Abstract
To investigate the expression of KRT80 in non-small cell lung cancer (NSCLC) patients and its relationship with clinicopathological factors, prognosis, as well as the differences in KRT80 expression between Xuanwei area and Non-xuanwei area, lung adenocarcinoma and lung squamous cell carcinoma. Based on 178 clinical cases, immunohistochemical methods combined with public databases were used to examine the expression of KRT80 in NSCLC patients and analyze its correlation with various clinicopathological factors and prognosis. The study confirmed the up-regulation of KRT80 expression in NSCLC cancer tissues. Significant regional specific and histological subtype differences in KRT80 expression were revealed. Although the expression level of KRT80 has no direct significant correlation with the prognosis of NSCLC patients, it has a good ability to distinguish cancerous tissue from paracancer tissue. KRT80 can be used as a diagnostic biomarker for NSCLC patients, but its specific mechanism and clinical application value still need to be further explored.
Similar content being viewed by others
Introduction
Global Cancer Statistics 2022 showed that lung cancer is not only the most common type of cancer worldwide, accounting for 12.4% of all cancer cases, but also the leading cause of cancer deaths, accounting for 18.7% of cancer-related deaths worldwide1. Non-small cell lung cancer (NSCLC) is the most common type of lung cancer, accounting for approximately 85% of all lung cancer cases with a survival rate of less than 15%, with lung adenocarcinoma (LUAD) and lung squamous cell carcinoma (LUSC) being the most common NSCLC subtypes2. Lung squamous cell carcinoma tends to occur in men and is strongly associated with smoking, while LUAD usually occurs in women who do not smoke3. Remarkably, the Xuanwei region of China’s Yunnan Province has one of the highest rates of lung cancer in the world and often exhibits familial clustering4. Xuanwei Lung cancer (XWLC) refers to a lung cancer in Xuanwei City and Fuyuan County, Yunnan Province, China, with high morbidity and mortality due to the extensive use of local bituminous coal, characterized by a younger age of onset, significant gender differences, and a mortality rate much higher than the national average5. Lung cancer in this region is dominated by adenocarcinoma, and the risk is higher among female residents6. Studies have shown that the high incidence of lung cancer is not significantly related to gender or smoking habits, but is mainly closely related to the behavior of burning bituminous coal in the family7. While immunotherapy and targeted therapy have significantly improved the efficacy of NSCLC treatment over the past 20 years, the majority of NSCLC patients develop resistance to targeted drugs and disease progression at advanced stages8. Therefore, the search for new diagnostic and prognostic biomarkers for NSCLC remains critical.
Keratin, also known as cytokeratin, is an intermediate filament (IF) forming protein of epithelial cells and is expressed in both normal and malignant epithelial cells9. These small molecular weight structural proteins (molecular weight from 40 to 76 kDa) are able to interact with a variety of regulatory proteins to initiate a signaling cascade10. As a typical marker of epithelial cells, keratin is widely expressed in a variety of cancers and plays an important role in regulating cell migration, invasion and epithelial-mesenchymal transition (EMT)11. The Keratin 80 (KRT80) gene, located on chromosome 12q13, encodes a protein of 452 amino acids that promotes the formation of intermediate filaments (IF) heterodimers, structurally closer to type II hair keratin12. KRT80 is overexpressed in a variety of tumors and can effectively enhance the proliferation, invasiveness and migration of cancer cells, which is closely related to poor prognosis of cancer patients13.
In this study, the expression of KRT80 in NSCLC was investigated by immunohistochemistry, and its correlation with clinicopathological features and prognosis were analyzed. We also paid special attention to the differences in the expression of KRT80 in different geographical regions (Xuanwei and Non-xuanwei region) and different histological subtypes (LUAD and LUSC). The study results revealed that the expression level of KRT80 in NSCLC patients in Xuanwei area was significantly higher than that in Non-xuanwei area, and the expression level in lung adenocarcinoma was significantly higher than that in lung squamous cell carcinoma. In addition, the expression of KRT80 may have a certain correlation with the clinicopathological features such as lymph node metastasis and tumor size in NSCLC patients, but this relationship still needs further study to clarify. Although the association between KRT80 and patient outcomes is not significant, its potential as a diagnostic biomarker for NSCLC is of concern. The findings of this study not only provide preliminary evidence for the potential of KRT80 as a biomarker for NSCLC, but also reveal differences in its expression across geographic regions and lung cancer subtypes, providing new directions for future research. Future studies can further explore the molecular mechanism of KRT80 in NSCLC and its interaction with the tumor immune microenvironment, in order to provide a new perspective for the diagnosis and treatment of NSCLC.
