Abstract
Osteoporotic refracture may result from multiple risk factors. However, few studies have explored the association between the interval from the initial fracture to surgery (i.e., the timing of surgery) and osteoporotic refracture. This study aims to investigate the significant risk factors of osteoporotic refracture and to provide more reliable interventions for its prevention. A total of 502 hospitalized patients with osteoporotic fractures from January 2017 to December 2022 at Nanjing Medical University Affiliated Wuxi People’s Hospital were retrospectively analyzed. This included 52 cases in the refracture group and 450 cases in the non-refracture group. Univariate analysis revealed significant differences between the refracture and non-refracture groups. These differences included age, height, body mass index (BMI), bone mineral density (BMD), hemoglobin concentration, total serum protein concentration, pain level, and the interval from fracture to surgery. Further binary logistic regression and Cox proportional hazard regression both indicated that the interval from fracture to surgery, pain level, and age were independent risk factors for refracture. According to the results of receiver operating characteristic (ROC), the prediction accuracy of interval time was high, with area under ROC (AUC) of 0.782, sensitivity of 63.5%, specificity of 84.4%, and threshold value of 10.5. Our study suggests that a longer interval from initial fracture to surgery is associated with an increased risk of refracture, with 10.5 days being the optimal threshold based on ROC analysis.
Similar content being viewed by others
Introduction
Osteoporotic fracture belongs to fragility fracture, which is a serious consequence of osteoporosis in low-energy external force or daily activities because of the decreased bone strength and the destruction of bone microstructure1. With the aging of the population, incidence of osteoporotic fracture is also growing2. It is generally accepted that fracture risk has positive correlations with age and risk of falls, while has negative correlation with BMD. Besides, history of fracture is a significant risk factor of osteoporotic refracture3,4. Osteoporotic fracture and refracture bring not only great inconvenience to people’s life, but heavy economic burden to the society5,6. Therefore, early detection of risk factors and use of appropriate protective measures are effective health care strategies in the management of osteoporotic refracture7,8.
Studies have shown close relations between osteoporotic refractures and sarcopenia, surgical methods, age, gender, and biomechanical indicators9,10,11,12. However, few researchers have explored the association between the interval from the initial fracture to surgery (i.e., timing of surgery) and osteoporotic refracture. Therefore, by comparing multiple indicators between patients with and without refractures, this study aims to investigate significant risk factors of osteoporotic refracture as well as to provide more reliable interventions for the prevention of osteoporotic refracture. In addition, the study intends to explore the association between timing of surgery after the initial fracture and osteoporotic refracture for the prediction in high-risk populations.
Methods
Study population
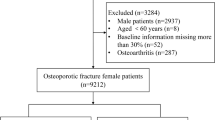
A total of 786 hospitalized patients with osteoporotic fractures from January 2017 to December 2022 in were enrolled, including 105 cases with refracture and 681 cases without refracture. We confirmed that all methods are conducted in accordance with the Chinese Ministry of Health’s "Ethical Review Measures for Biomedical Research Involving Human Subjects (Trial)" and the relevant provisions of the Helsinki Declaration on biological human trials.
The inclusion criteria were as follows: (1) fragility fracture without obvious inducement or low-energy external force (e.g., fall down on a flat surface, slight sprain, etc.) due to the decrease of bone strength and the destruction of bone microstructure; (2) met the surgical indications. Patients were excluded if (1) they received conservative treatments for the initial fracture; (2) they had missing data; (3) they had unclear time of fracture; (4) they had serious concomitant diseases affecting normal life, such as chronic obstructive pulmonary disease (COPD), coronary heart disease, sequelae of stroke, malignant tumors, infectious diseases (bacteria, fungi, viruses and tuberculosis), and diseases affecting lower limb function. (5) they were not treated with routine anti-osteoporotic therapy after the fracture. The routine anti-osteoporosis treatment we use includes: Calcium carbonate 1200 mg/day, taken orally in two doses, continuously; VitD3 800 IU/day, taken orally in two doses, continuously; Alendronate 70 mg, orally administered weekly for one year. We excluded 284 patients and finally obtained 502 eligible patients, including 52 cases in refracture group and 450 cases in non-refracture group (Fig. 1).
