Abstract
This study aimed to evaluate the factors influencing the adoption and application of regenerative endodontic therapy (RET) among endodontists and pediatric dentists across multiple countries, focusing on demographic, professional, and geographic variability.A cross-sectional survey was conducted with 1394 participants from 13 countries. The survey included demographic information, motivational and demotivational factors, and seven clinical scenarios to assess RET application. Odds ratios (OR) and 95% confidence intervals (CI) were calculated for RET adoption using univariate logistic regression. Meta-analysis was performed to account for heterogeneity.The findings revealed significant variability in RET practices. Immature teeth with apical periodontitis and necrotic pulp had the highest odds of RET application (OR = 21.25, 95% CI 16.43–27.49), while mature teeth with necrotic pulp showed significantly lower odds (OR = 0.11, 95% CI 0.09–0.14). Barriers to RET included insufficient training (25.8%), patient disapproval (17.1%), and concerns over unconvincing results (15.9%). Endodontists were more likely to perform RET than pediatric dentists (OR = 2.11 vs. OR = 1.33), and younger practitioners demonstrated higher adoption rates. Countries like Turkey and Yemen exhibited the highest RET application rates, whereas Serbia and Poland reported minimal adoption.Despite the well-documented biological advantages of RET, its broader adoption is hindered by gaps in training, knowledge, and systemic support. Addressing these barriers through targeted educational initiatives and policy integration can enhance the global implementation of RET, optimizing patient outcomes and advancing endodontic practice.
Similar content being viewed by others
Introduction
The concept of regenerative endodontic therapy (RET) involves biologically based therapies aimed at replacing damaged tooth structures and restoring the pulp-dentine complex1 RET primarily seeks to regenerate the pulp–dentine complex damaged by infection, trauma, or developmental anomalies, enabling the formation of a biological seal instead of the mechanical seal achieved with artificial obturating materials. Traditionally, RET has been limited to necrotic immature teeth2 However, it has recently gained significant attention within the scientific community, with numerous studies and guidelines from various specialist organizations advocating its use as the preferred approach for treating non-vital immature permanent teeth3,4,5 In parallel with advancements in tissue engineering, RET indications have expanded in recent years to include mature teeth with apical periodontitis, demonstrating commendable success rates6,7.
The majority of cases in the field of regenerative endodontics, as well as participants in related studies, predominantly involve endodontists8,9,10,11,12 However, given that RET is primarily indicated for immature permanent teeth in young patients, a significant proportion of these patients are managed by paediatric dental specialists. Despite this, the level of knowledge, experience, and clinical adoption of RET among paediatric dentists remains underexplored. Additionally, the differences in the adoption of RET between paediatric dentists and endodontists are not well-documented in the literature.
The first part of this comprehensive research investigated the experience of endodontists and paediatric dentists in performing RET13 The survey, conducted among 1394 participants from 13 different countries, primarily aimed to identify the preferred protocols utilized during RET. Our findings revealed notable discrepancies between the protocols implemented in clinical practice and the established guidelines, highlighting the need for further research and standardization. These results suggest gaps in training or potential misalignment between the training provided and the guidelines set forth by organizations such as the American Association of Endodontists (AAE) and the European Society of Endodontology (ESE). This aligns with recent findings indicating that some surveyed endodontists and paediatric dentists acknowledged lacking sound knowledge of regenerative endodontics14,15,16,17,18.
This study builds upon our previous multinational survey that examined general attitudes and protocol preferences in RET among pediatric dentists and endodontists. While the earlier work provided a broad overview, it did not investigate the contextual and clinical decision-making processes underlying RET applications. Addressing this gap, the current study aims to identify the specific factors that influence practitioners’ choices in various clinical scenarios. By presenting seven distinct cases and analyzing demographic and motivational patterns, this research offers a more nuanced understanding of how RET is applied across different age groups and tooth types, highlighting the need to align clinical practice with evidence-based guidelines.
Methods
Study design
Under the leadership of the principal investigator (F.P.H.), this multicenter study was conducted between January and March 2022 across three continents: Europe, Asia, and Africa. Researchers from 21 countries were identified based on their professional interests listed on ResearchGate and invited to participate via email. Of these, 13 agreed to participate and contributed data. The remaining 8 either did not respond, declined participation, or encountered local regulatory barriers that prevented their involvement. Therefore, the final sample was shaped by voluntary participation and feasibility rather than predefined geographic criteria, with one researcher ultimately representing each of the 13 participating countries.