Materials and methods
The online database
To assess the expression of KRT80 in NSCLC, our comprehensive database from the Gene Expression Omnibus (GEO, https://www.ncbi.nlm.nih.gov/gds/?term) website has been extracted using Affymetrix HG - U133_Plus_2 chip data. The GSE19188 dataset, which contained genome-wide gene expression analyses from 91 NSCLC and 65 normal lung tissues, was incorporated into the analysis14. In addition, we incorporated the GSE75037 dataset, which used Illumina WG6-V3 expression chips to analyze gene expression profiles in 83 lung adenocarcinomas and 83 matched adjacent non-malignant lung tissues, to analyze the expression of KRT80 in NSCLC15. To further validate and complement our findings, we utilized the GEPIA2 database and Kaplan-Meier (K-M) plotter database to analyze the potential impact of KRT80 mRNA expression on NSCLC. GEPIA2 is an online database (http://gepia2.cancer-pku.cn/#index) that integrates TCGA RNA-seq expression and clinical data for survival analysis of selected genes16. Through the expression analysis and survival analysis of KRT80 in the GEPIA2 database, we further explored the role of KRT80 in NSCLC and further explained the association between KRT80 and patient prognosis. Kaplan-Meier (K-M) plotter database (https://kmplot.com) includes gene expression data from databases such as the Gene Expression Omnibus (GEO), the European Genome Genome Archive (EGA), and the Cancer Genome Atlas (TCGA)17. It allows us to assess the correlation between specific gene expression levels and patient survival time by analyzing data from a large number of patients. Using this database, we were capable of exploring the potential association between KRT80 mRNA expression levels and survival in patients with NSCLC, providing us with an important tool to evaluate the potential of KRT80 as a prognostic biomarker.
Clinical data collection
In this study, we collected clinical data from patients with NSCLC, which has been approved by the Ethics Committee of the First Affiliated Hospital of Kunming Medical University. All participants provided written informed consent. The study included 175 patients, including 107 men and 68 women, with a median age of 57 years and an age range of 27 to 78 years. NSCLC patients were divided into the Xuanwei lung cancer (XWLC) group (72 patients) and the non-Xuanwei lung cancer group (103 patients), based on the definition of three consecutive generations of residents in coal producing areas and a history of coal burning for more than 10 years. The sample collection period was from December 2008 to October 2015, and 175 pairs of samples were obtained from the Third Affiliated Hospital of Kunming Medical University. The samples were treated with paraffin embedding after being fixed with 10% formaldehyde at room temperature for 24 h. We obtained samples of primary NSCLC tissue and its paired non-cancerous lung tissue (5 cm from the tumor edge). The tumor samples were staged according to the TNM Staging 7 th edition of Lung cancer and the American Joint Committee on Cancer (AJCC) staging system, including clinical and pathological staging18.
The patients included in this study were all diagnosed with stage I-III NSCLC, and patients receiving preoperative radiation, chemotherapy, or biologic therapy were excluded. None of the patients had a diagnosis of multiple primary cancers in other organs or tissues. Clinical data are derived from patient records. All 175 NSCLC patients underwent complete surgical resection, including primary tumor and mediastinal and bronchial lymph node dissection. All patients had valid and accurate follow-up data, ranging from 2 months to 110 months. Patient follow-up data were updated through medical records, interviews, and telephone calls.
According to the National Comprehensive Cancer Network (NCCN) guidelines19, adjuvant chemotherapy is not recommended for patients with stage IA, but may be beneficial for some patients with stage IB. For stage II and III NSCLC, which are challenging and controversial to treat, four cycles of platinum-based adjuvant chemotherapy are recommended to address micrometastatic disease.
Immunohistochemistry (IHC)
To assess the expression levels and distribution patterns of KRT80 in 175 pairs of non-small cell lung cancer (NSCLC) tissues, immunohistochemical (IHC) staining was conducted following established methodologies5. Tissue specimens were sectioned into 4 μm thick slices and subjected to heat treatment at 70 °C for 2 h. Dewaxing was performed using xylene, followed by rehydration through a graded alcohol series. For the detection of the KRT80 protein, the tissue sections were incubated with a rabbit polyclonal KRT80 antibody at a dilution of 1:500 (Catalog No: 16835-1-AP, Proteintech) at 4 °C for 12 h. Subsequently, the slices were rinsed three times with phosphate-buffered saline (PBS) and incubated with an avidin-biotin complex (Vector Laboratories, Inc.). The chromogenic reaction was conducted utilizing 3,3’-diaminobenzidine as the chromogen. A volume of 30 µL of the secondary antibody, provided in its original concentration from the DAB kit (Dako; Agilent Technologies, Inc.), was applied to the tissue sections and incubated at 37 °C for 30 min. Subsequently, the tissue sections underwent dehydration through a graded ethanol series at room temperature and were mounted in neutral gum for examination via optical microscopy (Leica Microsystems GmbH) at magnifications of 100x and 200x.
