Abstract
The study aimed to quantitatively assess functional risks in the medication administration process of elderly inpatients and develop management measures from a holistic system safety perspective. The functional resonance analysis method and decision-making trial and evaluation laboratory (DEMATEL) method were introduced to graphically model the medication administration process in elderly inpatients and identify safety issues affecting the complex interactions of functions. Semi-structured interviews based on the Fit between Individual, task, technology, and environment framework were used to explore medication safety management measures. A total of 18 functional modules were included in the medication process model for elderly inpatients. The DEMATEL results showed that medical order entry accounted for the highest proportion of the medication process, followed by label printing. Patient identification and drug verification, as downstream links, showed high impacts and influence. Among the safety management measures, task-technology fit and technology-individual fit were the most common. In the future, more research on medication management in elderly patients with different levels of care, settings and contexts, such as home and community, is needed. Attention should be paid to the integration and effect of implementing management measures to comprehensively safeguard patient medication safety.
Similar content being viewed by others
Introduction
Nearly one-quarter of hospitalized patients experience at least one adverse event. Among these, adverse drug events (ADEs) were reported to account for 39%, which was the most common type and the most likely to be prevented1. These preventable drug events occurred primarily in older patients, with cardiovascular medications causing the most harm2. The first step to effectively prevent ADEs and ensure patient medication safety is to comprehensively describe the medication administration process in elderly hospitalized patients and understand basic information about the causes and nature of adverse events.
Previous studies have analyzed the root cause of accidents by linearly decomposing ADEs based on traditional accident chain models and assessed influencing factors and medication risks with retrospective chart reviews. These traditional safety analysis methods are usually passive and linear. Thus, they tend to ignore important factors that are not statistically significant and make it difficult to accurately present the overall impact of small changes on the medication process. Since elderly patients are characterized by multi-morbidities and polypharmacy3, which increase the possibility of adverse events in admission and handover, coupled with the interplay of multiple subjects, technologies and links, a comprehensive and integrated safety analysis method is urgently needed to compensate for the deficiencies of the simple linear accident cause theory.
As the complexity of hospital information systems increases, the Safety-II framework has been proposed to complement Safety-1 linear analysis. In contrast to Safety-I, Safety-II argues that safety management should be shifted from ensuring that "as few things go wrong as possible" to ensuring "how things go well."4 In other words, Safety-II looks at how to ensure that things go well most of the time in complex situations, such as acute care settings. In addition, Safety-II is a positive conception of safety management that focuses on success rather than failure and values flexibility and adaptability. This shift in perspective helps to reveal potential positive factors in the system and provides new ideas for improving overall safety.
The functional resonance analysis method (FRAM) is considered an important analytical tool for investigating complex systems under the Safety-II framework4. It emphasizes the key role of variability and adaptability in a system by analyzing dependencies and interactions within the system. Typically, the construction of the FRAM model follows four steps5: (1) identifying and describing functions, (2) determining function variability, (3) aggregating variability, and (4) managing performance variability. Related studies have identified and described functions from a qualitative perspective. For example, Furniss et al. applied the FRAM to describe the process of intravenous infusion and specific manifestations of functional variability in the intensive care unit. However, these studies tend to miss some critical nodes (e.g., drug handover, etc.), rely mostly on subjective judgments in functional variability judgments4, and lack safety barriers to manage and monitor performance variability.
Studies have introduced various approaches to quantitatively assess functional variability to improve the analytical and computational capabilities of FRAM models6. Kaya et al.7 combined FRAM models with Monte Carlo simulation to calculate functional variability in terms of time and accuracy and assess the degree of impact of performance variability. Salehi et al.8 applied the FRAM to the elderly transition process, designed normal and emergency scenarios in combination with reinforcement learning (RL), and identified critical functions by calculating the importance of the functions. However, a review of quantitative FRAM model improvement efforts revealed that methods such as RL are based on historical data to simulate different scenarios, calculating the variability probability. Such methods are effective in identifying high variability functions but are limited in that they deviate from variability itself and ignore risks that low probability events may lead to system failure7. In addition, studies are less likely to explore the impact of regulatory requirements and current controls on functional variability from organizational and environmental perspectives9.
