Abstract
The purpose of this study was to assess the retinal relative peripheral refraction (RPR) in children with low myopia and pre-myopia, and investigate the differences in RPR using multispectral refraction topography (MRT). Ninety-five children were enrolled in the Department of Ophthalmology, Jinshan Hospital affiliated to Fudan University. MRT could measure total RPR (TRPR) of the 53° range centered on macular fovea. TRPR divided into four quadrants: superior RPR (RPR-S), inferior RPR (RPR-I), temporal RPR (RPR-T) and nasal RPR (RPR-N). The MRT analysis report also showed RPR in the visual field of 15° (RPR-15), 30° (RPR-30) and 45° (RPR-45) centered on the macular fovea, respectively. RPR-(15–30), RPR-(30–45) and RPR-(15–45) were calculated. TRPR (R = − 0.264, P = 0.010), RPR-I (R = − 0.261, P = 0.011), RPR-T (R = − 0.240, P = 0.019), RPR-45 (R = − 0.211, P = 0.040), RPR-(30–45) (R = − 0.232, P = 0.023) and RPR-(15–45) (R = − 0.243, P = 0.018) were negatively correlated with spherical refraction. Spherical equivalent of low myopia group was significantly less than pre-myopia group (− 1.18 ± 0.57 D vs. 0.13 ± 0.31 D, P < 0.001) whereas axial length of low myopia group was significantly longer than pre-myopia group (24.14 ± 0.70 mm vs. 23.35 ± 0.60 mm, P < 0.001). TRPR of low myopia group and pre-myopia group was 0.52 ± 0.62 D and 0.32 ± 0.41 D, respectively, without sigficant difference (P = 0.075). All the RPRs were hyperopia in the children with low myopia and pre-myopia, except for RPR-T in pre-myopia group. RPR-I in low myopia group was significantly larger than that in pre-myopia group (0.42 ± 0.72 (95% CI 0.22, 0.62) D vs. 0.04 ± 0.67 (95% CI − 0.17, 0.25) D, P = 0.010). In conclusion, RPRs become more hyperopia with the changing trend from pre-myopia to myopia. Children with low myopia and pre-myopia have relative peripheral hyperopia. Furthermore, children with low myopia have larger relative peripheral hyperopia compared with pre-myopia.
Similar content being viewed by others
Introduction
Myopia has been a worldwide epidemic issue1,2. The global prevalence of myopia and high myopia are 28.3% and 4.0% in 2010, and will increase to 50% and 10% by 20503. The highest prevalence of myopia in children has been reported in urban areas of Asia, where the prevalence of myopia is approximately 80–90% at the age of 17–18 and the prevalence of high myopia is approximately 10–20%2. It is worth noting that myopia and myopia-related complications can lead to visual impairment and economic burden4,5.
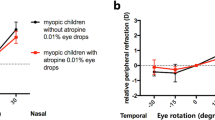
However, the precise mechanism of myopia development is still unclear. It is reported that peripheral refraction has an important influence in eye development6,7,8,9,10,11,12,13,14. In 1971, Hoogerheide et al6 firstly identified retinal peripheral refraction as a risk factor for the onset of myopia: pilots who developed myopia tended to have retinal peripheral hyperopia defocus before myopia occurred. Many subsequent studies showed that myopia had retina relative peripheral hyperopia, whereas hyperopia had relative retina peripheral myopia7,10,11,12. In addition, some modalities for slowing myopia progression are based on the peripheral refraction hypothesis theory, such as orthokeratology15, defocus incorporated multiple segments spectacle lenses16, etc. The retinal peripheral refraction at a few points on the horizontal and/or vertical meridian (often 5°–10° apart) were measured in previous studies due to the limitations of experimental technology, which can not fully reflect the retinal regional peripheral defocus11. Therefore, a more comprehensive assessment of peripheral refraction will provide a deeper understanding of its relationship with myopia.
