Abstract
Knee osteoarthritis (KOA) is a common degenerative joint disease that significantly reduces mobility and quality of life in elderly populations. Tai Chi, a low-impact mind-body exercise, has been suggested as a potential non-pharmacological intervention for managing KOA, but its biomechanical effects remain unclear. This study aimed to evaluate the effects of a 14-week Tai Chi program on clinical symptoms, lower limb biomechanics, and muscle activation patterns in elderly patients with KOA. A single-blinded randomized controlled trial was conducted, enrolling 24 participants aged 55–70 years with unilateral KOA. Participants were randomly assigned to a Tai Chi intervention group or a control group receiving health education only. Primary outcomes included joint range of motion, joint moments, and muscle activation, measured using a motion capture system and surface electromyography. Secondary outcomes, such as pain, stiffness, function (WOMAC), balance (BBS), and quality of life (SF-12), were also assessed pre- and post-intervention. The Tai Chi group demonstrated significant improvements in WOMAC pain (−1.58 ± 1.44 vs. 0.11 ± 0.78, p = 0.01), stiffness (−0.33 ± 0.78 vs. 0.56 ± 0.88, p = 0.02), and function scores (−2.58 ± 3.53 vs. 1.00 ± 2.78, p = 0.02) compared to the control group. Balance (BBS: 1.42 ± 1.88 vs. −0.89 ± 1.27, p = 0.01) and physical health (SF-12 PCS: 5.45 ± 6.76 vs. −1.05 ± 2.17, p = 0.01) were also enhanced. Biomechanically, Tai Chi reduced horizontal plane knee ROM (−3.03 ± 1.00°, p = 0.01) and maximum knee extension moments (affected side: −0.09 ± 0.04 N/kg, p = 0.04, Non-affected side: -0.11 ± 0.05 N/kg, p = 0.03). Tibialis anterior muscle activation increased significantly (5.66 ± 1.05%MVIC, p = 0.02), while other muscles showed non-significant trends. Tai Chi demonstrated significant clinical and biomechanical benefits for elderly KOA patients, suggesting its potential as a safe, accessible, and effective therapeutic intervention.
Similar content being viewed by others
Introduction
Knee osteoarthritis (KOA) is a prevalent chronic degenerative joint disorder characterized by cartilage degradation, pain, stiffness, and functional impairment, significantly diminishing the quality of life and independence of affected individuals1. Globally, KOA impacts over 260 million people, making it one of the leading causes of disability, as reported in the 2021 Global Burden of Disease Study2,3. With an aging population and increasingly sedentary lifestyles, the prevalence of KOA is projected to rise, highlighting the urgent need for effective, safe, and sustainable management strategies4.
Current pharmacological treatments, such as nonsteroidal anti-inflammatory drugs (NSAIDs), primarily alleviate symptoms. However, their prolonged use is associated with adverse side effects, including gastrointestinal complications and cardiovascular risks5,6. Consequently, non-pharmacological interventions, particularly exercise-based therapies, have gained attention for their low-risk and cost-effective nature in KOA management.
Tai Chi, a traditional Chinese mind-body exercise integrating slow movements, controlled breathing, and mindfulness, has emerged as a promising therapeutic approach. Robust clinical evidence from randomized trials and meta-analyses demonstrates its efficacy in alleviating pain, improving physical function, and enhancing psychological well-being in KOA patients7,8. Consequently, major clinical guidelines, including those from the American College of Rheumatology, now endorse Tai Chi as a first-line therapy for KOA management1,6. Despite these clinical advances, the biomechanical mechanisms underlying its therapeutic effects remain poorly understood.
Existing research has predominantly focused on clinical outcomes, with limited investigation into Tai Chi’s effects on lower-limb biomechanics during functional activities such as gait9,10. Critical biomechanical factors—including abnormal joint loading, altered range of motion (ROM), and neuromuscular imbalances—are well-established contributors to KOA progression11,12,13. While studies like Wang et al. (2016) reported pain reduction following Tai Chi, they omitted joint kinetic analyses14, and Zhu et al. (2016) documented gait improvements without electromyographic (EMG) data to elucidate neuromuscular adaptations15. These knowledge gaps hinder the development of biomechanically optimized rehabilitation protocols.