Evaluation of IHC
In the immunohistochemical (IHC) analysis, brown-yellow staining was predominantly localized within the cytoplasm, with occasional presence in the nuclei of KRT80-positive cells. The staining results were evaluated by two independent pathologists from the Third Affiliated Hospital of Kunming Medical University, who employed fluorescent inverted microscopy at magnifications of x100 and x200, while remaining blinded to the clinical parameters. The magnitude and intensity of the immune response were evaluated using a semi-quantitative approach. The specific scoring criteria were defined as follows: a score of 0 indicated 0% immune response cells; a score of 1 corresponded to less than 5% immunoreactive cells; a score of 2 represented 5–50% immune response cells; and a score of 3 denoted more than 50% immune response cells. The intensity of immunoreactivity was scored as follows: 0 for negative, 1 for weak, 2 for intermediate, and 3 for strong. These scores were categorized based on the cumulative immunoreactivity scores: 0 was classified as negative, 1–2 as weak, 3 as moderate, and 4–6 as strong20. A final immunoreactivity score greater than 0 was considered positive, whereas a score of 0 was deemed negative.
Statistical analysis
All statistical analyses were performed using R software (version 4.0.4) and SPSS version 26 (SPSS for Windows, release 26.0; SPSS, Chicago, IL, USA) and Prism 9.8 (GraphPad software, Inc., San Diego, CA, USA). Kaplan-Meier curve and log-rank test were used to evaluate the difference in survival rate among all groups. Wilcoxon test or Student ‘st test was used for continuous data, and Fisher exact test or Chi-square test was used for categorical variables. P < 0.05 was the threshold of significance, and the difference was statistically significant.
Results
KRT80 in online database
In this study, we performed a preliminary analysis of the GSE19188 dataset, which included 91 NSCLC cases and 65 normal lung tissue samples, and the GSE75037 dataset, which included 83 lung adenocarcinomas and 83 corresponding adjacent normal lung tissue. The analysis results (Fig. 1a) showed that the expression level of KRT80 in NSCLC was significantly higher than that in normal lung tissue (p < 0.001), and there was significant heterogeneity in the expression level of KRT80 in different pathological subtypes of NSCLC. Specifically, the expression level of KRT80 in both LUAD and LUSC was significantly higher than that in normal lung tissue (p < 0.001), and the expression level in lung adenocarcinoma was higher than that in lung squamous cell carcinoma. In contrast, there was no significant difference in KRT80 expression in large cell carcinoma compared with normal lung tissue. We performed a confirmatory analysis through the GEPIA2 database and the results were consistent with our preliminary analysis (Fig. 1b-c). In addition, we searched KRT80 survival curve data from the GEPIA2 database and Kaplan-Meier plotter database (Fig. 1d). The results showed that in the GEPIA2 database, the survival prognosis of NSCLC patients with high expression of KRT80 was worse (p = 0.017), while in LUAD and LUSC patients, there was no significant difference in survival prognosis between the high expression and low expression groups of KRT80. In Kaplan-Meier plotter database, there was no significant correlation between the expression level of KRT80 and survival prognosis.
KRT80 in Online databases. (a) Expression of KRT80 in NSCLC in GEO database. (b-c) Box diagram of KRT80 expression difference in GEPIA2 database and its pan-cancer expression. (d) Survival curve of KRT80 in GEPIA2 database and Kaplan-meier plotter database (231849_at). LCC: Large cell lung cancer, LUAD: lung adenocarcinoma, LUSC: lung squamous cell carcinoma, * Indicates a statistical difference.
The expression of KRT80 in NSCLC and its correlation with clinicopathological parameters
In this study, 175 samples were divided into KRT80-negative group and KRT80-positive group according to KRT80 expression. The positive and negative expressions of KRT80 in cancer tissues and adjacent normal lung tissues were shown in Fig. 2a. Table 1 shows in detail the expression pattern of KRT80 in NSCLC patients and its correlation with multiple clinicopathological features. Overall, the positive expression rate of KRT80 in cancer tissues of NSCLC patients (64.6%, 113/175) was significantly higher than that in para-cancer tissues (29.7%, 52/175) (p = 0.000). Chi-square test results showed that the positive expression of KRT80 in NSCLC was significantly correlated with area (P = 0.000), age (p = 0.045) and pathological type (p = 0.001), but was not significantly correlated with gender, smoking history, drinking history, pathological type, pT stage, pTNM, and tumor size. Regionally, the positive rate of KRT80 expression was 83.3%(60/72) in xuanwei area and 51.5% (53/103) in Non-xuanwei area. In terms of pathological types, the positive rate of KRT80 was 71.8% (94/131) in LUAD and 43.2% (19/44) in LUSC. The tumor stages were: stage I 86 cases (49.1%), stage II 34 cases (19.4%), and stage III 55 cases (31.5%). The median follow-up time was 39 months, and the follow-up time ranged from 2 to 110 months. Of the 175 patients, 71 (40.6%) died from non-small cell lung cancer, while 104 (59.4%) were still alive at the end of follow-up.