Before initiating the study, ethical approval was obtained from the Nigde Ömer Halisdemir University Ethics Committee in Turkey (Approval No: 2021/118). Additionally, participating researchers secured ethical approvals in their respective countries, as required. Notable approvals included those from Mahsa University Ethics Committee in Malaysia (RMC/EC01/2022), University of Novi Sad Ethics Committee in Serbia (01-39/167/1), University of Zagreb Ethics Committee in Croatia (05-PA-30-IV-1/2022), and University of Coimbra Ethics Committee in Portugal (CE-086/2022). All methods were performed in accordance with the relevant guidelines and regulations, as outlined in the Declaration of Helsinki and the institutional ethical standards.
The questionnaire, finalized in English, consisted of 14 questions and was developed in January 2022 using an online survey platform (Google Forms; https://www.google.com/intl/tr_tr/forms/about/). The questions were organized into four distinct sections, each designed to gather specific information from the participants. Only respondents who indicated prior experience with performing RET proceeded to complete the entire survey (n = 792, 57% of total respondents). For the detailed survey content, please refer to Table 1. The first Sect. (4 questions) focused on collecting demographic information, including participants’ age, gender, specialization, and country of practice. The second Sect. (2 questions) investigated both the motivational and demotivational factors influencing participants’ preferences for RET as a treatment modality. The third Sect. (7 questions) presented a series of clinical scenarios, specifically designed to evaluate the practical application of RET in various clinical contexts. The final question asked participants where they received their initial training in RET. All questions were closed-ended and structured to allow for quantitative analysis; no open-ended or qualitative questions were included in the survey. This approach was chosen to standardize responses across a large multinational sample and to enable robust statistical comparisons.
Prior to distribution, the reliability of the questionnaire was evaluated using the test-retest reliability method. A group of 20 participants (10 endodontists and 10 paediatric dentists) completed the questionnaire twice, with a 15-day interval between responses. Reliability, assessed through Kappa statistics, demonstrated almost perfect agreement (k = 0.8), confirming the consistency and dependability of the survey instrument.
The study included endodontists, paediatric dentists, academicians, and graduates currently enrolled in specialization programs in endodontics or paediatric dentistry. Participation was voluntary, and anonymity was strictly maintained to ensure confidentiality. A survey link was created, and access to the data was restricted solely to the principal investigator (F.P.H.). The survey link was disseminated through various channels, including dental associations, national endodontist and paediatric dentistry societies, professional web pages, email lists, and social media platforms. To enhance the response rate, each researcher sent at least two reminder emails, spaced 2 weeks apart. The final response was recorded on March 20, 2022.
Given the extensive scope of the study, a sample size calculation was not feasible; hence, a convenience sampling method was employed due to the wide geographical distribution of the target population and the exploratory nature of the study. Given the logistical challenges associated with probabilistic sampling across multiple countries and the lack of a unified registry of pediatric dentists and endodontists, this approach enabled timely and practical data collection. Convenience sampling is commonly used in international cross-sectional surveys involving healthcare professionals, as it allows researchers to reach a diverse range of respondents who are actively engaged in clinical practice. While this method limits the ability to generalize findings to the broader population, it remains an effective strategy for capturing real-world insights and identifying emerging trends in clinical decision-making.
Statistical analysis
Statistical analyses were conducted using Jamovi software and Review Manager 5.4. Descriptive statistics, including frequencies and percentages, were utilized to summarize participant demographics and responses. Comparative analyses were performed using chi-squared tests, and Cramer’s V values were calculated to assess the strength of associations between categorical variables. For the meta-analysis, conducted in Review Manager 5.4, heterogeneity among studies was evaluated using the I2 statistic. In the presence of significant heterogeneity, a random-effects model was applied to account for variability across studies. Additionally, univariate logistic regression analysis was performed to calculate odds ratios (OR) and 95% confidence intervals (CI) for individual predictors. A p-value of 0.05 was set as the threshold for statistical significance.
Results
Demographic characteristics of the participants are summarized in Table 2. A total of 1394 respondents participated in the study, comprising 41% males (n = 571) and 59% females (n = 823). The majority of participants were aged between 20 and 34 years (47.5%), followed by 35–44 years (36.4%), 45–54 years (10.9%), and over 55 years (5.2%). Regarding specialization, 61.2% of the respondents were endodontists (n = 853), while 38.8% were pediatric dentists (n = 541). Representation across countries varied, with the highest number of participants from Turkey (n = 183), followed by Yemen (n = 143), Egypt (n = 145), and other countries from Europe, Asia, and Africa.