This randomized controlled trial (RCT) comprehensively evaluates the effects of a 14-week Tai Chi intervention on clinical outcomes and lower-extremity biomechanics in KOA patients. We hypothesize that Tai Chi training, compared to health education alone, will significantly improve pain and physical function, optimize knee joint kinematics and kinetics during gait, and enhance neuromuscular activation patterns, thereby elucidating its multidimensional therapeutic mechanisms.
Methods
This single-blinded RCT was conducted as a sub-study of a registered sarcopenia-related clinical research framework (Chinese Clinical Trial Registry No. ChiCTR2300078229; registered December 1, 2023), although this sub-study is not explicitly listed out in the trial registration. This sub-study aimed to evaluate the effects of a 14-week Tai Chi intervention on clinical outcomes and lower-limb biomechanical parameters in elderly patients with KOA. Prior to enrollment, all participants provided written informed consent following a comprehensive explanation of the study protocol.
Recruitment of participants
Participants were recruited from community centers in Guangzhou, China. The inclusion criteria were: (1) age 55–70 years; (2) body mass index (BMI) ≤ 28 kg/m²16; and (3) a clinical diagnosis of unilateral KOA according to the American College of Rheumatology criteria17, to enable biomechanical comparisons. These criteria ensured cohort homogeneity and allowed focused analysis of Tai Chi’s biomechanical effects and clinical symptom improvements in unilateral KOA.
Exclusion criteria included: (1) inability to walk 20 m independently; (2) knee surgery or corticosteroid injections within the past six months; (3) regular participation in lower limb strength training (e.g., weight training, resistance exercises); or (4) any musculoskeletal or mental condition that could interfere with participation. These exclusions minimized confounding variables and safety risks, thereby reducing interference in joint function assessments (e.g., biomechanical metrics, pain severity) and strengthening study validity.
Ultimately, 24 eligible participants were enrolled in the study. As a pilot trial, the sample size (n = 24) was determined based on feasibility considerations (e.g., recruitment capacity, resource availability) rather than formal power calculations, consistent with methodological recommendations for pilot trials prioritizing feasibility assessment and effect size estimation18,19.
Intervention protocol
Participants were stratified by age, gender, and KOA severity and randomized using a computer-generated block sequence (block size = 4) created by an independent statistician via SPSS 26.0. Allocation details were concealed in sequentially numbered, opaque envelopes, which were opened after baseline assessments to notify participants of group assignments via text message. To maintain blinding, participants were informed that the study aimed to evaluate “knee health interventions,” with no disclosure of group-specific details.
The experimental group underwent a 14-week Chen-style Tai Chi intervention based on the standardized 24-form protocol. Training sessions were overseen by a Class 1 National Martial Arts Athlete (certified by the Chinese Wushu Association) to ensure protocol adherence. The program consisted of three 60-minute supervised sessions per week, each comprising: (1) a 10-minute warm-up of gentle stretching and joint mobilization; (2) a 40-minute Tai Chi practice focusing on controlled weight-shifting, deep knee flexion through self-selected squat depth: high, medium, or low - with lower positions indicating greater exercise intensity, and multiplanar joint rotations; and (3) a 10-minute cool-down period with breathing exercises and static stretching. Certified instructors provided real-time feedback on movement precision including knee alignment and trunk posture though formal kinematic assessments were not conducted. The intervention progressed from fundamental posture acquisition during the initial two weeks to integrated form practice through weeks 3–14.
Both study arms participated in identical biweekly health education sessions (60 min each) covering KOA pathophysiology, lifestyle modification strategies, and pain management techniques, delivered by qualified health educators. These parallel education components served to control for placebo effects while maintaining blinding through temporal and spatial separation of group sessions (conducted at different times/locations).
