseases, which, if left untreated, contribute to a decline in both oral and overall health3. Studies indicate that HIV-positive individuals frequently experience higher rates of dental issues than the general population, with the DMFT index (which records decayed, missing, and filled teeth) being notably elevated in this group4. For example, research from countries such as Rwanda and Canada reveals a correlation between socio-economic factors, limited access to healthcare, and increased incidence of oral disease in HIV patients5. Financial constraints, stigmatization, and insufficient awareness are primary barriers to regular dental care, often resulting in unaddressed dental needs and progressive oral health deterioration6. In Iran, HIV continues to affect a significant segment of the population, with oral health disparities being prevalent among HIV-positive individuals. These disparities are compounded by socio-economic challenges, including low income, lack of insurance, and the pervasive stigma surrounding HIV7. Addressing these barriers in Iran’s healthcare context, particularly in Tabriz, could offer insights for policy reform and improved health outcomes for HIV-positive patients. Oral manifestations of HIV-positive patients, including periodontal diseases, candidiasis, and other mucosal lesions, have been extensively documented in various populations worldwide. However, most studies have focused on Western countries or resource-limited settings, and limited data exist on the oral health burden among HIV-positive patients in Iran. Additionally, while several studies have explored the impact of ART on systemic and oral health, there is a lack of research assessing the combined influence of HIV duration, ART exposure, and socioeconomic factors on oral health outcomes in this population. This study aimed to assess the oral health status, using the DMFT index, and to examine associations between oral disease prevalence and behavioral, clinical, and socioeconomic factors in HIV-positive individuals. By incorporating DMFT scores, periodontal status, and self-reported barriers to care, this research seeks to offer a more comprehensive understanding of oral health disparities in HIV-positive individuals, informing targeted interventions to improve dental care accessibility.
Methods
Study design
This was a descriptive-analytical, cross-sectional study conducted on HIV-positive patients in Tabriz, Iran. All methods were performed in accordance with the Dentistry School of Guilan University of Medical Sciences and Medicine Faculty of Tabriz University of Medical Sciences with the ethical code of (IR.GUMS.REC.1402.443) issued by the Guilan University of Medical Sciences. The sample size for this study was determined based on previous studies assessing oral health outcomes in HIV-positive patients. Considering an expected prevalence of oral health issues of approximately 70% among HIV-positive individuals, with a 95% confidence level and a margin of error of 8%, the minimum required sample size was calculated as 119 participants. The calculation was performed using the following formula for prevalence studies:
where n is the sample size, Z is the standard normal deviate (1.96 for a 95% confidence level), P is the expected prevalence (0.70), and d is the margin of error (0.08). To account for potential dropouts and missing data, a total of 134 participants were recruited. Participants were recruited between January 2024 – November 2024 at the Counseling, Care, and Treatment Center affiliated with Tabriz University of Medical Sciences.
Study population, sampling, and determination method
The study population included all HIV-positive patients with records at the Counseling, Care, and Treatment Center affiliated with Tabriz University of Medical Sciences. Patients selected for the study were those with documented, consistent follow-up visits at the center to receive services. All HIV-positive patients with documented and regular attendance at the center were included in the study, resulting in a final sample of 134 patients. The sample size was determined based on a power analysis to ensure statistical significance in detecting associations between DMFT index and independent variables such as smoking, drug use, education level, and CD4 count. To account for potential dropouts and incomplete data, we included 134 patients in the final analysis. A sample of 134 was chosen based on an expected oral disease prevalence of 70%, with 8% margin of error and 95% confidence level.
Participant characteristics and inclusion/exclusion criteria
HIV-positive adults (≥ 18 years) under continuous care at the center for at least three months were included. Patients unable to consent or complete the examination were excluded. Inclusion criteria for the study were as follows: adult HIV-positive patients (18 years or older) who were under continuous medical care at the center for at least three months. Exclusion criteria included patients under 18 years of age, individuals who declined participation or lacked the physical or cognitive ability to complete the questionnaire, and those who did not complete the examination or questionnaire. Exclusion criteria included patients under 18 years of age, individuals who declined participation or lacked the physical or cognitive ability to provide informed consent, and those with severe systemic conditions preventing oral examination. Participants who partially completed the questionnaire were not excluded but were analyzed separately for missing data.