Data collection
Eligible patients’ data were collected including age, gender, height, weight, BMI, history of hypertension and diabetes, BMD, hormone use, fracture site, laboratory indicators, pain scale, and the interval from the initial fracture to surgery. Based on the collected data, we investigated characteristics of refracture and its association with the interval from injury to operation after the initial fracture.
Statistical analysis
Variables were expressed as mean ± standard deviation (SD) and counts (proportion) for continuous and categorical ones, separately. Numerical differences between refracture group and non-refracture group were assessed by chi-square test for categorical variables, and t test or Mann–Whitney U test for continuous variables. Significant variables in univariate analysis were further included in binary logistic regression and Cox proportional hazards model in order to analyze the risk factors of refracture. ROC curve was developed to predict the cut-off value. The threshold for significance was set as P < 0.05. All statistical analyses were conducted using SPSS, Version 26.0 (SPSS Inc., Chicago, IL, USA).
Results
Baseline information
A total of 502 eligible patients were finally analyzed in this study, including 52 cases in refracture group with an average age of 78.74 ± 8.00 years, and 450 cases in non- refracture group with an average age of 68.86 ± 10.17 years. Univariate analysis showed no significant differences between the two groups in gender, history of hypertension and diabetes, hormone use, initial fracture site, prealbumin, serum calcium, serum phosphate, serum magnesium concentration, and blood glucose. Statistical differences were found in age (P < 0.001), height (P = 0.003), weight (P < 0.001), BMI (P = 0.007), BMD (P < 0.001), interval from the initial fracture to surgery (P < 0.001), pain scale (P < 0.001), hemoglobin (P < 0.001), and total protein (P = 0.041) (Table 1).
The median interval from initial fracture to refracture in the 52 patients with refracture was 25 months. The proportion of such patients who had a refracture within the 1st, 2nd, 3rd, and 4th year of the initial fracture was 34.6%, 13.5%, 21.2%, and 21.2%, respectively, with the risk of refracture significantly decreasing and stabilizing after 4 years. Approximately half (48%) and 2/3 (69%) of the refractures occurred within 2 and 3 years (Table 2).
Logistic regression of refracture
Significant variables (age, height, weight, BMI, BMD, interval from the initial fracture to surgery, pain scale, hemoglobin, total protein) in univariate analysis were further included in binary logistic regression. The results revealed that age (P = 0.002), pain scale (P < 0.001) and interval from the initial fracture to surgery (P < 0.001) were independent risk factors of osteoporotic refracture (Fig. 2, Table 3).
A plot of the time between initial fracture injury and surgery versus the probability of refracture shows that the longer the time between initial fracture injury and surgery, the greater the likelihood of refracture (Fig. 3).
Cox proportional hazards model of refracture
Significant variables (age, height, weight, BMI, BMD, interval from the initial fracture to surgery, pain scale, hemoglobin, total protein) in univariate analysis were further included in Cox proportional hazards model. The Cox model identified significant associations between osteoporotic refracture and age (P = 0.016), pain scale (P < 0.001) and interval from the initial fracture to surgery (P < 0.001) (Table 4).
Incidence of refracture was 10.4% (52/502) in our study. As shown in Fig. 4, Kaplan–Meier survival analysis suggested positive correlations between osteoporotic refracture and age (P < 0.05) (Fig. 4A), pain scale (P < 0.05) (Fig. 4B) and interval from the initial fracture to surgery (P < 0.05) (Fig. 4C).
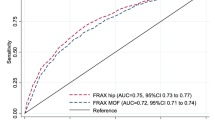
The predictive value of interval from injury to operation after the initial fracture on refracture
ROC curve was used to further determine the influence of risk factors on osteoporotic refracture, and the results supported a high prediction accuracy of interval time, with area under ROC (AUC) of 0.782, sensitivity of 63.5%, specificity of 84.4%. Besides, threshold value of 10.5 indicated that the incidence of osteoporotic refracture would increase when operation time exceeding 10.5 days after the initial fracture injury (Fig. 5, Table 5).
