Abstract
Serratus anterior plane block (SPB) as a regional anesthesia technique is used for analgesia in modified radical mastectomy (MRM). The new serratus anterior plane (SAP) block is a novel approach that has been described recently. This study aimed to elucidate the effectiveness and safety of SAP block for pain management after MRM and compare the analgesic effects of SPB and SAP block with those of a control group during the postoperative period of MRM. In a prospective randomized controlled trial, sixty patients (n = 60) who underwent MRM surgery received either SPB or SAP block analgesia. The primary endpoint was the visual analog scale (VAS) score (at rest or with movement) at 2 h after MRM. The secondary outcomes were VAS scores at different time points (6, 12, 24 h) after MRM, stress hormone levels, and the consumption of opioid analgesics during the surgery. Sixty subjects were enrolled. The VAS scores with movement at 2 h postoperation were significantly lower in the SAP group than in the SPB group (P = 0.027). The patients in the SAP and SPB groups had lower VAS scores compared with the Control group at 2 and 6 h after MRM, both at rest and with movement (P < 0.001). The SPB and SAP blocks significantly reduced the consumption of opioid analgesics during surgery compared with the control group (P < 0.001). This study revealed that both SPB and SAP blocks had good postoperative analgesic effects on modified radical mastectomy surgery, reduced the consumption of opioids, and decreased the stress response during surgery compared with the control group. Compared with SPB, the SAP block may have better analgesic effects during the early postoperative period of modified radical mastectomy surgery.
Trial registration: This study was registered in the Chinese Clinical Trial Registry (Date of Registration: 08/08/2021, registration number: ChiCTR2100049692).
Similar content being viewed by others
Introduction
Breast cancer is the most common cancer among women accounting for 30% of new female cancer cases in 20211. Surgery is the first and most effective therapy for breast cancer. Modified radical mastectomy (MRM), which associated with an axillary lymph node dissection or sentinel lymph node biopsy, is a widely used surgical procedure. A significant clinical problem in which more than half of breast cancer patients complain of moderate to severe pain after surgery should be taken seriously2,3. Severe postoperative pain has a significant negative impact on patient’s quality of life.
Pectoral nerve (PECS) blocks, including PECS I and II and serratus plane blocks, have provided adequate analgesia for MRM4. PECS II is the modified PECS I, and it infiltrates the interfascial planes between the pectoralis major and minor and between the pectoralis minor and serratus anterior with local anesthetic5,6. Blanco proposed a serratus anterior plane block (SPB) to inject the local anesthetic into the plane superficial to the serratus muscle7. In 2019, Franco et al. proposed a novel analgesic technique that is thought to consolidate PECS and SPB into a single thoracic fascial plane block: the new serratus anterior plane (SAP) block8. In this new block, a certain amount of local anesthetic was placed into the plane between the lateral border of the pectoralis major and the serratus anterior to block the lateral cutaneous branches of the intercostal nerves, the long thoracic nerve, and the thoracic dorsal nerve.
SPB is considered an alternative to paravertebral block because of its safe and easy operation and adequate analgesia. It has been widely used clinically in breast surgery, rib fracture, thoracoscopic surgery, and thoracotomy9,10,11,12. A prospective randomized controlled trial has shown that SAP block provides analgesia after MRM surgery13, but its efficiency remains unproven; no clinical trial has compared SAP block with SPB. This study aimed to further elucidate the effectiveness and safety of SAP block for pain after MRM and compare the results with those of SPB.
Method
This research was a prospective randomized controlled clinical trial conducted at the First College of Clinical Medical Science, China Three Gorges University, Yichang Central People’s Hospital, Hubei, China, after receiving approval from the Research Ethics Board and registering with the Chinese Clinical Trial Registry (Date of Registration: 08/08/2021, registration number: ChiCTR2100049692). We confirm that all experiments were performed by the Declaration of Helsinki, and informed consent was obtained from all participants or their legal guardians.
The inclusion criteria were women aged 18–65 years, with an American Society of Anesthesiologists physical status of 1–2, a body mass index (BMI) of 35 kg/m2 or less, and undergoing unilateral MRM under general anesthesia. In addition, surgery was scheduled at 8 am and involved an operation duration of less than 4 h. The exclusion criteria were BMI > 35 kg/m2, allergy to local anesthetics, contraindication to regional anesthesia, pre-existing infection at the block site; chronic pain or history of opioid abuse, history of diseases such as hypertension, heart disease, diabetes, and history of long-term use of drugs related to hormone levels.