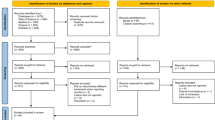
The analysis highlights considerable variability in RET adoption among countries. Yemen (OR = 15.45, 95% CI 8.68–27.50) and Turkey (OR = 11.27, 95% CI 6.92–18.35) exhibit significantly higher odds of performing RET compared to Poland (OR = 0.04, 95% CI 0.02–0.06) and Serbia (OR = 0.00, 95% CI 0.00–0.01), which show the lowest odds. The heterogeneity across studies is substantial, as indicated by an I2 value of 97% (p < 0.00001). A random-effects model was applied to account for this variability, and the overall odds ratio for RET adoption was calculated as 1.38 (95% CI 0.52–3.69), though this was not statistically significant (p = 0.52). These findings underscore the influence of country-specific factors on RET adoption (Fig. 1).
Gender analysis shows that male participants were more likely to perform RET (OR = 2.55, 95% CI 2.01–3.23) compared to females (OR = 1.37, 95% CI 1.13–1.67). Age analysis indicates that the 35–44 age group had the highest likelihood of performing RET (OR = 3.05, 95% CI 2.36–3.94), while those aged 55 years and above had the lowest odds (OR = 0.22, 95% CI 0.11–0.44). Among specializations, endodontists showed higher odds of performing RET (OR = 2.11, 95% CI 1.74–2.55) compared to pediatric dentists (OR = 1.33, 95% CI 1.05–1.70). Finally, workplace analysis reveals that practitioners in universities had the highest odds of performing RET (OR = 2.31, 95% CI 1.83–2.91), followed by those in private practice (OR = 1.56, 95% CI 1.24–1.97), while those in public health centers had the lowest odds (OR = 1.19, 95% CI 0.83–1.72) (Fig. 2).
Figure 3 presents the OR and 95% CI for performing RET across seven different clinical scenarios. Case 2, which describes an immature tooth with acute symptoms (pain, swelling, etc.) and a necrotic pulp with a periapical lesion, demonstrated the highest odds of RET performance (OR = 21.25, 95% CI 16.43–27.49). In contrast, Case 3, representing a mature tooth with necrotic pulp and periapical lesion, exhibited significantly lower odds (OR = 0.11, 95% CI 0.09–0.14). Similarly, scenarios involving mature teeth (Case 4) or teeth with severe root resorption (Case 5 and Case 6) also showed low odds of RET being performed (OR = 0.05 for both, 95% CI 0.04–0.07). Case 1, involving an immature tooth with necrotic pulp and periapical lesion, had a moderate likelihood of RET performance (OR = 2.78, 95% CI 2.27–3.40).
Endodontists exhibited higher RET application rates compared to pediatric dentists in most cases, particularly in straightforward scenarios such as Case 1 (63.4% vs. 62.2%, p = 0.734) and Case 2 (83.9% vs. 80.2%, p = 0.187). However, the difference became more pronounced in complex cases such as Case 3, where endodontists had a significantly higher application rate than pediatric dentists (29.5% vs. 17.0%, p < 0.001). When analyzed by experience, PhD holders and those with more than 21 years of clinical experience demonstrated lower RET application rates in challenging cases (e.g., Case 3), suggesting a potential hesitancy toward adopting RET in complex scenarios. In contrast, younger practitioners (0–5 years of experience) showed relatively higher application rates, especially in cases like Case 6 (31.1%, p = 0.068). Workplace analysis revealed that university-based practitioners had the highest overall application rates, followed by those in private practices and public health centers. Geographic analysis indicated significant variability across countries, with some nations, such as Portugal and Egypt, reporting notably higher application rates in most cases compared to Poland and Saudi Arabia (Table 3).
Across all participants, the most commonly cited reason for performing RET was its high success rate due to biological benefits (57.6%), followed by ease of performance (24%) and patient demand (10.3%). Motivational factors showed variation by specialization and country. Endodontists more frequently cited biological success, while pediatric dentists were more influenced by ease of application and patient requests. Country-based differences were also evident, with some nations emphasizing biological success (e.g., Portugal, the Netherlands), and others prioritizing ease of performance (e.g., Poland, Malaysia). These differences were statistically significant (p < 0.001) and are detailed in Table 4.
The most frequently reported barriers to RET use were lack of clinical experience or knowledge (25.8%), patient disapproval (17.1%), and concerns about outcome predictability (15.9%). Other concerns included insufficient equipment, treatment complexity, and multi-session demands. Specialization and country-based patterns were again observed—for instance, pediatric dentists more commonly reported patient disapproval, whereas endodontists cited material shortages. Country-specific trends, including Poland’s high rate of reported knowledge gaps, are summarized in Table 5 (p < 0.001).