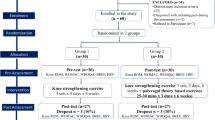
All participants were instructed to maintain their customary physical activity patterns throughout the study duration. Protocol adherence was strictly enforced, requiring attendance at ≥ 80% of scheduled sessions (Tai Chi: 34/42; control: 6/7 education sessions) for continued study participation. The experimental procedure is illustrated in Fig. 1.
Data collection and processing
Data collection was conducted at two time points: baseline (December 25, 2023-December 31, 2023) and post-intervention (April 14, 2024-April 20, 2024). The primary outcomes assessed were changes in lower limb biomechanics and muscle activation patterns, which are crucial indicators of motor function improvement and pain reduction. Secondary outcomes included assessments of pain, stiffness, and physical function using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC); quality of life measured through the Short Form 12 Health Survey (SF-12); and balance quality, evaluated using the Berg Balance Scale (BBS). These measures provided a comprehensive understanding of the intervention’s impact on participants’ clinical and functional statuses.
The biomechanical evaluations were conducted in the biomechanics laboratory at Guangzhou Sport University, equipped with advanced instrumentation to capture precise movement data. Kinetic data were recorded using two three-dimensional force platforms (AMTI OR6-7, Watertown, MA, USA, 60 × 40 cm) embedded in the laboratory floor, which operated at a sampling rate of 1000 Hz. Concurrently, kinematic data were collected through a motion capture system (Nexus Vicon, Oxford, UK) at 100 Hz, which meticulously recorded the range of motion of the lower limb joints using 36 reflective markers placed on participants’ lower limbs, as per the protocols established in prior research by our team20.
Surface electromyography (sEMG) data were captured using a 16-channel Trigno Wireless EMG System (Trigno Wireless EMG System, Delsys Inc., Natick, MA, USA), which had a sampling rate of 2000 Hz. This system was specifically used to monitor muscle activity in key muscle groups including the gluteus maximus, gluteus medius, biceps femoris, rectus femoris, and tibialis anterior. To ensure optimal signal quality, hair was removed and the skin was thoroughly cleaned before placing the sensors, minimizing electrical impedance21,22.
Before the tests, participants changed into standardized black shorts and performed a series of stretching and warm-up exercises in the experimental hall. During this preparatory phase, researchers provided detailed explanations of the testing procedures and addressed any questions to ensure participants were fully informed. Reflective markers and sEMG sensors were carefully affixed to the designated joint areas and muscle groups using kinesiology tape, following established methodologies from previous studies20.
Prior to gait tests, static data were collected to serve as a baseline reference. Participants were then positioned at the starting line, and upon hearing the start command, walked at a normal pace along a 6-meter pathway. To ensure data quality, force platform 1 recorded data from one foot while force platform 2 recorded data from the other, with three valid trials successfully captured per participant.
After completing the gait tests, participants performed maximum voluntary isometric contraction (MVIC) tests for the designated muscle groups, following the required protocols20. Additionally, before the experiments began, participants were allowed multiple practice trials to familiarize themselves with the equipment and procedures.
The collected data were processed using Vicon Nexus and Visual 3D software. Kinematic data were filtered with a cutoff frequency of 10 Hz, while kinetic data were filtered at 50 Hz. Key gait events, such as heel strike and toe-off, were identified, and gait cycles were defined as the period from one heel strike to the next on the same side. Joint moments were normalized to each participant’s body weight for standardization. sEMG data underwent high-pass filtering at 400 Hz, rectification, and subsequent low-pass filtering at 20 Hz. All muscle signals were then normalized using MVIC values. The root mean square (RMS) was subsequently calculated to represent muscle activation levels during walking23.
Data analysis
Statistical analyses were conducted using SPSS (version 26.0). The Shapiro-Wilk test was used to assess the normality of the data. Independent samples t-tests were performed to evaluate group differences in baseline characteristics as well as in the changes in clinical outcomes before and after the intervention. These changes were calculated as the difference between post-intervention and pre-intervention values. Paired samples t-tests were used to assess within-group differences before and after the intervention.