Multispectral refraction topography (MRT) is Chinese novel self-developed multispectral fundus imaging system17,18,19,20. MRT is designed to measure the retinal peripheral refraction within a certain range in 2–3 s through the deeply developed algorithm formula. Relative peripheral refraction (RPR) is described in the MRT analysis report.
Pre-myopia, defined as “A refractive state of an eye of ≤ + 0.75D and > − 0.50D in children” by the International Myopia Institute21, is an important peroid before the onset of myopia. It was reported that the 12-month incidence of myopia in the children with pre-myopia was 61.3% in Shanghai, China22. Thus, analyzing the differences of PRP in children between low myopia and pre-myopia is conducive to understanding the myopia development. The purpose of this study was to assess RPR in children with low myopia and pre-myopia, and investigate the differences in RPR using MRT.
Methods
Subjects
This was an observational study. The study was approved by the Ethics Committee of Jinshan Hospital affiliated to Fudan University (No. JIEC 2024-S46). All study procedures adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from the parents or guardians of all children after full explanation.
Inclusion criteria were: (1) 6 to 14 years, (2) the spherical equivalent (SE) range of + 0.75 D ~ − 3.00 D, (3) without cylinder power based on subjective refraction. Exclusion criteria were: (1) serious ocular diseases (e.g., keratoconus, morning glory syndrome, Stargardt disease, Coats disease, etc.), and (2) systemic diseases affecting ocular refraction (e.g., Marfan syndrome, etc.).
Ninety-five children were enrolled in the department of Ophthalmology, Jinshan Hospital affiliated to Fudan University. The mean age, SE and axial length (AL) were 8.5 ± 1.7 (95% CI 8.2, 8.9) years, − 0.61 ± 0.80 (95% CI − 0.78, − 0.45) D, 23.80 ± 0.76 (95% CI 23.65, 23.97) mm, respectively. According to SE, the children were then divided into two groups: low myopia group (− 3.00 D ≤ SE ≤ − 0.50 D, n = 54), pre-myopia group (− 0.50 D < SE ≤ + 0.75 D, n = 41).
Examination
All children underwent comprehensive examination including uncorrected distance visual acuity (UCVA), cycloplegical subjective refraction, best corrected distance visual acuity (BCDVA), intraocular pressure, slit-lamp examination and dilated fundoscopy. Cycloplegia was achieved by topical application of 4 drops of tropicamide 0.5% (Bausch & Lomb Pharmaceutical Co., Ltd, Shandong, China) at 5-min intervals. Cycloplegia was considered complete if the pupil diameter was more than 6 mm and pupillary constriction was absent. Subjective refraction was then performed using a comprehensive refractometer (CV-5000, Topcon, Japan) according to the standard procedure by an experienced optometrist 30 min after the last eye drop. AL was measured with IOL Master 500 (Carl Zeiss Meditec, German).
Multispectral refraction topography (MRT, MSI C2000, Thondar Technology Co., Ltd, Shenzhen, China) is used to measure the relative peripheral refraction (RPR) with good agreement and repeatability after cycloplegia19,23. The principle of MRT has been demonstrated in detail in the previous studies17,18,19,20. Briefly, Children are positioned on the headrest and asked to focus on an internal fixation target in the examination room with dim illumination. MRT measurements are taken, and only the measurements with a quality score of > 80% are recorded for further analysis. MRT can obtain the RPR through measuring a total of 128 × 128 points with intervals of 0.5°. RPR then converted to a color image (Fig. 1A,B) through the calculation process by the equipment software: hyperopia is warm (from yellow to red), and myopia is cold (from blue to green). After color conversion, a set of three dimensional images can be obtained and provide a direct view of the relative refraction of the retina (Fig. 1C,D). The MRT analysis report shows the total RPR (TRPR) of the circular visual field of 53° centered on macular fovea. TRPR is divided into four quadrants, RPR in the upper quadrant (RPR-S), RPR in the inferior quadrant (RPR-I), RPR in the temporal quadrant (RPR-T) and RPR in the nasal quadrant (RPR-N), respectively. The MRT analysis report also shows average RPR in the visual field of 15° (RPR-15), average RPR in the visual field of 30° (RPR-30) and average RPR in the visual field of 45° (RPR-45) centered on the macular fovea, respectively. In addition, RPR in the visual field from 15° to 30° is recorded as RPR-(15–30), RPR in the visual field from 30° to 45° is recorded as RPR-(30–45) and RPR in the visual field from 15° to 45° is recorded as RPR-(15–45), respectively. RPR-(15–30) is calculated as RPR-30 minus RPR-15, RPR-(30–45) as RPR-45 minus RPR-30, RPR-(15–45) as RPR-45 minus RPR-15. RPR-(15–30), RPR-(30–45) and RPR-(15–45) represent the amount of RPR in the midperipheral retina.
