Abstract
In patients with Crowe III developmental dysplasia of the hip (DDH), surgery presents challenges such as severe bone defects and inadequate acetabular cup coverage. This study compares the clinical efficacy of 3D-printed personalized Augments prostheses with conventional femoral head reshaping and structural bone grafting in total hip arthroplasty (THA) for patients with Crowe III DDH. A retrospective analysis was conducted on 52 Crowe III patients. The 3D group (26 cases) used 3D printing technology combined with computer simulation to design personalized Augments prostheses. Preoperative models were printed to simulate the surgical procedure, and high-porosity porous structured Augments prostheses and acetabular cup layers were printed using titanium alloy powder. The non-3D group (26 cases) underwent traditional femoral head reshaping and structural bone grafting. The study compared the differences in lower limb length, the horizontal and vertical distances of the hip joint rotation center from the teardrop line, acetabular cup abduction angle, acetabular cup coverage, operation time, intraoperative blood loss, postoperative time to mobilization, time to hospital discharge, Harris hip scores during follow-up, and complications between the two groups. In the 3D group compared to the non-3D group, intraoperative blood loss (261.92 ± 14.70 vs. 313.85 ± 20.02 ml, P < 0.05), time to mobilization (1.27 ± 0.45 vs. 4.85 ± 1.05 days, P < 0.05), and time to discharge (2.77 ± 0.65 vs. 5.85 ± 0.92 days, P < 0.05) were significantly lower, as was the limb length discrepancy on the first postoperative day (0.25 ± 0.21 cm vs. 0.48 ± 0.28 cm, P < 0.05). The acetabular cup coverage rates on the first postoperative day and at 3 months postoperatively (1 ± 0.00 vs. 0.93 ± 0.07; 1 ± 0.00 vs. 0.83 ± 0.11, P < 0.05) were significantly higher in the 3D group. The Harris hip scores at 3, 6, and 12 months postoperatively were also higher in the 3D group than in the non-3D group, with statistically significant differences (P < 0.05). The application of 3D-printed personalized augment prostheses in total hip arthroplasty provides a relatively feasible treatment option for patients with Crowe type III DDH. This approach contributes to personalized treatment and shows potential in improving surgical accuracy and certain treatment outcomes.
Similar content being viewed by others
Introduction
Developmental dysplasia of the hip (DDH) patients typically present with hip joint dysplasia, limb shortening, and gait abnormalities, which are significant contributors to secondary osteoarthritis of the adult hip joint, leading to severe joint dysfunction1. Research indicates that total hip arthroplasty (THA) is effective in treating adult DDH. However, it is a challenging procedure, demanding high technical proficiency from physicians in THA techniques2,3. In Crowe type III DDH cases, the degree of femoral head dislocation exceeds 75%, with a shallow acetabulum unable to contain the femoral head. Long-term biomechanical abnormalities lead to progressive femoral head dislocation, cartilage degeneration, femoral head necrosis, and severe osteoarthritis4. For such patients, acetabular reconstruction is crucial for surgical success, aiming to restore the normal rotation center while ensuring the initial stability of the prosthesis5. Traditional bone grafting combined with total hip arthroplasty struggles to locate the position of the rotation center and address acetabular stability and coverage issues, potentially resulting in surgical failure and complications6,7,8. In recent years, the combination of 3D printing technology and three-dimensional simulation has garnered attention to address these challenges9,10.
This study integrates the aforementioned technologies to conduct personalized simulations and customize individualized Augments prostheses for patients. Using computer-aided design, the optimal acetabular cup placement and cup size are determined based on the patient’s hip joint anatomy. Bone defects are assessed, and Augments prostheses tailored to the patient’s individual condition are designed. High-porosity titanium alloy porous structures are 3D printed, providing high initial stability and facilitating rapid bone integration, thereby enhancing the precision and success rate of the surgery.
This article aims to explore the clinical efficacy of integrating 3D printing technology with personalized Augments prostheses and acetabular prostheses compared to autologous femoral head structural bone grafting and traditional acetabular prostheses in THA for treating patients with Crowe type III DDH. It analyzes the therapeutic outcomes and safety of both surgical techniques. We hope that this research will provide more clinical evidence for this innovative treatment approach, bringing new breakthroughs and hope for the treatment of Crowe Type III DDH patients, and advancing the innovative development of 3D printing combined with personalized customization technology.