Previous studies have introduced the Decision-making Test and Evaluation Experiment Method (DEMATEL) to compensate for these shortcomings. The DEMATEL is used to deal with experts’ fuzzy judgment of the level of influence between elements and transform fuzzy values into specific quantitative indexes. The method effectively coordinates the differences in expert ratings by analyzing direct and indirect influences between elements. Thus, it improves the objectivity and reasonableness of decision-making results10,11,12. Since experts have their own characteristics in terms of knowledge reserve, skill level, and practical experience, expert weight must be scientifically allocated to ensure the accuracy and reliability of the results.
This study addressed the above limitations by aiming to (i) systematically model the medication process in elderly inpatients using the FRAM model, (ii) improve the DEMATEL to quantitatively assess the interactions of modules, and (iii) propose countermeasures to mitigate patient harm from a holistic perspective.
Methods
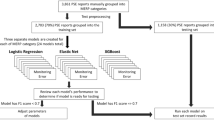
Mixed methods were used in this study to graphically model the entire medication administration process of elderly inpatients from admission to discharge based on the FRAM model. The DEMATEL was introduced to assess functional variability and weight in the entire process. Qualitative interviews were conducted to seek risk measures in conjunction with the quantitative scores of potential risks of the modules.
Setting
The study was conducted in the geriatric cardiology department of a tertiary hospital in Nanjing, Jiangsu Province, China. There were 30 beds in the geriatric cardiology department, with one family member accompanying each patient and one doctor and nurse for every 9–12 patients. All medications in the geriatric cardiology unit were dispensed by the pharmacy and then centrally configured and distributed by the ward nurses. Currently, a mixture of paper and electronic records is used in the department. Information management was applied in admission assessment, medical order entry, drug configuration, medication administration, medication rounds, handover, and discharge. The study was conducted in accordance with the Declaration of Helsinki 2013 and approved by the Jiangsu Province Hospital Ethics Committee (internal ethics committee registration 2024-SR-135). Written informed consent was obtained from all participants included in the study. The study designs and results are described according to the Mixed Methods Appraisal Tool (MMAT) (Supplementary Table S1).
Study design
Participant observation
Participant observation is considered the first method of scientific research and helps researchers penetrate specific situations and scenarios to obtain more information about the workflow and interaction patterns of medical personnel. The researchers participated in clinical work as interns to achieve an in-depth understanding. They directly observed the patient admission assessment, prescription entry, and medication administration processes. A flow chart of medication administration for elderly inpatients was drawn, and the prerequisites to ensure proper execution were summarized. The study graphically modeled each medication administration process based on the FRAM model from six different aspects: input (I), output (O), preconditions (P), resources (R), time (T), and control (C), as shown in Fig. 1.
DEMATEL
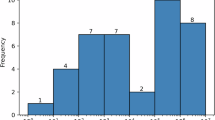
The DEMATEL is a system analysis method based on graph theory. It analyzes logical relationships between elements in the system and identifies key elements based on experts’ ratings. Two head nurses and two quality management members were invited to rate the issues. The function issue degrees range from 0 to 4, with a score of 0 for little or no impact on that function and the next links and a score of 4 indicating that the function is impacted, resulting in the loss of all subsequent functions. Based on the expert’s judgment criteria and familiarity with the issues, the experts ' weights were calculated to be 0.264, 0.236, 0.25, and 0.25, respectively. The degree of impact of an issue was equal to the sum of the expert weight * impact score. The frequency of occurrence of an issue was based on the data from the system and was categorized into levels 1–5, with one issue in more than 5 years designated as level 1 and daily occurrences as level 5. Functional variability is equal to frequency * the degree of impact of the safety issues, as detailed in Eq. (1).
The DEMATEL method contains five brief steps12: (1) experts assess the degree of mutual influence between elements (Eq. 1) using the average method to integrate into direct influence matrix H of group opinion (Eq. 2); (2) normalize the relationship matrix, and obtain canonical direct influence matrix N according to Eq. (3); (3) calculate integrated influence matrix T based on Eq. (4); (4) calculate the influence degree, influenced degree, center degree, and cause degree of each function based on Eq. (5); and (5) convert the influence centrality into influence weight. The larger the weight value, the stronger the influence of the element in the whole system, which is then defined as a key element.
In Eq. (3): \({a}_{ij}\) (i, j = 1,2,…, n) is the degree of influence between functions i and j.
In Eq. (4): I is the unit matrix.