Clarification on the origin of the variable table
The questionnaire used in this study was not directly adapted from previously published studies but was developed based on widely accepted frameworks and guidelines for health research in Iran. The design of the variables and their categorization was guided by resources such as:
-
Zhivar Amoozan Educational Resources: A resource for completing research proposal components, including variable tables, with detailed explanations on scales and roles of variables.
-
Pajouheshyar Research System: A platform widely utilized in Iranian medical research for organizing and presenting variables in proposals.
-
Meditorha Resources on Research Variables: Provides detailed insights into the categorization and operationalization of variables in medical research.
Although the questionnaire was designed specifically for this study, its structure is based on these foundational methodologies to ensure consistency and validity.
Data collection procedures and tools
Baseline information, including age, education level, occupation, HIV transmission route, ART initiation date, and type of antiretroviral medication, was gathered from the data management software and patient records at the counseling center. Examination sessions and questionnaire completion were organized in coordination with center administrators, with patients invited to participate. After explaining the study’s objectives and assuring participants that no personal identifiers were necessary, informed consent was obtained from each participant. Oral health assessments included the DMFT (Decayed, Missing, and Filled Teeth) index and periodontal disease evaluation using a periodontal probe. Oral lesions were identified through visual inspection of the oral cavity under lighting conditions similar to those used in a dental unit. Patients with dentures were excluded from DMFT and periodontal disease assessments. A structured questionnaire was used to collect data on demographic characteristics, oral health behaviors, and self-reported barriers to dental care. The questionnaire was adapted from previously validated instruments used in HIV-related oral health research and modified to align with the study’s objectives and the Iranian healthcare context. The questionnaire covered socioeconomic factors (education, income, insurance status), health behaviors (smoking, substance use, oral hygiene practices), and access to dental care. Additionally, it included self-reported oral health conditions, such as gingival bleeding, tooth loss, and mucosal lesions, which were later confirmed by clinical examination. Validation Process: The questionnaire underwent content validation by three oral health experts and two infectious disease specialists, ensuring relevance and clarity. A pilot study involving 15 HIV-positive patients was conducted to assess comprehensibility and response consistency. Minor modifications were made based on participant feedback before full-scale implementation.
Data collection instruments
Data sources included the center’s data management software, patient files, structured interviews, completed questionnaires, and clinical examinations, all of which provided essential information for the study. Data collection was conducted by two trained and calibrated dental examiners with expertise in oral health assessment among immunocompromised patients. Prior to the study, the examiners underwent a training session to ensure standardization in data collection, including the assessment of DMFT index and periodontal diseases. Inter-examiner reliability was assessed. Additionally, periodic intra-examiner calibration was performed to maintain consistency throughout the study.
Oral health assessment and indices used
Examiners were trained and calibrated; periodic intra-examiner reliability was ensured. The Decayed, Missing, and Filled Teeth (DMFT) index was selected as the primary measure of oral health status in this study due to its widespread use in epidemiological studies assessing dental caries and treatment needs. The DMFT index is a well-validated and standardized tool endorsed by the World Health Organization (WHO) for evaluating caries experience in populations.
While the WHO Dentition Status Index (2013 Oral Health Assessment Form for HIV Oral Manifestations) provides a broader classification of oral health status, including lesion-specific evaluations, the DMFT index was chosen for this study because:
-
It provides a quantitative measure of dental caries burden, which is a significant concern in HIV-positive individuals.
-
It allows for comparability with prior epidemiological studies on oral health in HIV populations.
-
It aligns with the study’s objective, which focuses on assessing the relationship between HIV infection, ART duration, and dental caries burden.