Materials and methods
General information
A retrospective case analysis was conducted, involving 70 patients with DDH who were admitted to the Department of Orthopedics at Shenyang Medical College Affiliated Central Hospital from March 2017 to June 2020. All patients were clinically diagnosed with and confirmed to have Type III DDH. Ultimately, 52 patients meeting the inclusion criteria were included in the study.
The group treated with individualized Augments prostheses and acetabular prostheses using 3D printing is referred to as the “3D group” (26 cases), while the group treated with autologous femoral head structural bone grafting and traditional acetabular prostheses is referred to as the “Non-3D group” (26 cases). Please refer to Fig. 1 for the study flowchart. All patients exhibited positive signs of the “4” sign and Trendelenburg sign, accompanied by significant limping gait and notable hip joint pain on the affected side, with incomplete dislocation of the femoral head.
The study obtained approval from the relevant medical ethics department at Shenyang Medical College Affiliated Central Hospital. All patients were informed about the study and provided voluntary consent to participate by signing an informed consent form.
Inclusion criteria
(1) Patients with Crowe Type III DDH presenting with hip joint pain accompanied by limping gait and poor response to various conservative treatments; (2) Patients undergoing primary unilateral hip joint replacement; (3) Absence of coagulation dysfunction and other high-risk bleeding factors before surgery; (4) Presence of acetabular bone defects, managed intraoperatively with customized Augments prostheses or conventional autologous femoral head structural bone grafting.
Exclusion criteria
(1) Patients with severe liver or kidney dysfunction, cerebrovascular accidents, or other contraindications for THA; (2) Patients with bilateral DDH.
Preoperative patient Preparation and management
Comprehensive preoperative examinations were conducted for all patients. Bilateral hip joint anteroposterior X-ray, bilateral full-length lower limb anteroposterior and lateral X-ray images were obtained (using the digital radiography (DR) system from Philips in the Netherlands). Additionally, bilateral hip joint CT scans with 3D reconstruction were performed (using the 256-slice spiral CT scanner from Philips in the Netherlands, with a scanning layer thickness of 0.6 mm). Measurements included assessment of lower limb length discrepancy, distance from the femoral head rotation center to the teardrop horizontal and vertical distances (following the method described by Russotti et al.11), evaluation of acetabular wall thickness, acetabular bone mass, and proximal femoral canal narrowing.
For the 3D group, CT data were used for virtual simulation, calculation, design, 3D model printing, and customization of individualized Augments prostheses.
Customization of individualized augments prostheses
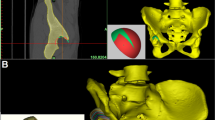
The CT imaging data of bilateral hip joints of the patient (Fig. 2A) were imported into Mimics 20.0 software (Materialise, Belgium) workstation in DICOM format for three-dimensional modeling (Fig. 2B). Through a collaborative effort between engineers and surgical physicians, the true acetabular position and acetabular cup model for the prosthesis were calculated (Fig. 3A). Parameters such as bone defect shape, size, etc., were measured, and the model of the Augments prosthesis was designed, followed by determining the placement position of the Augments prosthesis (Fig. 3B and C) and selecting the femoral prosthesis model (Fig. 3D).
Subsequently, the data from three-dimensional modeling and virtual design were exported in STL format and imported into FlashPrint 5 software (FlashForge Technology, China). The 3D models of the original hip joint, the hip joint after virtual design, and the Augments prosthesis were printed using PLA (polylactic acid) as the printing material (Fig. 4) to conduct preoperative simulation and demonstrate the surgery.
Engineers utilize the EBM Q10 plus software (Acram AB, Sweden) to print personalized trabecular bone Augments designed with Ti-6 Al-4 V as the raw material (Fig. 5A and B). The acetabular prosthesis (Fig. 5C and D) used in surgery is also a 3D-printed trabecular bone structure. Detailed inspection and sterilization are required.
The personalized Augments prostheses printed need to be sent to a specialized quality inspection department for assessment, including strength, compression resistance, tensile strength, and fatigue resistance, among other aspects. Only Augments prostheses that pass the quality inspection can be put into use.