In Eq. (5): \({D}_{i}\) is the degree of influence; \({C}_{i}\) is the degree of being influenced; \({M}_{i}\) is centrality, assessing the importance of the elements; \({R}_{i}\) is the cause degree, assessing the degree of influence between elements; \(d\) is the distance from the element to the origin in the scatter plot, assessing the weight of the element in the system; and \({t}_{ij}\) is the element in the composite influence matrix T.
Interviews
Purposive sampling was used to recruit 10–15 medical personnel in the ward as interviewees. Considering different positions and seniority, the interviewees included at least probationer nurses, charge nurses, dispensary nurses, office nurses, and physicians to ensure the representativeness of the population. Bertaux recommended at least 15 participants in a qualitative study to ensure data adequacy13. However, when newly collected data duplicates existing data, and no new information is provided in the interviews, the data can be considered saturated, and the interview can be stopped14.
A total of 13 participants were included in the study. The basic information is detailed in Table 1. An interview outline was designed by the researchers and developed in consultation with experts (Supplementary Material 2). One-on-one interviews were conducted with the participants by trained project members to refine the medication administration process in elderly inpatients and to summarize safety issues and countermeasures. The interviews were audio-recorded, and the non-verbal behaviors of the participants were recorded.
Data extraction and analysis
In the study, direct observation meant that the project members observed the actual process and recorded it, and document analysis meant that the project members analyzed the data from the system.The conditions for the whole medication administration process in elderly patients were summarized based on the preliminary observation data and graphically modeled using the FRAM Model Visualizer. The FRAM model of the medication process for elderly inpatients was adjusted through interviews with clinical staff to refine the prerequisites, resources, and regulations of each module. At the same time, safety issues and corresponding countermeasures were summarized based on the interview data. After the interviews, the audio files were transcribed verbatim into a manuscript and submitted to two researchers for checking and generating a first draft. Then, the researchers verified the key information with the interviewees to generate a final draft. Prior to formal analysis, the interviews were coded by removing private information according to the order of the interviews. All interview data were imported into NVivo 14.0 software for collation and analysis. Two researchers coded the countermeasures and summarized the frequency of each theme according to the Fit between Individuals, Tasks, Technologies and Environments (FITTE) framework15. Where areas of controversy existed, themes were discussed and identified with the third researcher.
Experts were invited to review the FRAM model again for comprehensiveness and accuracy before formal scoring. The experts’ scores were summarized using Excel 2019 to calculate the variability risk of each function. A direct influence matrix and a comprehensive influence matrix were formed using experts’ scores. An influence-influenced degree scatter plot and centrality-causality scatter plot were drawn to intuitively analyze the importance of each function.
Results
FRAM: medication administration process in elderly inpatients
The medication administration process for elderly inpatients was divided into 18 separate functions based on the FRAM model (Fig. 2), with the six aspects of each function detailed in Supplementary Table S3. Supplementary Table S4 shows the medication safety issues for medical personnel.
Quantitative analysis of system functional risk
First, the experts reviewed the adapted FRAM model of the medication administration process in elderly inpatients. The FRAM model is comprehensive and accurate and facilitates the assessment of functional variability. Second, the interrelationships between functions were quantified based on the experts’ scores (Eq. 1–2), and a direct influence matrix was obtained, as shown in Supplementary Table 5. Finally, the influence, influenced, centrality, cause, and weight of each function were obtained by calculating Eqs. (3–5) (Table 2). The influence-influenced scatterplot and centrality-cause scatterplot were plotted (Supplementary Fig. 6). Table 2 shows that F2 (medical order entry) was the most important in the medication process of elderly inpatients, followed by F8 (label printing) and F14 (patient identification and medication verification).
The two auxiliary lines in Supplementary Fig. 6 indicate the mean degree values of influence and being influenced. The first quadrant indicates that F14 had both high influence and influenced degrees. The two lines in the scatter plots of centrality-cause are the mean of the centrality degree and 0. The modules in quadrant 1 (Supplementary Fig. S6) present high centrality and cause degree, indicating that the function held an important position, with F2 having the principal role, followed by F8 and F7 (check orders). The modules in quadrant 4 were considered outcome elements with equal significance. Among these, F14 played a vital role, followed by F15 (medication round) and F16 (handover).
