Abstract
Burns are among the most common injuries throughout history, and their treatment varies depending on the severity. Third-degree burns, the most severe and deadly type, cause numerous fatalities worldwide each year but can be treated using the skin mesh grafting technique—one of the latest advancements in burn care. However, an optimal skin mesh geometry has not yet been identified. This study aims to determine the best geometrical design for skin meshes by minimizing average stress, using Abaqus software for numerical analysis and extracting the hyperelastic mechanical properties of skin used in mesh grafts. Hyperelastic properties of healthy and meshed skin were obtained through uniaxial tensile tests, and different geometries were analyzed using Abaqus. The optimal mesh geometry was then determined using genetic algorithms in Abaqus and MATLAB. A rectangular mesh, measuring 1.939 mm in length and 1.698 mm in width, was identified as the best design with an average stress of 0.0757 MPa. These findings have potential applications in clinical burn research, contributing to the development of improved treatment methods.
Similar content being viewed by others
Introduction
The skin is the body’s first line of defense and the largest single organ. In addition to shielding the body from harm, it helps regulate body temperature through sweating and synthesizes vitamin D1,2. Despite its relatively thin average thickness of about 2 millimeters, the skin plays a crucial role in maintaining overall health3. Burns, caused by factors such as electric shock, is one of the main threats to skin integrity. Burns can vary in severity, and the deeper the burn, the more layers of skin are damaged4,5,6. According to the World Health Organization, around 300,000 people die from burn-related injuries each year, a significant and concerning figure4. Skin grafting is a common treatment for burns, where healthy skin from an undamaged area of the patient’s body is transplanted to the injured site7,8. Grafted skin is often meshed to reduce the amount of healthy skin required9,10,11,12,13,14,15,16,17. Depending on the thickness of the grafted skin, this procedure is classified into two types: split-thickness and full-thickness grafts18,19,20. However, an optimal mesh design, in terms of geometry, has not yet been identified. This study aims to determine the best geometric shape for skin graft meshes, focusing on minimizing stress distribution across the skin.
Historical research indicates that skin grafting was first practiced as a treatment for severe skin injuries in Egypt around 1500 BCE20. The technique was further developed in India and eventually spread to Europe by the first century CE20,21. Over the past 200 years, research in this field has seen considerable progress. In 1872, a study assessed the optimal amount of skin to harvest for grafting. Skin samples ranging from 4 to 8 cm² and extending to part of the dermis were compared with other grafting methods to evaluate their benefits20,22.
In 2014, researchers investigated the different tools available for meshing grafted skin and the mesh ratios they produced23. Mesh ratio refers to the extent to which stretched grafted skin can cover an area larger than its original surface23. A 2017 study explored the relationship between mesh ratios and patient demographics, such as age and gender, providing further insight into their effects on skin graft outcomes24.
Recent research has also focused on developing polymer-based skin meshes. In 2022, a study identified the optimal shape for minimizing maximum stress among nine different polymeric mesh samples25. Another study in 2023 used biaxial tensile tests on silicone skin models with various mesh patterns, generating stress-strain curves for each design26. A further study in 2023 investigated the effect of cutting synthetic skin samples into rectangular meshes at different angles27.
Despite these advances, an ideal geometric design for skin graft meshes has not been determined. In this study, we aim to find the optimal mesh geometry through numerical optimization. First, the mechanical properties of the skin were measured. Then, using Abaqus software and MATLAB, we developed an optimization code based on genetic algorithms to identify the most suitable mesh design in terms of geometry.
Materials and methods
Extraction of mechanical properties
Sample preparation
Healthy and meshed skin samples were obtained from Razi Hospital in Rasht (Fig. 1a, b). After being removed from the patient’s body, the samples were placed in 0.9% normal saline solutions and sent to the laboratory in insulated packaging with ice. The tests were conducted within 8 h. During the testing, the samples were kept in 0.9% normal saline at 37 °C to maintain their biological conditions. Figure 1 shows images of both samples before sectioning.
Loading procedure
For the tests, a Santam STM-1 tensile testing machine was used, which has a precision of 0.05 Newtons. Data was recorded every 0.003 min, and at the end of the test, data related to displacement and force were retrieved from the machine. After placing each sample in the testing device (Fig. 1c), a pre-load of 0.1 Newtons was applied along the axis to achieve a suitable flat shape, which provides meaningful measurements. The samples were also subjected to 5 cyclic loads of 10% of the final strain. The machine speed was set to 0.02 mm per second for quasi-static tensile testing. This loading rate corresponds to pseudostatic conditions, which have been employed in previous studies to characterize nonlinear hyperelastic properties28,29.