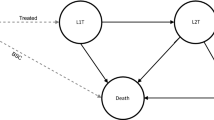
In order to further explore the influence of factors such as KRT80 expression on the prognosis of patients with NSCLC, univariate and multivariate cox regression analysis was performed (Fig. 2b). Univariate analysis showed that differentiation, pT stage, pN stage, pTNM stage and tumor size were significantly correlated with prognosis (p < 0.05). However, in multivariate analysis, only the pN period remained significant (p = 0.020). Patients with non-small cell lung cancer with lymph node metastasis had a 2.656 times greater risk of disease progression or death than those without lymph node metastasis (HR: 2.656, 95% CI :1.169–6.032). Kaplan-Meier (K-M) survival curve analysis showed that there was no significant difference in survival prognosis between KRT80 positive expression group and negative group in NSCLC patients (p = 0.35, Fig. 2c). To assess the potential of KRT80 as a biomarker for NSCLC, receiver operating characteristic (ROC) curves were constructed. The area under the curve (AUC) is 0.6686 (p < 0.0001, Fig. 2d), which corresponds to a exploratory diagnostic potential classifier in NSCLC.
The expression of KRT80 in NSCLC and its correlation with clinicopathological parameters in different regions
We divided 175 patients into Xuanwei group (72 cases) and non-Xuanwei group (103 cases) according to the region. Table 2 details the expression of KRT80 in both Xuanwei and non-Xuanwei patients and its correlation with clinicopathological parameters. The results showed that the expression of KRT80 was not significantly correlated with most clinicopathological features (p > 0.05). Specifically, in the Xuanwei group, the expression of KRT80 was moderately correlated with the degree of tumor pathological differentiation (Low vs. Moderately-Gigh vs. Unknown, p = 0.032). In the Non-xuanwei group, the expression of KRT80 was correlated with the histological type of the tumor (p = 0.037). In Xuanwei group, univariate cox analysis showed that pN stage (p = 0.000), pTNM stage (p = 0.004) and Tumor size (p = 0.003) were significantly correlated with prognosis (p < 0.05)(Fig. 3a). However, in the multivariate cox analysis, only the significance of Tumor size(p = 0.012) was retained. The K-M curve showed (Fig. 3b) that there was no significant correlation between the expression of KRT80 and patient survival in Xuanwei group (p = 0.54). As shown in the ROC curve (Fig. 3c), the AUC value is 0.7014 (p < 0.0001), and the maximum AUC is 1, which indicates a perfect classifier for Xuanwei NSCLC. In the non-Xuanweil group, univariate cox analysis showed that pT stage (p < 0.05), pN stage (p = 0.001), pTNM stage(p = 0.000) were significantly correlated with prognosis (Fig. 3d). However, in the multivariate cox analysis, only the significance of the pT stage was retained (regardless of the T1 vs. T2 vs. T3 vs. T4 group or the T1-2 vs. T3-4 group). As shown in the K-M curve (Fig. 3e), there was no significant correlation between KRT80 expression and survival prognosis in the non-Xuanwei group (p = 0.43). As shown in the ROC curve (Fig. 3.f), the AUC value is 0.6456 (p = 0.0003), which indicates a moderate diagnostic performance for non-Xuanwei NSCLC.
Expression of KRT80 in Xuanwei and Non-xuanwei region. (a) Univariate and multivariate cox analysis of KRT80 in Xuanwei patients. (b-c) Survival curve and ROC curve of KRT80 patients in Xuanwei area. (d) Univariate and multivariate cox analysis of KRT80 in Non-xuanwei patients. (e-f) Survival curve and ROC curve of KRT80 patients in Non-xuanwei area. Statistical significance was shown by p-values that were less than 0.05.