Risk mitigation measures
Risk mitigation measures were divided into four categories according to the FITTE framework (Table 3), with task-technology fit being the most common, followed by technology-individual fit. The most common measure in task-technology fit was to change the options and settings in the system (n = 13), including adding fields in the order and options in the list. For example, adding fields for target values and the flow rate of high-alert medications in the system facilitated drug verification and the execution of medical orders. The default execution time of standing orders was 8:00 a.m. and 2:00 p.m. Considering the work schedule and performance appraisal, the option of pre-execution time was added to the system interface list.
Changes to the visual display (n = 15) were emphasized in the technology-individual fit, more commonly modifying the information displayed in the interface. During medication administration, charge nurses were often asked by patients about the amount of medication prescribed and the number of unfulfilled orders. However, these must be viewed individually by accessing "Ward Pending Orders" in other modules. Therefore, adding the number of all medication orders and unfulfilled orders to the user interface was an effective measure to simplify complex operations and improve work efficiency. In addition, medical personnel like to customize the alerts according to departmental characteristics and work requirements. Since elderly patients often use cardiovascular medications, which increase the risk of falls, adding alerts for high-alert medication risk assessments would facilitate the transition to a more preventive model of patient safety management.
Discussion
Safety analysis of medication administration in elderly inpatients
This study introduced an improved FRAM to construct a medication administration process model for elderly inpatients, expanding admission assessment, medication withdrawal, handover, and discharge. Semi-structured interviews were used to identify medication safety issues. The coupled roles of each module in the process and the medication safety of elderly patients were quantitatively assessed using the DEMATEL. The medication administration process, in order of importance, was medical order entry, label printing, patient identification, and medication verification (Table 2). Combined with results in the graphs above, the modules of medical order entry and label printing were of high importance as upstream links and had a wide range of influences, whereas patient identification and drug verification, as the last links before patient medication administration, were shown to be susceptible to errors influenced by other modules.
The study found that the order of importance of the medication administration process in elderly patients was similar to that of previous studies, i.e., adverse events occurred mainly in prescribing2 and nursing administration,2,16 while the riskiness of the envisaged admission assessment session was not considerably increased, presumably related to the use of electronic medication management systems (EMMSs). Dabliz et al.17 and Vaghasiya et al.18 confirmed the perceptions in the study, where the use of an integrated EMMS provided the physician with drop-down list options, such as drug name, dosage, and frequency, reducing medication bias associated with handwriting and also reducing the severity of errors. In addition, the assistance of family members was conducive to correcting medication bias due to misinformation conveyed at the time of admission. Considering the characteristics of forgetfulness and visual and hearing impairments in elderly patients, this supports the involvement of family members to facilitate effective medication communication19,20.
Printing, sorting, and gluing labels are given more weight than patient identification and medication verification in the medication administration process for elderly patients, which may be related to incomplete label information, poor layout, and unclear labeling. Related studies investigated indicate that in terms of the comprehensibility and readability of drug labels, users aged 40 and above prefer to increase the font size and color to emphasize key information, especially in clinical departments with heavy medical tasks such as intensive care units21,22. Poorly managed medication labels also mean that nurses put more effort into checking them, or they are likely to be incorrectly labeled and not easily recognized by the system. However, a cross-sectional study found that nurses had poor compliance with double-checking procedures for drug labels23, and 21.5% of infusion bags were unlabeled. Only 8.3% of infusion labels had basic details such as the patient’s name, drug and time, which ultimately resulted in only 34.9% of medications being administered at the prescribed time. Considering nurses’ adherence to risk mitigation measures, redesigning medication labeling would be an effective measure to reduce medication errors.
Among the downstream functions, the module of patient identification and medication verification was the most affected by other modules, mainly due to the insufficient information management of patients’own medications (POM). Although POM management is not recommended in hospitals, the vast majority of hospitals are unable to prevent it24. Hospitalized patients’ medications were generally managed by the ward, and nurses dispensed them on their own after doctors prescribed self-contained orders based on the patient’s condition. However, POM does not display barcodes and needs to be recorded manually in the system. This situation was not uncommon. The survey showed that more than half of the medical institutions lacked POM management organization and related quality control management, and there was no standardized POM checking process or implementation records25. Although 85.3% of the interviewees believed that it was important to establish an inpatient POM management system, related functional design and application were inadequate and much room for improvement remained25.