Sample size
The sample size estimation was carried out under the presumption of a 2-sided α level of 0.05, 80% statistical power, and the expected effect size. Drawing from a previous study on TRPR among hyperopia, emmetropia, and myopia groups, it was hypothesized that the difference in TRPR between low myopia group and pre-myopia group would be 0.2 D, with a standard deviation of 0.3 D. This would require a total of 72 children (36 per group).
Statistical analysis
Both eyes of each child were examined, and only data from the right eye was used for analysis. Data analysis was performed using the SPSS17.0 software. The distribution of each parameter was assessed using the Kolmogorov–Smirnov test. For normally distributed variables, data were expressed as the mean ± standard deviation. Independent t test was used to compare the differences in age, SE, AL and RPR between both groups. Chi-square test was used to compare gender differences between both groups. One-way analysis of variance (ANOVA) with the Bonferroni post-hoc test were used to compare the differences of RPR-S, RPR-I, RPR-T and RPR-N in each group. Pearson correlation was used to analyze the association of RPR with age, SE, and AL. P < 0.05 was considered as statistically significant.
Results
The histograms of SE and RPR frequency of all the children were shown in Fig. 2. The mean values of TRPR and all the regional RPRs were hyperoia. The associations of TRPR, RPR-S, RPR-I, RPR-T, RPR-N, RPR-15, RPR-30, RPR-45, RPR-(15–30), RPR-(30–45) and RPR-(15–45) with age, SE, AL were shown in Table 1. As shown in Fig. 3, TRPR (R = − 0.264, P = 0.010, Fig. 3A), RPR-I (R = − 0.261, P = 0.011, Fig. 3B), RPR-T (R = − 0.240, P = 0.019, Fig. 3C), RPR-45 (R = − 0.211, P = 0.040, Fig. 3D), RPR-(30–45) (R = − 0.232, P = 0.023, Fig. 3E) and RPR-(15–45) (R = − 0.243, P = 0.018, Fig. 3F) were negatively correlated with SE. Exception for those, no significant correlations were found between other RPRs and age, SE, AL (all P > 0.05).
The basic characteristics of children in low myopia group and pre-myopia group group were shown in Table 2. There were significant differences in SE and AL between groups (both P < 0.001), whereas no significant differences were observed in age or gender (P = 0.575 and P = 0.404, respectively).
The mean values and 95% CI of RPRs of children in low myopia group and pre-myopia group, as well as the differences between both groups were presented in Table 3. All the RPRs were hyperopia in the children with low myopia and pre-myopia, except for RPR-T in pre-myopia group. RPR-I in low myopia group was significantly larger than that in pre-myopia group (0.42 ± 0.72 (95% CI 0.22, 0.62) D vs. 0.04 ± 0.67 (95% CI − 0.17, 0.25) D, P = 0.010). Furthermore, the difference in RPR-T between both groups had a trend toward significance (0.21 ± 0.71 (95% CI 0.01, 0.40) D vs. − 0.09 ± 0.75 (95% CI − 0.33, 0.15) D, P = 0.052). Although there were no significant differences in all the other RPRs between both groups (all P > 0.05) except for RPR-I, all the other RPRs in low myopia group were larger than those in pre-myopia group.