Figure 4 illustrates a network graph of factorial correlations using Cramer’s V, highlighting the strength of associations among various factors influencing RET. Strong associations (Cramer’s V > 0.15) were observed between country and RET performing status (Cramer’s V = 0.455), indicating that geographic location significantly impacts the likelihood of performing RET. Similarly, moderate associations (0.10 < Cramer’s V ≤ 0.15) were found between specialization and motivating factors (Cramer’s V = 0.167), as well as between specialization and demotivating factors (Cramer’s V = 0.128), suggesting that professional background influences these aspects. Weaker correlations (0.05 < Cramer’s V ≤ 0.10) were noted between RET performing status and factors such as age and gender, indicating a more limited impact of demographic variables. Interestingly, workplace showed minimal correlation with other variables, reflecting its limited role in influencing RET decisions.
The majority of participants (44%) received their first training on RET during their PhD or MSc programs, reflecting the importance of formal education in fostering knowledge and skills in RET. However, a concerning 18.6% of respondents reported never having received any training on RET, with this percentage being notably higher among pediatric dentists (20.5%) and practitioners with over 20 years of experience (28.6%). Countries with the highest rates of RET application, such as Turkey and Jordan, also exhibited the most robust training infrastructures, with a significant proportion of participants receiving RET training during doctoral or specialization programs. In contrast, Serbia, which showed the lowest RET application rate, also reported a striking lack of RET-focused training (88% of participants never received training) (Table 6).
Discussion
This study provides comprehensive insights into the factors influencing the adoption and application of RET among endodontists and pediatric dentists across multiple countries. Our findings reveal substantial variability in RET practices, driven by demographic, professional, and geographic factors. While high success rates and biological benefits were key motivating factors, barriers such as insufficient knowledge, lack of clinical experience, and concerns over unconvincing results were commonly reported. These results underscore the need for targeted educational initiatives and resource allocation to address existing gaps and align clinical practices with established guidelines. Furthermore, the variability observed in RET adoption across different clinical scenarios and demographic groups highlights the complexity of decision-making processes in contemporary endodontic practice.
The variability in RET adoption across countries, as demonstrated in this study, reflects the complex interplay of factors such as training, clinical experience, healthcare infrastructure, and cultural attitudes. Countries like Yemen and Turkey, which exhibited the highest odds of performing RET (OR = 15.45 and OR = 11.27, respectively), also reported the highest rates of RET training in doctoral and specialization programs. This suggests a strong correlation between formal education and the adoption of RET in clinical practice. Conversely, in countries such as Serbia and Poland, where RET adoption was minimal (OR = 0.00 and OR = 0.04, respectively), the lack of RET training in curricula, insufficient resources, and limited knowledge emerged as significant barriers. For instance, in Serbia, 93.3% of respondents cited a lack of training as the primary reason for not performing RET, consistent with the absence of RET-focused content in the country’s PhD and MSc programs. Language barriers further exacerbate this issue, as clinicians may struggle to access and interpret international guidelines from organizations such as the AAE, ESE, and EAPD13.
While a substantial proportion of participants reported receiving their initial RET training during MSc or PhD programs, the survey did not collect detailed information on the specific content, duration, or standardization of this education. Therefore, it remains unclear whether such training followed a structured curriculum based on international guidelines. This variability may partially explain the discrepancies observed in RET practices among similarly qualified participants. Future studies should explore not only the presence but also the quality and comprehensiveness of RET training across postgraduate programs, to better assess its impact on clinical application.
In addition to educational and linguistic factors, systemic and cultural differences may also contribute to the observed variability. For example, access to advanced materials and newer procedures like RET is often more limited in public health settings compared to private practices, particularly in lower-resource countries. Furthermore, clinician attitudes toward biologically based techniques and patient openness to innovative treatment options may vary across regions, influencing the perceived feasibility and desirability of RET. In some countries, conventional root canal therapy may still be considered the standard of care, while others show a stronger cultural inclination toward tissue preservation and regenerative concepts.
Endodontists were significantly more likely to perform RET compared to pediatric dentists (OR = 2.11 vs. OR = 1.33), which can be attributed to their specialized training and focus on endodontic procedures. Pediatric dentists, despite encountering more suitable cases in younger patients, demonstrated lower application rates (53.7%), likely due to challenges associated with younger patients, such as extended treatment sessions and the need for cooperation. These results are consistent with previous studies9,19 indicating that pediatric dentists often consider RET less practical in their patient population, favoring alternative treatments or referrals to specialized centers.