The expression of KRT80 and its correlation with clinicopathological parameters in different lung cancer subtypes
We divided 175 patients into lung adenocarcinoma group (72 cases) and lung squamous cell carcinoma group (103 cases) according to histological type. Table 3 details the expression of KRT80 in lung adenocarcinoma group and lung squamous cell carcinoma group and its correlation with clinicopathological parameters. The results showed that in the lung adenocarcinoma group, the expression of KRT80 was only correlated with the region (p = 0.001), and the positive expression rate of KRT80 in Xuanwei region (54/63, 85.7%) was significantly higher than that in Non-xuanwei region (40/68, 58.8%). There was no significant correlation between the expression of KRT80 and clinicopathologic features in lung squamous cell carcinoma group (p > 0.05). In the lung adenocarcinoma group, univariate cox analysis showed that KRT80 expression (p = 0.049), area (p = 0.009), differentiation (p = 0.049), pT stage (p = 0.017), pN stage (p = 0.000), pTNM stage (p = 0.000) and tumor size (p = 0.000) were significantly correlated with prognosis (Fig. 4a). In multivariate cox analysis, KRT80 expression (p = 0.002), differentiation (p = 0.049), pN stage(p = 0.022) and tumor size (p = 0.006) were still significantly correlated with prognosis. K-M curve showed that KRT80 expression was significantly correlated with survival in lung adenocarcinoma group (p = 0.045, Fig. 4b). As shown in the ROC curve (Fig. 4c), the AUC value was 0.6908 (p < 0.0001), suggesting a reasonably effective classifier for lung adenocarcinoma. In the lung squamous cell carcinoma group, univariate cox analysis showed a significant correlation between pN stage (p = 0.033) and prognosis (Fig. 4d). As shown in the K-M curve (Fig. 4e), there was no significant correlation between KRT80 expression and survival in lung squamous cell carcinoma group (p = 0.22). As shown in the ROC curve (Fig. 4f), the AUC value was 0.6023 (p = 0.0985), indicating that the classifier may not be sufficiently effective for diagnosing lung squamous cell carcinoma.
Expression of KRT80 in LUAD and LUSC. (a) Univariate and multivariate analysis of patients with LUAD. (b-c) KRT80 survival curve and ROC curve of LUAD patients. (d) Univariate and multivariate analysis of patients with LUSC. (e-f) KRT80 survival curve and ROC curve of LUSC patients. A p value less than 0.05 indicates a statistically significant difference.
Discussion
NSCLC is an aggressive tumor with a high mortality rate and is prone to distant metastasis21. In Xuanwei, Yunnan Province, China, the incidence and mortality of lung cancer is notably elevated, which is mainly related to the long-term exposure of local residents to polycyclic aromatic hydrocarbons (PAHs) and particulate pollution from indoor coal burning22. Keratin is the intermediate filament of epithelial cells that is expressed in a tissue-specific manner and is used as a biomarker for cancer diagnosis23,24. In the field of lung cancer, keratin members such as KRT6 A, KRT14, KRT17, and keratin-19 fragment (Cyfra21-1) can be used as prognostic biomarkers for lung cancer25,26,27,28. KRT80 is a unique member of the keratin family because it is widely expressed in a variety of epithelial cells13. KRT80 has been shown to be overexpressed in a variety of cancers and associated with poor prognosis12,29,30,31. However, the research on the role of KRT80 in lung cancer remains limited. At present, studies on the role and impact of KRT80 in NSCLC have mainly relied on bioinformatics methods. Our study is among the few that validate KRT80 expression in NSCLC using clinical samples. Compared with Jing Jiang et al. 's study32, this study only included 16 samples, while our study had a larger sample size, including a total of 175 cases, and included more comprehensive clinicopathological parameters. Such a large sample size provides us with a more solid data base, thus enhancing the reliability and generalizability of our findings. In addition, our study focused on the expression differences of KRT80 in different regions and different histological subtypes (LUAD and LUSC).
We systematically analyzed KRT80 expression and its association with clinicopathological features in 175 patients with NSCLC. The results showed that KRT80 was highly expressed in cancer tissues. The expression of KRT80 was significantly correlated with the region and pathological type. Specifically, the positive expression rate of KRT80 in patients in Xuanwei area was significantly higher than that in Non-xuanwei area, and the positive expression rate in patients with lung adenocarcinoma was also significantly higher than that in patients with lung squamous cell carcinoma. These results suggest that the positive expression of KRT80 may be influenced by region-specific factors and different histological subtypes of lung cancer. Through univariate and multivariate cox regression analysis, postoperative lymph node staging (pN stage) is an independent prognostic factor for NSCLC patients, but its confidence interval is wide, and the accuracy of this prognostic factor needs to be further verified in future studies. The expression level of KRT80 is not significantly associated with the survival prognosis of patients, so it may not be suitable as a prognostic biomarker for total population of NSCLC. The area under the ROC curve (AUC) is often used to evaluate the predictive performance of biomarker models33. For cancer biomarkers with potential clinical utility, the AUC value should be higher than 0.6, while an AUC value higher than 0.7 is obtained from high-quality cancer biomarkers34. The results of our ROC curve analysis showed that the AUC value corresponding to KRT80 was close to 0.7, indicating that KRT80, as a biomarker, has a relatively significant diagnostic value and can effectively distinguish cancer tissues from normal tissues.