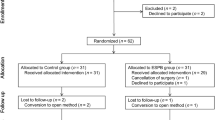
All patients provided written informed consent to participate. Using the computer-generated random number tables, 69 subjects were randomly divided into three groups: the SAP group, the SPB group, and the control group (C group). The results of group allocation were concealed in numbered and sealed opaque envelopes. These envelopes were opened by a nurse, whereas an experienced anesthesiologist performed the corresponding block.
All the subjects underwent standardized monitoring after arriving in the operating room. We used ultrasound in all the instances in the study groups (SonoSite M-Turbo, USA), with a high-frequency linear ultrasound probe (6–13 MHz). The patients were placed in the supine position, with the arm abducted at 90°, and the puncture site skin was sterilized with 1% povidone-iodine.
The SAP blocks were prepared by an experienced clinical professor. The ultrasound probe was placed obliquely over the anterior chest at the position of the fourth rib (Fig. 1a) to identify the fourth to fifth ribs, the pectoralis major, and the serratus anterior. The block needle was inserted via an in-plane technique from medial to lateral until the needle tip (80 mm, 21 gauge) was positioned in the fascial plane between the end of the pectoralis major and the serratus anterior muscle (Fig. 1c). Then, 20 ml of 0.375% ropivacaine was injected into the target interfascial plane after confirming that the needle tip was in the designated position with 3 ml of saline and ensuring negative aspiration.
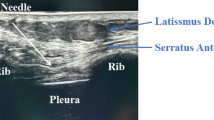
The same investigator installed the SPB blocks. The ultrasound probe was placed on the upper chest of the affected side in the sagittal plane (Fig. 1b), with the probe moving inferiorly and laterally until the fourth and fifth ribs, latissimus dorsi, and serratus muscles were located (Fig. 1d). After the block needle was inserted via the in-plane technique and 3 ml of saline was confirmed such that the needle tip was located in the plane between the serratus anterior and latissimus dorsi, 20 ml of 0.375% ropivacaine was administered into this gap.
The sensation of pain and warmth were assessed every 5 min for 30 min after completion of the blocks. We evaluated the sensory block by “cold testing” and applied it to the breast areas with a cotton swab dipped in alcohol, in contrast to the contralateral breast (scale from 0 to 2, 0 = no block; 1 = diminished sensation; 2 = no sensation). For the analgesia assessment, a toothpick was applied to the skin of the affected breast and compared with the other side (scale from 0 to 2, 0 = no block; 1 = unsharp pinprick; 2 = no sensation). A block was regarded as successful if both scores were greater than 1.
The patients in the C group received standard general anesthesia without block intervention. Patients in the test groups received general anesthesia after successful blocking. General anesthesia was induced using propofol (2 mg kg−1), midazolam (0.04 mg kg−1), sufentanil (0.4 µg kg−1), rocuronium (0.6 mg kg−1), and lidocaine (1.5 mg kg−1) for the application of endotracheal intubation. After confirming the tube position, volume-controlled ventilation was performed, and the tidal volume and respiratory rate were adjusted to maintain the end-tidal CO2 within 35–45 mmHg. Intraoperative continuous infusion of propofol, remifentanil, and cisatracurium was performed to maintain anesthesia. Intravenous sufentanil (0.1 µg kg−1) for perioperative analgesia was administered when the mean arterial blood pressure (MAP) or heart rate (HR) increased by ≥ 20% from the baseline measurement. The bispectral index was maintained in the range of 40–60 intraoperatively. A total of 5 mg tropisetron was administered to all patients to prevent postoperative nausea and vomiting (PONV), and sufentanil (0.1 µg kg−1) was applied to improve postoperative pain. Propofol and remifentanil were discontinued at the end of the surgery, and muscle relaxation was reversed if necessary. All patients were sent to the postanesthetic care unit. After surgery, the visual analog scale (VAS, scale from 0 to 10, 0 = no pain; 10 = extreme pain) scores and the need for rescue analgesia (flurbiprofen 1 mg kg−1) were recorded when the VAS score was > 4.