Design and Positioning of Acetabular and Augments Prostheses, and Determination of Femoral Implant Size. (A): Original acetabular positioning and model simulation for the patient. (B): Assessment of bone defect and simulation of personalized Augments prosthesis. (C): Simulation positioning of acetabular and Augments prostheses in coronal, transverse, and sagittal planes. (D): Measurement of femoral medullary canal thickness for determination of femoral implant size.
Surgical procedure and brief process for the 3D group
All surgeries in this study were performed by the same team, led by a senior surgeon with extensive experience in hip replacement, to ensure consistency in surgical technique.
After the anesthesia takes effect, the patient is positioned on the lateral side (Fig. 6A). A posterior lateral approach is utilized, and layer-by-layer dissection is performed. The external rotator muscle group is severed at the greater trochanter, and the joint capsule is detached. The hip joint is dislocated, and the femoral neck is cut approximately 1.5 cm above the lesser trochanter to remove the femoral head. Utilizing three-dimensional modeling and 3D models, the original acetabulum is identified along the inferior and inner aspect of the dislocated femoral head, and progressive clearing, excision of the acetabular labrum, and removal of proliferative tissue are performed. The acetabulum is reamed at the predetermined position and direction, and a new acetabulum is created at the true acetabular position (Fig. 6B). After achieving the design effect, a trial reduction of the acetabular prosthesis is performed. Following this, the original acetabulum is reamed at the site of bone defect above the true acetabulum according to the designed position, direction, and acetabular reaming size (Fig. 6B). Then, the Augments prosthesis trial is inserted. Subsequently, the individualized Augments prosthesis is installed and secured with screws. Bone cement is applied appropriately at the interface between the Augments prosthesis and the acetabular prosthesis before inserting the acetabular prosthesis and securing it with screws (Fig. 6C). After placing the femoral side prosthesis, the hip joint is reduced. During reduction, stability, range of motion, tension of the sciatic nerve, and blood vessel tension are checked. If tension is significant, the soft tissues around the hip joint are moderately released. The incision is closed layer by layer.
Postoperative management
Routine measures are taken to prevent infection and anticoagulation is administered postoperatively. The affected limb is maintained in neutral abduction and extension position after surgery. On the first postoperative day, follow-up X-rays of both hips in the anteroposterior and lateral views, along with full-length anteroposterior and lateral views of both lower limbs are obtained (Fig. 6D). Passive and active exercises are initiated for the affected limb to improve quadriceps muscle strength and prevent joint dislocation. For the 3D group, standing and walking with assistance may be initiated on the first postoperative day after the follow-up examination. For the Non-3D group, crutch-assisted ambulation is recommended for the first week postoperatively, followed by full weight-bearing at 4–8 weeks after the follow-up examination.
Main observational indicators
-
(1)
Radiological Evaluation: Preoperative and postoperative X-rays were taken on the first day, recording the pre- and postoperative differences in leg length between the two groups of patients; comparing the pre- and postoperative distances from the femoral head center to the teardrop level and vertically11; comparing the acetabular cup anteversion angles between the two groups of patients; comparing the acetabular cup coverage rates between the two groups of patients on the first day postoperatively and at 3 months postoperatively12.
-
(2)
Surgical Evaluation: Comparing the surgical times between the two groups of patients: from the start of skin incision to closure of the surgical incision; intraoperative blood loss: the sum of blood collected by suction and absorbed by gauze; time to ambulation after surgery: the time from completion of surgery to the first standing from bed by the patient; time to discharge after surgery: the time from surgery completion to the patient leaving the hospital.
-
(3)
Functional and Complication Evaluation: Recording the Harris hip function scores before treatment, at 3 months, 6 months, and 12 months postoperatively; recording complications at 3 months postoperatively. Subsequent annual follow-ups included bilateral hip X-rays to observe for dislocation, infection, nerve damage, bone resorption, and implant loosening.
Intraoperative images and postoperative X-rays of a patient from the 3D group. (A): Patient positioning and incision marking. (B): Intraoperative reconstruction of the positioning of acetabular and Augments prostheses based on three-dimensional modeling and 3D models. (C): Intraoperative installation effect of Augments prostheses, acetabular prostheses, and acetabular liners. (D): Postoperative first-day bilateral hip anteroposterior X-ray images of the patient.