In addition, symmetry of four retinal quadrants was evaluated in low myopia group and pre-myopia group, respectively. In low myopia group, there were significant differences in the four quadrants (P < 0.001). Bonferroni post-hoc test showed that RPR-N was larger than RPR-S (P = 0.005), RPR-I (P = 0.002), RPR-T (P < 0.001). In pre-myopia group, there were also significant differences in the four quadrants (P < 0.001). Bonferroni post-hoc test showed that RPR-N was larger than other three quadrants (all P < 0.001), and RPR-S was larger than RPR-T (P = 0.017).
Discussion
In the present study, RPRs in the children with low myopia and pre-myopia were evaluated using MRT. The majority of RPRs were negatively correlated with SE. All the RPRs were hyperopia in the children with low myopia and pre-myopia, except for RPR-T in pre-myopia group. RPR-I in low myopia group was significantly larger than that in pre-myopia group, and the difference in RPR-T between both groups had a trend toward significance. It was noted that all the RPRs in low myopia group were larger than those in pre-myopia group. In addition, retinal asymmetry was observed both in the children with low myopia and pre-myopia.
In this study, negative correlations of TRPR, RPR-I, RPR-T, RPR-45, RPR-(30–45) and RPR-(15–45) with SE indicated that with SE changing from positive values to negative values, children had greater amount of hyperopic defocus in these retinal regions. Hu et al24 found negative correlations between RPR-S, RPR-T, RPR-(15–30), RPR-(30–45) and spherical equivalent (SE) in Shenzhen school children using MRT. Lu et al17 found that SE negatively correlated with RPR-S, RPR-I, and RPR-N in Chinese school children using MRT. These discrepancies may be due to different SE range (+ 0.75 D ~ − 3.00 D in this study vs. + 3.0 D ~ − 6.0 D in Hu’s study vs. + 0.5 D ~ − 10 D in Lu’s study) and age span (6–14 yearsd in this study vs. 10–13 years Hu’s study vs. 5–18 years in Lu’s study) between these studies. However, no significant association between RPR-15, RPR-30 and RPR-(15–30) with SE were observed, which were consistent with the findings of Lu and co-workers17. These results suggested RPR in the visual field of 30° centered on the macular fovea maybe have little effect on the myopia development. There was also no correlation between RPR at the temporal 30° position and SE in Japanese myopic children using an open-field autorefractor FR-500025.
Furthermore, there was no significant association between RPR and age in this study. This was similar to the finding of Atchison et al.26 Peripheral refraction was similar with the same central refraction between young persons group and old persons group using a Shin-Nippon SRW5000 autorefractor26. However, Li et al12 found that the 14 years children had more relative hyperopia than the 7 years children, especially in the temporal region. Chen et al10 found that adult myopic individuals had more peripheral relative hyperopia than children. This suggested that age may be an influencing factor for peripheral refraction. The peripheral refraction gradually increased with age, which maybe remain in a relatively stable state in adulthood. The small sample size and age span in this study may not reflect this trend. In addition, The discrepancy may be due to ethnicity9,27.
In this study, TRPR of children in low myopia group and pre-myopia group were 0.52 ± 0.62 D and 0.32 ± 0.41 D, respectively, which was consistent with the results of children measured by MRT in previous studies17,28. The increasing trend of RPR with SE from pre-myopia to low myopia was similar to the finding of Lu and co-workers17. Lu et al17 found that the majority of RPRs measured by MRT were hyperopia among emmetropia group, low myopia group and moderate myopia group, with the moderate myopia group the highest RPR on the whole. However, Lan et al29 found that pattern of peripheral retinal defocus was similar in the majority of emmetropic Chinese children with an open-view Hartmann-Shack wavefront sensor, and more than 70% of the children had a nearly flat horizontal refraction with a slightly myopic shift in the superior retina. Retinal relative peripheral refraction in the rectangular 60 × 36° range was measured in the study of Lan and co-workers29, whereas circular retinal relative peripheral refraction in the 53° range centered on the macular fovea was measured in the present study. Thus peripheral refraction can not be compared directly due to the different detection area ranges among different studies.