Outcomes
We collected general clinical data such as age, height, weight, and the side affected preoperatively. The study’s primary endpoint was the VAS scores (at rest or with movement) at 2 h after MRM. The secondary outcomes were VAS scores at different time points (6, 12, 24 h) after MRM, stress hormone levels, and the consumption of opioid analgesics during the surgery. We recorded the MAP and HR at five time points: before anesthesia (T0, baseline), before intubation (T1), skin incision (T2), 30 min after skin incision (T3), and 10 min after extubation (T4). Three blood samples were collected to measure the serum cortisol (Cor), norepinephrine (NE), and blood glucose (Glu) levels at T0, T2, and T4. We recorded the consumption of propofol, remifentanil, and sufentanil during surgery. In addition, the rate of PONV and the rescue analgesia within 24 h after surgery were recorded.
The sample size was calculated based on our pre-experimental results. Substitute the pre-experimental grouping mean in VAS scores at 2 h postoperatively between groups, with a standard deviation of 2.0. Using G*Power 3.1 version (University of Dusseldorf, Germany), a sample size of 18 subjects per group was estimated to detect such a difference with 80% power at an alpha level of 0.05. To account for potential dropouts, we planned to include 20 patients in each group.
All data were analyzed using SPSS Version 26.0 (IBM Corporation, USA). The normality of continuous outcome distributions was assessed with the Shapiro–Wilk test. Normally distributed continuous outcomes are presented as the mean ± standard deviation (SD), while group comparisons were conducted using One–Way Analysis of Variance and the Least Significant Difference post hoc test. Non-normally distributed data were described as medians (25th–75th percentiles), with group comparisons performed via the Kruskal–Wallis test and Dunn–Bonferroni post hoc test. Data for qualitative variables are presented as counts (percentages) and analyzed through the chi-square test.
Results
Figure 2 presents the CONSORT diagram of the enrollment process. A total of 69 participants were assessed for eligibility; 6 refused, 63 were recruited and randomized, 2 were excluded due to block failure, and 1 was excluded for severe anaphylaxis after induction. The data from the 60 subjects were analyzed, and the demographic parameters and characteristics of the surgical interventions were comparable between the groups (Table 1).
Compared with those in the C group, the VAS scores at rest and with movement at 2 and 6 h postoperation were significantly lower in the SAP and SPB groups (P < 0.001), and the VAS scores at movement at 2 h postoperation were significantly lower in the SAP group than in the SPB group (P = 0.027 < 0.05) (Table 2). The consumption of sufentanil, remifentanil, and propofol during surgery was decreased in the SAP and SPB groups compared with the control group (P < 0.001), and no statistically significant difference was recorded between the SAP and SPB groups (P > 0.05) (Table 3, Supplementary material Table 5). A significantly greater incidence of PONV and rescue analgesia within 24 h after surgery were observed in the C group than in the SAP and SPB groups (P < 0.01) (Table 3). In addition, the extubation time was significantly shorter in the SAP and SPB groups than in the C group (P < 0.001), and no significant difference was recorded between the SAP and SPB groups (P > 0.05) (Table 3).
Statistically insignificant differences were observed among the MAP of the three groups at the points T0 (baseline), T1, and T3, whereas a significantly lower MAP was observed in the SAP and SPB groups at T2 and T4 compared with the C group (P < 0.05). No significant difference in the MAP was detected between the SAP group and the SPB group (P > 0.05) (Fig. 3A). The HR did not differ among patients in the three groups at any time point (P > 0.05) (Fig. 3B, Supplementary material Table 1).
Mean arterial blood pressure (A) and heart rate (B) changes in the three groups at different time points. SAP: new serratus anterior plane; SPB: Serratus anterior plane block; T0: before anesthesia; T1: before intubation; T2: skin incision; T3: 30 min after skin incision; T4: 10 min after extubation. *P < 0.05 for the SPB group versus the C group. #P < 0.05 for the SAP group versus the C group.
Compared with those in the C group, the serum Cor and NE levels were lower at T2 and T4 in the SAP and SPB groups (P < 0.001), and there was no difference between the SAP and SPB groups (P > 0.05) (Fig. 4A,B, Supplementary material Table 2 and Table 3). Moreover, the Glu levels in the C group were dramatically higher than those in the SAP and SPB groups at T4 (P < 0.001), whereas the difference between the SAP and SPB groups was not significant (P > 0.05) (Fig. 4C, Supplementary material Table 4).
Changes in serum Cor (A), NE (B), and Glu (C) levels in the three groups at different time points. SAP: new serratus anterior plane; SPB: Serratus anterior plane block; Cor: serum cortisol. NE: serum norepinephrine. Glu: blood glucose. T0: before anesthesia; T2: skin incision; T4: 10 min after extubation. *P < 0.05 for the SPB group versus the C group. #P < 0.05 for the SAP group versus the C group.