Discussion
It is well-known that as a leading cause of fractures, osteoporosis has both high morbidity and mortality all over the world13,14,15. In recent years, a growing body of evidence suggests that osteoporotic refracture is closely related to treatments, surgical type and sarcopenia. Levy et al.16 enrolled 250 patients with initial vertebral fractures and divided them into four groups: surgery only group, medication only group, surgery combined with medication group, and no treatment group. Their results showed that surgery could not reduce the risk of vertebral refracture, but the combination of medication and surgery might shorten the time to refracture. A retrospective study of Chen et al.17 conducted multivariate analysis and confirmed that sarcopenia was closely related to osteoporosis, and sarcopenia and paraspinal muscles were independent risk factors for osteoporotic refracture. However, no known empirical research has focused on exploring the impact of the interval from injury to operation after the initial fracture on osteoporotic refracture. Therefore, this study compared refracture patients with non-refracture patients and mainly explored the risk factors of osteoporotic refracture.
A limited number of researchers have investigated vertebral re-fractures, ultimately finding that early surgical intervention significantly reduces the incidence of vertebral re-fractures compared to delayed surgery18,19. This finding aligns with our perspective. One retrospective study (N = 62) compared early (≤ 4 weeks, n = 36) versus delayed (> 4 weeks, n = 26) intervention, demonstrating significantly lower 6-month refracture rates in the early group (8.3% vs 34.6%, P < 0.01) at the follow-up of 6 months20. The second study (N = 51) with 1.2-year follow-up similarly found reduced secondary fracture risks with early percutaneous kyphoplasty (PKP) (32 vs 19 cases)21. However, both investigations presented notable methodological constraints that warrant cautious interpretation of results. Primarily, the limited cohort sizes (N = 62 and N = 51 respectively) substantially restricted statistical power for detecting subtle between-group differences. Furthermore, the relatively abbreviated follow-up durations (≤ 1.2 years) potentially compromised the capacity to assess long-term complication patterns, particularly given the chronic nature of osteoporosis-related skeletal fragility. These methodological shortcomings collectively undermine the generalizability and conclusive strength of the reported temporal advantages of early PKP implementation. In contrast to these prior investigations, the current study demonstrates substantially greater statistical validity through both an expanded cohort size and prolonged follow-up duration, thereby providing stronger evidence regarding clinical outcomes.
Our study implied no differences between refracture and non-refracture in gender, history of hypertension and diabetes, hormone use, initial fracture site, prealbumin, serum calcium, serum phosphate, serum magnesium concentration, and blood glucose. However, statistical differences were found in age, height, weight, BMI, BMD, interval from the initial fracture to surgery, pain scale, hemoglobin, and total protein. Further binary logistic regression and Cox proportional hazard regression both proved that only age, pain scale and interval from the initial fracture to surgery were the independent risk factors of osteoporotic refracture.
Advanced age critically exacerbates osteoporotic fracture risk through synergistic deteriorations in skeletal and systemic homeostasis. Aging disrupts bone remodeling by reducing osteoblast activity and increasing osteoclast-mediated resorption, leading to progressive bone loss and microarchitectural degradation, notably cortical thinning and trabecular deterioration22. Concurrently, sarcopenia—age-related declines in muscle mass and strength—impairs balance, elevates fall risk, and disrupts muscle-bone crosstalk, as diminished mechanical loading from atrophied muscles further accelerates bone resorption23. These processes are amplified by chronic low-grade inflammation ("inflamm-aging"), characterized by dysregulated IL-6, TNF-α, and NF-κB signaling, which suppress bone formation, enhance osteoclastogenesis, and delay fracture healing24. Together, impaired remodeling, sarcopenia-driven biomechanical failure, and inflammatory dysregulation converge to reduce skeletal resilience, necessitating multifactorial interventions targeting bone-muscle interactions and inflammatory pathways in the elderly.