To analyze group differences in biomechanical and sEMG data after the intervention, generalized linear mixed models (GLMMs) were applied. An intention-to-treat (ITT) approach was utilized to include participants who dropped out during the study, with missing data imputed using the last observation carried forward (LOCF) method. All data are presented as mean ± standard deviation (\(\bar\chi\) ± sd). A significance level of p < 0.05 was set for all statistical tests.
Results
Attrition and attendance rates
A total of 24 participants were enrolled and randomized into the Tai Chi group (n = 12) or the control group (n = 12). By the end of the 14-week intervention, the Tai Chi group had an attrition rate of 8.3% (1 participant), while the control group experienced an attrition rate of 16.7% (2 participants). The main reasons for dropout included scheduling conflicts and insufficient time for participation.
Changes in participant characteristics and clinical outcomes
Table 1 presents the characteristics outcomes before and after the intervention, while Figs. 2, 3 and 4 display the clinical outcomes (WOMAC scores, SF-12 scores, and BBS scores, respectively) across the study period. Baseline assessments revealed no significant differences in demographics or clinical outcomes between the two groups. Post-intervention, the Tai Chi group demonstrated significant weight reduction, but changes in BMI were not statistically significant (Table 1). Notably, the Tai Chi group exhibited significant improvements in WOMAC scores for pain, stiffness, and function, as well as better physical health quality (PCS of SF-12) and balance performance (BBS), compared to the education group (Figs. 2, 3 and 4).
Changes in Biomechanical outcomes
Tables 2 and 3 present the kinematic and kinetic outcomes, respectively. Prior to the intervention, there were no significant differences in lower-limb biomechanical parameters between the two groups. Following the intervention, the Tai Chi group showed a significant reduction in knee joint ROM in the horizontal plane compared to the control group. Although sagittal plane ROM exhibited a modest increase in the Tai Chi group, this change did not reach statistical significance (Table 2). Additionally, the Tai Chi group demonstrated significant reductions in maximum knee extension moments for both the affected and non-affected sides when compared to the control group (Table 3).
Changes in muscle activation
Table 4 presents the muscle activation patterns before and after the intervention. Muscle activation patterns did not differ significantly between groups at baseline. Significant increases in tibialis anterior muscle activation were observed in the Tai Chi group post-intervention. Although activation trends were noted for other muscles, including the gluteus maximus, gluteus medius, and rectus femoris, these changes did not reach statistical significance. A slight reduction in biceps femoris activation was observed, though this was also not statistically significant.
Discussion
This study aimed to investigate the effects of Tai Chi training on lower limb biomechanics and muscle activation patterns in patients with KOA during walking. The findings demonstrate that a 14-week Chen-style Tai Chi intervention significantly improved clinical symptoms, biomechanical characteristics, and muscle activation patterns in KOA patients. These results provide empirical evidence for Tai Chi’s role in optimizing knee joint mechanics and neuromuscular coordination during gait.
Participation rate and improvements in clinical outcomes
The Tai Chi group exhibited higher participation rates compared to the education group, likely due to its immediate benefits in pain relief and joint mobility14. These factors may have motivated participants to adhere to the intervention.
In terms of clinical outcomes, this study revealed significant improvements in WOMAC scores, encompassing pain, stiffness, and functional dimensions, among participants in the Tai Chi group. These results are consistent with findings from previous studies14,24,25.
As a moderate intensity aerobic exercise, Tai Chi strengthens lower limb muscles, thereby reducing joint pressure and alleviating pain15. Additionally, the multi-directional, dynamic movements emphasized in Tai Chi, which are less commonly incorporated in traditional rehabilitation programs, may effectively improve joint flexibility, reduce soft tissue adhesions, and relieve muscle tension. These mechanisms contribute to improvements in stiffness, pain, and lower limb functionality in KOA patients25,26.