Integration and validation of FRAM and DEMATEL
This study integrated the FRAM model and the DEMATEL method to construct a unique theoretical framework and practical tool for analyzing complex systems. The FRAM model describes the interactions between functions in complex socio-technical systems in terms of the multidimensionality of people, technology, and organizations. It provides insight into the sources of performance variability in safety management. However, the model has limitations in quantifying the possibility of success and failure and in identifying appropriate security barriers9. This study quantitatively complemented the FRAM model using an improved DEMATEL method. The study integrated the knowledge background and practical experience of experts to scientifically allocate the weights of different experts. The DEMATEL transforms experts’ fuzzy judgment on functional variability into specific values. The direct and indirect influences among the elements are clarified by constructing a direct influence matrix. Based on the centrality-causality analysis, the weights of the elements are determined, and then the key modules are identified12. The combination of the two methods retains the dynamic panoramic perspective of the FRAM model, and the DEMATEL method significantly enhances the relevance and actionability of the response measures.
Current studies have shown some progress in formal and quantitative improvements of the FRAM model. Van Stralen et al.26 applied the FRAM to construct models of high-alert medication management guidelines and medication administration in daily practice. The study revealed gaps between clinical practice and guidelines by examining normal medication administration behaviors. The influencing factors that led to practice deviations from the guidelines were also explored in depth. Furniss et al.27 conducted a multidisciplinary workshop to explore intractable problems caused by conflicting rules and recommendations and mismatched needs and competencies. Although standardized methodology was not used in these studies, the results provided a valuable reference for the risk assessment of functional variability. In addition, Kaya et al.7 and Salehi et al.8 designed virtual scenarios to calculate the probability of functional variability occurring in some techniques, such as RL. They assessed the relative importance of function by combining both normal and emergency scenarios. However, the probability of variability is not equivalent to variability itself. Therefore, comprehensively analyzing functional variability from multiple dimensions, such as time, precision, and the effect of current safety mechanisms, is closer to real clinical situations, thus providing more accurate decision support for the safety management of complex systems.
Mixed methods are the most popular method in healthcare research and the most common type used for developing and validating FRAM models9. Among them, semi-structured interviews, workshops, and focus groups are common methods used to validate the FRAM model as reliable9,28. This study utilized interviews and the DEMATEL to review the comprehensiveness and accuracy of the FRAM model. Researchers used interview data to refine the whole elderly inpatient process from admission to discharge and the conditions guaranteeing the normal operation of each model. The comprehensiveness of the FRAM model was confirmed after expert discussion. In the centrality-cause scatter plot (Supplementary Fig. S6), functionality F2 medical prescription entry was more associated with other functions and had a wide range of influence, and F14 patient identification was a downstream link and located in the fourth quadrant with a high degree of being influenced. The DEMATEL results verified that the FRAM model was accurate.
Improve individual-task-technology-environment fit to ensure patient safety
Previous studies found that even when two hospitals used the same system, they differed in their effectiveness in preventing ADEs and reducing injuries29. Considering that environmental and contextual factors could affect the use of information systems, the interactions between the medication process components were analyzed at the individual, task, technology, and environment levels, and measures of adverse events were summarized through interviews with medical personnel. Improving task-technology and technology-individual fit were the main risk management measures, consistent with previous studies (Table 3)30,31.
One of the mismatches between tasks and technology was more evident in field observations. Some tasks were a mix of paper and electronic records, and medical personnel needed to upload operational information to the system, resulting in cumbersome and inefficient workflows. Many physicians also complained about this, wishing that "routine tasks could be performed in a simple way without having to use the system for additional steps"32. Previous research found that the higher the level of task-technology fit, the higher the level of perceived usefulness and ease of use by users, and the lower the risk level 33,34. Thus, the study proposed that adding options to fields and lists in the system would optimize workflow and increase productivity. This was also verified by experiments that specifically analyzed the changes made to the EMMS, where the options added to the lists facilitated the system in supporting tasks previously performed on paper, ensuring real-time and accurate record-keeping35.