Post-fracture pain severity and delayed surgical intervention synergistically elevate refracture risk through interconnected biological and behavioral pathways. Severe pain contributes to reduced mobility, limiting weight-bearing activities essential for bone remodeling and accelerating disuse-induced bone loss25. Chronic pain further disrupts skeletal homeostasis via neuroendocrine dysregulation: sympathetic overactivation drives β2-adrenergic receptor-mediated osteoblast suppression and osteoclast activation through norepinephrine excess, while HPA axis dysfunction elevates cortisol levels, compounding bone formation deficits26. Concurrently, pain-induced gait instability and analgesic-related central nervous system impairment (e.g., opioid use) heighten fall susceptibility, particularly in vertebral or hip fracture patients27. Furthermore, the high level of pain might be due to long-term dangerous weight-bearing, these patients themselves are relatively weak in health awareness and unable to control their own bad behaviors. The specific reasons need to be further verified.
It is worth noting that the prediction accuracy of interval from the initial fracture to surgery was high, with area under ROC (AUC) of 0.782, sensitivity of 63.5%, specificity of 84.4%, and threshold value of 10.5. The interval between fracture and surgery critically impacts outcomes. Early surgical intervention preserves fracture-site vascularity, optimizing callus formation and healing capacity. Delays, however, promote fibrotic tissue accumulation, prolong inflammatory bone resorption, and extend immobility-related BMD declines (0.5–1% weekly) and sarcopenia progression28. Prolonged inflammation shifts from acute osteogenic signaling to chronic osteoclast dominance, while delayed mechanical stabilization increases secondary fall risks, particularly during the high-risk first post-fracture month29,30. Therefore, in this critical period, we recommend that patients should take surgery as soon as possible to prevent the occurrence of adverse consequences such as refracture.
In addition, some studies have shown that women with a history of osteoporotic fractures have an increased risk of refractures, with the highest risk within two years after the first fracture31,32. Balasubramanian et al.33 collected massive data of female patients with fracture and reported that 10% of patients had refracture within 1 year after the first fracture, 18% within 2 years, and 31% within 5 years. Patients with previous fractures and underlying diseases are at high risk of refracture, so it is necessary to apply refracture prevention in order to reduce mortality and rate of refracture, as well as to lower medical costs34,35. Our results demonstrated that 34.6% and 48.1% patients had refractures within 1 year and 2 years after the initial fractures, separately. Thus, the duration of secondary prevention of osteoporotic refracture should be at least more than 2 years after the initial fracture.
There are some limitations in this study. Firstly, the retrospective single-center design of this study limits both the statistical power (due to a small sample size) and the external validity of the findings. Secondly, potential confounding factors (e.g., patient activity levels, fall history, adherence to anti-osteoporotic medication, smoking and alcohol consumption) were not controlled for. Thirdly, while our study achieved statistical significance for key predictors (surgical timing, pain score, age), the limited sample size in the refracture group (n = 52) warrants cautious interpretation. Therefore, a prospective, multicenter, and large-sample study is needed to further confirm the results of this study.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- BMI:
-
Body mass index
- BMD:
-
Bone mineral density
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under ROC
- COPD:
-
Chronic obstructive pulmonary disease
- SD:
-
Standard deviation
- PKP:
-
Percutaneous kyphoplasty
References
Anam, A. K. & Insogna, K. Update on osteoporosis screening and management. Med. Clin. North Am. 105, 1117–1134. https://doi.org/10.1016/j.mcna.2021.05.016 (2021).
Goldstein, C. L., Chutkan, N. B., Choma, T. J. & Orr, R. D. Management of the elderly with vertebral compression fractures. Neurosurgery 77(Suppl 4), S33-45. https://doi.org/10.1227/neu.0000000000000947 (2015).
Barron, R. L., Oster, G., Grauer, A., Crittenden, D. B. & Weycker, D. Determinants of imminent fracture risk in postmenopausal women with osteoporosis. Osteoporos. Int. 31, 2103–2111. https://doi.org/10.1007/s00198-020-05294-3 (2020).
Kanis, J. A., Johnell, O., Oden, A., Johansson, H. & McCloskey, E. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos. Int. 19, 385–397. https://doi.org/10.1007/s00198-007-0543-5 (2008).
Burge, R. et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J. Bone Miner. Res. 22, 465–475. https://doi.org/10.1359/jbmr.061113 (2007).
Pike, C. T. et al. Prevalence and costs of osteoporotic patients with subsequent non-vertebral fractures in the US. Osteoporos. Int. 22, 2611–2621. https://doi.org/10.1007/s00198-010-1494-9 (2011).
