Abstract
This cross-sectional study examined the health impacts of occupational dust exposure on workers in Fujian Province, China, using data collected from 2020 to 2021. The primary objective was to assess the associations between occupational dust exposure and several adverse health outcomes, including abnormal chest X-ray (Abn-CXR), abnormal pulmonary function tests (Abn-PFTs), pneumoconiosis (PC), abnormal electrocardiograms (Abn-ECGs), abnormal liver function tests (Abn-LFTs), hypertension (HTN), and hearing loss (HL). logistic regression models were employed to identify significant risk factors. Stratified analyses by age and gender were performed to evaluate demographic differences in health risks. The results showed that workers currently employed, those with over 10 years of dust exposure, and workers exposed to silica, cement, or coal dust had a higher risk of Abn-CXR, Abn-PFTs, PC, Abn-ECGs, Abn-LFTs, HTN, and HL. Stratified analyses further revealed that male workers and individuals over 40 years old experienced a higher risk of abnormal health outcomes. These findings underscore the urgent need for targeted interventions, improved protective measures, and stricter occupational safety regulations to reduce the health burden associated with dust exposure in the workplace.
Similar content being viewed by others
Introduction
Occupational dust comprises heterogeneous mixtures of inhalable particulate matter generated during industrial processes, with its health hazards arising from the complex interplay between physical characteristics (e.g., particle size distribution and morphology) and chemical composition (e.g., crystalline silica content, and heavy metal contaminants)1,2,3,4. Globally, occupational dust exposure imposes a substantial disease burden. According to estimates from the World Health Organization (WHO), approximately 860,000 preventable deaths attributable to occupational dust exposure occur annually, with nearly 30% of these involving non-respiratory pathologies such as cardiovascular and metabolic disorders5,6. Emerging evidence suggests that occupational dust exposure is a multi-system health hazard, with effects extending beyond classical respiratory diseases (e.g., pneumoconiosis) to include cardiovascular, metabolic, and sensory system impairments, thereby constituting a critical challenge in global occupational health7,8,9,10.
Occupational dust may induce multiorgan toxicity through both shared pathological mechanisms (e.g., systemic inflammation and oxidative stress) and substance-specific pathways11,12. Inhaled dust particles, regardless of their composition, commonly trigger alveolar macrophages to release pro-inflammatory mediators (e.g., TNF-α and IL-6) into systemic circulation, leading to chronic low-grade inflammation—a key contributor to cardiovascular dysfunction13,14. This mechanism is supported by longitudinal evidence of elevated blood pressure among copper–gold miners over 5-year follow-up periods15. The pathogenic cascade begins when inhaled particles initiate a series of molecular events. For example, crystalline silica activates the NLRP3 inflammasome pathway, promoting irreversible pulmonary fibrosis16,17,18, while cement dust exposure demonstrates progressive dose-dependent declines in pulmonary function parameters19,20,21. Moreover, certain metal dusts (e.g., aluminum and chromium) have been found to disrupt metabolic homeostasis through oxidative stress-mediated DNA damage and mitochondrial dysfunction, while coal dust containing polycyclic aromatic hydrocarbons exhibits distinct multi-system toxicity profiles22,23. Epidemiological studies have identified specific “composition-target organ” relationships: silica is predominantly associated pulmonary disease, metallic dust with cardiometabolic disorders, and coal dust with impaired pulmonary ventilation capacity24,25,26,27,28. These findings collectively underscore the multi-system health risks posed by occupational dust exposure, highlighting the need for strengthened health surveillance among exposed workers.
Despite increasing awareness of occupational dust-related adverse health impacts, China, as the world’s primary manufacturing center, lacks systematic investigations into the multi-system effects because of dust exposure29. Existing domestic research has largely focused on single dust types or isolated health outcomes, leaving a critical gap in understanding the full scope of dust-related multi-system health consequences. To address this gap, we analyzed the occupational health surveillance data from Fujian Province (2020–2021) to: (1) describe the distribution of abnormalities across multiple organ systems (e.g., radiographic anomalies, electrocardiographic abnormalities, and pulmonary function impairment) among dust-exposed workers stratified by demographic and occupational characteristics; and (2) analyze associations between occupational factors (e.g., dust type and exposure duration) and health risks. Findings of this study may provide implications for the development of dust-related occupational health management strategies and contribute China-specific data to the global literature on occupational dust-related health effects.
Methods
Data sources and study participants
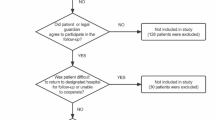
This cross-sectional study was conducted as part of the "Implementation Plan for Occupational Disease Prevention and Control in 2021" issued by the General Office of China’s National Health Commission. Health monitoring data were collected from workers exposed occupational dust between January 1, 2020, and December 31, 2021, in Fujian Province. The 2020 dataset included demographic and occupational characteristics such as age, sex, industry type, job category, income level, duration of dust exposure, employment status, company size, as well as medical examinations including chest X-rays and electrocardiograms. In 2021, the health surveillance was expanded to include blood pressure measurements, pulmonary function tests, liver function tests, and hearing loss assessments. A total of 8915 participants completed both chest X-ray and electrocardiogram examinations. Among them, 5693 underwent both blood pressure and pulmonary function tests, while 2,302 for hearing loss assessments, and 2220 for liver function tests.
Assessment of dust exposure categories
In this study, occupational exposure to dust was assessed for various types, including cement, silica, coal, metal, and others (e.g., limestone dust, wood dust, and gypsum dust). The monitoring was conducted across high-risk industries such as mining, cement manufacturing, metal processing, thermal power generation, and construction. All monitoring procedures were conducted in accordance with the national standards for determination of dust in the air of workplace (GBZ/T 192 series standards)30,31.