Customizing the management system based on user characteristics and requirements will directly increase technical availability36,37 and, thereby, increase the security of the system as a whole38. The majority of the participants included in the study were senior personnel with a relative lack of digital skills, which, combined with the increase in hospital information systems components and changes in workflow, made it difficult for them to cope with job pressures39. In addition, the interviewees indicated that some information had to be searched repeatedly in the interface to be found, and some information was scattered in different modules of the system, which undoubtedly increased the number of operational steps and consumed more time40,41. Considering the characteristics of the users and the nature of their work, the information in the user interface should be rearranged to include drug-related information side-by-side to assist in decision-making and minimize errors of omission, such as navigation41.
Alarm-related problems are common usability challenges that lead to patient harm42. The complexity of the condition and the variety of medications used by elderly inpatients increase the difficulty of the system in detecting and preventing safety problems. Medications such as valium used at night cannot be alerted in time for timely assessment by medical personnel, which also tends to increase the risk of nighttime falls. Despite the widespread use and optimization of systems, improvements in overall safety performance are not evident, and the safety performance of the systems varies widely across hospitals. For example, the effectiveness of the alerts for treating repeated contraindications is not the same43 and indicates the need for improvements in hospital information technology in terms of personalized settings and safety performance enhancement43,44.
Limitations
This study combined on-site observations, semi-structured interviews, and system data to identify the medication administration process and related problems in elderly inpatients, which was limited in terms of the target population and scope. Thus, the data on healthcare personnel behavior was limited, and the spatial distribution and motion features should be considered to identify the behaviors of medical personnel. Second, no obvious issues on environment and context were found, but this did not mean that they do not exist, as the World Health Organization’s Global Patient Safety Challenge calls for "ensuring medication safety at different levels of care, environments, and contexts." A slight move in one part may affect the whole situation. Although the measures were proposed with a holistic view, it is important to monitor the situation and assess the impact of the various measures, as they may interact with each other.
Conclusion
This study applied the FRAM method to develop a functional model of the medication administration process in elderly inpatients. Interactions between the modules were identified by on-site observations, document analysis, and semi-structured interviews. The safety issues and current measures were described from human, technological, organizational, and environmental perspectives. The improved DEMATEL method assigns different weights to each expert and transforms experts’ fuzzy judgment on functional variability into specific values. A direct impact matrix was constructed based on the FRAM model and experts’ scores to quantify functional variability, as well as the effectiveness of control measures. It helped to identify the key function modules that affect the safe operation of the system, such as prescription entry, label printing, patient identification, and medication verification. However, the current study population was restricted to inpatients, and the number of experts involved in scoring was limited, which may affect the judgment of functional variability. Future studies will need to extend to medication management for elderly patients in different settings and contexts, such as the home and community, to ensure patient medication safety in all aspects. In addition, the study proposes risk management measures from the perspective of overall functional safety to improve individual-task-technology-environment fit, while empirical studies are still lacking. Therefore, the implementation effects of the measures must be continuously observed and evaluated in the future.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available, because some of the data involves personal privacy, but are available from the corresponding author on reasonable request.
References
Bates, D. W. et al. The safety of inpatient health care. N Engl. J. Med. 388, 142–153 (2023).
Hodkinson, A. et al. Preventable medication harm across health care settings: A systematic review and meta-analysis. BMC Med. 18, 313 (2020).
Xuelin, S. & Xin, Hu. Current situation and rational use of clinical drugs in the elderly. Chin. J. Clin. Healthc. 21, 123–126 (2018).
Sujan, M. et al. What kinds of insights do Safety-I and Safety-II approaches provide? A critical reflection on the use of SHERPA and FRAM in healthcare. Saf. Sci. 173, 106450 (2024).
Hollnagel, E. FRAM: The Functional Resonance Analysis Method: Modelling Complex Socio-Technical Systems (CRC Press, 2017). https://doi.org/10.1201/9781315255071.
Huang, W., Yin, D., Xu, Y., Zhang, R. & Xu, M. Using N-K Model to quantitatively calculate the variability in functional resonance analysis method. Reliab. Eng. Syst. Safe 217, 108058 (2022).
Kaya, G. K. & Hocaoglu, M. F. Semi-quantitative application to the functional resonance analysis method for supporting safety management in a complex health-care process. Reliab. Eng. Syst. Safe 202, 106970 (2020).
Salehi, V., Tran, T. T., Veitch, B. & Smith, D. A reinforcement learning development of the FRAM for functional reward-based assessments of complex systems performance. Int. J. Ind. Ergon. 88, 103271 (2022).