However, additional oral health parameters, such as periodontal disease prevalence and mucosal lesions (e.g., candidiasis, leukoplakia, and ulcers), were also documented to ensure a comprehensive assessment of oral health status among HIV-positive patients. Periodontal disease was evaluated using the World Health Organization’s Community Periodontal Index (CPI). This index assesses gingival health, periodontal pockets, and loss of attachment, allowing for standardized classification of periodontal status in epidemiological studies. The use of the CPI ensured that our findings are comparable with other studies in similar populations.
Study variables
Variables included demographic, clinical (CD4, ART duration), and behavioral (smoking, drug use) factors. The primary outcome was DMFT score. The primary variable of interest was the DMFT (Decayed, Missing, and Filled Teeth) index. Independent variables assessed for correlation with the DMFT index included smoking status, drug use, education level, and CD4 count. Additional demographic and clinical variables, such as age, gender, and duration of ART, were also evaluated. The main study variables are presented in the Table 1.
Validity and reliability
To assess the content validity index (CVI) of the questionnaire, the Waltz and Basel method was applied, involving a panel of six experts: two oral disease specialists, one endodontist, one social dentistry specialist, one infectious disease expert, and one epidemiologist. These specialists evaluated the relevance, simplicity, clarity, and transparency of each question on a Likert scale. Content validity was calculated as the ratio of experts who rated each question as 3 or 4 to the total number of experts; questions scoring below a CVI of 0.79 were excluded. Internal consistency was verified using Cronbach’s alpha, with support from a biostatistician, and was processed in SPSS software.
Data analysis
Data were analyzed using SPSS version 26. Descriptive statistics (mean, standard deviation, frequencies, and percentages) were used to summarize demographic and clinical characteristics. Bivariate analyses, including Pearson’s correlation and chi-square tests, were conducted to assess associations between the DMFT index and independent variables such as smoking, drug use, education level, and CD4 count. Multivariate linear regression was performed to identify independent predictors of DMFT scores, adjusting for potential confounders. Statistical significance was set at p < 0.05, and 95% confidence intervals (CIs) were reported. To minimize selection bias, all eligible patients with regular visits were included. Information bias was reduced by using validated tools and trained examiners. Recall bias was minimized by collecting most data from clinical records. Quantitative variables like DMFT, CD4 count, and age were analyzed as continuous data. Categorical variables (e.g., smoker/non-smoker) were grouped based on clinical relevance. Pearson’s correlation, chi-square, and multivariate linear regression were used to assess associations between DMFT and independent variables. Missing data were analyzed separately; cases with incomplete clinical records were excluded from regression. Significance was defined as p < 0.05. No sampling weights or sensitivity analyses were applied.
Results
Demographic characteristics of the study population
A total of 134 HIV-positive patients participated in this study, of whom 96 (71.6%) were male and 38 (28.4%) were female, with an average age of 44 years (± 10 years), ranging from 19 to 73 years. No patients were lost to follow-up due to the cross-sectional design. Most patients (48.9%) had only a middle or high school education, and only 15% had education levels higher than a high school diploma. Women had higher levels of educational attainment compared to men. Approximately 56.7% of the participants were married, while the remaining patients were single. Health insurance coverage was prevalent, with 86% of patients insured. The study also revealed a significant economic disparity, as more than 65% of participants were classified below the poverty line, with a higher percentage of women affected than men (Table 1).
Substance use and health indicators
The prevalence of smoking and drug use among all patients was 50% and 37.3%, respectively. However, there was a marked difference in these behaviors between genders, with 50% of men and only 5% of women reporting smoking, and drug use being significantly higher in men (50%) compared to women (5.3%) (Table 1).
