Abstract
Anterior shoulder dislocation is a common orthopedic emergency. While many reduction methods require sedation, the FARES (FAst, REliable, and Safe) and Spaso methods allow reduction without anesthesia. We conducted a single-center, prospective, randomized controlled trial comparing the FARES and Spaso methods for anterior shoulder dislocation reduction. Patients aged 20 to 90 years were enrolled. The assigned closed reduction procedures were performed without patient sedation by trained orthopedic residents. If two attempts with the assigned method failed, the alternative method was used. The primary outcome was the first-attempt success rate, while secondary outcomes included overall success rate with both methods, reduction time, and pain scores. During November 2013 and December 2015, a total of 32 patients were randomized to the FARES (n = 17) or Spaso (n = 15) method. The first-attempt success rates were 71.6% for the FARES group and 80.0% for the Spaso group (p = 0.691). Among patients with failed closed reduction using the first technique, all patients in the Spaso-following-FARES group achieved successful reduction, whereas none in the FARES-following-Spaso group achieved successful reduction (p = 0.092). Pain scores during reduction were comparable between the FARES (4.29 ± 1.69) and Spaso (3.80 ± 2.65) techniques, with no statistically significant difference (p = 0.542). Follow-up data were available for 28/32 patients (87.5%; mean 5.3 ± 2.2 years). Four patients were lost (3 FARES, 1 Spaso; p = 0.726). Recurrent dislocation occurred in 3 patients (10.7%; 1 FARES, 2 Spaso; p = 0.947), and 2 patients (1 per group; p = 0.876) underwent surgery (arthroscopic stabilization and rotator cuff repair). Both the FARES and Spaso methods were effective for reducing anterior shoulder dislocations. Combining these methods may improve overall reduction rates. Clinical trial registration: This trial was registered at ClinicalTrials.gov (Registration number: NCT01979237) on 08/11/2013.
Similar content being viewed by others
Introduction
Anterior shoulder dislocation is a common occurrence in orthopedic emergencies, accounting for up to 60% of all major joint dislocations1. A study in the United States reported an incidence of 23.9 per 100,000 person-years2. The most frequent type is anteroinferior dislocation. In Taiwan, the annual incidence between 2000 and 2005 was 15.3 per 100,000 population, with a mean treatment cost of US$612 per case3.
Several reduction methods have been described4,5,6 and sedation is typically required in these procedures5,7. However, sedation related complications, such as respiratory depression and anaphylaxis, necessitate close monitoring during and after the procedure8. Alternatively, the reduction techniques can be performed without anesthesia are relatively feasible and safe9,10,11.
The FARES (FAst, REliable, and Safe) method, introduced by Sayegh et al. in 200912, and the Spaso method, first described by Spaso Miljesic in 199813, are notable for achieving successful reduction without sedation14,15. Unlike traditional methods that often require forceful manipulation or sedation, both techniques aim to achieve reduction through gradual, controlled maneuvers, minimizing pain and complications. Both techniques have been reported as effective, safe, and more comfortable than traditional methods12,16,17,18.
Despite their clinical utility, direct comparative data between these two methods remain limited. Previous studies have primarily evaluated each technique individually, without determining which method offers superior success rates, faster reduction times, or lower pain levels. Furthermore, the effectiveness of a sequential approach remains unexplored. To address these gaps, this study aims to compare the efficacy, safety, and pain levels of the FARES and Spaso methods in a prospective randomized trial. We hypothesize that the FARES method will demonstrate a higher success rate in the reduction of anterior shoulder dislocations compared to the Spaso method. Additionally, we propose that a sequential approach may improve the overall reduction success rate, reducing the need for sedation or alternative reduction methods.
Methods
Study cohort
The inclusion criteria comprised patients aged 20 to 90 years who presented with anterior shoulder dislocation, with or without an associated greater tuberosity fracture. Only fully conscious and sober patients who sought medical attention within 24 h of dislocation and had no prior use of sedatives or muscle relaxants before orthopedic consultation were included. Patients were excluded if they were younger than 20 or older than 90 years, arrived at the emergency department more than 24 h after the injury, had received sedatives or muscle relaxants prior to orthopedic consultation, were unconscious or intoxicated, had polytrauma, experienced hemodynamic instability, or had Neer classification three- or four-part fractures.