Statistical analysis
Statistical analysis was conducted using SPSS version 27.0 software. Descriptive statistics were employed to calculate the means and standard deviations for continuous variables, and frequencies for categorical variables. The Shapiro-Wilk test was used to assess normality for continuous variables, while the chi-square test was utilized for categorical variables. Quantitative data were analyzed using both independent samples t-tests and Mann-Whitney U tests. The level of statistical significance was set at p < 0.05.
Results
Baseline and Follow-up data
Baseline and follow-up data were similar between the two groups of patients, with all between-group comparisons having p-values > 0.05. Follow-up was obtained for all 52 included patients through telephone calls, outpatient visits, etc. The average follow-up time postoperatively was 25.65 ± 2.97 months for the 3D group and 26.46 ± 3.83 months for the non-3D group, as detailed in Table 1.
Radiological findings
On the first day postoperatively, both the 3D and non-3D groups showed significant correction of limb length discrepancies, with a difference in limb lengths of (0.25 ± 0.21 cm vs. 0.48 ± 0.28 cm, p < 0.05), indicating statistically significant differences. All cases exhibited hip joint rotation centers that were close to normal postoperatively, with the horizontal distance between rotation centers for the two groups being (3.05 ± 0.23) vs. (3.17 ± 0.32) cm and the vertical distance being (2.05 ± 0.19) vs. (2.17 ± 0.23) cm, showing no statistically significant differences. The anteversion angles were (45.17 ± 2.38° vs. 44.65 ± 2.10°) for the two groups, with no statistically significant differences. The acetabular coverage rates on the first day and at 3 months postoperatively ((1 ± 0.00 vs. 0.93 ± 0.07; 1 ± 0.00 vs. 0.83 ± 0.11, p < 0.05) respectively) showed statistically significant differences between the two groups. See Table 2 for details.
Surgical data evaluation
The surgical time in the two groups was 66.04 ± 4.01 vs. 68.27 ± 3.24 min, with no statistically significant difference (P > 0.05).
In both groups, there were statistically significant differences in intraoperative blood loss (261.92 ± 14.70 vs. 313.85 ± 20.02 ml, p<0.05), time to ambulation after surgery (1.27 ± 0.45 vs. 4.85 ± 1.05 days, p < 0.05), and time to discharge after surgery (2.77 ± 0.65 vs. 5.85 ± 0.92 days, p < 0.05). See Table 3 for details.
Functional and complication evaluation
At 3, 6, and 12 months postoperatively, the Harris hip function scores in the 3D group were higher than those in the non-3D group, with statistically significant differences observed. There were no statistically significant differences in complications at 3 months postoperatively. See Table 4 for details.
Follow-up revealed primary wound healing in all cases. At 3 months postoperatively, both the 3D and non-3D groups had 2 cases of mild limping, which resolved after guided functional exercises. In the non-3D group, 3 cases of autologous femoral head bone graft resorption were observed. Bone graft resorption has led to acetabular bone defects and insufficient coverage. However, the patient currently shows no signs of hip pain or acetabular cup loosening but remains at high risk. At the final follow-up, all patients demonstrated good walking function, with no occurrences of dislocation, infection, nerve damage, or implant loosening.
Discussion
In early stages, patients with developmental dysplasia of the hip (DDH) exhibit deficient acetabular development, resulting in the failure to establish a normal congruent relationship between the femoral head and the acetabulum. As individuals age, the abnormal anatomical relationships and stress patterns continue to impact the biomechanical environment of the hip joint, ultimately exacerbating different acetabular morphologies and femoral head dislocations13. Crowe III DDH patients typically present with significant upward displacement of the femoral head (greater than 75%), with load-bearing concentrated in the upper portion of the acetabulum. Consequently, acetabular deficiencies are commonly observed at the superior margin, leading to reduced bone coverage for prosthetic implants1,4.
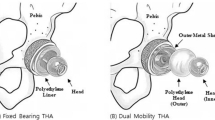
In Crowe III DDH patients, acetabular reconstruction is the most crucial and challenging aspect of THA14. During acetabular reconstruction, it is imperative to restore normal anatomical mechanics, increase prosthetic coverage, and ensure initial stability. Additionally, maintaining appropriate cup anteversion and inclination angles is essential to prevent dislocation or loosening3,15. Current methods of acetabular reconstruction include autogenous bone grafting to augment the acetabulum, medial wall osteotomy for medialization of the implant and intentional high placement of the implant. However, these methods have their limitations, such as non-union, bone absorption, collapse, high rates of implant cup loosening, reduced range of motion, and inability to correct a limping gait15,16,17.