HIV health metrics
Sexual transmission was the most common route of HIV acquisition, accounting for 55.2% of cases, with women twice as likely as men to have contracted HIV through sexual contact. Injection drug use was noted exclusively among male participants, comprising 33.6% of the male cases (Table 1). The mean duration since HIV diagnosis among all participants was approximately nine years, with no significant gender differences. Patients had an average ART treatment duration of 85 months, with a range from 4 to 218 months (Table 1). Tenofovir was the most widely used medication, prescribed to 90.6% of men and 84.2% of women, while Efavirenz was used by only 3.1% of men and 2.6% of women. The advanced stage of HIV infection (AIDS), defined by CD4 counts below 200 cells/mm³, was observed in only 4.5% of the patients. Notably, 62% of patients had an undetectable viral load, and in 84% of the cases, the viral load was less than 200 copies/mL. Women generally showed better immune status than men, with 63.2% having an undetectable viral load, and a mean CD4 count of 841 cells/mm³ compared to 596 cells/mm³ in men (Table 1).
Oral health status
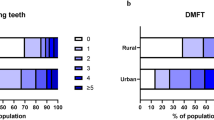
The study evaluated the participants’ oral health using the DMFT index and observed mucosal lesions. Dental decay was prevalent, with 90% of patients experiencing dental caries. The mean number of decayed, missing, and filled teeth were 4.4, 9.05, and 2.8, respectively, resulting in a mean DMFT score of 16.7 (Table 2). Gender differences were noted in the components of the DMFT index: while there was no significant difference in the mean number of decayed teeth, women exhibited fewer missing teeth (mean difference of four teeth) and had a higher number of filled teeth (mean difference of four teeth) than men (Table 2). Consequently, women had a lower overall DMFT score, averaging 2.7 points lower than men. Approximately 39% of the patients used dentures, with a higher prevalence among men (43.8%) than women (28.9%). Patients with dentures were excluded from the DMFT and periodontal disease assessments. Additionally, angular cheilitis was three times more common in men than in women (Fig. 1).
Periodontal health
Periodontal disease was highly prevalent among the study population, with 69% exhibiting either gingivitis or periodontitis (Table 2, and 3). The rates of periodontitis were higher in men, whereas gingivitis was more common among women. Other oral conditions observed included angular cheilitis, aphthous ulcers, candidiasis, hairy leukoplakia, and oral cancer. Angular cheilitis was more frequent among men (21.9%) and aphthous ulcers were more common among women (28.9%). Notably, none of the female patients exhibited oral candidiasis, hairy leukoplakia, or oral cancer (Fig. 1).
Knowledge and behavioral practices related to oral health
Participants’ knowledge of factors impacting oral health was assessed through a series of six questions. Approximately 80% of patients answered these questions correctly, though the question regarding the appropriate time for brushing teeth had the lowest accuracy rate (66 − 60%). Regarding oral health practices, nearly all patients reported daily consumption of dairy products, such as cheese (Tables 2 and 3). However, a significant number of both men and women (72% and 67%, respectively) did not engage in regular dental check-ups. Additionally, 34% of the participants never used a toothbrush or dental floss, and only 27% brushed their teeth twice or more per day (Table 2, and 3), with men reporting lower daily usage of toothbrush and floss compared to women.
Barriers to accessing dental services
Access to dental care was notably affected by economic and social barriers. The most commonly reported barrier was financial hardship, with 66% of patients indicating that costs hindered their ability to access dental services. Stigmatization and discrimination were also prominent concerns, affecting 27% of the participants, with a higher impact reported by women (32%) compared to men (26%). Half of the participants (50%) reported disclosing their HIV status to their dentists; among these, 22% of women and 9% of men faced refusal of services due to their HIV status. Interestingly, 28% of patients reported that they never disclosed their HIV status when seeking dental care.
Access to free dental health resources
In terms of access to free dental health resources and educational materials, 80% of men and 64% of women reported not receiving any free hygiene products such as toothbrushes, dental floss, or toothpaste from counseling centers. Only 28% of women and 17% of men had received free dental extractions at these centers. Additionally, 74% of men and 66% of women stated that they had never received oral health education from a healthcare provider or dental professional.