Discussion
This prospective, randomized controlled study investigated the analgesic efficacy and safety of SPB versus SAP block in MRM surgery. Our findings showed that SPB and SAP blocks provided superior analgesia in the early postoperative period compared with the control group. In addition, SPB and SAP blocks reduced the consumption of opioid analgesics, inhibited the stress response, and facilitated postoperative recovery compared with the control group. Compared with the SPB, the SAP block reduces the VAS score with movement at 2 h post-surgery.
Patients post-MRM surgery are frequently associated with acute pain and PONV, whereas regional anesthesia has been explored to alleviate postoperative pain and improve patient prognosis14,15. The thoracic paravertebral nerve block is regarded as a feasible option for classical multimodal analgesia because it benefits postoperative analgesia; however, the difficulty of the operation and severe complications may contribute to the low utilization of this block16,17. The SPB improves postoperative pain after MRM surgery by infiltrating the lateral cutaneous branches of intercostal nerves, the long thoracic nerve, and the thoracic dorsal nerve18,19,20. After Blanco5,7 proposed the PECS blocks and SPB, Franco8 presented the SAP block, which attempts to consolidate all three blocks into one thoracic fascial plane block. Compared with SPB, the SAP block is injected closer to the target nerve and avoids the risk of damaging the long thoracic nerve and the vessels around it. Given that SPB and SAP blocks are superficial blocks, we can identify the relevant anatomical structures under ultrasound and reduce the incidence of complications, such as damage to blood vessels and nerves, during the puncture process. We selected 20 ml of 0.375% ropivacaine for injection, which can achieve a certain analgesic effect while avoiding the systemic toxicity of local anesthetics21,22.
Previous studies have reported that SPB and SAP block can improve postoperative analgesia and reduce opioid requirements during the perioperative period13,23,24, which is similar to the results of this study. To our knowledge, this research is the first study to compare SPB with SAP blocks. We observed that the SAP block provided better analgesia when moving the upper arm at 2 h after surgery, probably because the SAP block was closer to the target nerve and better infiltrated the intercostobrachial nerve that innervates the axillary tail of the breast, axilla, and upper medial arm6,25.
Regional anesthesia inhibits the stress response to surgery. It involves several hormonal changes, such as changes in cortisol and catecholamine levels, that can influence postoperative outcomes through beneficial effects on organ function26. Similar to previous studies in which the regional blocks can reduce the stress response to surgical trauma in MRM procedures13,27. Our study revealed that SPB and SAP blocks reduce stress hormone levels during the skin incision and postoperative periods compared with the control group. The serum Glu levels were significantly lower in the SPB and SAP groups than in the control group after surgery. At the time of skin incision, the Glu level in the SPB and SAP groups was lower than that in the control group, but this difference was not statistically significant. In contrast, no significant differences in the serum Cor, NE, or Glu levels were detected between the SAP and SPB groups.
However, this study has several limitations. (1) The results were derived from a single center, and the small sample size may pose a problem of reduced statistical power and decreased effectiveness of the SAP block. (2) Due to ethical restrictions, no active control intervention was conducted on the block with saline. This situation introduced a risk of bias in the subsequent stages of the trial. (3) To evaluate the success of the block, we administered it while the patients were awake, and this invasive procedure may have induced anxiety among the patients. Moreover, performing these procedures while the patients were awake compromised the study’s ability to be fully double-blinded. (4) Although we confirmed that all subjects underwent MRM surgery, the area blocked with the SPB or SAP block alone may not have encompassed the entire surgical area of the breast, leading to potential bias in the analysis. (5) In this study, to ensure homogeneity of the study population and minimize confounding factors, we excluded patients with comorbidities based on the inclusion criteria. This may introduce sample selection bias, limiting the universality and applicability of the research results.
In conclusion, our study further elucidates the effectiveness and safety of SAP block for pain management after MRM. It revealed that both SPB and SAP blocks provide significant analgesic effects post-MRM surgery, reduce opioid analgesic consumption, and decrease the stress response during surgery compared to the control group. Additionally, in contrast to SPB, the SAP block may offer superior analgesic effects in the early postoperative period following MRM surgery. Anesthetists can choose either the SPB or SAP block based on their personal preferences and clinical experiences.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Change history
06 August 2025
The original online version of this Article was revised: In the original version of this Article, Ruizhen Gao was incorrectly affiliated with ‘Department of Anesthesiology, Wuhan Third Hospital, Wuhan, 430074, China.’ Their correct affiliation is ‘Department of Anesthesiology, The First College of Clinical Medical Science, China Three Gorges University, Yichang Central People’s Hospital, 2 Jiefang Road, Xiling District, Yichang City, Hubei, China.’ The original Article has been corrected.