Reduction procedures
All reductions were performed by second- and third-year orthopedic residents under the supervision of an attending physician. To ensure procedural consistency, all participating residents underwent standardized training before performing reductions in the study. This training program included didactic instruction, video-based training, and supervised hands-on simulation practice to ensure uniform technique application.
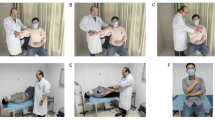
The FARES method is performed with the patient in a supine position12. The physician holds the wrist with both hands, keeping the elbow fully extended and the forearm in a neutral position. Gentle longitudinal traction is applied without counter-traction, accompanied by small vertical oscillations of approximately 5 cm at a frequency of 2–3 Hz to facilitate muscle relaxation. The arm is then gradually abducted beyond 90°, maintaining oscillation and traction. At 90° of abduction, gentle external rotation is applied to further relax the capsule and promote reduction. A distinct “clunk” or sudden release of resistance confirms successful reduction.
The Spaso method involves placing the patient in a supine position. The physician grasps the wrist or distal forearm while keeping the elbow extended and the forearm in a neutral position. Gentle vertical traction is applied to lift the arm toward the ceiling, promoting muscle relaxation and facilitating reduction. Traction is maintained even if the patient lifts their shoulder off the bed due to pain. A slight external rotation is then applied to align the humeral head with the glenoid. A “clunk” or sudden release confirms reduction. If unsuccessful after 1–2 min, gentle pressure on the humeral head may aid in completing the reduction.
Randomization was conducted using opaque, pre-sealed envelopes to ensure allocation concealment. These envelopes were prepared blindly by an independent research assistant not involved in patient treatment or outcome assessment. Each envelope contained a randomized allocation to either the FARES or Spaso method and was sequentially numbered. The envelopes were opened only after patient eligibility was confirmed. Upon enrollment, an orthopedic resident retrieved the next sequential envelope, ensuring that the allocation process remained unbiased and unpredictable. For patients whose eligibility was uncertain, the treating orthopedic resident consulted with the attending physician before randomization.
In this study, "first-attempt success rate" refers to the overall success rate after two attempts within the initially assigned method, before switching to the alternative method. If the first two reduction attempts with the assigned method failed, the alternative method was used for two additional attempts. If neither method successfully reduced the dislocation, a rescue protocol involving midazolam or propofol anesthesia was implemented, and the reduction method was determined by the treating physician. The primary outcome was the first-attempt success rate within two attempts of the assigned method. The secondary outcome was the overall success rate, including cases requiring the alternative method. Additionally, reduction time and Visual Analog Scale (VAS) scores were recorded before reduction, during reduction, and before discharge. Patients were followed up for an average of 5.3 ± 2.2 years. Recorded follow-up events included recurrent dislocation and subsequent surgical interventions.
Statistical analysis
The sample size was initially determined based on a power analysis assuming a difference in first-attempt success rates between the FARES and Spaso methods. Based on prior literature, an expected success rate of 85% for FARES and 70% for Spaso was assumed. To detect a 15% difference in success rates with a power of 80% (β = 0.2) and a significance level of 0.05 (α = 0.05), a total of 100 participants (50 per group) was originally planned. Analysis was performed using parametric and non-parametric tests, as appropriate for the data distribution. Independent-sample Student’s t-tests were used to compare reduction time and pain scores at different time points, while Fisher’s exact test was used for success rate comparisons. All analyses were conducted using SAS statistical software (SAS Institute, Inc., Cary, North Carolina). A p-value < 0.05 was considered statistically significant.
Results
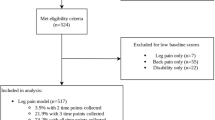
During the study period, a total of 41 patients met inclusion criteria. Six of them were excluded and 3 declined to participate. Ultimately, 32 patients were included, with 17 randomly assigned to the FARES method and 15 to the Spaso method (Fig. 1).