In this study, all the RPRs were hyperopia in the children with low myopia and pre-myopia, except for RPR-T in pre-myopia group. Li et al12 found that myopic children have relative peripheral hyperopia, while hyperopic and emmetropic children have relative peripheral myopia in Chinese children with 7 and 14 years using WAM-5500. Chen et al10 found peripheral hyperopia in the myopia group and peripheral myopia in the hyperopia group, while the peripheral refraction in the emmetropia group was similar to the macular fovea in children and adults using a Shin-Nippon auto-refractor. Sng et al11 measured the peripheral refraction of 15° and 30° at the nasal and temporal visual fields in Singaporean Chinese children using WAM-5500. Compared with the central refraction, children with moderate-high myopia had relative hyperopia at all peripheral eccentricities, and children with low myopia had relative hyperopia only at the temporal and nasal 30°, whereas children with emmetropia and hyperopia had peripheral relative myopia at all eccentricities11. In the above studies, only the relative peripheral refraction at a few points on the retinal horizontal and/or vertical meridian were studied, which can not fully understand the relationship between the retinal regional peripheral refraction and myopia.
Furthermore, RPR-I in low myopia group was significantly larger than that in pre-myopia group. All the other RPRs in low myopia group were larger than those in pre-myopia group, although without significant differences. The difference in RPR-T between both groups had a trend toward significance in this study. Lu et al17 found that RPR-I, RPR-N and RPR-(30–45) were larger in low myopia group than that in emmetropia group, whereas RPR-15 and RPR-(15–30) were smaller in low myopia group than that in emmetropia group after cycloplegia using MRT. Wu et al30 found that only RPR-T in myopia group (− 10 D ≤ SE ≤ − 0.50 D) was significantly larger than that in emmetropia group after cycloplegia using MRT at West China Hospital, Sichuan University. Hu et al24 found that there were significant differences of RPR-S and RPR-T in Shenzhen school children between low myopia group and emmetropia group under natural pupil without cycloplegia using MRT. It should be noted that the RPR measurements are influenced by multiple factors. Cycloplegia31 and decreased illumination32 can lead to a significant hyperopic shift of RPR with an increase in eccentricity. Pre-myopia is an important peroid before the onset of myopia. Children with myopia had greater peripheral hyperopia defocus before developing myopia9,11. However, a 2-years longitudinal study demonstrated that relative peripheral hyperopia did not predict development nor progression of myopia in Chinese children aged 7 and 14 years33. The relationship between relative peripheral hyperopia and myopia development in children need to be confirmed in future study.
In this study, RPR-N was larger than RPR-S, RPR-I and RPR-T in low myopia group, whereas RPR-N was larger than other three quadrants, and RPR-S was larger than RPR-T in pre-myopia group. The results demonstrated the asymmetry in the posterior visual field in low myopia group and pre-myopia group. The characteristic of retinal morphology was similar to the finding of Osuagwu and co-workers34. Osuagwu et al34 found considerable nasal-temporal asymmetry for hyperopes and emmetropes, and superior-inferior asymmetry for hyperopes in Australian adults using a COAS-HD Hartmann-Shack aberrometer. However, Lin et al35 found symmetrical peripheral refraction in the nasal and temporal retina in myopic children using a custom Hartmman-Shack wavefront sensor. Tabernero et al36 found that the peripheral retinal morphology of low myopia was more irregular compared with emmetropia using a scanning photorefractor. In the future, the correlation between retinal peripheral refraction and morphology can be further explored by 3D MRI.