In contrast, reconstructing the original acetabulum of the hip joint can restore normal anatomical relationships, which is crucial for improving abductor muscle function, correcting a limping gait, and ensuring long-term survival of the prosthesis18. However, original acetabular reconstruction is challenging due to difficulties in positioning, and it still faces severe bone defects after reconstruction. In such cases, combining 3D printing technology for three-dimensional reconstruction, design, and customization of individualized Augments prostheses can effectively address these issues. In our study, all patients underwent reconstruction at the original acetabulum of the hip joint with the placement of a Augments prosthesis at the site of acetabular bone defects. Both the acetabular cup prosthesis and Augments prosthesis were made of 3D-printed high-porosity titanium alloy porous structures, providing high initial stability, rapid bone integration, and restoration of normal anatomical relationships and coverage of the hip joint prosthesis cup.
3D printing enables three-dimensional reconstruction, calculation, and customization with individualized and precise characteristics. Studies have shown that many complications associated with THA in DDH patients can be alleviated through careful preoperative planning and surgical techniques3. The use of three-dimensional simulation technology allows for a comprehensive assessment of the morphological characteristics of true and false acetabula in DDH patients and the calculation of bone defects in the original acetabulum of the hip joint, facilitating detailed preoperative planning19. Research by Chen et al.20 demonstrated acceptable accuracy of 3D simulation in predicting the dimensions of acetabular components in DDH patients, which can enhance the effectiveness of THA and is recommended for DDH cases. Wang et al.21 conducted finite element analysis of acetabular cup stability in THA for DDH using metal reinforcement and bone grafting. The study found that metal reinforcement interfaces achieved stronger direct fixation.
Modern healthcare is shifting from solely focusing on curing diseases to optimizing treatment strategies and improving patient outcomes. In the field of orthopedics, treatment is progressing toward minimally invasive, precise, efficient, and individualized approaches. 3D printing technology enables personalized customization based on the anatomical characteristics of the patient’s acetabulum, making it particularly suitable for complex bone defects such as Crowe type III developmental dysplasia of the hip (DDH). It allows for better anatomical matching and improved initial stability, facilitating individualized treatment planning and optimizing the overall diagnostic and therapeutic process. Moreover, 3D printing technology is highly consistent with the concept of fast-track surgery (FTS), as its porous structure promotes bone integration and preoperative planning enhances surgical precision. In this study, the 3D group demonstrated excellent performance in minimizing surgical trauma and intraoperative blood loss, as well as accelerating postoperative recovery, highlighting its advantages in improving surgical quality and enhancing recovery. This was also the primary reason for our choice to use 3D-printed implants.
In the early stages of treatment, our team considered designing and printing an integrated implant for the management of Crowe III DDH. Although simulations and design evaluations confirmed the technical feasibility of printing a single-piece structure, it required extremely high printing precision and surgical expertise, with limited intraoperative flexibility. This made it difficult to accommodate subtle variations in bone defects encountered during surgery. Moreover, performing both hip replacement and acetabular defect reconstruction with a one-piece implant posed significant challenges, such as accurately locating the native acetabulum, determining the center of rotation, and assessing bone defects.In contrast, modular 3D-printed augments allow for intraoperative adjustment of position and angle based on the patient’s actual bone defect, providing basic surgical adaptability and tolerance. Therefore, we ultimately adopted a dual-module design combined with intraoperative bone cement fixation, which ensured good initial stability while retaining necessary flexibility during the procedure.
In this study, all 52 cases of Crowe III DDH patients achieved good postoperative recovery. The research demonstrated that in correcting limb length and improving hip joint function, the 3D group showed superior results and enabled early mobilization and rehabilitation exercises. Comparing surgical data between the two groups, the 3D group exhibited significantly less intraoperative blood loss, shorter time to ambulation after surgery, and shorter time to discharge compared to the non-3D group. Although the surgical duration was similar between the groups, the 3D group required additional time for bone cement fixation, resulting in a 13-minute waiting period, yet overall operative and exposure times were shorter in the 3D group. Among the graft group, three patients experienced bone resorption. The maximum limb length discrepancy in this study was 3.1 cm, with no cases of nerve traction paralysis postoperatively; however, both groups had two patients with slight limping at the 3-month follow-up, which resolved after guided functional exercises. Further research is needed on the maximum achievable limb lengthening in DDH patients. Through analysis of symptoms, imaging data, and Harris functional scores before and after treatment, 3D printing technology combined with personalized Augments prostheses achieved more satisfactory early efficacy in treating Crowe III DDH patients.