Abbreviations
- BMI:
-
Body mass index
- Cor:
-
Cortisol
- Glu:
-
Glucose
- HR:
-
Heart rate
- MAP:
-
Mean arterial blood pressure
- MRM:
-
Modified radical mastectomy
- NE:
-
Norepinephrine
- PECS:
-
Pectoral nerve
- PONV:
-
Postoperative nausea and vomiting
- SAP:
-
New serratus anterior plane
- SPB:
-
Serratus anterior plane block
- VAS:
-
Visual analog scale
References
Siegel, R. L., Miller, K. D., Fuchs, H. E. & Jemal, A. Cancer statistics, 2021. CA Cancer J. Clin. 71(1), 7–33. https://doi.org/10.3322/caac.21654 (2021).
Fecho, K. et al. Acute and persistent postoperative pain after breast surgery. Pain Med. 10(4), 708–715. https://doi.org/10.1111/j.1526-4637.2009.00611.x (2009).
Habib, A. S., Kertai, M. D., Cooter, M., Greenup, R. A. & Hwang, S. Risk factors for severe acute pain and persistent pain after surgery for breast cancer: A prospective observational study. Reg. Anesth. Pain Med. 44(2), 192–199. https://doi.org/10.1136/rapm-2018-000040 (2019).
Grape, S., Jaunin, E., El-Boghdadly, K., Chan, V. & Albrecht, E. Analgesic efficacy of PECS and serratus plane blocks after breast surgery: A systematic review, meta-analysis and trial sequential analysis. J. Clin. Anesth. 63, 109744. https://doi.org/10.1016/j.jclinane.2020.109744 (2020).
Blanco, R. The, “pecs block”: A novel technique for providing analgesia after breast surgery. Anaesthesia 66(9), 847–848. https://doi.org/10.1111/j.1365-2044.2011.06838.x (2011).
Robinson, H. et al. Anatomical evaluation of a conventional pectoralis II versus a subserratus plane block for breast surgery. Anesth. Analg. 131(3), 928–934. https://doi.org/10.1213/ANE.0000000000005039 (2020).
Blanco, R., Parras, T., McDonnell, J. G. & Prats-Galino, A. Serratus plane block: A novel ultrasound-guided thoracic wall nerve block. Anaesthesia 68(11), 1107–1113. https://doi.org/10.1111/anae.12344 (2013).
Franco, C. D. & Inozemtsev, K. Refining a great idea: the consolidation of PECS I, PECS II and serratus blocks into a single thoracic fascial plane block, the SAP block. Reg. Anesth. Pain Med. 1, 1. https://doi.org/10.1136/rapm-2019-100745 (2019).
De Cassai, A. et al. Serratus anterior plane block for video-assisted thoracoscopic surgery: A meta-analysis of randomised controlled trials. Eur. J. Anaesthesiol. 38(2), 106–114. https://doi.org/10.1097/EJA.0000000000001290 (2021).
Jack, J. M., McLellan, E., Versyck, B., Englesakis, M. F. & Chin, K. J. The role of serratus anterior plane and pectoral nerves blocks in cardiac surgery, thoracic surgery and trauma: A qualitative systematic review. Anaesthesia 75(10), 1372–1385. https://doi.org/10.1111/anae.15000 (2020).
Beard, L. et al. Multicenter longitudinal cross-sectional study comparing effectiveness of serratus anterior plane, paravertebral and thoracic epidural for the analgesia of multiple rib fractures. Reg. Anesth. Pain Med. 45(5), 351–356. https://doi.org/10.1136/rapm-2019-101119 (2020).
Chai, B. et al. Research progress on serratus anterior plane block in breast surgery: A narrative review. Pain Ther. 12(2), 323–337. https://doi.org/10.1007/s40122-022-00456-z (2023).
Tang, W. et al. Application of a new serratus anterior plane block in modified radical mastectomy under ultrasound guidance: A prospective, randomized controlled trial. J. Clin. Anesth. 74, 110377. https://doi.org/10.1016/j.jclinane.2021.110377 (2021).