There may be several limitations in this study. Firstly, the sample size in this study was small. Secondly, the range of + 0.75 D ~ − 3.0 D of SE in this study was narrow, whereas moderate and high myopia were not included. However, children without cylinder power in this study can avoid some interference effect of ocular astigmatism on peripheral refraction. Thirdly, the angle kappa was not measured in this study, so the difference between the anatomical and optical axis and its potential effect on PRP were not analyzed. Finally, this study was a cross-sectional observation and could not explain the causal relationship between peripheral refraction and myopia.
In conclusion, RPRs become more hyperopia with the changing trend from pre-myopia to myopia. Children with low myopia and pre-myopia have relative peripheral hyperopia. Furthermore, children with low myopia have larger relative peripheral hyperopia compared with pre-myopia. Longitudinal prospective studies are required to provide further insight into the relationship between RPR and myopia development and progression.
Data availability
Data are available upon request from the corresponding author.
References
Baird, P. N. et al. Myopia. Nat. Rev. Dis. Primers 6(1), 99 (2020).
Morgan, I. G. et al. The epidemics of myopia: Aetiology and prevention. Prog. Retin. Eye Res. 62, 134–149 (2018).
Holden, B. A. et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 123(5), 1036–1042 (2016).
Bourne, R. et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: A systematic review and meta-analysis. Lancet Glob. Health 5(9), e888–e897 (2017).
Jiang, Y. et al. Visual impairment in highly myopic eyes: The ZOC-BHVI high myopia cohort study. Clin. Exp. Ophthalmol. 48(6), 783–792 (2020).
Hoogerheide, J., Rempt, F. & Hoogenboom, W. P. Acquired myopia in young pilots. Ophthalmologica 163(4), 209–215 (1971).
Mutti, D. O., Sholtz, R. I., Friedman, N. E. & Zadnik, K. Peripheral refraction and ocular shape in children. Invest. Ophthalmol. Vis. Sci. 41(5), 1022–1030 (2000).
Atchison, D. A., Pritchard, N. & Schmid, K. L. Peripheral refraction along the horizontal and vertical visual fields in myopia. Vis. Res. 46(8–9), 1450–1458 (2006).
Mutti, D. O. et al. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Invest. Ophthalmol. Vis. Sci. 48(6), 2510–2519 (2007).
Chen, X. et al. Characteristics of peripheral refractive errors of myopic and non-myopic Chinese eyes. Vis. Res. 50(1), 31–35 (2010).
Sng, C. C. et al. Peripheral refraction and refractive error in Singapore Chinese children. Invest. Ophthalmol. Vis. Sci. 52(2), 1181–1190 (2011).
Li, S. M. et al. Peripheral refraction in 7- and 14-year-old children in central China: The anyang childhood eye study. Br. J. Ophthalmol. 99(5), 674–679 (2015).
Verkicharla, P. K., Suheimat, M., Schmid, K. L. & Atchison, D. A. Peripheral refraction, peripheral eye length, and retinal shape in myopia. Optom. Vis. Sci. 93(9), 1072–1078 (2016).
Romashchenko, D., Rosen, R. & Lundstrom, L. Peripheral refraction and higher order aberrations. Clin. Exp. Optom. 103(1), 86–94 (2020).
VanderVeen, D. K. et al. Use of orthokeratology for the prevention of myopic progression in children: A report by the American Academy of Ophthalmology. Ophthalmology 126(4), 623–636 (2019).
Zhang, H. et al. Myopia control effect is influenced by baseline relative peripheral refraction in children wearing defocus incorporated multiple segments (DIMS) spectacle lenses. J. Clin. Med. 11(9), 25 (2022).
Xiaoli, L. et al. Comparative study of relative peripheral refraction in children with different degrees of myopia. Front. Med. (Lausanne) 9, 800653 (2022).
Ni, N. J. et al. Novel application of multispectral refraction topography in the observation of myopic control effect by orthokeratology lens in adolescents. World J. Clin. Cases 9(30), 8985–8998 (2021).