Dust exposure classification was based on a two-step approach integrating industry type and job category. Initial categorization was based on industry characteristics and primary dust exposure types. For example, workers in cement manufacturing were classified as exposed to cement dust, those in mining/stone processing as silica dust, coal mining/thermal power industry workers as coal dust, metal smelting/machining workers as metal dust, and construction/other manufacturing workers as other dust exposures. Further refinement was based on specific job tasks. Drillers and tunnelers in mining were classified as silica dust-exposed, coal pulverizer operators as coal dust-exposed, and welders as metal dust-exposed. For complex cases involving mixed exposures, a panel of occupational health experts conducted a standardized review to ensure accurate classification. A control group of workers undergoing pre-employment examinations, with no history of occupational dust exposure, was included for comparison.
Classification of occupational characteristics
Duration of dust exposure was calculated in years based on employment records. Employment status was categorized as either “pre-employment” or “currently employed”. Company size was classified as large, medium, or small based on production capacity. Income levels were classified as high, medium, or low, according to job category and prevailing industry wage standards.
Measurements of variables
Abnormal chest X-ray (Abn-CXR)
Chest X-ray of all participants were independently evaluated by two physicians. According to the 2022 International Classification of Radiographs of Pneumoconioses (ILO) standards and general radiological practice, Abn-CXR were defined as long as meeting any of the following criteria32,33,34:
-
(1)
Small opacities presence of small opacities with profusion ≥ 1/0 or 0/1 (i.e., at least one lung zone showing definite or suspected small opacities).
-
(2)
Large opacities dense shadows ≥ 1 cm in diameter (Type A: 1–5 cm; Type B: > 5 cm but not exceeding the area of the right upper lung zone; Type C: exceeding Type B), either unilateral or bilateral.
-
(3)
Pleural abnormalities pleural thickening (> 3 mm, measured at the lateral chest wall or diaphragm), pleural plaques or calcifications.
-
(4)
Non-specific changes Increased, coarse, or disorganized lung markings, solitary pulmonary nodules or other non-specific findings (e.g., old fibrotic foci, calcifications).
Abnormal pulmonary function tests (Abn-PFTs)
Pulmonary function tests, including forced vital capacity (FVC), forced expiratory volume in 1 s (FEV₁), and the FEV₁/FVC ratio, were performed by trained technicians following standardized protocols. Abn-PFTs was defined according to the American Thoracic Society/European Respiratory Society (ATS/ERS) guidelines based on the following criteria for ventilatory impairment: for an obstructive ventilatory defect, FEV₁/FVC < 0.7 (fixed ratio) or < lower limit of normal (LLN) plus FEV₁ < 80% predicted; for a restrictive ventilatory defect, FVC < 80% predicted plus FEV₁/FVC ≥ LLN plus total lung capacity (TLC) < 80% predicted; and for a mixed ventilatory defect, FEV₁/FVC < LLN plus FVC < 80% predicted35,36. In this study, Abn-PFTs was defined as meeting any one of the above criteria.
Pneumoconiosis (PC)
PC was diagnosed based on abnormal chest X-ray, combined with the following criteria32,37,38:
-
(1)
Small opacities (predominantly rounded or irregular) with a profusion of ≥ 1/1 involving ≥ 2 lung zones; or the presence of large opacities (≥ 10 mm in diameter, classified as A, B, or C).
-
(2)
Occupational exposure evidence: a documented history of occupational dust exposure (e.g., to silica, coal dust, or cement dust) for ≥ 1 year.
-
(3)
Exclusion of other diseases: non-occupational diseases such as tuberculosis, lung cancer, and sarcoidosis were excluded through clinical assessment.
Abnormal electrocardiograms (Abn-ECGs)
EGG measurements were performed using a routine 12-lead electrocardiogram. All measurements were taken with participants lying supine, ensuring clean skin. The ECG results were independently evaluated by two trained physicians.
Hypertension (HTN)
HTN was defined according to the WHO/ISH recommendations, with systolic BP ≥ 140 mmHg or diastolic BP ≥ 90 mmHg39.
Abnormal liver function tests (Abn-LFTs)
Abn-LFTs were defined as any of the following biomarkers exceeding the reference ranges: AST (0–37 U/L for men, 0–31 U/L for women); ALT (0–40 U/L for men, 0–31 U/L for women); ALP (40–129 U/L for men, 35–104 U/L for women); GGT (11–51 U/L for men, 7–33 U/L for women); or TBIL (> 17.1 μmol/L)40.
Hearing loss (HL)
HL was defined as the average hearing threshold of > 25 dB in either ear across the frequencies of 500, 1000, 2000, 3000, 4000, 6000, and 8000 Hz41,42,43,44.
Statistical analysis
Continuous variables were expressed as means ± standard deviation (SD), while categorical variables were described as frequencies (n) and proportions (%). Logistic regression models were used to explore risk factors for abnormal health indicators, with Abn-CXR, Abn-PFTs, PC, Abn-ECGs, HTN, Abn-LFTs and HL as dependent variables, and company size, employment status, duration of dust exposure and dust categories as independent variables. Stratified analyses by sex and age were performed to assess potential differences in the associations across these subgroups. Odds ratios (OR) with 95% confidence intervals (CI) were calculated for all variables. P value < 0.05 was considered as statistically significant. All analyses were performed using R software (version 4.3.2).
Ethical considerations and consent statement
Ethical approval for this study and its research protocol were obtained from the Biomedical Research Ethics Review Committee of Fujian Medical University. The monitoring activities were carried out across the nine prefecture-level cities and the Pingtan Comprehensive Experimental Area within Fujian Province. The monitoring activities were conducted at the prefecture level, encompassing all subordinate cities, counties, and districts within each jurisdiction. The Fujian Center for Prevention and Control of Occupational Diseases and Chemical Poisoning was responsible for assigning tasks related to the monitoring of occupational disease hazards in workplaces across the various municipal administrative regions.