Flowchart of patient enrollment and allocation. A total of 41 patients met the inclusion criteria during the study period. Nine patients were excluded, including 6 who did not meet inclusion criteria and 3 who declined to participate. The remaining 32 patients were randomized, with 17 allocated to the FARES method and 15 to the Spaso method.
The baseline characteristics of the study population are summarized in Table 1. There was no between-group difference among age, gender and injury mechanism. The mean age was 49.12 ± 25.89 years in the FARES group and 49.13 ± 21.73 years in the Spaso group (p = 0.999). Male patients accounted for 58.8% (10/17) in the FARES group and 53.3% (8/15) in the Spaso group (p = 0.997). Regarding the mechanism of injury, in the FARES group, 1 case (5.9%) resulted from a traffic accident, 12 cases (70.6%) were due to falls, and 4 cases (23.5%) were attributed to other causes, including cases from excessive motion of the affected shoulder and 1 case due to a traction injury. In the Spaso group, 5 cases (33.3%) resulted from traffic accidents, 6 cases (40%) were due to falls, and 4 cases (27%) were classified as other causes, including 3 from low-energy trauma such as simple traction and 1 from a contusion. First-ever dislocation was observed in 10 patients (58.8%) in the FARES group and 10 patients (66.7%) in the Spaso group (p = 0.762).
The mean reduction time was 6.15 ± 9.79 min in the FARES group and 4.52 ± 4.64 min in the Spaso group (Table 2). No significant difference was observed between the two groups (p = 0.550). The original FARES technique was used without modifications. The first-attempt success rates were 71.6% for the FARES method and 80.0% for the Spaso method (p = 0.691). In the FARES group, 5 patients had failed reduction on the first two attempts and all of them were successfully reduced using the Spaso method. In contrast, in the Spaso group, 3 patients experienced initial failure and none of them were reduced with subsequent FARES method applied after two failed attempts with the Spaso method, No additional successful reductions were achieved.
Pain scores were recorded using the Visual Analog Scale (VAS) at multiple time points: before reduction, during reduction, and before discharge (Table 2, Fig. 2). In both the FARES and Spaso groups, pain scores during reduction were lower than those before reduction. Before reduction, patients in the Spaso group reported a higher level of pain, with a mean VAS score of 7.73 ± 2.71, compared to 6.29 ± 1.65 in the FARES group (p = 0.088). During the reduction procedure, the mean VAS during reduction was slightly lower in the Spaso group (3.80 ± 2.65) than in the FARES group (4.29 ± 1.69, p = 0.542). By the time of discharge, pain levels had further decreased in both groups, with the FARES group reporting a slightly lower mean VAS score (1.41 ± 0.71) compared to the Spaso group (1.79 ± 1.05, p = 0.269).
Concomitant greater tuberosity fractures were identified in 3 patients. Two cases were randomized to the FARES group, and reduction was unsuccessful on the first attempt. However, when the Spaso method was subsequently applied, both cases were successfully reduced. The third case, randomized to the Spaso group, was successfully reduced on the first attempt using the Spaso method.
Follow-up data were available for 28 of 32 patients (87.5%) over an average of 5.3 ± 2.2 years. Of the 4 patients lost to follow-up, 3 were in the FARES group and 1 in the Spaso group, with no significant difference between groups (p = 0.726). Recurrent dislocation occurred in 3 patients (10.7%), with 1 in the FARES group and 2 in the Spaso group (p = 0.947). Additionally, 2 patients (1 per group) underwent surgical intervention (arthroscopic stabilization in FARES and rotator cuff repair in Spaso; p = 0.876).
Discussion
This study demonstrates that both the FARES and Spaso methods effectively reduce anterior shoulder dislocations without anesthesia. The Spaso method achieved a higher initial success rate (80%) compared to FARES (71%). Notably, when Spaso was applied after a failed FARES attempt, the overall success rate increased to 100%, suggesting that a sequential approach may enhance success rates before resorting to anesthesia. However, using FARES after a failed Spaso attempt did not lead to additional successful reductions. To the best of our knowledge, this is the first study to directly compare the FARES and Spaso methods for anterior shoulder dislocation. Furthermore, this is also the first study that explores the sequential approach after the close reduction technique.