Based on these important findings, we further explored the differences in the expression of KRT80 in different geographical regions (Xuanwei region and Non-xuanwei region) and different histological types (lung adenocarcinoma and lung squamous cell carcinoma), aiming to further understand the role of KRT80 in NSCLC and its influencing factors. Unique environmental factors in Xuanwei, such as long-term exposure to polycyclic aromatic hydrocarbons (PaHs) and indoor coal-fired particles22, may lead to differences in KRT80 expression patterns. In the Xuanwei group, KRT80 expression was correlated with the degree of pathological differentiation of tumors, while in the non-Xuanwei group, KRT80 expression was correlated with the histological type of tumors. These results may indicate that KRT80 plays a different role in NSCLC in different regions. Although this phenomenon has been preliminarily observed in the current study, the complex underlying molecular mechanism behind it remains to be further explored and elucidated. Although KRT80 has been studied as a potential prognostic marker in a variety of cancers, its application as a prognostic marker has certain limitations. For example, the effects of KRT80 on prognosis and clinically relevant indicators in patients with various cancers have not been extensively studied, and even opposite conclusions have been drawn in different studies of the same cancer13. Therefore, it is necessary to deepen the molecular mechanism research and increase clinical studies to clarify the clinical application prospect of KRT80. Multivariate Cox regression analysis showed that tumor size was an independent prognostic factor in the Xuanwei group, while pT stage was an independent prognostic factor in the non-Xuanwei group. These results further emphasize the importance of tumor stage and size in NSCLC prognosis. This conclusion is contrary to the findings of Jing Jiang et al.32, who suggested that KRT80 is associated with the prognosis of patients with NSCLC. This difference may be due to differences in the selection of subjects and sample size between the two studies, which may have affected the consistency of the findings. However, ROC curve analysis indicated that KRT80 has a good ability to distinguish cancerous tissue from non-cancerous lung tissue in Xuanwei and Non-xuanwei region.
Finally, we divided the patients into lung adenocarcinoma group and lung squamous cell carcinoma group according to histological type, and analyzed the correlation between KRT80 expression and clinicopathological parameters. In the lung adenocarcinoma cohort, KRT80 expression exhibited a significant correlation with region, and KRT80 serves as an independent prognostic factor for patients with lung adenocarcinoma. However, there was no significant correlation between KRT80 expression and survival prognosis in lung squamous cell carcinoma group. These results suggest that KRT80 may have different biological significance and prognostic value in different pathological types of NSCLC. It is noteworthy that KRT80, as a biomarker, may exhibit sufficient effectiveness in diagnosing lung adenocarcinoma but not lung squamous cell carcinoma.
In the field of lung cancer research, several studies have revealed the role of KRT80 in NSCLC. KRT80 promotes the proliferation, migration, invasion and EMT of non-small cell lung cancer by regulating TGF-β/SMAD signaling pathway, which may be a potential target for NSCLC treatment. The regional and histological variation in KRT80 expression may stem from microenvironmental TGF-β/SMAD gradients, receptor availability specific to cell types, and SMAD - dependent transcriptional regulation. Together, they shape the spatial heterogeneity in KRT80 - driven EMT and invasion, underscoring the TGF-β/SMAD pathway’s crucial role in modulating KRT80’s oncogenic effects in NSCLC11. In addition, Hiroki Sanada et al. studied tumor suppressive microRNAs (miRNAs) and found that high expression of KRT80 was significantly correlated with poor prognosis of lung adenocarcinoma (LUAD) patients, with the 5-year survival rate and disease-free survival rate were significantly reduced35. Gang Li et al. also found that the expression level of KRT80 was increased in lung adenocarcinomas and was associated with poor prognosis of patients when studying KRT family genes36. Fan Feng et al.. revealed the correlation between the high expression of KRT80 and the lower overall survival rate of LUAD patients based on the differential expression genes shared by tuberculosis and LUAD37. At the same time, it was observed that the expression level of KRT80 increased with the increase of clinicopathological stage, suggesting that KRT80 may be associated with the progression of tumor metastasis. Jing Jiang et al. identified KRT80 as a new prognostic and predictive biomarker of human lung adenocarcinoma by bioinformatics methods, and the transcription level of KRT80 in LUAD samples was positively correlated with clinical parameters such as lymph node metastasis stage, distant metastasis, and pathological stage32. However, these studies mainly rely on bioinformatics methods and experiments at the cell sample level. Our study, based on 175 clinical samples, adopted a more direct and systematic approach to clinical data analysis. We not only verified the expression pattern of KRT80 in NSCLC, but also explored its relationship with various clinicopathological features, including region, age, pathological type and prognosis. In addition, our study evaluated the independent effect of KRT80 expression on patient prognosis through Cox regression analysis, providing more comprehensive clinical evidence.