Additionally, the objectives of the monitoring activities were clearly communicated to the relevant manufacturing entities by the local governments. Designated departments within each manufacturing enterprise were responsible for obtaining informed written consent from all participants. Participation in the health monitoring was entirely voluntary, and individuals had the right to decline or withdraw from the survey at any time according to their personal circumstances. The confidentiality of all participants’ information was rigorously maintained throughout the data collection process and the entire investigation period. Furthermore, all methodologies employed in this study were conducted in strict adherence to the principles outlined in the Declaration of Helsinki.
Results
Population characteristics
The study included a total of 8915 workers from Fujian Province, China, with 3222 participants recruited in 2020 and 5693 in 2021. As shown in Table 1, the majority of participants were male (81.4%), and more than half (59.4%) were aged over 40 years old. A significant proportion of participants were from small-sized companies (43.0%) and most were currently employed (82.6%). Over two-thirds of the participants (70.9%) had been exposed to dust for less than 10 years. The income distribution showed that 44.3% of participants were classified as low-income. Regarding dust exposure, cement dust was the most common type (31.1%), followed by silica dust (23.2%), coal dust (17.6%), metal dust (10.6%), and other types (7.8%), while 9.7% of workers reported no occupational dust exposure.
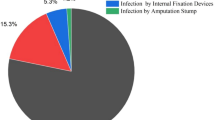
Prevalence of health outcomes in 2020–2021
The prevalence of abnormal health outcomes among workers exposed to occupational dust during 2020–2021 is summarized in Table 2. Among them, the prevalence of Abn-CXR was higher in males (83.9%), workers aged > 40 years (73.7%), those employed in small enterprises (52.5%), middle-income workers (41.1%), currently employed workers (87.5%) and workers exposed to silica dust (32.5%). PC prevalence was elevated in workers aged > 40 years (77.4%), males (85.2%), low-income earners (60.0%), employees of medium-sized enterprises (43.9%), currently employed individuals (93.5%), and silica dust-exposed workers (38.7%), while no cases of PC were reported among workers without any occupational dust exposure. Abn-ECGs were more common in males (85.0%), workers aged > 40 years (60.2%), those employed in medium-sized enterprises (37.6%), currently employed workers (85.6%), low-income workers (51.6%), and workers exposed to cement dust (29.3%). Other abnormal findings (Abn-PFTs, HTN, Abn-LFTs and HL) followed similar demographic patterns, being more prevalent in males, currently employed workers, those with low-to-middle incomes, workers aged > 40 years, and those exposed to silica or cement dust.
Logistic regression analysis of occupational risk factors in 2020–2021
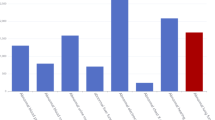
As shown in Fig. 1 and Table S1, workers in medium- or large-sized enterprises exhibited a significantly higher risk of Abn-ECGs (OR = 2.96, 95% CI 2.62–3.36), Abn-PFTs (OR = 1.28, 95% CI 1.07–1.53), and HL (OR = 2.20, 95% CI 1.76–2.75), but a lower risk of Abn-CXR (medium enterprises: OR = 0.72, 95% CI 0.63–0.84; large enterprises: OR = 0.58, 95% CI: 0.47–0.70). Dust exposure exceeding 20 years significantly increased the risk of various health abnormalities, particularly PC (OR = 5.51, 95% CI 3.61–8.42). Compared to pre-employment status, currently employed workers showed a significantly elevated risk of all health outcomes, including Abn-CXR (OR = 1.44, 95% CI 1.18–1.75), Abn-ECGs (OR = 1.35, 95% CI 1.19–1.54), Abn-PFTs (OR = 1.50, 95% CI 1.23–1.84), HTN (OR = 1.26, 95% CI 1.05–1.50), Abn-LFTs (OR = 1.37, 95% CI: 1.11–1.67), HL(OR = 1.42, 95% CI 1.12–1.80) and PC (OR = 2.82, 95% CI 1.48–5.38). Compared to non-exposed workers, those exposed to cement dust had an increased risk of Abn-ECGs (OR = 1.28, 95% CI 1.06–1.53), Abn-LFTs (OR = 1.45, 95% CI 1.03–2.04), and HL (OR = 1.94, 95% CI 1.32–2.83). Silica dust exposure was associated with an increased risk of nearly all examined conditions. Coal dust mainly elevated the risk of Abn-CXR, Abn-ECGs, Abn-PFTs, and HL. Metal dust predominantly increased the risk of Abn-CXR, Abn-ECGs, Abn-PFTs, and HTN. Other dust types primarily contributed to Abn-CXR, Abn-PFTs, and HTN. Compared to cement dust, silica dust posed the highest risk for PC (OR = 2.75, 95% CI 1.77–4.29), followed by coal dust (OR = 1.74, 95% CI: 1.05–2.88) and metal dust (OR = 2.04, 95% CI 1.16–3.61).
Logistic regression analysis of occupational risk factors in 2020–2021: (a) Logistic regression analysis of the association between occupational risk factors and abnormal chest X-ray. (b) Logistic regression analysis of the association between occupational risk factors and abnormal pulmonary function tests. (c) Logistic regression analysis of the association between occupational risk factors and pneumoconiosis. (d) Logistic regression analysis of the association between occupational risk factors and abnormal electrocardiograms. (e) Logistic regression analysis of the association between occupational risk factors and hypertension. (f) Logistic regression analysis of the association between occupational risk factors and abnormal liver function tests. (g) Logistic regression analysis of the association between occupational risk factors and hearing loss. Models were adjusted for income level, gender and age. *p < 0.05, **p < 0.01, ***p < 0.001.