Previous studies have reported success rates ranging from 67.6% to 95% for these methods, depending on patient characteristics and operator experience12,14,16,17. The FARES method has been shown to achieve success rates of up to 95%, while Spaso has demonstrated 67.6% to 87.5%, improving with experience. Our findings align with this range, though our study reported slightly lower success rates. This may be attributed to the inclusion of patients with greater tuberosity fractures, which may have negatively impacted reduction success, particularly in the FARES group. Additionally, all reductions were performed by second- or third-year orthopedic residents, whereas some prior studies included more experienced specialists, potentially influencing outcomes.
Our study suggests that the Spaso method may be a more effective reduction technique, particularly in cases with associated greater tuberosity fractures, while FARES remains a viable alternative. Both methods were well-tolerated, reinforcing their role as non-sedation options for emergency reduction.
Pain levels during reduction were comparable to prior studies, though the mean VAS before reduction was slightly higher in our cohort. This may be due to patient anxiety, muscle spasms, or differences in pain assessment timing. Additionally, as our study did not use sedation or muscle relaxants, the reported pain levels may have been higher than those in studies where premedication was administered.
Both the FARES and Spaso methods rely on gentle traction rather than forceful manipulation, thereby minimizing pain. Our study demonstrated that pain scores during reduction were lower than before reduction, supporting the concept of ligamentotaxis, which redistributes soft tissue tension and reduces abnormal bony contact, thereby alleviating pain. Although the mean VAS before reduction and before discharge appeared higher in the Spaso group and lower during reduction, there was no significant difference in pain scores between the two groups.
The mean reduction time in our study was 6.15 min for the FARES group, which is longer than the 2-min average reduction time in previous studies12,17. However, no modifications were made to the original FARES technique. The longer reduction time observed in our study may be attributed to operator experience, patient-specific factors (e.g., muscle tension and anxiety), or differences in positioning. Further research is warranted to determine whether standardized training protocols or patient relaxation techniques could enhance efficiency.
Greater tuberosity fractures are commonly associated with anterior shoulder dislocations, particularly in elderly and osteoporotic patients. Including these cases in our study may introduce confounding factors related to potential rotator cuff instability. However, given their clinical relevance, we included only non-displaced or minimally displaced fractures, which are typically managed conservatively, while excluding fractures requiring surgical fixation to enhance the study’s real-world applicability.
In our cohort, the Spaso method appeared more effective for shoulder dislocations with associated greater tuberosity fractures. Among the 3 patients with greater tuberosity fractures in our study, 2 were randomized to the FARES group, and neither was successfully reduced on the first attempt. However, when the Spaso method was subsequently applied, both cases were successfully reduced. The third patient, randomized to the Spaso group, was successfully reduced on the first attempt using the Spaso method. The FARES method involves vertical oscillation, which may cause fracture site motion, leading to pain and muscle spasm. In contrast, the Spaso method employs more static and gradual motions, which may minimize fracture site movement and reduce discomfort. Based on these observations, we recommend favoring the Spaso method over the FARES method for shoulder dislocations associated with greater tuberosity fractures. However, given the small sample size, further studies are needed to validate this observation before making definitive clinical recommendations.
Complications associated with shoulder dislocation reduction, including iatrogenic fractures, side effect associated with sedation such as cardiovascular, respiratory depression, vascular compromise, and neurological deficits19,20,21. The Hippocratic method has been reported to carry risks of brachial plexus and vascular injuries3, while the Kocher method is associated with an increased risk of spiral humeral fractures and axillary nerve injuries22,23. Notably, no procedure-related complications have been reported with FARES and Spaso methods. Consistently, in our study, no complications were observed during or after the use of either method. Both techniques rely on gentle and controlled maneuvers, which inherently minimize the risk of iatrogenic injury.