In summary, our study clearly demonstrated the up-regulation of KRT80 expression in cancer tissues of NSCLC patients, especially in lung adenocarcinoma patients and people in Xuanwei area. The expression of KRT80 showed significant regional specificity and histological heterogeneity among subtypes. Although KRT80 expression was not directly associated with patient prognosis, it showed a high ability to distinguish cancerous tissue from adjacent normal lung tissue, suggesting that KRT80 may be used primarily as a potential diagnostic biomarker rather than an independent prognostic indicator.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Bray, F. et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 74 (3), 229–263 (2024).
Chen, W. et al. Exosomal circSHKBP1 participates in non-small cell lung cancer progression through PKM2-mediated Glycolysis. Mol. Ther. Oncolytics. 24, 470–485 (2022).
Xia, Z., Xiao, J., Dai, Z. & Chen, Q. Membrane progesterone receptor α (mPRα) enhances hypoxia-induced vascular endothelial growth factor secretion and angiogenesis in lung adenocarcinoma through STAT3 signaling. J. Transl Med. 20 (1), 72 (2022).
Kuśnierczyk, P. Genetic differences between smokers and never-smokers with lung cancer. Front. Immunol. 14, 1063716 (2023).
Li, R. et al. Increased expression of the RNA-binding motif protein 47 predicts poor prognosis in non-small-cell lung cancer. Oncol. Lett. 19 (4), 3111–3122 (2020).
Wang, W. et al. Chemosensitizing effect of shRNA-mediated ERCC1 Silencing on a Xuanwei lung adenocarcinoma cell line and its clinical significance. Oncol. Rep. 37 (4), 1989–1997 (2017).
Zhang, Y. et al. Expanded PAH analysis of household air pollution in a rural region of China with high lung cancer incidence. Environ. Pollut. 361, 124717 (2024).
Zheng, Y. et al. EOAI, a ubiquitin-specific peptidase 5 inhibitor, prevents non-small cell lung cancer progression by inducing DNA damage. BMC Cancer. 23 (1), 28 (2023).
Cheng, Y. et al. Cytokeratin 18 regulates the transcription and alternative splicing of apoptotic–related genes and pathways in HeLa cells. Oncol. Rep. 42 (1), 301–312 (2019).
Yin, L. et al. KRT13 promotes stemness and drives metastasis in breast cancer through a plakoglobin/c-Myc signaling pathway. Breast Cancer Res. 24 (1), 7 (2022).
Tong, Y., Chen, X., Feng, Z., Xu, C. & Li, Y. Keratin 80 promotes migration and invasion of Non-Small cell lung Cancer cells by regulating the TGF-β/SMAD pathway. Evid. Based Complement. Alternat Med. 2022, 2630351 (2022).
Yun, W. J. et al. The facilitating effects of KRT80 on chemoresistance, lipogenesis, and invasion of esophageal cancer. Cancer Biol. Ther. 25 (1), 2302162 (2024).
Wei, X. Y. et al. Characters of KRT80 and its roles in neoplasms diseases. Cancer Med. 12 (13), 13991–14003 (2023).
S P. Expression data for early stage NSCLC. [updated 2019-03-25. (2010). Available from: https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE19188
Gazdar, A. G. L., Stephen, L., Wan, L. & Zhang, W. Expression profiling of 83 matched pairs of lung adenocarcinomas and non-malignant adjacent tissue 2016 [updated 2019-02-18.
Tang, Z., Kang, B., Li, C., Chen, T. & Zhang, Z. GEPIA2: an enhanced web server for large-scale expression profiling and interactive analysis. Nucleic Acids Res. 47 (W1), W556–w60 (2019).
Yang, Y. et al. Kinesin family member 3A inhibits the carcinogenesis of non-small cell lung cancer and prolongs survival. Oncol. Lett. 20 (6), 348 (2020).
Edge, S. B. & Compton, C. C. The American joint committee on cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann. Surg. Oncol. 17 (6), 1471–1474 (2010).
Ettinger, D. S. et al. NCCN guidelines insights: Non-Small cell lung cancer, version 1.2020. J. Natl. Compr. Canc Netw. 17 (12), 1464–1472 (2019).
Suwei, D. et al. NLK functions to maintain proliferation and stemness of NSCLC and is a target of Metformin. J. Hematol. Oncol. 8, 120 (2015).
Shi, L. et al. Regulatory roles of osteopontin in human lung cancer cell epithelial-to-mesenchymal transitions and responses. Clin. Transl Med. 11 (7), e486 (2021).