Preferred interventions to improve dental health
When asked about the most beneficial intervention that could address their dental health issues, the majority of both male and female patients (67%) indicated that having a dentist available at the counseling center would be the most effective solution. Access to dental insurance was also cited as an important measure by 8% of women and 17% of men. A smaller group (2.8% of women and 9% of men) highlighted the need for education on oral health as the most valuable intervention (Table 3).
Missing data were minimal (< 5%) and occurred mostly in self-reported questions. These cases were excluded from subgroup analyses. No interaction or subgroup analyses were performed due to sample size constraints.
Discussion
The study revealed high DMFT scores (mean: 16.7), with strong associations between oral health status and smoking, drug use, lower education, and low CD4 count among 134 HIV-positive patients in Tabriz, Iran. Significant findings were observed regarding smoking, drug use, education level, and CD4 count, alongside notable gender differences and high disease prevalence rates. The discussion contextualizes these findings within the existing literature, comparing results to previous studies, including those in both HIV-positive and general populations, and incorporates patient recommendations for improving oral healthcare access. The findings are generalizable to HIV-positive populations in urban Iran with similar healthcare access, but caution should be used when applying these results to rural or low-resource populations.
Correlations with DMFT (Decayed Teeth)
The DMFT index in this study averaged 16.7, with significant correlations observed with several variables. Higher DMFT scores were strongly associated with smoking and drug use, while education level and CD4 count showed inverse correlations. These results are consistent with findings in HIV-positive populations globally and emphasize the compounded impact of socio-economic, behavioral, and systemic factors.
-
Smoking and Drug Use: Patients who smoked or used drugs had significantly higher DMFT scores, averaging 23.7 compared to 13.6 in non-users. This aligns with findings from Carolyn et al. in San Francisco, which reported double the DMFT scores among young HIV-positive drug users compared to non-users8. Similarly, Rezaei Soufi’s study in Hamedan highlighted higher rates of dental decay in HIV-positive drug users compared to their non-using counterparts9.
-
Education Level: The negative correlation between education level and DMFT (r = -0.34, p < 0.05) highlights the role of health literacy in oral health maintenance. Patients with higher education levels likely possess greater awareness of oral hygiene practices, consistent with studies in Rwanda and Iran, which observed better oral health outcomes among educated individuals10.
-
CD4 Count: Immune deficiency, as measured by CD4 count, had a significant inverse relationship with DMFT scores (r = -0.28, p = 0.03). Patients with CD4 counts below 200 exhibited higher rates of dental decay and missing teeth, consistent with Wilfred et al.’s findings in Uganda and Fi Chin’s research in Shanghai, where immune suppression strongly predicted oral health deterioration11.
These results underscore the importance of addressing behavioral and socio-economic factors, alongside improving immune health, in mitigating oral health disparities in HIV-positive populations.
Comparisons with Non-HIV populations
The DMFT index in this study (16.7) was significantly higher than reported averages for non-HIV populations in Iran, which range from 9.5 to 12.312. This disparity reflects the compounded challenges faced by HIV-positive individuals, including the effects of ART, immune suppression, and social stigma. For example, while the prevalence of periodontal disease in this study was 69%, general population rates in Iran are approximately 45%. These differences emphasize the need for targeted oral health interventions tailored to the unique needs of HIV-positive patients. Prior studies have well-documented the prevalence of oral lesions and dental conditions among HIV-positive populations. However, our findings provide new insights into the specific challenges faced by HIV-positive individuals in Iran, particularly regarding financial barriers (66%) and stigma (27%) preventing access to dental care. This is one of the few studies in the region to quantify these social determinants and their correlation with poor oral health outcomes.
Moreover, while previous research has demonstrated the association between HIV and periodontitis, our study further highlights the significant impact of smoking, substance use, and socioeconomic status on oral health indicators such as DMFT scores and periodontal disease severity. The identification of low education levels and lack of routine dental visits as key predictors of severe tooth loss offers practical implications for oral health interventions.
These findings emphasize the need for integrating preventive dental care into HIV treatment programs, ensuring affordable, stigma-free access to oral healthcare within behavioral disease counseling centers.