Demographic factors also played a role, with male practitioners demonstrating higher odds of performing RET than females, possibly reflecting differences in clinical confidence or access to advanced training. Age emerged as another critical factor, with younger practitioners (35–44 years) showing the highest adoption rates, likely due to the inclusion of RET training in modern postgraduate curricula. Conversely, specialists with over 50 years of experience were less likely to perform RET, as this technique was not commonly included in doctoral programs during their education. These trends align with previous studies20,21 reporting that most practitioners performing RET received their training during postgraduate programs, while nearly 18.6% of respondents never received any formal RET training. Workplace settings also played a significant role; university-affiliated practitioners had the highest odds of performing RET, reflecting better access to resources and evidence-based guidelines. This is consistent with findings from Tong et al.19, which emphasize the importance of university environments in fostering the adoption of advanced techniques like RET. Addressing these disparities through targeted educational initiatives, including integration of RET into undergraduate and postgraduate curricula, is essential for improving clinical confidence and ensuring equitable adoption of RET across all practitioner groups.
In our study, significant differences in RET application rates were observed depending on the case scenarios, reflecting the role of clinical judgment and knowledge gaps. In all countries except for Poland, respondents preferred applying RET to immature teeth with apical periodontitis and pulp necrosis over other case scenarios, aligning with current recommendations for RET3,4. However, when acute symptoms accompanied these cases, a 21.9% decrease in RET application rate was observed. This decline is noteworthy, as the presence of acute symptoms in an immature tooth with pulp necrosis does not constitute a contraindication for RET22 and has even been reported as a positive prognostic factor in recent studies23. Such findings highlight potential knowledge gaps among clinicians regarding appropriate case selection or an inclination toward more conventional treatments due to a sense of familiarity.
Responses regarding the application of RET in mature teeth revealed significant ambiguity among participants. While 41.2% of respondents favored RET over RCT, a considerable 33% expressed uncertainty about its appropriateness in such cases. Notably, only 24.9% reported applying RET to mature teeth with periapical lesions and necrotic pulp, and an even smaller proportion (17.4%) utilized RET in retreatment cases of mature teeth. This hesitancy may stem from the perception that RET offers limited advantages for mature teeth, particularly when thick dentinal walls provide adequate fracture resistance, diminishing the biological benefits associated with the procedure2,6,7,22,24.
Interestingly, the reluctance observed among participants to apply RET in mature teeth appears discordant with the growing body of evidence supporting its efficacy. While recent meta-analyses10,11,12 report high success rates for RET in mature permanent teeth—ranging from 95 to 96%—only about one in four respondents indicated using RET in such cases, and an even smaller percentage did so in retreatment scenarios. In particular, the systematic review by Li et al.12 found no significant difference in success or symptom-free rates between immature and mature necrotic permanent teeth treated with RET. Moreover, positive vitality responses were significantly more common in mature teeth, challenging the traditional assumption that immature teeth are the only viable candidates for RET. Several factors may explain this discrepancy. First, the perception of RET as a technique primarily suited for immature teeth may persist in clinical education and practice. Second, the lack of standardized protocols and long-term outcome data may contribute to clinicians’ hesitancy, particularly in private or public non-academic settings. Additionally, variations in access to materials, training quality, and regulatory guidance across countries may influence the level of confidence in RET adoption. These findings underscore the importance of bridging the gap between emerging evidence and clinical implementation through clearer guidelines, hands-on training, and long-term outcome dissemination.
To better understand the case selection criteria for RET, our survey included scenarios involving complications such as horizontal root fractures and root resorptions. More than 70% of respondents would not apply RET in these cases, despite evidence suggesting that RET can promote hard tissue healing in such conditions24,25,26. This reluctance may stem from the limited and low-quality evidence currently available for RET in complex cases, leading clinicians to favor treatments with more predictable outcomes. Addressing these gaps through robust clinical trials and targeted educational initiatives is essential to expand the adoption of RET in a wider range of clinical scenarios.
The success of RET is assessed through a hierarchy of goals: primary goals include symptom resolution and evidence of bone healing; secondary goals focus on increasing root wall thickness and root length, which are desirable for long-term outcomes; and tertiary goals involve positive vitality testing, which would confirm the organization of functional pulp tissue. While achieving all these objectives simultaneously remains challenging, symptom relief and apical healing alone have reported success rates between 91% and 94%27,28. Despite these promising outcomes, “results are not reassuring” were ranked as the second and third most common reasons cited by pediatric dentists and endodontists, respectively, for not performing RET. This highlights potential knowledge gaps or skill deficiencies among practitioners, particularly regarding the evidence base supporting RET’s effectiveness.