Gender stratified analysis of health outcomes in 2020–2021
As illustrated in Fig. 2 and Table S2, gender-stratified analysis revealed distinct patterns in dust-related health risks. Among male workers, employment in medium- and large-sized enterprises was associated with a lower risk of Abn-CXR (medium: OR = 0.62, 95% CI 0.53–0.73; large: OR = 0.50, 95% CI 0.40–0.62), whereas no such association was observed in female workers. Compared to pre-employment status, both male and female workers exhibited an increased risk of Abn-CXR, Abn-ECGs, Abn-PFTs, and Abn-LFTs during current employment. However, the association between current employment and HL or PC was only found in male workers. Long-term dust exposure (> 10 years) significantly elevated the risk of nearly all examined health conditions in males. In contrast, among female workers, 10–20 years of dust exposure only increased the risk of abnormal Abn-CXR (OR = 2.36, 95% CI 1.58–3.52), and > 20 years of exposure showed no statistically significant association with Abn-LFTs, HL, or PC. Furthermore, silica dust exerted multi-system health effects in male workers, significantly increasing the risks of Abn-CXR, Abn-PFTs, Abn-ECGs, Abn-LFTs, HTN, HL and PC, whereas coal dust and metal dust exposures in males primarily increased the risks of Abn-CXR, Abn-ECGs, and Abn-PFTs. Among female workers, silica dust only significantly elevated the risks of Abn-CXR and PC; coal dust was only associated with Abn-PFTs; and metal dust only increased Abn-LFTs and PC risk. These results indicate that the impact of occupational dust exposure on health outcomes is more widespread among male workers.
Gender stratified analysis of occupational risk factors in 2020–2021. (a) Gender stratified analysis of occupational risk factors and abnormal chest X-ray. (b) Gender stratified analysis of occupational risk factors and abnormal pulmonary function tests. (c) Gender stratified analysis of occupational risk factors and pneumoconiosis. (d) Gender stratified analysis of occupational risk factors and abnormal electrocardiograms. (e) Gender stratified analysis of occupational risk factors and abnormal hypertension. (f) Gender stratified analysis of occupational risk factors and abnormal liver function tests. (g) Gender stratified analysis of occupational risk factors and hearing loss. Models were adjusted for income level and age. *p < 0.05, **p < 0.01, ***p < 0.001.
Age stratified analysis of health outcomes in 2020–2021
Age-stratified analysis (Fig. 3 and Table S3) revealed distinct patterns of occupational health risks across different age groups. Among workers aged > 40 years, current employment was associated with increased risks for nearly all health conditions, while no statistically significant associations were observed between current employment with PC, HTN and HL in the age group ≤ 40 years. In the age group > 40 years, workers with > 10 years of dust exposure demonstrated elevated risks for almost all conditions, with those exposed > 20 years exhibiting higher risks compared to those with 10–20 years of exposure. Conversely, among ≤ 40-year-old workers, > 10 years of dust exposure showed no significant association with Abn-LFTs, and an increased risk of PC was only evident in those with 10–20 years of exposure. The health impacts varied significantly by dust type. For workers > 40 years, silica and coal dust exposures were significantly associated with Abn-CXR, Abn-PFTs, HL and PC risk, while metal dust primarily increased the risks of Abn-CXR, Abn-ECGs and PC. Among workers ≤ 40-year-old, all dust types showed no associations with PC risk when compared to cement dust. However, silica dust was associated with increased risks of Abn-CXR, HTN, Abn-LFTs and HL when compared to non-exposed workers. These findings suggest that occupational dust exposures impact health outcomes differently by age, with older workers showing more pronounced effects of long-term cumulative exposure on cardiopulmonary function and pneumoconiosis risk.
Age stratified analysis of occupational risk factors in 2020–2021. (a) Age stratified analysis of occupational risk factors and abnormal chest X-ray. (b) Age stratified analysis of occupational risk factors and abnormal pulmonary function tests. (c) Age stratified analysis of occupational risk factors and abnormal pneumoconiosis. (d) Age stratified analysis of occupational risk factors and abnormal electrocardiograms. (e) Age stratified analysis of occupational risk factors and abnormal hypertension. (f) Age stratified analysis of occupational risk factors and abnormal liver function tests. (g) Age stratified analysis of occupational risk factors and abnormal hearing loss. Models were adjusted for income level and gender. *p < 0.05, **p < 0.01, ***p < 0.001.
Sensitivity analysis addressing healthy worker effect bias
To assess the potential bias of the Healthy Worker Effect (HWE), we additionally included data from 198 workers who had left employment but had complete health examination records during 2020–2021. These individuals had at least 1 year of service and clearly defined exposure to occupational dust factors for sensitivity analysis. After inclusion, nearly all health outcome prevalence rates increased: the prevalence of Abn-CXR rose from 11.4 to 12.6%, Abn-PFTs increased from 16.1 to 16.9%, and PC elevated from 1.7 to 2.6%. The results of the sensitivity analysis are shown in Table S4. Among workers with long-term dust exposure (> 10 years), the adjusted ORs for PC risk increased from 4.049 (P < 0.001) to 5.204 (P < 0.001) in the 10–20 year exposure group and from 5.514 (P < 0.001) to 7.391 (P < 0.001) in the > 20 year exposure group. Similarly, this pattern was also observed for all other health outcomes: Abn-CXR increased from OR = 2.099 (P < 0.001) to 2.275 (P < 0.001), Abn-PFTs from OR = 1.543 (P < 0.001) to 1.658 (P < 0.001) and HL from OR = 1.896 (P < 0.001) to 2.030 (P < 0.001) in the > 20-year exposure group. Dust-specific analyses showed that silica dust exposure led to increased risks of Abn-CXR (OR = 2.448, P < 0.001 to OR = 2.748, P < 0.001), PC (OR = 2.753, P < 0.001 to OR = 3.363, P < 0.001), Abn-PFTs (OR = 1.696, P = 0.003 to OR = 1.830, P < 0.001) and HL (OR = 2.373, P < 0.001 to OR = 2.529, P < 0.001). Similarly, coal and metal dust exposures demonstrated elevated ORs for Abn-CXR, Abn-PFTs and PC. These findings confirm the presence of HWE but also demonstrate that the positive associations between long-term dust exposure (> 10 years) and specific dust types (silica, coal, and metal) with all health outcomes remain robust.