Furthermore, Tai Chi’s emphasis on precise movement control and smooth weight-shifting enhances dynamic balance, reduces the risk of falls, and improves daily activity capabilities26,27. Notably, the lack of significant BMI changes between groups replicates findings from earlier trials14,24. This null effect suggests that Tai Chi’s clinical efficacy may result primarily from neuromuscular re-education and biomechanical optimization rather than anthropometric modifications.
Moreover, Tai Chi has been reported to alleviate psychological issues such as anxiety and depression28. Although no significant differences in mental health scores were observed between the groups in this study, both groups exhibited improvements, likely due to the social interactions involved in group-based activities.
In summary, Tai Chi demonstrated remarkable efficacy in relieving pain, improving joint function, and enhancing quality of life in KOA patients.
Improvements in biomechanical outcomes
Following the intervention, the Tai Chi group showed significant improvements in horizontal plane ROM and reductions in knee joint maximum extension moments, indicating Tai Chi’s positive effects on optimizing joint movement patterns and reducing abnormal joint activities.
The observed reduction in horizontal plane ROM reflects enhanced rotational stability that may be a critical adaptation for mitigating cartilage degradation. Excessive tibiofemoral rotation during gait increases shear stress on articular surfaces, accelerating cartilage wear and exacerbating medial compartment loading through uneven force distribution29,30. Tai Chi’s emphasis on axial alignment—such as maintaining knee-over-toe positioning during semi-squats—strengthens proprioceptive feedback and coordinates muscle activation (e.g., tibialis anterior, quadriceps), thereby suppressing aberrant rotational kinematics31,32. This neuromuscular optimization redistributes joint loads from shear-dominant to compression-dominant forces, which align with cartilage’s structural tolerance, reducing pathological stress concentrations33,34.
While the modest increase in sagittal plane ROM (flexion-extension) did not reach statistical significance, prior studies have shown dose-dependent improvements in knee flexion-extension ROM with longer Tai Chi interventions15. These movement patterns, characterized by controlled multi-plane rotations and progressive squat depth, enhance joint flexibility while strengthening stabilizing musculature (e.g., hamstrings, gluteus medius), thereby improving dynamic stability31,32, reducing focal stress peaks during weight-bearing activities33.
Notably, in addition to the reduction in knee joint maximum extension moments observed in this study, prior research has suggested that Tai Chi may also reduce the knee adduction moment, alleviating medial compartment joint loads and potentially reducing the risk of KOA progression34. This mechanism is likely associated with the observed reduction in abnormal horizontal plane movements.
In summary, Tai Chi improves knee joint movement patterns and load distribution, enhancing dynamic stability and supporting overall improvements in gait function.
Improvements in muscle activation
This study found that the Tai Chi intervention significantly increased the activation of the tibialis anterior muscle. Additionally, trends of increased activation were observed in the gluteus maximus, gluteus medius, and rectus femoris, while the activation of the biceps femoris slightly declined; however, none of these changes reached statistical significance.
The tibialis anterior plays a critical role in lower limb stability and weight-shifting control during the single-leg stance phase of the gait cycle. Insufficient activation of this muscle often leads to gait abnormalities and impaired balance35,36.The observed selective enhancement of tibialis anterior activation reflects the specific neuromuscular demands imposed by Tai Chi’s characteristic movement patterns. During transitional postures such as Single Whip to Cloud Hands, precise dorsiflexion control is required to stabilize the ankle during weight-shifting phases27. The tibialis anterior may serve as a primary dynamic stabilizer through two key mechanisms: (1) eccentric control of plantarflexion during heel strike to attenuate impact forces, and (2) concentric activation during swing phase to ensure proper foot clearance26,35. This repetitive, task-specific activation pattern—combined with Tai Chi’s emphasis on controlled ankle dorsiflexion during semi-squats—likely explains the muscle’s preferential adaptation27.
Although changes in other lower limb muscles did not reach statistical significance, the observed trends are consistent with previous studies31,32. These non-significant changes may be attributed to the relatively short intervention duration and larger muscles (e.g., gluteus maximus) may require longer intervention periods to induce measurable hypertrophy, as their role in Tai Chi—maintaining hip stability during slow, controlled movements—may be less dynamically challenged compared to high-intensity exercises. Future studies could explore the effects of Tai Chi on strengthening major muscle groups more comprehensively by extending the intervention duration or increasing training intensity.