It is crucial for scientifically validated biological treatments like RET to be better integrated into healthcare systems and adequately supported by insurance providers. Respondents who had performed RET overwhelmingly cited its high success rates and biological advantages as primary motivators. These advantages are especially relevant for immature permanent teeth, where RET facilitates the thickening of dentin walls, continued root development, and hard tissue deposition, offering superior outcomes compared to apexification29. Furthermore, RET is a cost-effective and straightforward procedure, utilizing tools and medicaments readily available in most dental offices, thereby enhancing its feasibility in diverse clinical settings.
While this study provides comprehensive insights into the factors influencing the adoption and application of RET, several limitations must be acknowledged. First, the cross-sectional design of the survey limits the ability to establish causal relationships between the observed trends and specific factors influencing RET adoption. Additionally, reliance on self-reported data introduces the potential for recall bias, as participants may not accurately remember or report their clinical practices and experiences. The study’s multinational nature, while a strength in terms of generalizability, also presents challenges. Differences in healthcare systems, cultural attitudes, and educational standards across the participating countries may have influenced the responses, potentially introducing heterogeneity that could not be fully accounted for in the analysis.
Another limitation lies in the sampling approach. The use of convenience sampling, while practical and often necessary in multinational healthcare surveys, inherently limits the representativeness of the sample. This method relies on voluntary participation, which may attract respondents who are more interested in regenerative endodontics or more engaged in academic or professional networks. Consequently, the perspectives of clinicians who are less familiar with or less supportive of RET may be underrepresented. This introduces a potential selection bias that could influence the observed trends in RET adoption. Although a minimal correlation between workplace setting and RET performance was found, university-affiliated clinicians—who typically have greater access to training opportunities and up-to-date guidelines—may still have been overrepresented in the sample. This overrepresentation could have contributed to an upward bias in reported RET adoption rates, potentially overstating the level of real-world implementation, particularly in public or private non-academic settings. Moreover, since the sampling was not probabilistic, the generalizability of the results to the broader populations of endodontists and pediatric dentists remains limited. While this approach enabled the collection of valuable, real-world data from a diverse and geographically widespread sample, future studies should consider incorporating stratified or randomized sampling methods where feasible, to enhance the robustness and external validity of the findings.
Additionally, while the study identified when participants first received RET training (e.g., during MSc or PhD programs), it did not assess the structure, standardization, or content of that training. This limits our ability to determine whether differences in RET adoption are attributable to variations in training quality. Given that postgraduate curricula may differ widely across institutions and countries, future studies should investigate not only whether training was received but also the comprehensiveness and guideline-alignment of such educational experiences. Moreover, the observed variability in RET application across different clinical scenarios—particularly in complex cases—may also reflect inconsistencies in how RET is taught or emphasized during training. The absence of standardized clinical decision-making frameworks in education could contribute to divergent approaches among similarly qualified professionals.
While our findings suggest notably low RET adoption and limited training in countries such as Serbia and Poland, these results should be interpreted with caution. They reflect the responses of a limited number of participants and may not fully capture the broader national context. Cultural factors, differences in postgraduate curricula, availability of RET-related materials, and healthcare system structures likely play significant roles in shaping these patterns. Further country-specific research would be needed to draw more definitive conclusions.
Furthermore, the study did not include any open-ended or qualitative survey components. This was a deliberate methodological choice to ensure consistency in responses across a large multinational sample and to facilitate statistical analysis. However, the absence of qualitative input limits the ability to capture more nuanced practitioner perspectives, particularly regarding motivations, challenges, and contextual factors influencing RET adoption. Future studies may benefit from incorporating mixed-method approaches to enrich interpretation.
This study offers several notable strengths that enhance its contribution to the understanding of RET practices. Foremost, its multinational design provides a broad perspective on RET adoption, capturing diverse clinical experiences and practices across countries with varying healthcare systems and educational standards. This comprehensive scope enhances the generalizability of the findings, making them applicable to a wide range of contexts. A significant strength of the study is its focus on both endodontists and pediatric dentists, two key professional groups involved in RET. By exploring the differences and similarities in their approaches, the study highlights unique insights into how specialization and clinical experience influence decision-making in RET application. This dual focus enables a nuanced understanding of the barriers and motivators specific to each group.