Lu, W. et al. Agreement and repeatability of central and peripheral refraction by one novel multispectral-based refractor. Front. Med .(Lausanne) 8, 777685 (2021).
Zheng, X. et al. Relationship between peripheral refraction in different retinal regions and myopia development of young Chinese people. Front. Med. (Lausanne) 8, 802706 (2021).
Flitcroft, D. I. et al. IMI—Defining and classifying myopia: A proposed set of standards for clinical and epidemiologic studies. Invest. Ophthalmol. Vis. Sci. 60(3), M20-30 (2019).
He, X. et al. Effect of repeated low-level red light on myopia prevention among children in China with premyopia: A randomized clinical trial. JAMA Netw. Open 6(4), e239612 (2023).
Xu, X., Zang, W., Wang, A. & Yang, C. Repeatability and agreement of multispectral refraction topography in school children before and after cycloplegia. Biomed. Eng. Online 23(1), 110 (2024).
Hu, H. L. et al. Relative peripheral refraction in school children with different refractive errors using a novel multispectral refraction topographer. Int. J. Ophthalmol. 17(8), 1477–1482 (2024).
Furuse, T., Hasebe, S. & Tokutake, T. Peripheral refraction in Japanese schoolchildren with low to moderate myopia. Jpn. J. Ophthalmol. 66(1), 74–80 (2022).
Atchison, D. A., Pritchard, N., White, S. D. & Griffiths, A. M. Influence of age on peripheral refraction. Vis. Res. 45(6), 715–720 (2005).
Kang, P. et al. Peripheral refraction in different ethnicities. Invest. Ophthalmol. Vis. Sci. 51(11), 6059–6065 (2010).
Li, T., Chen, Z., She, M. & Zhou, X. Relative peripheral refraction in myopic children wearing orthokeratology lenses using a novel multispectral refraction topographer. Clin. Exp. Optom. 106(7), 746–751 (2023).
Lan, W., Lin, Z., Yang, Z. & Artal, P. Two-dimensional peripheral refraction and retinal image quality in emmetropic children. Sci. Rep. 9(1), 16203 (2019).
Wu, D. W. et al. Refraction difference value variations in children and adolescents with different refractive errors. Int. J. Ophthalmol. 17(12), 2236–2242 (2024).
Lu, W. et al. The influence of accommodation on retinal peripheral refraction changes in different measurement areas. J. Ophthalmol. 2023, 5553468 (2023).
Marcellan, V. M., Remon, L. & Avila, F. J. Peripheral refraction under different levels of illuminance. Ophthal. Physiol. Opt. 44(1), 191–198 (2024).
Atchison, D. A. et al. Relative peripheral hyperopia does not predict development and progression of myopia in children. Invest. Ophthalmol. Vis. Sci. 56(10), 6162–6170 (2015).
Osuagwu, U. L., Suheimat, M. & Atchison, D. A. Peripheral aberrations in adult hyperopes, emmetropes and myopes. Ophthal. Physiol. Opt. 37(2), 151–159 (2017).
Lin, Z. et al. Two-dimensional peripheral refraction and retinal image quality in orthokeratology lens wearers. Biomed. Opt. Express 11(7), 3523–3533 (2020).
Tabernero, J. & Schaeffel, F. More irregular eye shape in low myopia than in emmetropia. Invest. Ophthalmol. Vis. Sci. 50(9), 4516–4522 (2009).
Acknowledgements
This study was sponsored by Shanghai Municipality Health Bureau Project (202240058). We thanks all the children in this study.
Author information
Authors and Affiliations
Contributions
TL and XDZ designed the study. TL and BJ collected data. TL analyzed data. TL, BJ and XDZ drafted the manuscript, and all authors revised and finally approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, T., Jiang, B. & Zhou, X. Assessment of relative peripheral refraction in children with low myopia and pre-myopia using multispectral refraction topography. Sci Rep 15, 21361 (2025). https://doi.org/10.1038/s41598-025-04334-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04334-4