Figure 1c shows a view of the meshed sample under tension in the device.
Numerical simulation
Geometry extraction
The skin is modeled as a rectangular prism with a length of 80 millimeters, a width of 20 millimeters, and a thickness of 0.2 millimeters. The thickness of the skin was selected based on the average thickness of the skin samples obtained for the experiments. In this study, skin meshes with various shapes were initially considered, including horizontal rectangles, vertical rectangles, horizontal rhombuses, and vertical rhombuses.
Boundary condition
For the boundary conditions, no mesh is considered within 21.5 millimeters from the top and 21.5 millimeters from the bottom. In the space up to 20 millimeters above the lowest part of the shape, all degrees of freedom are fixed to keep the shape stationary from the bottom. Additionally, displacement is considered 2 millimeters below the highest point of the shape. Figure 2 shows an illustration of these boundary conditions on the object as rendered in the software.
The material properties were determined based on the mechanical properties extracted from skin tests. For extracting isotropic tissue properties using uniaxial data, the skin tissue was modeled as a hyperelastic, incompressible, homogeneous, and isotropic material.
Based on various hyperelastic models30,31, an appropriate isotropic hyperelastic model was selected to describe the mechanical properties of the samples. The chosen model is the optimized Yeoh model, which can be used in many numerical software packages.
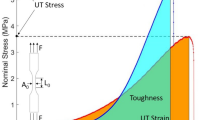
After obtaining the data from the device following the tests, which include displacement in millimeters and force in Newtons, stress and strain can be calculated using the relationships provided below32,33:
where F is the force, A is the cross-sectional area, ΔL is the change in length, and L0 is the initial length of the sample.
The Yeoh model is based on a strain energy density function that is a series of powers of the strain invariants I1, I2, and I3 in the Cauchy-Green deformation tensor34. The strain energy function and its corresponding Cauchy stress are as follows:
where c1, c2, and c3 are the model constants, and λ is the stretch.
All uniaxial data were fitted to the above model using the nonlinear Levenberg-Marquardt algorithm, and the parameters of the constitutive models were determined for each dataset.
Details of numerical solutions
In this study, Abaqus 2021 (Dassault Systemes Simulia Corp., Providence, RI, USA) was utilized. Tetrahedral meshes were employed for shape analysis due to their greater flexibility in handling complex geometries. Although hexahedral elements often yield higher accuracy in many cases, their application here was constrained by the geometric complexity. Nevertheless, mesh sensitivity analysis confirmed that the density of the tetrahedral mesh was adequate to ensure accurate and reliable results.
Additionally, to address the potential issue of volumetric locking, which can occur in incompressible materials, we used hybrid meshes and ensured mesh independence. As a result, this issue did not arise during the software simulations.
After performing mesh independence checks, the element size was set to 0.5 millimeters for all shapes. Additionally, as previously mentioned, degrees of freedom for displacement and rotation in all three directions were fixed in the region specified in Fig. 2, which is 21.5 millimeters from the bottom. This ensured that this part was completely fixed, and displacement was considered in the vertical direction from the highest point of the skin down to 21.5 millimeters below it.
Optimization
The model analyzed in this study includes two variable parameters: L1, the length of the meshes and L2, their width (Fig. 2). Based on previous research and the reliability of the von Mises stress value as an indicator, this parameter was selected as the cost function for optimization, with the objective of minimizing it to identify the optimal mesh configuration.
To achieve the optimal dimensions for the skin mesh, an optimization process using the Genetic Algorithm (GA) was implemented in Python 3.9. GA is an iterative approach to solving constrained and unconstrained optimization problems based on natural biological evolution. In this algorithm, a population of individuals is continuously produced. In this study, 50% of the new generation consists of crossover children, 33% from elite parents, and 17% from mutations. The initial population size was 60 individuals. The dimensions of these individuals were randomly set within a range of 1 to 2 millimeters for the length and width of the meshes. The evolution process continued for a total of 250 generations, with the goal of minimizing the average stress.
In this study, to perform numerical optimization for determining the best geometric dimensions, the length and width of rectangular meshes, as well as the horizontal and vertical diameters of rhombic meshes, were considered as the chromosomes in each generation of the optimization algorithm.