This study has several limitations. First, the sample size was relatively small (32 cases: 17 in the FARES group and 15 in the Spaso group), which may limit the statistical power and generalizability of our findings. Future studies with larger cohorts are needed to validate our results. Second, the procedures were performed by 12 different orthopedic residents, introducing potential variability in technique. While all residents were second- or third-year trainees, minor differences in skill and experience could have influenced the outcomes. Future studies should consider standardizing procedural training or involving a more homogeneous group of practitioners. Third, while we followed up with patients for an average of 5.3 years, further studies should include more detailed assessments of long-term recurrence rates and imaging evaluations (e.g., MRI for Bankart lesions or Hill-Sachs defects). This would help determine whether the choice of reduction method influences the likelihood of recurrent dislocation or structural damage over time. Fourth, while we included patients with greater tuberosity fractures, only non-displaced or minimally displaced fractures were studied. The impact of these fractures on reduction techniques warrants further investigation in larger studies.
Conclusion
Both the FARES and Spaso methods effectively reduce anterior shoulder dislocations, and combining these techniques may enhance success rates. Our findings also indicate that the Spaso method might be particularly effective for dislocations with associated greater tuberosity fractures. However, larger scale studies are required to confirm their efficacy and clinical relevance.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to patient confidentiality but are available from the corresponding author on reasonable request.
References
Verweij, L. P., Baden, D. N., van der Zande, J. M. & van den Bekerom, M. P. Assessment and management of shoulder dislocation. BMJ 371, m4485 (2020).
Patrick, C. M. et al. Epidemiology of shoulder dislocations presenting to United States emergency departments: An updated ten-year study. World J. Orthop. 14(9), 690–697 (2023).
Yang, N. P. et al. Epidemiological survey of orthopedic joint dislocations based on nationwide insurance data in Taiwan, 2000–2005. BMC Musculoskelet. Disord. 12, 253 (2011).
Puha, B., Gheorghevici, T. S., Veliceasa, B., Popescu, D. & Alexa, O. Clasic versus novel in reduction of acute anterior dislocation of the shoulder: A comparison of four reduction techniques. Rev. Med. Chir. Soc. Med. Nat. Iasi. 120(2), 311–315 (2016).
Cunningham, N. J. Techniques for reduction of anteroinferior shoulder dislocation. Emerg. Med. Australas. 17(5–6), 463–471 (2005).
Dong, H., Jenner, E. A. & Theivendran, K. Closed reduction techniques for acute anterior shoulder dislocation: A systematic review and meta-analysis. Eur. J. Trauma Emerg. Surg. 47(2), 407–421 (2021).
Wronka, K. S., Ved, A. & Mohanty, K. When is it safe to reduce fracture dislocation of shoulder under sedation? Proposed treatment algorithm. Eur. J. Orthop. Surg. Traumatol. 27(3), 335–340 (2017).
Innes, G., Murphy, M., Nijssen-Jordan, C., Ducharme, J. & Drummond, A. Procedural sedation and analgesia in the emergency department, Canadian Consensus Guidelines. J. Emerg. Med. 17(1), 145–156 (1999).
Anjum, R. et al. Reducing shoulder dislocation without anaesthesia or assistant: Validation of a new reduction manoeuvre. Chin. J. Traumatol. 22(5), 274–277 (2019).
O’Connor, D. R., Schwarze, D., Fragomen, A. T. & Perdomo, M. Painless reduction of acute anterior shoulder dislocations without anesthesia. Orthopedics 29(6), 528–532 (2006).
Baden, D. N. et al. Effects of reduction technique for acute anterior shoulder dislocation without sedation or intra-articular pain management: A systematic review and meta-analysis. Eur. J. Trauma Emerg. Surg. 49(3), 1383–1392 (2023).
Sayegh, F. E. et al. Reduction of acute anterior dislocations: A prospective randomized study comparing a new technique with the Hippocratic and Kocher methods. J. Bone Joint Surg. Am. 91(12), 2775–2782 (2009).