The inclusion of detailed clinical scenarios as part of the survey represents another strength. By evaluating responses to seven distinct cases, the study provides a practical lens through which to assess real-world application of RET principles. This approach moves beyond theoretical knowledge, offering insights into how clinicians apply RET in diverse and challenging cases. The incorporation of meta-analytic elements to quantify heterogeneity and evaluate trends across countries also strengthens the analytical depth of the research. By addressing key clinical and systemic questions, this study lays a strong foundation for advancing RET education and practice globally. Its multifaceted design and thorough analysis provide a robust framework for future research and clinical guideline development.
These findings also align with the World Health Organization’s 2030 goals for oral health, which emphasize reducing inequalities in access to care, strengthening the oral health workforce, and promoting evidence-based, person-centered approaches. By identifying the key clinical, educational, and systemic barriers to RET adoption across different countries, this study contributes to global efforts to advance equitable, biologically based dental care. The results may inform future policy development, curriculum reforms, and clinical guideline integration in line with international oral health objectives.
Based on the findings of this study, we propose several practical strategies to enhance the global adoption of RET. First, standardizing RET education across postgraduate and, where applicable, undergraduate curricula may help bridge existing knowledge gaps. Second, national dental associations should consider integrating RET protocols into official clinical guidelines and supporting translations of key documents into local languages. Third, increasing institutional investment in RET-related materials—particularly in public healthcare settings—would improve accessibility and support implementation. Lastly, further high-quality clinical trials and continuing education initiatives are needed to build clinician confidence, particularly in complex cases.
Conclusion
This multinational study underscores the complexities in the adoption and application of RET among endodontists and pediatric dentists, revealing significant variability influenced by demographic, professional, and geographic factors. While RET is widely recognized for its biological advantages and high success rates in immature permanent teeth, barriers such as insufficient training, knowledge gaps, and systemic limitations hinder its broader adoption, particularly for mature teeth and complex cases. The study’s strengths include its comprehensive scope, detailed clinical scenarios, and dual focus on two key professional groups, providing valuable insights into the motivations and challenges in RET practice. However, limitations such as reliance on self-reported data, cross-sectional design, and potential heterogeneity across countries highlight the need for cautious interpretation. To promote global adoption of RET, future efforts should focus on addressing evidence gaps, enhancing training programs, and integrating RET into healthcare systems, enabling it to fulfill its potential as a transformative approach in endodontics.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available considering that we have not required consents to publish this data, but are available from the corresponding author on reasonable request.
References
Murray, P. E., Garcia-Godoy, F. & Hargreaves, K. M. Regenerative endodontics: A review of current status and a call for action. J. Endod.. 33, 377–390 (2007).
He, L. et al. Regenerative endodontics for adult patients. J. Endod. 43, S57–S64 (2017).
American Association of Endodontics. American Association of Endodontics clinical considerations for a regenerative procedure. (2016). Available from: http://www.aae.org/uploadedfiles/publications_and_research/research/currentregenerativeend
Galler, K. et al. European society of endodontology position statement: Revitalization procedures. Int. Endod. J. 49, 717–723 (2016).
Duggal, M. et al. Interventions for the endodontic management of non-vital traumatised immature permanent anterior teeth in children and adolescents: A systematic review. Eur. Arch. Paediatr. Dent. 18, 139–151 (2017).
Paryani, K. & Kim, S. G. Regenerative endodontic treatment of permanent teeth after completion of root development: A report of 2 cases. J. Endod. 39, 929–934 (2013).
Glynis, A. et al. Regenerative endodontic procedures for the treatment of necrotic mature teeth with apical periodontitis: A systematic review and meta-analysis. J. Endod. 47, 873–882 (2021).
Bezgin, T. & Sönmez, H. Review of current concepts of revascularization/revitalization. Dent. Traumatol. 31, 267–273 (2015).
Lee, J. Y. et al. Regenerative endodontic procedures among endodontists: A web-based survey. J. Endod.. 44, 250–255 (2018).
Scelza, P. et al. Prognosis of regenerative endodontic procedures in mature teeth: A systematic review and meta-analysis. Materials 14, 4418 (2021).
Nangia, D. et al. Treatment outcome of regenerative endodontic procedures in mature permanent teeth compared to nonsurgical endodontic treatment: A systematic review and meta-analysis. J. Conserv. Dent. 24, 530–538 (2021).
Li, J. et al. Treatment outcome of regenerative endodontic procedures for necrotic immature and mature permanent teeth: A systematic review and meta-analysis. Oral Health Prev. Dent. 21, b4100877 (2023).