Discussion
This study systematically evaluated the comprehensive health impacts of occupational dust exposure, elucidating the associations between dust types, exposure duration, demographic characteristics and multi-system health risks. The results demonstrated that workers with over 10 years of dust exposure and currently employed workers exhibited significantly increased risks of Abn-ECGs, Abn-PFTs, HTN, Abn-LFTs, HL and PC. Interestingly, employees in large and medium-sized enterprises showed lower risks of abnormal Abn-CXR compared to those in small-sized enterprises. Distinct variations were observed in health impacts across different dust types, with silica dust demonstrating particularly extensive effects on health outcomes. Furthermore, significant differences in health risks were identified across gender and age groups, highlighting the necessity for targeted intervention strategies.
This study demonstrates that occupational dust exposure is significantly associated with pulmonary health risks, particularly strongly linked to Abn-CXR, Abn-PFTs, and the development of PC. Both current workplace exposure and > 10 years of dust exposure were found to significantly impact lung health, with silica dust-exposed workers showing particularly elevated PC risks, while cement and coal dust-exposed workers also exhibited elevated risks of Abn-PFTs. Additionally, the study also revealed modifying effects of age and gender, with male workers exhibiting more extensive pulmonary health impacts from long-term dust exposure. The influence of different dust types on PC risk was primarily concentrated in workers over 40 years old, suggesting that cumulative long-term exposure is a key driver in pulmonary disease development. Company size demonstrated dual effects on workers’ pulmonary health: medium/large companies showed lower risks of Abn-CXR, potentially due to better protective measures and occupational health education. However, these workers paradoxically exhibited higher risks of Abn-PFTs, which may be attributed to greater work intensity or higher levels of dust exposure. The mechanisms warrant further investigation45,46. Overall, these findings align with international research, reinforcing the associations between long-term dust exposure, specific dust types, and occupational pulmonary diseases47,48.
Beyond the well-documented pulmonary diseases, occupational dust exposure exhibits multi-system health effects on workers, particularly on cardiovascular consequences. Chronic dust exposure has been shown to significantly increase the risk of cardiac arrhythmias among workers49. Furthermore, long-term high-level exposure to particulate matter demonstrates a dose-dependent association with elevated myocardial infarction risk50. Our findings reveal that silica, cement, and metal dust exposures not only significantly increased the risks of Abn-CXR and PC but also correlated with a higher prevalence of Abn-ECGs. These effects may be mediated through shared pathological mechanisms, including systemic inflammation and oxidative stress51. Notably, we observed a significantly increased risk of Abn-ECGs among male workers with 11–20 years of exposure, while this association was not statistically significant in female workers. This gender disparity may stem from a limited statistical power due to a smaller female sample size or to the potential cardioprotective effects of estrogen through vascular endothelial modulation52. Future studies with larger female samples are warranted to validate these findings and further explore sex-specific pathophysiological mechanisms underlying these differences.
HTN is closely associated with overweight/obesity and dyslipidemia and remains a major contributor to cardiovascular diseases53. Epidemiological studies have revealed that exposure to particulate matter contributes to elevated cardiovascular mortality and morbidity, particularly among mining operation workers. Increased blood pressure has been identified as a significant health risk among dust-exposed workers. For instance, research had found significantly higher blood pressure levels among welders exposed to welding fumes compared to controls54. Similarly, hypertension and obesity have been reported as prevalent health conditions among U.S. coal miners55. In our study, male workers with > 10 years of dust exposure and those currently employed in dust-related occupations exhibited elevated hypertension risks, particularly among those exposed to silica and metal dust. These findings underscore the substantial cardiovascular health impacts of occupational dust exposure and emphasize the need for targeted health monitoring and interventions. Future research should incorporate more comprehensive clinical indicators to better characterize and address cardiovascular risks among dust-exposed workers.
Noise-induced hearing loss (NIHL) is increasingly prevalent in low-and middle-income countries (LMICs), where noise control measures and hearing protection are often inadequate56. Workers in industries such as mining, construction, printing, sawmills, and cement plants are particularly vulnerable to NIHL57. In this study, we found that male workers with over 10 years of occupational dust exposure had significantly increased HL risks, and most associations between different dust types and HL were observed in workers aged > 40 years, potentially due to the combined effects of age-related hearing loss (ARHL) and cumulative long-term occupational exposure. This finding aligns with the observed trend of more pronounced pulmonary function decline with longer dust exposure duration19. Furthermore, workers exposed to cement, silica, and coal dust exhibited particularly elevated HL risks, likely reflecting the synergistic effect of noise and specific dust types in high-intensity workplaces58,59. Based on these findings, incorporating hearing screening into occupational health assessments is strongly recommended, especially for older workers in high-noise and high-dust environments, to enable early identification and intervention for hearing impairment.