The slight increases in the activation levels of the gluteus maximus, gluteus medius, and rectus femoris may be associated with Tai Chi’s use of semi-squat postures, while the slight decrease in biceps femoris activation may reflect optimized knee flexion-extension control25,37. Tai Chi’s emphasis on fluid movement patterns and balanced load distribution reduces the over-reliance on compensatory muscle activation, thereby optimizing the overall muscle activation pattern. Previous studies have also indicated that Tai Chi may enhance synergistic activation of the rectus femoris and biceps femoris, promoting joint stability and reducing cartilage wear and pain38. The observed reduction in horizontal plane ROM and extension moments further supports this hypothesis.
These biomechanical and neuromuscular changes collectively enhance gait stability and lower limb coordination, effectively reducing joint stress and slowing KOA progression. They also provide strong support for restoring patients’ daily activity capabilities.
Overall, this study systematically analyzed clinical outcomes, biomechanical characteristics, and muscle activation patterns, revealing the significant benefits of Tai Chi training for KOA patients. The results suggest that Tai Chi not only alleviates pain and improves joint function but also enhances gait mechanics and neuromuscular coordination, offering a comprehensive lower limb support system during walking. These multifaceted mechanisms underscore Tai Chi’s great potential as a non-pharmacological intervention in KOA management.
Limitations and future directions
This pilot study has limitations, including a small sample size (n = 24) and a 14-week intervention duration insufficient to assess long-term effects or structural adaptations. Joint contact forces were not directly quantified, and confounding factors (e.g., daily activity levels, medication use) were not rigorously controlled. Future studies should expand sample sizes and extend intervention durations (≥ 6 months), complemented by long-term follow-ups to evaluate sustained therapeutic effects. Advanced biomechanical assessments, such as musculoskeletal modeling, are recommended to quantify joint loading dynamics. Integrating wearable devices for activity monitoring and standardizing medication tracking protocols will enhance methodological rigor, ultimately advancing personalized Tai Chi regimens for knee osteoarthritis management.
Conclusion
This study highlights the benefits of a 14-week Tai Chi program in improving clinical symptoms and biomechanics in elderly patients with KOA. Tai Chi effectively alleviated pain, stiffness, and functional limitations while improving joint ROM, joint loading, and muscle activation. These findings underscore Tai Chi’s potential as an effective, low-impact, and accessible therapeutic approach for managing KOA and improving overall quality of life.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to privacy issues. However, data will be available upon formal request to the corresponding author.
Abbreviations
- KOA:
-
Knee osteoarthritis
- ROM:
-
Range of motion
- sEMG:
-
Surface Electromyography
- RMS:
-
Root Mean Square
- WOMAC:
-
Western Ontario and McMaster Universities Osteoarthritis
- BBS:
-
Berg Balance Scale
- SF-12:
-
Short Form 12 Health Survey
References
Kolasinski, S. L. et al. 2019 American college of rheumatology/arthritis foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Rheumatol. 72, 220–233 (2020).
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396, 1204–1222 (2020).
Murray, C. J. L. Findings from the global burden of disease study 2021. Lancet 403, 2259–2262 (2024).
Ji, S. et al. Prevalence and factors associated with knee osteoarthritis among middle-aged and elderly individuals in rural Tianjin: a population-based cross-sectional study. J. Orthop. Surg. Res. 18, 266 (2023).
Duong, V. et al. Evaluation and treatment of knee pain: A review. JAMA 330, 1568–1580 (2023).
Sharma, L. Osteoarthritis of the knee. N Engl. J. Med. 384, 51–59 (2021).
Wen, Y-R. et al. Are Mind-Body exercise beneficial for treating pain, function, and quality of life in Middle-Aged and old people with chronic pain?? A systematic review and Meta-Analysis. Front. Aging Neurosci. 14 https://doi.org/10.3389/fnagi.2022.921069 (2022).