Salehi, V., Veitch, B. & Smith, D. Modeling complex socio-technical systems using the FRAM: A literature review. Human Factors Ergon. Manuf. Serv. Ind. 31, 118–142 (2021).
Selerio, E., Caladcad, J. A., Catamco, M. R., Capinpin, E. M. & Ocampo, L. Emergency preparedness during the COVID-19 pandemic: Modelling the roles of social media with fuzzy DEMATEL and analytic network process. Socio-econ. Plan Sci. 82, 101217 (2022).
Ke, Z. et al. Improve the satisfaction of medical staff on the use of home nursing mobile APP by using a hybrid multi-standard decision model. BMC Nurs. 23, 302 (2024).
Si, S.-L., You, X.-Y., Liu, H.-C. & Zhang, P. DEMATEL technique: A Systematic review of the state-of-the-art literature on methodologies and applications. Math. Probl. Eng. 2018, 3696457 (2018).
Bertaux, D. Biography and Society: The Life History Approach in the Social Sciences (SAGE Publications, 1981).
Grady, M. P. Qualitative and Action Research: A Practitioner Handbook (Phi Delta Kappa Educational Foundation, 1998).
Prgomet, M., Georgiou, A., Callen, J. & Westbrook, J. Fit between individuals, tasks, technology, and environment (FITTE) framework: A proposed extension of FITT to evaluate and optimise health information technology use. Stud. Health Technol. Inform. 264, 744–748 (2019).
Carayon, P. et al. Characterising the complexity of medication safety using a human factors approach: An observational study in two intensive care units. BMJ Qual. Saf. 23, 56–65 (2014).
Dabliz, R. et al. Medication safety improvements during care transitions in an Australian intensive care unit following implementation of an electronic medication management system. Int. J. Med. Inform. 145, 104325 (2021).
Vaghasiya, M. R., Poon, S. K., Gunja, N. & Penm, J. The impact of an electronic medication management system on medication deviations on admission and discharge from hospital. Int. J. Environ. Res. Public Health 20, 1879 (2023).
Tobiano, G., Chaboyer, W., Teasdale, T., Raleigh, R. & Manias, E. Patient engagement in admission and discharge medication communication: A systematic mixed studies review. Int. J. Nurs. Stud. 95, 87–102 (2019).
Heyworth, L. et al. Aligning medication reconciliation and secure messaging: Qualitative study of primary care providers’ perspectives. J. Med. Internet Res. 15, e264 (2013).
Pons, E. S. et al. Users’ preferences and perceptions of the comprehensibility and readability of medication labels. PLoS ONE 14, e0212173 (2019).
Lohmeyer, Q. et al. Effects of tall man lettering on the visual behaviour of critical care nurses while identifying syringe drug labels: A randomised in situ simulation. BMJ Qual. Saf. 32, 26–33 (2023).
Allison Rout, J., Yusuf Essack, S. & Brysiewicz, P. Evaluation of intermittent antimicrobial infusion documentation practices in intensive care units: A cross-sectional study. Intens. Crit. Care Nur. 79, 103527 (2023).
Jezequel, J. A risk-analysis survey on patients’ own medication usage among inpatients in a French general hospital. Le Pharmacien Hospitalier et Clinicien 47, e1–e7 (2012).
Suggestions on clinical management of inpatients’ own medications in Chinese medical institutions. Chin. J. Hosp. Pharm. 43, 1651–6 (2023).
van Stralen, S. A., van Eikenhorst, L., Vonk, A. S., Schutijser, B. C. F. M. & Wagner, C. Evaluating deviations and considerations in daily practice when double-checking high-risk medication administration: A qualitative study using the FRAM. Heliyon 10, e25637 (2024).
Furniss, D. et al. Using FRAM to explore sources of performance variability in intravenous infusion administration in ICU: A non-normative approach to systems contradictions. Appl. Ergon. 86, 103113 (2020).
Kaya, G. K., Ovali, H. F. & Ozturk, F. Using the functional resonance analysis method on the drug administration process to assess performance variability. Saf. Sci. 118, 835–840 (2019).
Gates, P. J., Hardie, R.-A., Raban, M. Z., Li, L. & Westbrook, J. I. How effective are electronic medication systems in reducing medication error rates and associated harm among hospital inpatients? A systematic review and meta-analysis. J. Am. Med. Inform. Assoc. 28, 167–176 (2021).