Influence of ART duration on DMFT
Contrary to some studies, this research found no significant association between ART duration and DMFT scores. Prior studies have suggested that long-term ART use, particularly regimens involving Tenofovir, may contribute to dental decay due to side effects like xerostomia and reduced bone density13. The lack of correlation in this study could be due to the lower prevalence of advanced AIDS stages among participants or variations in ART regimens used. Future longitudinal studies are needed to clarify this relationship.
Poor oral health parameters
The findings of this study revealed a high prevalence of poor oral health indicators among HIV-positive patients, with elevated DMFT scores, significant tooth loss, and a high occurrence of periodontal disease. These findings are consistent with previous research indicating that HIV-positive individuals are at an increased risk for oral health deterioration due to immunosuppression, long-term antiretroviral therapy (ART), and socioeconomic factors. The high prevalence of missing teeth and periodontal disease may be attributed to delayed dental visits, financial constraints, and lack of access to routine preventive care. The high DMFT index (16.7) observed in our study suggests extensive dental decay and untreated oral health issues among the participants. Poor oral hygiene practices, compounded by barriers to care, such as stigma and discrimination, likely contribute to this burden. Additionally, periodontal disease was present in 38.3% of participants, which aligns with studies demonstrating an increased risk of periodontitis in HIV-infected populations due to altered immune responses and chronic inflammation. The low prevalence of mucosal lesions, such as oral candidiasis and hairy leukoplakia, could be linked to effective ART regimens, which have been shown to reduce the incidence of opportunistic infections in well-managed HIV patients. However, angular cheilitis and aphthous ulcers were relatively common, possibly due to micronutrient deficiencies and immune dysregulation.
These results emphasize the urgent need for targeted oral health interventions, including regular screenings, improved access to affordable dental care, and patient education to enhance oral hygiene behaviors. Integrated dental services within HIV care programs could help mitigate these disparities and improve overall health outcomes in this population.
Gender disparities in DMFT scores
Men had higher DMFT scores than women, likely due to higher rates of smoking and drug use. However, when controlling for lifestyle factors, women exhibited slightly higher DMFT scores (15.2 vs. 12.8). This finding may reflect gender-based disparities in access to care or differences in biological susceptibility to dental decay. Similar trends have been reported in studies from Uganda and Rwanda, where women faced greater barriers to dental care despite better adherence to hygiene practices14.
Prevalence of oral mucosal lesions
Oral mucosal lesions were prevalent in this study, with periodontal disease affecting 69% of participants. Angular cheilitis (17.9%) and aphthous ulcers (16.4%) were more common in men and women, respectively. Advanced immune deficiency-related lesions, such as candidiasis and hairy leukoplakia, were rare (< 5%), consistent with the low prevalence of advanced AIDS stages in this cohort. These findings align with Mendel Douglas and Mohraz’s studies, which documented higher lesion rates among immunocompromised patients15,16.
Patient recommendations for oral healthcare improvements
Patients identified several barriers to accessing dental care, with financial constraints (66%) and stigma (27%) being the most significant. They recommended integrating dental services within HIV counseling centers and providing free or subsidized care to reduce financial burdens. These suggestions echo findings from other studies, which highlight the need for systemic reforms to improve access and reduce discrimination17.
Recommendations for improving oral health care in HIV-Positive populations
The findings underscore the critical need for systemic changes to improve oral healthcare access and reduce disparities among HIV-positive populations. Key patient recommendations include:
-
1.
Integrating Dental Services in HIV Care: Offering dental services at HIV counseling and treatment centers can improve access to regular dental care, reduce stigma, and encourage preventive practices.
-
2.
Subsidizing Dental Care Costs: Providing subsidized or free dental care for low-income HIV-positive individuals would alleviate the financial burden and promote routine check-ups.
-
3.
Expanding Oral Health Education: Public health initiatives should emphasize the importance of brushing, flossing, and dietary habits, targeting areas with lower literacy rates to increase awareness and improve oral hygiene.