Study limitations
There are several limitations to this study. First, the cross-sectional design precludes establishing causal relationships between occupational exposures and health outcomes, although significant associations were observed. Second, although we included data from workers who left employment during the survey period in our sensitivity analyses, residual HWE bias may still persist because we could not obtain detailed information on workers who left specifically due to health-related reasons. Third, this study lacked smoking data. Given the reported 40–50% smoking prevalence among male adults in Fujian Province60,61, smoking could be a potential confounding factor in our assessment of Abn-PFTs and cardiovascular outcomes. Future investigations would benefit from including detailed smoking history to better delineate the specific effects of occupational dust exposure. Finally, daily environmental exposure data were not collected in this study, limiting evaluation of daily environmental risks that could influence health outcomes. Future studies should use longitudinal designs to establish causality, improve occupational health records to better assess HWE, and collect key confounders such as smoking and daily environmental exposures.
Conclusions
This comprehensive study highlights the multi-system health risks associated with occupational dust exposure among Chinese workers. Our findings demonstrate that long-term exposure (> 10 years), especially to silica, cement, coal, and metal dust, was strongly associated with adverse outcomes across several domains, including pulmonary (Abn-CXR, Abn-PFTs, PC), cardiovascular (Abn-ECGs, HTN), metabolic (Abn-LFTs), and auditory (HL) health. The health impacts exhibit distinct demographic patterns, with male workers and those aged > 40 years showing more pronounced risks. These findings underscore the urgent need for enhanced occupational health protections, targeted surveillance, and interventions to mitigate the health burdens of dust exposure in the workplace.
Data availability
The datasets used during the current study are available from the corresponding author on reasonable request.
References
Australia, S. W. Workplace Exposure Standard-Flour Dust (cereal) (Safe Work Australia, 2019).
Schenker, M. Exposures and health effects from inorganic agricultural dusts. Environ. Health Perspect. 108(Suppl 4), 661–664. https://doi.org/10.1289/ehp.00108s4661 (2000).
Kasongo, J., Alleman, L. Y., Kanda, J. M., Kaniki, A. & Riffault, V. Metal-bearing airborne particles from mining activities: A review on their characteristics, impacts and research perspectives. Sci. Total Environ. 951, 175426. https://doi.org/10.1016/j.scitotenv.2024.175426 (2024).
Ahmad, R., Akhter, Q. S. & Haque, M. Occupational cement dust exposure and inflammatory nemesis: Bangladesh relevance. J. Inflamm. Res. 14, 2425–2444. https://doi.org/10.2147/jir.S312960 (2021).
in WHO global air quality guidelines: Particulate matter (PM(2.5) and PM(10)), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide (World Health Organization © World Health Organization 2021., 2021).
Brauer, M. et al. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2162–2203. https://doi.org/10.1016/s0140-6736(24)00933-4 (2024).
Kangarlou, M. B., Saleh, E. & Dehdashti, A. Metabolic syndrome risk factors among mill workers exposed to noise and respirable dust. Sci. Rep. 15, 10440. https://doi.org/10.1038/s41598-025-93706-x (2025).
Gellissen, J., Pattloch, D. & Möhner, M. Effects of occupational exposure to respirable quartz dust on acute myocardial infarction. Occup. Environ. Med. 76, 370–375. https://doi.org/10.1136/oemed-2018-105540 (2019).
Wang, D. et al. Association of silica dust exposure and cigarette smoking with mortality among mine and pottery workers in China. JAMA Netw. Open 3, e202787. https://doi.org/10.1001/jamanetworkopen.2020.2787 (2020).
Chen, W. et al. Long-term exposure to silica dust and risk of total and cause-specific mortality in Chinese workers: A cohort study. PLoS Med. 9, e1001206. https://doi.org/10.1371/journal.pmed.1001206 (2012).
Hedbrant, A. et al. Occupational quartz and particle exposure affect systemic levels of inflammatory markers related to inflammasome activation and cardiovascular disease. Environ. Health 22, 25. https://doi.org/10.1186/s12940-023-00980-1 (2023).
Li, Y. et al. Associations of long-term exposure to air pollution and physical activity with the risk of systemic inflammation-induced multimorbidity in Chinese adults: Results from the China multi-ethnic cohort study (CMEC). BMC Public Health 23, 2556. https://doi.org/10.1186/s12889-023-17518-2 (2023).
Dostert, C. et al. Innate immune activation through Nalp3 inflammasome sensing of asbestos and silica. Science 320, 674–677. https://doi.org/10.1126/science.1156995 (2008).
Kang, H., Gu, X., Cao, S., Tong, Z. & Song, N. Integrated multi-omics analyses reveal the pro-inflammatory and pro-fibrotic pulmonary macrophage subcluster in silicosis. Ecotoxicol. Environ. Saf. 284, 116899. https://doi.org/10.1016/j.ecoenv.2024.116899 (2024).
Rodriguez-Fernandez, R. et al. Non-communicable disease risk factor patterns among mining industry workers in Papua, Indonesia: Longitudinal findings from the cardiovascular outcomes in a Papuan population and estimation of risk (COPPER) study. Occup. Environ. Med. 72, 728–735. https://doi.org/10.1136/oemed-2014-102664 (2015).
Hornung, V. et al. Silica crystals and aluminum salts activate the NALP3 inflammasome through phagosomal destabilization. Nat. Immunol. 9, 847–856. https://doi.org/10.1038/ni.1631 (2008).
Swanson, K. V., Deng, M. & Ting, J. P. The NLRP3 inflammasome: Molecular activation and regulation to therapeutics. Nat. Rev. Immunol. 19, 477–489. https://doi.org/10.1038/s41577-019-0165-0 (2019).