Mulac, A., Mathiesen, L., Taxis, K. & Granås, A. G. Barcode medication administration technology use in hospital practice: A mixed-methods observational study of policy deviations. BMJ Qual. Saf. 30, 1021–1030 (2021).
Taft, T. et al. ‘Are we there yet?’ Ten persistent hazards and inefficiencies with the use of medication administration technology from the perspective of practicing nurses. J. Am. Med. Inform. Assoc. 30, 809–818 (2023).
Canfell, O. J. et al. The impact of digital hospitals on patient and clinician experience: Systematic review and qualitative evidence synthesis. J. Med. Internet Res. 26, e47715 (2024).
Renjie, Li., Jianpeng, G. & Shuai, Lv. The impact of task-technology fit on college students’ intention to continue using online learning: Based on an empirical survey of 258 universities in China. China High. Educ. Res. 12, 45–50 (2022).
Huaizhen, Y., Yangbo, T. & Zhaoquan, J. A literature review of task-technology fit theory and tendency prospects. Foreign Econ. Manag. 38, 29–41 (2016).
Kinlay, M. et al. Electronic medication management systems: Analysis of enhancements to reduce errors and improve workflow. Appl. Clin. Inform. 12, 1049 (2021).
Bouraghi, H. et al. Challenges and advantages of electronic prescribing system: A survey study and thematic analysis. BMC Health Serv. Res. 24, 689 (2024).
Xiaojun, Xu., Guanghui, C., Dandan, Q. & Wang, Lu. The influence of the operation mechanism of the information ecological chain of tourism business websites on user perception under the digital economy. Inf. Sci. 41, 78–86 (2023).
Classen, D. C., Longhurst, C. A., Davis, T., Milstein, J. A. & Bates, D. W. Inpatient EHR user experience and hospital EHR safety performance. JAMA Netw. Open 6, e2333152 (2023).
De Leeuw, J. A., Woltjer, H. & Kool, R. B. Identification of factors influencing the adoption of health information technology by nurses who are digitally lagging: in-depth interview study. J. Med. Internet Res. 22, e15630 (2020).
Kinlay, M. et al. Stakeholder perspectives of system-related errors: Types, contributing factors, and consequences. Int. J. Med. Inform 165, 104821 (2022).
Roman, L. C., Ancker, J. S., Johnson, S. B. & Senathirajah, Y. Navigation in the electronic health record: A review of the safety and usability literature. J. Biomed. Inform. 67, 69–79 (2017).
Howe, J. L., Adams, K. T., Hettinger, A. Z. & Ratwani, R. M. Electronic health record usability issues and potential contribution to patient harm. JAMA 319, 1276–1278 (2018).
Classen, D. C. et al. National trends in the safety performance of electronic health record systems from 2009 to 2018. JAMA Netw. Open 3, e205547 (2020).
Holmgren, A. J. et al. Assessing the safety of electronic health records: a national longitudinal study of medication-related decision support. BMJ Qual. Saf. 29, 52–59 (2020).
Acknowledgements
Thanks to quality management platform of the Jiangsu Province Hospital. We are also grateful to our study participants for their cooperative responses during data collection.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Jiangsu Province Hospital [grant number CXTDA2017019]; Jiangsu Province Postgraduate Practice Innovation Project [grant number SJCX24_0830]; and 2024 Jiangsu Province Local Standards [grant number No.210].
Author information
Authors and Affiliations
Contributions
Yang: designed the study, analyzed the data, wrote and revised the manuscript. Yin: conceived and designed the study, collected the data, analyzed the data and wrote the manuscript. Xu: analyzed the data and wrote the manuscript. Gu: conceived the study and contributed to the design of the study. Li, Yan, Jiang, Lu, Fu, Yu and Hou: contributed to the interpretation of the data and the data collection process.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The conduct of the study was in accordance with the Declaration of Helsinki 2013 and approved by Jiangsu Province Hospital Ethics Committee (internal ethics committee registration 2024-SR-135).
Consent to participate
Written informed consent was obtained from all participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yang, J., Yin, X., Xu, Y. et al. Medication safety analysis of elderly inpatients based on improved functional resonance analysis method (FRAM): a mixed methods study. Sci Rep 15, 19496 (2025). https://doi.org/10.1038/s41598-025-04458-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04458-7