Baim, S. & Blank, R. Approaches to fracture risk assessment and prevention. Curr. Osteoporos. Rep. 19, 158–165. https://doi.org/10.1007/s11914-021-00659-x (2021).
Saag, K. G. & Geusens, P. Progress in osteoporosis and fracture prevention: focus on postmenopausal women. Arthritis Res. Ther. 11, 251. https://doi.org/10.1186/ar2815 (2009).
Lidar, S. et al. Sarcopenia is an independent risk factor for subsequent osteoporotic vertebral fractures following percutaneous cement augmentation in elderly patients. J. Clin. Med. 11, 5778. https://doi.org/10.3390/jcm11195778 (2022).
Lin, W. C. et al. Refractures in cemented vertebrae after percutaneous vertebroplasty: A retrospective analysis. Eur. Spine J. 17, 592–599. https://doi.org/10.1007/s00586-007-0564-y (2008).
Sriruanthong, K., Philawuth, N., Saloa, S., Daraphongsataporn, N. & Sucharitpongpan, W. Risk factors of refracture after a fragility fracture in elderly. Arch. Osteoporos. 17, 98. https://doi.org/10.1007/s11657-022-01143-4 (2022).
Zhao, C. et al. The effects of biomechanical factors on adjacent vertebral compression fractures after percutaneous kyphoplasty: A propensity score matching analysis. Osteoporos. Int. 33, 1795–1806. https://doi.org/10.1007/s00198-022-06428-5 (2022).
Kanis, J. A., Cooper, C., Rizzoli, R. & Reginster, J. Y. Executive summary of the European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Calcif. Tissue Int. 104, 235–238. https://doi.org/10.1007/s00223-018-00512-x (2019).
Johnston, C. B. & Dagar, M. Osteoporosis in Older Adults. Med. Clin. North Am. 104, 873–884. https://doi.org/10.1016/j.mcna.2020.06.004 (2020).
Yong, E. L. & Logan, S. Menopausal osteoporosis: Screening, prevention and treatment. Singapore Med. J. 62, 159–166. https://doi.org/10.11622/smedj.2021036 (2021).
Levy, H., Seydafkan, S., Rice, J. D., Easley, K. A. & Tangpricha, V. Comparative efficacy of vertebroplasty, kyphoplasty, and medical therapy for vertebral fractures on survival and prevention of recurrent fractures. Endocr. Pract. 18, 499–507. https://doi.org/10.4158/ep11349.Or (2012).
Chen, Q. et al. Relationship between sarcopenia/paravertebral muscles and the incidence of vertebral refractures following percutaneous kyphoplasty: A retrospective study. BMC Musculoskelet. Disord. 23, 879. https://doi.org/10.1186/s12891-022-05832-6 (2022).
Phillips, F. M. et al. Early radiographic and clinical results of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Spine 28, 2260–2265. https://doi.org/10.1097/01.BRS.0000085092.84097.7B (2003).
Nieuwenhuijse, M. J., van Erkel, A. R. & Dijkstra, P. D. Percutaneous vertebroplasty for subacute and chronic painful osteoporotic vertebral compression fractures can safely be undertaken in the first year after the onset of symptoms. J. Bone Joint. Surg. Br. 94, 815–820. https://doi.org/10.1302/0301-620X.94B6.28368 (2012).
Zhou, X. et al. Early versus late percutaneous kyphoplasty for treating osteoporotic vertebral compression fracture: A retrospective study. Clin. Neurol. Neurosurg. 180, 101–105. https://doi.org/10.1016/j.clineuro.2019.03.029 (2019).
Minamide, A. et al. Early versus delayed kyphoplasty for thoracolumbar osteoporotic vertebral fractures: The effect of timing on clinical and radiographic outcomes and subsequent compression fractures. Clin. Neurol. Neurosurg. 173, 176–181. https://doi.org/10.1016/j.clineuro.2018.07.019 (2018).
Wölfel, E. M. et al. Senescence of skeletal stem cells and their contribution to age-related bone loss. Mech. Ageing Dev. 221, 111976. https://doi.org/10.1016/j.mad.2024.111976 (2024).