Bredeck, G. et al. Inhalable Saharan dust induces oxidative stress, NLRP3 inflammasome activation, and inflammatory cytokine release. Environ. Int. 172, 107732. https://doi.org/10.1016/j.envint.2023.107732 (2023).
Nordby, K. C. et al. Thoracic dust exposure is associated with lung function decline in cement production workers. Eur. Respir. J. 48, 331–339. https://doi.org/10.1183/13993003.02061-2015 (2016).
Ural, B. B. et al. Inhaled particulate accumulation with age impairs immune function and architecture in human lung lymph nodes. Nat. Med. 28, 2622–2632. https://doi.org/10.1038/s41591-022-02073-x (2022).
Skaaby, S. et al. Occupational inhalant exposures and longitudinal lung function decline. Eur. Respir. J. https://doi.org/10.1183/13993003.04341-2020 (2021).
Wise, S. S., Holmes, A. L. & Wise, J. P. Sr. Hexavalent chromium-induced DNA damage and repair mechanisms. Rev. Environ. Health 23, 39–57. https://doi.org/10.1515/reveh.2008.23.1.39 (2008).
Armstrong, B., Hutchinson, E., Unwin, J. & Fletcher, T. Lung cancer risk after exposure to polycyclic aromatic hydrocarbons: A review and meta-analysis. Environ. Health Perspect. 112, 970–978. https://doi.org/10.1289/ehp.6895 (2004).
Howlett, P., Gan, J., Lesosky, M. & Feary, J. Relationship between cumulative silica exposure and silicosis: a systematic review and dose-response meta-analysis. Thorax 79, 934–942. https://doi.org/10.1136/thorax-2024-221447 (2024).
Hoy, R. F. et al. Artificial stone-associated silicosis: A rapidly emerging occupational lung disease. Occup. Environ. Med. 75, 3–5. https://doi.org/10.1136/oemed-2017-104428 (2018).
Navas-Acien, A., Guallar, E., Silbergeld, E. K. & Rothenberg, S. J. Lead exposure and cardiovascular disease: A systematic review. Environ. Health Perspect. 115, 472–482. https://doi.org/10.1289/ehp.9785 (2007).
Cohen, R. A. et al. Lung pathology in U.S. coal workers with rapidly progressive pneumoconiosis implicates silica and silicates. Am. J. Respir. Crit. Care Med. 193, 673–680. https://doi.org/10.1164/rccm.201505-1014OC (2016).
Vanka, K. S. et al. Understanding the pathogenesis of occupational coal and silica dust-associated lung disease. Eur. Respir. Rev. https://doi.org/10.1183/16000617.0250-2021 (2022).
Schlünssen, V. et al. The prevalences and levels of occupational exposure to dusts and/or fibres (silica, asbestos and coal): A systematic review and meta-analysis from the WHO/ILO joint estimates of the work-related burden of disease and injury. Environ. Int. 178, 107980. https://doi.org/10.1016/j.envint.2023.107980 (2023).
China, M. o. H. o. t. P. s. R. o. Standard Methods for Determination of Dust in Workplace Air (GBZ/T 192.2-2007): Part 2—Respirable Dust Concentration. (China Standards Press, 2007).
China, M. o. H. o. t. P. s. R. o. Standard Methods for Determination of Dust in Workplace Air (GBZ/T 192.1-2007): Part 1—Total Dust Concentration. (China Standards Pres, 2007).
Office, I. L. Guidelines for the Use of the ILO International Classification of Radiographs of Pneumoconioses. Revised edition 2022. (International Labour Organization, International Labour Organization, 2022).
Aberle, D. R., Gamsu, G., Ray, C. S. & Feuerstein, I. M. Asbestos-related pleural and parenchymal fibrosis: Detection with high-resolution CT. Radiology 166, 729–734. https://doi.org/10.1148/radiology.166.3.3340770 (1988).
Remy-Jardin, M., Degreef, J. M., Beuscart, R., Voisin, C. & Remy, J. Coal worker’s pneumoconiosis: CT assessment in exposed workers and correlation with radiographic findings. Radiology 177, 363–371. https://doi.org/10.1148/radiology.177.2.2217770 (1990).
Graham, B. L. et al. Standardization of spirometry 2019 update. An official American thoracic society and european respiratory society technical statement. Am. J. Respir. Crit. Care Med. 200, e70–e88. https://doi.org/10.1164/rccm.201908-1590ST (2019).
Quanjer, P. H. et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: The global lung function 2012 equations. Eur. Respir. J. 40, 1324–1343. https://doi.org/10.1183/09031936.00080312 (2012).
China, N. H. C. o. t. P. s. R. o. Diagnosis of occupational pneumoconiosis: Clinical and radiological criteria. (2019).
Wei, F. et al. Characteristics of pneumoconiosis in Zhejiang Province, China from 2006 to 2020: A descriptive study. BMC Public Health 23, 378. https://doi.org/10.1186/s12889-023-15277-8 (2023).
McCarthy, C. P., Bruno, R. M., Rahimi, K., Touyz, R. M. & McEvoy, J. W. What is new and different in the 2024 European society of cardiology guidelines for the management of elevated blood pressure and hypertension?. Hypertension 82, 432–444. https://doi.org/10.1161/hypertensionaha.124.24173 (2025).
Xu, J. et al. Association between the sarcopenia index and abnormal liver function in the adult population in the United States: A cross-sectional study (Lausanne). Front. Med. 10, 1266253. https://doi.org/10.3389/fmed.2023.1266253 (2023).
Baiduc, R. R., Sun, J. W., Berry, C. M., Anderson, M. & Vance, E. A. Relationship of cardiovascular disease risk and hearing loss in a clinical population. Sci. Rep. 13, 1642. https://doi.org/10.1038/s41598-023-28599-9 (2023).