-
4.
Anti-Stigmatization Training for Healthcare Providers: Training programs for healthcare professionals can foster an inclusive environment, addressing biases and reducing discrimination, thus encouraging patients to seek timely care.
Limitations and future research
This study’s cross-sectional design limits causal inference, and reliance on patient self-reports may introduce bias. Future longitudinal studies with larger sample sizes could explore the long-term effects of ART on oral health and investigate potential mechanisms behind observed gender disparities in dental health. Also, this study is limited by its cross-sectional design, which does not allow causal inference. Self-reported behaviors may be subject to recall or social desirability bias. Also, the exclusion of patients unable to complete questionnaires may introduce selection bias.
Conclusion
This study highlights the significant burden of oral health issues among HIV-positive patients, with a high prevalence of dental caries, periodontal disease, and tooth loss. The DMFT index was notably high, with missing teeth contributing significantly to the overall score. Periodontal disease was a common finding, indicating the need for early intervention and routine dental care to prevent disease progression. Additionally, socioeconomic barriers, including financial constraints and stigma, were identified as key obstacles preventing patients from accessing timely dental treatment. Given the strong association between poor oral health and factors such as smoking, drug use, lower education levels, and CD4 count, targeted preventive and treatment strategies should be integrated into HIV care services. Providing accessible, stigma-free dental care within HIV counseling centers can help mitigate oral health disparities and improve overall patient well-being. Further research is recommended to explore long-term oral health outcomes in this population and assess the effectiveness of intervention programs aimed at improving dental health among HIV-positive individuals.
Data availability
All data generated or analysed during this study are included in this published article.
Change history
06 October 2025
A Correction to this paper has been published: https://doi.org/10.1038/s41598-025-19521-6
Abbreviations
- AA:
-
Amino Acid
- AIDS:
-
Acquired immunodeficiency syndrome
- ANOVA:
-
Analysis of variance
- ART:
-
Antiretroviral therapy
- BA:
-
Buccal angle
- BB:
-
Buccal bone
- BMC:
-
Bone mineral content
- BT:
-
Bite thickness
- CH:
-
Crown height
- CL:
-
Crown length
- CR:
-
Clinical relevance
- CVI:
-
Content validity index
- DA:
-
Decayed area
- DMF:
-
Decayed, missing, and filled
- DMFT:
-
Decayed, missing, and filled teeth
- EK:
-
Enamel kinetics
- EM:
-
Enamel microhardness
- GUMS:
-
Gingival and upper mucosal structures
- HCV:
-
Hepatitis C Virus
- HIV:
-
Human immunodeficiency virus
- HR:
-
Hazard ratio
- IR:
-
Infrared
- JE:
-
Junctional epithelium
- PLWHA:
-
People Living with HIV/AIDS
- REC:
-
Root exposure condition
- SM:
-
Submucosa
- SO:
-
Specific Oral
- SPSS:
-
Statistical package for the social sciences
- SS:
-
Statistical significance
- VA:
-
Visual analogue
- VL:
-
Viral load
- WHO:
-
World Health Organization
References
Barranca-Enríquez, A. & Romo-González, T. Your health is in your mouth: A comprehensive view to promote general wellness. Front. Oral Health. 3, 971223 (2022).
Omolehinwa, T. et al. Oral health outcomes in an HIV cohort with Comorbidities- implementation roadmap for A longitudinal prospective observational study. Res. Sq (2023).
Hirata, C. H. Oral manifestations in AIDS. Braz J. Otorhinolaryngol. 81 (2), 120–123 (2015).
Murererehe, J., Malele-Kolisa, Y., Niragire, F. & Yengopal, V. Prevalence of dental caries and associated risk factors among people living with HIV/AIDS and HIV uninfected adults at an HIV clinic in Kigali, Rwanda. PLoS One. 18 (4), e0276245 (2023).