Osawa, Y. et al. Longitudinal association between muscle and bone loss: Results of US and Japanese cohort studies. J. Cachexia Sarcopenia Muscle. 15, 746–755. https://doi.org/10.1002/jcsm.13438 (2024).
Tao, H. et al. Urolithin A suppresses RANKL-induced osteoclastogenesis and postmenopausal osteoporosis by, suppresses inflammation and downstream NF-κB activated pyroptosis pathways. Pharmacol. Res. 174, 105967. https://doi.org/10.1016/j.phrs.2021.105967 (2021).
He, B. et al. Effect of surgical timing on the refracture rate after percutaneous vertebroplasty: A retrospective analysis of at least 4-year follow-up. Biomed. Res. Int. 27, 5503022. https://doi.org/10.1155/2021/5503022 (2021).
Elefteriou, F. Regulation of bone remodeling by the central and peripheral nervous system. Arch. Biochem. Biophys. 473, 231–236. https://doi.org/10.1016/j.abb.2008.03.016 (2008).
Daoust, R. et al. Recent opioid use and fall-related injury among older patients with trauma. CMAJ 190, E500–E506. https://doi.org/10.1503/cmaj.171286 (2018).
Herrmann, M. et al. Interactions between muscle and bone-where physics meets biology. Biomolecules 10, 432. https://doi.org/10.3390/biom10030432 (2020).
Stavre, Z. et al. Schnurri-3 inhibition suppresses bone and joint damage in models of rheumatoid arthritis. Proc. Natl. Acad. Sci. USA 120, e2218019120. https://doi.org/10.1073/pnas.2218019120 (2023).
Santosa, K. B. et al. Higher amounts of opioids filled after surgery increase risk of serious falls and fall-related injuries among older adults. J. Gen. Intern. Med. 35, 2917–2924. https://doi.org/10.1007/s11606-020-06015-6 (2020).
Bonafede, M. et al. Predicting imminent risk for fracture in patients aged 50 or older with osteoporosis using US claims data. Arch. Osteoporos. 11, 26. https://doi.org/10.1007/s11657-016-0280-5 (2016).
Söreskog, E. et al. Risk of major osteoporotic fracture after first, second and third fracture in Swedish women aged 50 years and older. Bone 134, 115286. https://doi.org/10.1016/j.bone.2020.115286 (2020).
Balasubramanian, A. et al. Risk of subsequent fracture after prior fracture among older women. Osteoporos. Int. 30, 79–92. https://doi.org/10.1007/s00198-018-4732-1 (2019).
Cummings, S. R. & Eastell, R. Risk and prevention of fracture in patients with major medical illnesses: A mini-review. J. Bone Miner. Res. 31, 2069–2072. https://doi.org/10.1002/jbmr.3030 (2016).
Osuna, P. M., Ruppe, M. D. & Tabatabai, L. S. Fracture liaison services: Multidisciplinary approaches to secondary fracture prevention. Endocr. Pract. 23, 199–206. https://doi.org/10.4158/ep161433.Ra (2017).
Funding
This study was supported by Wuxi Funds for Science and Technology Development [grant number Y20222020]; General Program of Wuxi Medical Center of Nanjing Medical University [grant number WMCG202515]; Wuxi Funds for Science and Technology Development [grant number K20231052].
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Z.X., Y.L. and P.W.. The first draft of the manuscript was written by Z.X. and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The institutional review board of Nanjing Medical University Affiliated Wuxi People’s Hospital approved this retrospective study (2023-KY23100). This is a retrospective anonymised data collecting data on patients with osteoporotic fractures. The identity of the patients cannot be revealed.Due to the retrospective nature of the study, Research Ethics Committee of Wuxi People’s Hospital waived the need of obtaining informed consent.
Consent for publication
In this study, there were no images or data that would reveal the patient’s identity. Following this journal instructions, there is no need in this case to perform informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, Z., Wang, P., Qiu, Y. et al. Association between timing of surgery and refracture after initial osteoporotic fractures. Sci Rep 15, 19925 (2025). https://doi.org/10.1038/s41598-025-04672-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-04672-3