Organization, W. H. Deafness and hearing loss. (2020).
Kuo, P. L., Di, J., Ferrucci, L. & Lin, F. R. Analysis of hearing loss and physical activity among US adults aged 60–69 years. JAMA Netw. Open 4, e215484. https://doi.org/10.1001/jamanetworkopen.2021.5484 (2021).
Szeto, B., Valentini, C. & Lalwani, A. K. Low vitamin D status is associated with hearing loss in the elderly: A cross-sectional study. Am. J. Clin. Nutr. 113, 456–466. https://doi.org/10.1093/ajcn/nqaa310 (2021).
Li, Y. et al. Time trends and future prediction of coal worker’s pneumoconiosis in opencast coal mine in China based on the APC model. BMC Public Health 18, 1010. https://doi.org/10.1186/s12889-018-5937-0 (2018).
Lagiso, Z. A., Mekonnen, W. T., Abaya, S. W., Takele, A. K. & Workneh, H. M. Chronic respiratory symptoms, lung function and associated factors among flour mill factory workers in Hawassa city, southern Ethiopia: “Comparative cross-sectional study”. BMC Public Health 20, 909. https://doi.org/10.1186/s12889-020-08950-9 (2020).
Oo, T. W. et al. Assessment of respiratory dust exposure and lung functions among workers in textile mill (Thamine), Myanmar: A cross-sectional study. BMC Public Health 21, 673. https://doi.org/10.1186/s12889-021-10712-0 (2021).
Perret, J. L. et al. Respiratory surveillance for coal mine dust and artificial stone exposed workers in Australia and New Zealand: A position statement from the thoracic society of Australia and New Zealand. Respirology 25, 1193–1202. https://doi.org/10.1111/resp.13952 (2020).
Gliga, A. R. et al. Short and long-term associations between serum proteins linked to cardiovascular disease and particle exposure among constructions workers. Scand. J. Work Environ. Health 49, 145–154. https://doi.org/10.5271/sjweh.4071 (2023).
Lee, S. et al. Effects of Asian dust-derived particulate matter on ST-elevation myocardial infarction: Retrospective, time series study. BMC Public Health 21, 68. https://doi.org/10.1186/s12889-020-10067-y (2021).
Pollard, K. M. Silica, silicosis, and autoimmunity. Front. Immunol. 7, 97. https://doi.org/10.3389/fimmu.2016.00097 (2016).
Ansari, M. Y. et al. Estimating age and gender from electrocardiogram signals: A comprehensive review of the past decade. Artif. Intell. Med. 146, 102690. https://doi.org/10.1016/j.artmed.2023.102690 (2023).
Du, T. et al. 2017 pediatric hypertension guidelines improve prediction of adult cardiovascular outcomes. Hypertension 73, 1217–1223. https://doi.org/10.1161/hypertensionaha.118.12469 (2019).
Landen, D. D., Wassell, J. T., McWilliams, L. & Patel, A. Coal dust exposure and mortality from ischemic heart disease among a cohort of U.S. coal miners. Am. J. Ind. Med. 54, 727–733. https://doi.org/10.1002/ajim.20986 (2011).
Casey, M. L. et al. Evaluation of high blood pressure and obesity among US coal miners participating in the enhanced coal workers’ health surveillance program. J. Am. Soc. Hypertens. 11, 541–545. https://doi.org/10.1016/j.jash.2017.06.007 (2017).
Kitcher, E. D., Ocansey, G., Abaidoo, B. & Atule, A. Occupational hearing loss of market mill workers in the city of Accra, Ghana. Noise Health 16, 183–188. https://doi.org/10.4103/1463-1741.134919 (2014).
Rathipe, M. & Raphela, S. F. Hearing loss and respiratory health symptoms among large-scale sawmill workers of the timber processing factories within the Gert Sibande District Municipality: A comparative cross-sectional study. BMC Public Health 23, 1196. https://doi.org/10.1186/s12889-023-16086-9 (2023).
Li, Y. et al. Applying machine learning algorithms to explore the impact of combined noise and dust on hearing loss in occupationally exposed populations. Sci. Rep. 15, 9097. https://doi.org/10.1038/s41598-025-93976-5 (2025).
Zhou, B. & Zhang, J. Occupational epidemiological characteristics of noise-induced hearing loss and the impact of combined exposure to noise and dust on workers’ hearing-a retrospective study. Front. Public Health 12, 1488065. https://doi.org/10.3389/fpubh.2024.1488065 (2024).
Chan, K. H., Xiao, D., Zhou, M., Peto, R. & Chen, Z. Tobacco control in China. Lancet Public Health 8, e1006–e1015. https://doi.org/10.1016/s2468-2667(23)00242-6 (2023).
Prevention, C. C. f. D. C. a. Adult Tobacco Survey Report of Fujian Province 2018–2019. (2020).
Acknowledgements
The authors would like to express their gratitude to Fujian Center for Prevention and Control of Occupational Diseases and Chemical Poisoning for providing the surveillance data.
Funding
The study was supported by the Natural Science Foundation of Fujian Province (Grant No. 2021J01722) and the 2019 Minjiang Scholar Start-up Research Fund of Fujian Province.
Author information
Authors and Affiliations
Contributions
M.L. and J.X. designed the study. C.W., Y.J., J.L, and Y.Z. in collected the data. M.L., J.X. and J.L. analysed the data. C.W. and Y.J. contributed to the interpretation of results. M.L., J.X. and J.L. wrote and reviewed the manuscript. All authors discussed the results and commented on the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, M., Wu, C., Zhang, Y. et al. Effects of occupational dust exposure on the health status of workers in China. Sci Rep 15, 19487 (2025). https://doi.org/10.1038/s41598-025-04014-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04014-3