Murererehe, J., Malele-Kolisa, Y., Niragire, F. & Yengopal, V. Oral health-related quality of life among people living with HIV and HIV-negative adults in Kigali, Rwanda: a comparative cross-sectional study. BMC Oral Health. 24 (1), 128 (2024).
Lieneck, C. et al. Facilitators and barriers to oral healthcare for women and children with low socioeconomic status in the united States: A narrative review. Healthc. (Basel) ;11(16). (2023).
Shaghaghian, S., Homayooni, M., Amin, M. & Rezazadeh, F. Oral health status of patients infected with human immunodeficiency virus and related factors, Iran: a cross-sectional study. BMC Oral Health. 21 (1), 657 (2021).
Bhavsar, R. et al. Dental caries and oral health status of psychoactive substance abusers. Int. J. Environ. Res. Public. Health ;19(10). (2022).
Rezaei-Soufi, L., Davoodi, P., Jazaeri, M. & Niknami, H. The comparison of root caries experience between HIV-positive patients and HIV-negative individuals in a selected Iranian population. Int. J. Dent. Hyg. 9 (4), 261–265 (2011).
Mafuvadze, B., Mahachi, L. & Mafuvadze, B. Dental caries and oral health practice among 12 year old school children from low socio-economic status background in Zimbabwe. Pan Afr. Med. J. 14, 164 (2013).
Nittayananta, W. et al. Effects of long-term use of HAART on oral health status of HIV-infected subjects. J. Oral Pathol. Medicine: Official Publication Int. Association Oral Pathologists Am. Acad. Oral Pathol. 39, 397–406 (2010).
Soltani, M. R., Sayadizadeh, M., Raeisi Estabragh, S., Ghannadan, K. & Malek-Mohammadi, M. Dental caries status and its related factors in Iran: A Meta-Analysis. J. Dent. (Shiraz). 21 (3), 158–176 (2020).
Nittayananta, W. et al. Effects of long-term use of HAART on oral health status of HIV-infected subjects. J. Oral Pathol. Med. 39 (5), 397–406 (2010).
Beklen, A., Sali, N. & Yavuz, M. B. The impact of smoking on periodontal status and dental caries. Tob. Induc. Dis. 20, 72 (2022).
Samarasekera, U. Minoo Mohraz-Iran’s leader in HIV research. Lancet Infect. Dis. 21 (12), 1640 (2021).
A Z. - Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. Lancet Infect. Dis. ;10(5):303–304. (2010).
Parish, C., Siegel, K., Pereyra, M., Liguori, T. & Metsch, L. Barriers and facilitators to dental care among HIV-Infected adults. Spec. Care Dentist. 35 (6), 294–302 (2015).
Funding
This study was funded by the Guilan University of Medical Sciences with the code of IR.GUMS.REC.1402.443. The funders had no role in the study design, data collection, analysis, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
Saman Khodavirdizadeh Ghahremani and Ramin Ghasemi Shayan have collected data, and drafted the article, respectively. Dr. Seyed Javad Kia was the main supervisor of the project and provided guidance during the process, Dr. Khosousi Sani and Dr. Gholamreza Khodavirdizadeh Ghahremani critically revised it.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical consideration
This project was done at the Dentistry School of Guilan University of Medical Sciences and Medicine Faculty of Tabriz University of Medical Sciences with the ethical code of (IR.GUMS.REC.1402.443) issued by the Guilan University of Medical Sciences.
Human ethics and consent to participate
All the patients included in this study were the patients of Counseling, Care, and Treatment Center of Tabriz University of Medical Sciences. Informed consents were obtained from all the patients.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained an error in the spelling of the author Ramin Ghasemishayan which was incorrectly given as Ramin Ghasemi Shayan.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Khodavirdizadeh Ghahremani, S., Ghasemishayan, R., Kia, S.J. et al. A cross-sectional study of oral health and disease prevalence in HIV-positive patients in Tabriz, Iran (2024). Sci Rep 15, 18931 (2025). https://doi.org/10.1038/s41598-025-03940-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-03940-6