Hatipoğlu, F. P. et al. Attitude and practice of regenerative endodontic procedures among endodontists and paediatric dentists: A multinational survey. Int. J. Paediatr. Dent. 33, 521–534 (2023).
Mayya, A. et al. Knowledge, attitude, and perception among endodontists toward regenerative endodontics: A cross-sectional survey. J. Int. Soc. Prev. Community Dent. 11, 68 (2021).
Burns, L. E. et al. Clinician decision-making for the endodontic treatment of immature permanent teeth: A National survey. Int. J. Paediatr. Dent. (2025). Epub ahead of print.
Anna, B. et al. Current trends in regenerative endodontics: A web-based survey. J. Endod. 50, 181–188 (2024).
Alrayes, M. H. et al. Regenerative endodontics in Saudi Arabia: A review of knowledge-based surveys. Saudi Endod. J. 15, 101–111 (2025).
Botero, T. et al. Web-based survey on regenerative endodontic practices among members of the American association of endodontists. J. Endod. 50, 1281–1288 (2024).
Tong, H. et al. Regenerative endodontic therapy for managing immature non-vital teeth: Experiences and opinions of paediatric dental practitioners. Eur. Arch. Paediatr. Dent. 22, 145–155 (2021).
Chakravarthy, D. et al. Knowledge and attitude levels on regenerative endodontic procedures among dental residents in puducherry. J. Sci. Dent. 11, 44–47 (2021).
Mayya, A. et al. Knowledge, attitude, and perception among endodontists: A cross-sectional survey. J. Int. Soc. Prev. Commun. Dent. 11, 68–76 (2021).
Nageh, M. et al. Assessment of regaining pulp sensibility in mature necrotic teeth using a modified revascularization technique with platelet-rich fibrin: A clinical study. J. Endod. 44, 1526–1533 (2018).
Chrepa, V. et al. Clinical outcomes of immature teeth treated with regenerative endodontic procedures—A San Antonio study. J. Endod. 46, 1074–1084 (2020).
Saoud, T. M. A. et al. Regenerative endodontic procedures for traumatized teeth: A review of three cases. J. Endod. 42, 1476–1482 (2016).
Lu, J. & Kahler, B. Regenerative endodontic procedures for two traumatized mature anterior teeth with root fractures. BMC Oral Health 22, 1–7 (2022).
Kaval, M., Güneri, P. & Çalışkan, M. Regenerative endodontic treatment of perforated internal root resorption: A case report. Int. Endod. J. 51, 128–137 (2018).
Tong, H. J. et al. Regenerative endodontic therapy in nonvital immature permanent teeth: A systematic review and meta-analysis. J. Endod. 43, 1453–1464 (2017).
Torabinejad, M. et al. Regenerative endodontic treatment or MTA apical plug in necrotic teeth: A systematic review and meta-analysis. J. Endod. 43, 1806–1820 (2017).
Jeeruphan, T. et al. Comparison of radiographic and survival outcomes of immature teeth treated with regenerative endodontic or apexification methods. J. Endod. 38, 1330–1336 (2012).
Author information
Authors and Affiliations
Contributions
F.P.H. designed the study. Ö.H. performed the data analysis and revised the manuscript. The manuscript was written by F.P.H. J.F.B.M., N.T., and P.J.P revised the final draft. All other authors contributed to data collection. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Ethical approval was obtained from the Nigde Ömer Halisdemir University Ethics Committee in Turkey (Approval No: 2021/118). Additionally, participating researchers secured ethical approvals in their respective countries, as required. Notable approvals included those from Mahsa University Ethics Committee in Malaysia (RMC/EC01/2022), University of Novi Sad Ethics Committee in Serbia (01-39/167/1), University of Zagreb Ethics Committee in Croatia (05-PA-30-IV-1/2022), and University of Coimbra Ethics Committee in Portugal (CE-086/2022). All methods were performed in accordance with the relevant guidelines and regulations, as outlined in the Declaration of Helsinki and the institutional ethical standards.
Consent for publication
All participants provided informed consent by voluntarily agreeing to participate in the online survey after being informed about the purpose of the study. Participants were assured that their responses would be kept confidential and used solely for research purposes. Written informed consent was obtained from the participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pertek Hatipoğlu, F., Hatipoğlu, Ö., Taha, N. et al. Determinants of regenerative endodontic therapy use among pediatric and endodontic specialists in 13 countries. Sci Rep 15, 19493 (2025). https://doi.org/10.1038/s41598-025-04060-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-04060-x