Chen, Y-W. et al. The effect of Tai Chi on four chronic conditions-cancer, osteoarthritis, heart failure and chronic obstructive pulmonary disease: a systematic review and meta-analyses. Br. J. Sports Med. 50, 397–407 (2016).
Zou, L. et al. Effects of Tai Chi on lower limb proprioception in adults aged over 55: A systematic review and Meta-Analysis. Arch. Phys. Med. Rehabil. 100, 1102–1113 (2019).
Zou, L. et al. Tai Chi for chronic illness management: synthesizing current evidence from Meta-Analyses of randomized controlled trials. Am. J. Med. 134, 194–205e12 (2021).
Dixon, P. C. et al. Muscular co-contraction is related to varus thrust in patients with knee osteoarthritis. Clin. Biomech. (Bristol Avon). 60, 164–169 (2018).
Hodges, P. W. et al. Increased duration of co-contraction of medial knee muscles is associated with greater progression of knee osteoarthritis. Man. Ther. 21, 151–158 (2016).
Davis, E. M. et al. Longitudinal evidence links joint level mechanics and muscle activation patterns to 3-year medial joint space narrowing. Clin. Biomech. (Bristol Avon). 61, 233–239 (2019).
Wang, C. et al. Comparative effectiveness of Tai Chi versus physical therapy for knee osteoarthritis: A randomized trial. Ann. Intern. Med. 165, 77–86 (2016).
Zhu, Q. et al. Effects of Tai Ji Quan training on gait kinematics in older Chinese women with knee osteoarthritis: A randomized controlled trial. J. Sport Health Sci. 5, 297–303 (2016).
Hawker, G. A. et al. Measures of adult pain: visual analog scale for pain (VAS pain), Numeric Rating scale for pain (NRS pain), McGill pain Questionnaire (MPQ), Short-Form McGill pain Questionnaire (SF-MPQ), Chronic pain Grade scale (CPGS), Short Form-36 Bodily pain scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis pain (ICOAP). Arthritis Care Res. (Hoboken). 63 (Suppl 11), S240–252 (2011).
Altman, R. et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and therapeutic criteria committee of the American rheumatism association. Arthritis Rheum. 29, 1039–1049 (1986).
Eldridge, S. M. et al. Defining feasibility and pilot studies in Preparation for randomised controlled trials: development of a conceptual framework. PLOS ONE. 11, e0150205 (2016).
Lancaster, G. A., Dodd, S. & Williamson, P. R. Design and analysis of pilot studies: recommendations for good practice. J. Eval Clin. Pract. 10, 307–312 (2004).
Pan, J. et al. Biomechanical analysis of lower limbs during stand-to-sit tasks in patients with early-stage knee osteoarthritis. Front. Bioeng. Biotechnol. 11 https://doi.org/10.3389/fbioe.2023.1330082 (2023).
Cheng, L. et al. Effects of platelet-rich plasma combined with isometric quadriceps contraction on cartilage in a rat model of knee osteoarthritis. Regen Ther. 26, 469–477 (2024).
Chang, S., Cheng, L. & Liu, H. Effects of three-duration Tai-Chi exercises on depression and sleep quality in older women. Eur. Geriatr. Med. 15, 1141–1148 (2024).
Hubley-Kozey, C. L. et al. Neuromuscular alterations during walking in persons with moderate knee osteoarthritis. J. Electromyogr. Kinesiol. 16, 365–378 (2006).
Wang, C. et al. Tai Chi is effective in treating knee osteoarthritis: a randomized controlled trial. Arthritis Rheum. 61, 1545–1553 (2009).
Lee, A. C. et al. Effects of Tai Chi versus physical therapy on mindfulness in knee osteoarthritis. Mindfulness (N Y). 8, 1195–1205 (2017).
Mao, M. et al. The effect of Tai Chi lower extremity exercise on the balance control of older adults in assistant living communities. BMC Complement. Med. Ther. 24, 112 (2024).