Yuen, M. C., Yap, P. G., Chan, Y. T. & Tung, W. K. An easy method to reduce anterior shoulder dislocation: The Spaso technique. Emerg. Med. J. 18(5), 370–372 (2001).
Ugras, A. A., Mahirogullari, M., Kural, C., Erturk, A. H. & Cakmak, S. Reduction of anterior shoulder dislocations by Spaso technique: Clinical results. J. Emerg. Med. 34(4), 383–387 (2008).
Sayegh, F. E. et al. Reduction of acute anterior dislocation with the FARES method. JBJS Essent. Surg. Tech. 2(3), e13 (2012).
Fernandez-Valencia, J. A., Cune, J., Casulleres, J. M., Carreno, A. & Prat, S. The Spaso technique: A prospective study of 34 dislocations. Am. J. Emerg. Med. 27(4), 466–469 (2009).
Maity, A., Roy, D. S. & Mondal, B. C. A prospective randomised clinical trial comparing FARES method with the Eachempati external rotation method for reduction of acute anterior dislocation of shoulder. Injury 43(7), 1066–1070 (2012).
Chamseddine, A. H. et al. FARES method for reduction without medication of first episode of traumatic anterior shoulder dislocation. Int. Orthop. 43(5), 1165–1170 (2019).
Pan, X. et al. Iatrogenic fracture during shoulder dislocation reduction: Characteristics, management and outcomes. Eur. J. Med. Res. 26(1), 73 (2021).
Sithamparapillai, A., Grewal, K., Thompson, C., Walsh, C. & McLeod, S. Intra-articular lidocaine versus intravenous sedation for closed reduction of acute anterior shoulder dislocation in the emergency department: A systematic review and meta-analysis. CJEM 24(8), 809–819 (2022).
Hara, T. et al. Practical guide for safe sedation. J. Anesth. 37(3), 340–356 (2023).
Beattie, T. F., Steedman, D. J., McGowan, A. & Robertson, C. E. A comparison of the Milch and Kocher techniques for acute anterior dislocation of the shoulder. Injury 17(5), 349–352 (1986).
Berkenblit, S. I., Hand, M. B. & MacAusland, W. R. Reduction of skiing-related anterior shoulder dislocation using Kocher’s method without traction. Am. J. Orthop. (Belle Mead NJ). 29(10), 811–814 (2000).
Acknowledgements
We thank Hsu Tei-Kai, Wang Chun-Liang, Chuang Hsiu-Ming, Hsieh Hsiang-Chieh, Kuo Ying-Kuei, Chen Nai-Chi, Chiang Ming-Hung, Li Wei-Sheng, Lin Hsin-Ying,and Tsai Yuen-Cheng for their assistance in performing reductions using the FARES or Spaso methods.
Funding
Financial support from the Ministry of Science and Technology, Taiwan (ROC) (MOST111-2221-E-341-002) and the Shin Kong Wu Ho-Su Memorial Hospital, Tawan (2024SKHADR023) are greatly appreciated.
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: S.H. Chang. Analyzed the data: S.H. Chang, L.W. Hung and K. H. Lee. Paper writing: S.H. Chang, L.W. Hung and K. H. Lee. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
We conducted a single-center, prospective, randomized controlled trial comparing the FARES and Spaso methods for anterior shoulder dislocations. This study was approved by the National Taiwan University Hospital (NTUH) Research Ethics Committee (REC) (Approval number: 201307037RINC). Informed consent was obtained from all participants or their legal guardians prior to enrollment. All methods were performed in accordance with the Declaration of Helsinki and relevant institutional and regulatory guidelines. This trial was registered at ClinicalTrials.gov (Registration number: NCT01979237) on 08/11/2013. Data were collected from patients with anterior shoulder dislocations treated in the emergency department between November 2013 and December 2015.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lee, KH., Chang, SH. & Hung, LW. FARES and Spaso method for anterior shoulder dislocation: a prospective randomized control study demonstrating the benefit of a combined approach. Sci Rep 15, 18974 (2025). https://doi.org/10.1038/s41598-025-04311-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04311-x