This study is a retrospective analysis without a randomized design, which may introduce selection bias and potentially affect the generalizability of the results and the reliability of causal inferences.The sample size included in the study was relatively small, totaling 52 patients overall. Although the average follow-up period exceeded 2 years, increasing the sample size and extending the follow-up duration could provide more reliable persuasive power and allow for mid-to-long-term efficacy assessment. In the future, we plan to conduct prospective, randomized controlled trials to further validate the findings of this study.
Conclusion
Total hip arthroplasty using 3D-printed personalized augment prostheses combined with acetabular implants offers a relatively appropriate treatment option for patients with Crowe type III DDH. Compared to traditional approaches, this technique has certain advantages in reducing intraoperative blood loss, shortening postoperative ambulation time and hospital stay, thereby facilitating early functional recovery. To some extent, it enhances the feasibility of individualized treatment and the precision of intraoperative procedures, providing new insights for complex acetabular reconstruction and the development of customized orthopedic implants.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to limitations of ethical approval involving the patient data and anonymity but are available from the corresponding author on reasonable request.
References
Kosuge, D., Yamada, N., Azegami, S., Achan, P. & Ramachandran, M. Management of developmental dysplasia of the hip in young adults: current concepts. Bone Joint J. (6), 95–b. https://doi.org/10.1302/0301-620x.95b6.31286 (2013).
Dhaliwal, A. S. et al. Current surgical techniques in the treatment of adult developmental dysplasia of the hip. J. Pers. Med. 13 (6). https://doi.org/10.3390/jpm13060942 (2023).
Greber, E. M. et al. Challenges in total hip arthroplasty in the setting of developmental dysplasia of the hip. J. Arthroplasty. 32 (9s), S38–s44. https://doi.org/10.1016/j.arth.2017.02.024 (2017).
Cheng, R. et al. Relations between the Crowe classification and the 3D femoral head displacement in patients with developmental dysplasia of the hip. BMC Musculoskelet. Disord. 20 (1), 530. https://doi.org/10.1186/s12891-019-2838-z (2019).
Zong, S. J., Wang, F. & Hu, S. L. Total hip replacement for developmental dysplasia of hip and postoperative nursing. J. Biol. Regul. Homeost. Agents. 30 (1), 173–179 (2016).
Karczewski, D. et al. Femoral head and neck autograft in arthroplasty for developmental dysplasia of the hip: a systematic review of long-term outcomes. Arch. Orthop. Trauma. Surg. 143 (8), 5361–5369. https://doi.org/10.1007/s00402-022-04736-3 (2023).
Kim, M. & Kadowaki, T. High long-term survival of bulk femoral head autograft for acetabular reconstruction in cementless THA for developmental hip dysplasia. Clin. Orthop. Relat. Res. 468 (6), 1611–1620. https://doi.org/10.1007/s11999-010-1288-6 (2010).
Schofer, M. D., Pressel, T., Schmitt, J., Heyse, T. J. & Boudriot, U. Reconstruction of the acetabulum in THA using femoral head autografts in developmental dysplasia of the hip. J. Orthop. Surg. Res. 6, 32. https://doi.org/10.1186/1749-799x-6-32 (2011).
Xu, J. et al. Three-Dimensional host bone coverage in total hip arthroplasty for Crowe types II and III developmental dysplasia of the hip. J. Arthroplasty. 32 (4), 1374–1380. https://doi.org/10.1016/j.arth.2016.11.017 (2017).
Yang, Y. et al. Morphological analysis of true acetabulum in hip dysplasia (Crowe classes I-IV) via 3-D implantation simulation. J. Bone Joint Surg. Am. 99 (17), e92. https://doi.org/10.2106/jbjs.16.00729 (2017).
Russotti, G. M. & Harris, W. H. Proximal placement of the acetabular component in total hip arthroplasty. A long-term follow-up study. J. Bone Joint Surg. Am. 73 (4), 587–592 (1991).