Ghandali, E. et al. The effect of Tai Chi exercises on postural stability and control in older patients with knee osteoarthritis. J. Bodyw. Mov. Ther. 21, 594–598 (2017).
Hu, L. et al. Tai Chi exercise can ameliorate physical and mental health of patients with knee osteoarthritis: systematic review and metaanalysis. Clin. Rehabil. 35, 64–79 (2021).
Graber, K. A. et al. Hip and trunk muscle activity and mechanics during walking with and without unilateral weight. J. Appl. Biomech. 37, 351–358 (2021).
Griffin, T. M. & Guilak, F. The role of mechanical loading in the onset and progression of osteoarthritis. Exerc. Sport Sci. Rev. 33, 195 (2005).
Zhou, M. et al. Effect of Tai Chi on muscle strength of the lower extremities in the elderly. Chin. J. Integr. Med. 22, 861–866 (2016).
Wayne, P. M. et al. Tai Chi training’s effect on lower extremity muscle co-contraction during single- and dual-task gait: Cross-sectional and randomized trial studies. PLOS ONE. 16, e0242963 (2021).
You, Y. et al. Effects of Tai Chi exercise on improving walking function and posture control in elderly patients with knee osteoarthritis: A systematic review and meta-analysis. Medicine 100, e25655 (2021).
Roos, P. E., Mituniewicz, A. & Liu, W. Biomechanical joint loading mechanism of Tai Chi gait in individuals with knee osteoarthritis: A pilot simulation study. Osteoarthr. Cartil. Open. 3, 100158 (2021).
Taniguchi, M. et al. Quantity and quality of the lower extremity muscles in women with knee osteoarthritis. Ultrasound Med. Biol. 41, 2567–2574 (2015).
Tayfur, B. et al. Neuromuscular joint function in knee osteoarthritis: a systematic review and meta-analysis. Ann Phys. Rehabil Med :101662. (2022).
Chen, P-Y. et al. Impacts of Tai Chi exercise on functional fitness in community-dwelling older adults with mild degenerative knee osteoarthritis: a randomized controlled clinical trial. BMC Geriatr. 21, 449 (2021).
Trepczynski, A. et al. Impact of antagonistic muscle co-contraction on in vivo knee contact forces. J. Neuroeng. Rehabil. 15, 101 (2018).
Funding
This work was supported by the Guangzhou Sports Science and Technology Collaborative Innovation Center (2023B04 J0466), Open Fund of the Guangdong Provincial Key Laboratory of Physical Activity and Health Promotion (2021B1212040014), Higher Education Teaching Reform Project of Guangdong Provincial Department of Education (Strategy and Practice Exploration of Innovative Training Mode for Sports Rehabilitation Professionals Under the Guidance Of Supply- Side Reform), The Basic and Applied Basic Research Project of Guangzhou City (2023 A04 J0554), and The Key Scientific Research Project of Guangdong Province Education Department (2024ZDZX2064).
These funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The sponsor approved the design, methods, subject recruitment, data collections and analysis in the grant proposal.
Author information
Authors and Affiliations
Contributions
J.P. was responsible for experimental design, manuscript drafting, and revisions. Z.X., S.Y., Z.H. and H.S. contributed to data collection, analysis, and interpretation. X.Z. and B.L. coordinated the research, supervised the project, and critically reviewed the manuscript. All authors approved the final manuscript and agreed to be accountable for their respective contributions.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Resource availability
The datasets generated and/or analyzed during the current study are not publicly available due to privacy issues. However, data will be available upon formal request to the corresponding author.
Ethics declarations
The project was approved by the Chinese Clinical Trial Registry (Registration No. ChiCTR2300078229; Initial registration date: 01/12/2023). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pan, J., Xie, Z., Ye, S. et al. The effects of Tai Chi on clinical outcomes and gait biomechanics in knee osteoarthritis patients: a pilot randomized controlled trial. Sci Rep 15, 18495 (2025). https://doi.org/10.1038/s41598-025-03943-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-03943-3