Chen, Y. et al. Effects and mechanism of microRNA–218 against lung cancer. Mol. Med. Rep. ;23(1). (2021).
Hamesch, K. et al. Serum keratin 19 (CYFRA21-1) links ductular reaction with portal hypertension and outcome of various advanced liver diseases. BMC Med. 18 (1), 336 (2020).
Wen, F. et al. Resistin activates p65 pathway and reduces glycogen content through keratin 8. Int. J. Endocrinol. 2020, 9767926 (2020).
Babu, S. et al. Keratin 17 and A2ML1 are negative prognostic biomarkers in non-small cell lung cancer. Pathol. Res. Pract. 263, 155643 (2024).
Xu, Q. et al. Keratin 6A (KRT6A) promotes radioresistance, invasion, and metastasis in lung cancer via p53 signaling pathway. Aging (Albany NY). 16 (8), 7060–7072 (2024).
Dong, Y. et al. Desmoglein 3 and keratin 14 for distinguishing between lung adenocarcinoma and lung squamous cell carcinoma. Onco Targets Ther. 13, 11111–11124 (2020).
Huang, H. et al. Lymphocyte percentage as a valuable predictor of prognosis in lung cancer. J. Cell. Mol. Med. 26 (7), 1918–1931 (2022).
Liu, O. et al. Keratin 80 regulated by miR-206/ETS1 promotes tumor progression via the MEK/ERK pathway in ovarian cancer. J. Cancer. 12 (22), 6835–6850 (2021).
Yasudome, R. et al. Molecular pathogenesis of colorectal cancer: impact of oncogenic targets regulated by tumor suppressive miR-139-3p. Int. J. Mol. Sci. 23, 19 (2022).
Janacova, L. et al. Catechol-O-methyl transferase suppresses cell invasion and interplays with MET signaling in Estrogen dependent breast cancer. Sci. Rep. 13 (1), 1285 (2023).
Jiang, J. et al. Identification of KRT80 as a Novel Prognostic and Predictive Biomarker of Human Lung Adenocarcinoma Via Bioinformatics Approaches (Comb Chem High Throughput Screen, 2024).
Kong, Q. et al. NMR-Based metabolomic analysis of Sera in mouse models of CVB3-Induced viral myocarditis and dilated cardiomyopathy. Biomolecules ;12(1). (2022).
Fekete, J. T. & Győrffy, B. ROCplot.org: validating predictive biomarkers of chemotherapy/hormonal therapy/anti-HER2 therapy using transcriptomic data of 3,104 breast cancer patients. Int. J. Cancer. 145 (11), 3140–3151 (2019).
Sanada, H. et al. Involvement of dual strands of miR-143 (miR-143-5p and miR-143-3p) and their target oncogenes in the molecular pathogenesis of lung adenocarcinoma. Int. J. Mol. Sci. ;20(18). (2019).
Li, G. et al. Keratin gene signature expression drives epithelial-mesenchymal transition through enhanced TGF-β signaling pathway activation and correlates with adverse prognosis in lung adenocarcinoma. Heliyon 10 (3), e24549 (2024).
Feng, F. et al. Tuberculosis to lung cancer: application of tuberculosis signatures in identification of lung adenocarcinoma subtypes and marker screening. J. Cancer. 15 (16), 5329–5350 (2024).
Acknowledgements
Not applicable.
Funding
This study was supported by the National Natural Science Foundation of China (No. 82160529), the Joint Fund of the Department of Science and Technology of Yunnan Province (No. 202001 AY070001-141), the Yunnan Revitalization Talent Support Program (grant no. RLQB20220014), and the 535 Talent Project of the First Affiliated Hospital of Kunming Medical University (No. 2023535D17). Kunming Medical University Graduate Student Innovation Fund Project (2024S059).
Author information
Authors and Affiliations
Contributions
Y.Z. and H.T.J. contributed equally to this work. Q.F. F.conceived and designed the study. Q.F.F. supervised the entire research process.Y.T.X., Z.L.W., and F.Z. performed the experiments and collected the data. C.L. and Q.Y. analyzed the data and prepared the figures. W.J. ,Q.M.Y.and J.Z. contributed to the interpretation of results and provided critical feedback on the manuscript. Y.Z. and H.T.J. wrote the main manuscript text, with input from all authors. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the First Affiliated Hospital of Kunming Medical University. All participants provided written informed consent. All methods were carried out in accordance with relevant guidelines and regulations.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zeng, Y., Jiang, H., Xia, Y. et al. Keratin 80 as a diagnostic biomarker with limited prognostic value in non-small cell lung cancer. Sci Rep 15, 19667 (2025). https://doi.org/10.1038/s41598-025-04256-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-04256-1