Dorr, L. D., Tawakkol, S., Moorthy, M., Long, W. & Wan, Z. Medial protrusio technique for placement of a porous-coated, hemispherical acetabular component without cement in a total hip arthroplasty in patients who have acetabular dysplasia. J. Bone Joint Surg. Am. 81, 83–92 (1999).
Yang, S., Zusman, N., Lieberman, E. & Goldstein, R. Y. Developmental dysplasia of the hip. Pediatrics 143 (1). https://doi.org/10.1542/peds.2018-1147 (2019).
Qian, H. et al. Total hip arthroplasty in patients with Crowe III/IV developmental dysplasia of the hip: acetabular morphology and reconstruction techniques. Orthop. Surg. 15 (6), 1468–1476. https://doi.org/10.1111/os.13733 (2023).
Dapuzzo, M. R. & Sierra, R. J. Acetabular considerations during total hip arthroplasty for hip dysplasia. Orthop. Clin. North. Am. 43 (3), 369–375. https://doi.org/10.1016/j.ocl.2012.05.012 (2012).
Mou, P., Liao, K., Chen, H. L. & Yang, J. Controlled fracture of the medial wall versus structural autograft with bulk femoral head to increase cup coverage by host bone for total hip arthroplasty in osteoarthritis secondary to developmental dysplasia of the hip: a retrospective cohort study. J. Orthop. Surg. Res. 15 (1), 561. https://doi.org/10.1186/s13018-020-02088-5 (2020).
Faldini, C. et al. Femoral head autograft to manage acetabular bone loss defects in THA for Crowe III hips by DAA: retrospective study and surgical technique. J. Clin. Med. 12 (3). https://doi.org/10.3390/jcm12030751 (2023).
Karaismailoglu, B., Erdogan, F. & Kaynak, G. High hip center reduces the dynamic hip range of motion and increases the hip load: A gait analysis study in hip arthroplasty patients with unilateral developmental dysplasia. J. Arthroplasty. 34 (6), 1267–1272e1. https://doi.org/10.1016/j.arth.2019.02.017 (2019).
Wen, X., Zuo, J., Liu, T., Gao, Z. & Xiao, J. Bone defect map of the true acetabulum in hip dysplasia (Crowe type II and III) based on three-dimensional image reconstruction analysis. Sci. Rep. 11 (1), 22955. https://doi.org/10.1038/s41598-021-02448-z (2021).
Chen, X. et al. Acetabular diameter assessment and Three-Dimensional simulation for acetabular reconstruction in dysplastic hips. J. Arthroplasty. 38 (8), 1551–1558. https://doi.org/10.1016/j.arth.2023.01.067 (2023).
Wang, Y. et al. Biomechanical effect of metal augment and bone graft on cup stability for acetabular reconstruction of total hip arthroplasty in hip dysplasia: a finite element analysis. BMC Musculoskelet. Disord. 23 (1), 277. https://doi.org/10.1186/s12891-022-05168-1 (2022).
Funding
This study was supported by Natural Science Foundation of Liaoning Province (2024-MS-222), Liaoning Provincial Department of Education Fund Project (JYTMS20231396) and the Science and Technology Plan Project of Shenyang City (Grant no. 22-321-32-13).
Author information
Authors and Affiliations
Contributions
Author contributionsAll authors contributed to the preparation, design, and successful execution of the study. They actively participated in the hospitalization, surgical procedures, and subsequent follow-up processes involving the relevant patients. H. R. L., L.Y and X.T. Z. were responsible for material preparation, data collection, and analysis. The initial draft of the manuscript was composed by H. R. L. and L. Y., with B.B. C. and Z.C.C providing comments on earlier versions of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
All procedures were in accordance with the ethical standards of institutional and/or national research councils. The study received approval from the Ethics Board of Central Hospital affiliated with Shenyang Medical College. Informed consent was obtained from the patients.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the images in Figure(1,2,3,4,5 and 6).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, B., Liang, H., Yang, L. et al. 3D printing individualized augments prosthesis and acetabular implant for the treatment of Crowe type III developmental dysplasia of the hip. Sci Rep 15, 19514 (2025). https://doi.org/10.1038/s41598-025-04586-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04586-0