Vingan, P. S. et al. Reducing disparities: regional anesthesia blocks for mastectomy with reconstruction within standardized regional anesthesia pathways. Ann. Surg. Oncol. 31(6), 3684–3693. https://doi.org/10.1245/s10434-024-15094-2 (2024).
Agarwal, R. R. et al. Single-injection thoracic paravertebral block and postoperative analgesia after mastectomy: A retrospective cohort study. J. Clin. Anesth. 27(5), 371–374. https://doi.org/10.1016/j.jclinane.2015.04.003 (2015).
Albi-Feldzer, A., Duceau, B., Nguessom, W. & Jayr, C. A severe complication after ultrasound-guided thoracic paravertebral block for breast cancer surgery: Total spinal anaesthesia: A case report. Eur. J. Anaesthesiol. 33(12), 949–951. https://doi.org/10.1097/EJA.0000000000000536 (2016).
Pace, M. M. et al. Ultrasound-guided thoracic paravertebral blockade: A retrospective study of the incidence of complications. Anesth. Analg. 122(4), 1186–1191. https://doi.org/10.1213/ANE.0000000000001117 (2016).
Mazzinari, G. et al. Interfascial block at the serratus muscle plane versus conventional analgesia in breast surgery: A randomized controlled trial. Reg. Anesth. Pain Med. 44(1), 52–58. https://doi.org/10.1136/rapm-2018-000004 (2019).
Yao, Y., Li, J., Hu, H., Xu, T. & Chen, Y. Ultrasound-guided serratus plane block enhances pain relief and quality of recovery after breast cancer surgery: A randomised controlled trial. Eur. J. Anaesthesiol. 36(6), 436–441. https://doi.org/10.1097/EJA.0000000000001004 (2019).
Mayes, J. et al. An anatomical evaluation of the serratus anterior plane block. Anaesthesia 71(9), 1064–1069. https://doi.org/10.1111/anae.13549 (2016).
Kunigo, T., Murouchi, T., Yamamoto, S. & Yamakage, M. Injection volume and anesthetic effect in serratus plane block. Reg. Anesth Pain Med. 42(6), 737–740. https://doi.org/10.1097/AAP.0000000000000649 (2017).
Biswas, A. et al. Serratus plane block: A cadaveric study to evaluate optimal injectate spread. Reg. Anesth. Pain Med. 43(8), 854–858. https://doi.org/10.1097/AAP.0000000000000848 (2018).
Hards, M. et al. The effect of serratus plane block performed under direct vision on postoperative pain in breast surgery. J. Clin. Anesth. 34, 427–431. https://doi.org/10.1016/j.jclinane.2016.05.029 (2016).
Arsalani-Zadeh, R., ElFadl, D., Yassin, N. & MacFie, J. Evidence-based review of enhancing postoperative recovery after breast surgery. Br. J. Surg. 98(2), 181–196. https://doi.org/10.1002/bjs.7331 (2011).
Woodworth, G. E., Ivie, R. M. J., Nelson, S. M., Walker, C. M. & Maniker, R. B. Perioperative breast analgesia: A qualitative review of anatomy and regional techniques. Reg. Anesth. Pain Med. 42(5), 609–631. https://doi.org/10.1097/AAP.0000000000000641 (2017).
Desborough, J. P. The stress response to trauma and surgery. Br. J. Anaesth. 85(1), 109–117. https://doi.org/10.1093/bja/85.1.109 (2000).
Altıparmak, B., Korkmaz Toker, M., Uysal, A. İ, Turan, M. & Gümüş, D. S. Comparison of the effects of modified pectoral nerve block and erector spinae plane block on postoperative opioid consumption and pain scores of patients after radical mastectomy surgery: A prospective, randomized, controlled trial. J. Clin. Anesth. 54, 61–65. https://doi.org/10.1016/j.jclinane.2018.10.040 (2019).
Acknowledgements
Ruizhen Gao and Gang Zhou contributed equally to this work.
Funding
Supported by the Yichang Science and Technology Innovation Fund (Num A22-2-043).
Author information
Authors and Affiliations
Contributions
All authors participated in the design of the experiment, data analysis, compilation and revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gao, R., Zhou, G., Zhu, W. et al. The new serratus anterior plane block is more effective than the SPB block for early postoperative analgesia following modified radical mastectomy surgery. Sci Rep 15, 24281 (2025). https://doi.org/10.1038/s41598-025-04438-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04438-x