Figure 3 shows the process of finding the best sample based on the genetic algorithm pattern for this study, where L3 is the width of the skin sample, L4 is the length of the skin sample, and w is the thickness of the skin sample.
Results and discussion
Mechanical properties extraction
In this study, 5 samples of healthy skin and 7 samples of meshed skin were subjected to uniaxial tensile testing. The thickness of the samples for both healthy and meshed skin was 0.2 millimeters. Based on the data from the uniaxial tensile tests conducted in this research, stress-strain curves for the samples were plotted. Figure 4 displays the curve for healthy skin, while Fig. 5 shows the curve for meshed skin. It is noteworthy that the properties of healthy skin were used to evaluate various mesh patterns for the skin. The average elastic modulus for the unmeshed and meshed skin samples was found to be 25.815 ± 7.0984 MPa and 5.337 ± 2.298 MPa, respectively, indicating that meshing reduces the skin’s strength. Then, the stress-strain curves were fitted using the Yeoh model in MATLAB, and the model constants were extracted (Tables 1 and 2). As indicated by the R² values, the samples were well-fitted to the Yeoh model.
In this study, both human skin and meshed skin were mechanically characterized. Due to their high water content and fibrous structure, all samples were considered incompressible materials35. Additionally, the samples were assumed to be isotropic and hyperelastic, with their mechanical behavior best described by the Yeoh model.
Both tissue types exhibited the well-known “stiffening” behavior commonly observed in many soft biological tissues. Under the isotropy assumption, this nonlinear response was accurately captured by the Yeoh model.
In general, the uniaxial tests indicate that healthy skin is stiffer than meshed skin. Up to the point of rupture, the mechanical response of skin in the axial direction is largely influenced by the exposure and behavior of collagen fibers within the different skin layers. Collagen serves as the primary load-bearing component under tension, and once it begins to tear, no other structural elements remain to support the load. In contrast, elastin fibers play a key role in the initial stages of stretching. At higher strain levels, collagen becomes more critical than elastin in resisting deformation. Therefore, both collagen and elastin are essential contributors to the mechanical stretching behavior of meshed skin.
The mechanical characterization results of skin tissues can be applied to study pathogenic and clinical conditions related to skin burns, aiding in the development of appropriate treatment strategies. The constitutive model coefficients were utilized in Abaqus for simulation as the material properties of the models.
Numerical simulation
First, a mesh sensitivity analysis was performed to ensure the reliability of the results. As the mesh dimensions increase, the available surface area for tetrahedral meshing decreases. To address this, the maximum seed size for the largest skin mesh dimensions was calculated to achieve the desired mesh quality.
As shown in Fig. 6, the number of elements varied from 17,619 to 84,335, and the maximum von Mises stress showed significant variation with mesh size. Specifically, between 17,619 and 33,212 elements, the results varied considerably—within approximately ± 15%. However, beyond 33,212 elements and up to 84,335 elements, the difference in stress results became negligible, with variations less than ± 5%. Consequently, the mesh containing 65,124 elements (element size 0.5 mm) was deemed sufficiently accurate and computationally efficient for further analysis.
To perform the optimization, simulations of skin mesh with different geometric shapes were first conducted. The selected geometric shapes were horizontal rectangle, vertical rectangle, horizontal rhombus, and vertical rhombus. Figure 7 shows images of the results for each of the 4 shapes with a displacement of 2 millimeters.
Finally, the shapes with a 2 mm displacement can be summarized as follows:
Ultimately, based on the results obtained in Table 3, the rectangular horizontal mesh shape was found to be the best model for the mesh. Therefore, it is expected that the horizontal rectangular mesh performs better than other shapes in terms of average stress. As shown in Table 4, the horizontal rectangular mesh indeed exhibits the best average stress. As mentioned, in this study, the length and width of rectangular meshes, as well as the horizontal and vertical diameters of rhombic meshes, were analyzed to determine the optimal geometric dimensions. The results showed that a rectangular mesh with a length of 1.939 mm and a width of 1.698 mm was optimal, yielding an average stress of 0.0757 MPa. Additionally, a rhombic mesh with a horizontal diameter of 1.946 mm and a vertical diameter of 1.485 mm was optimal, yielding an average stress of 0.0816 MPa. The stress contours for these models are shown in Figs. 8 and 9.
Tables 4 and 5 illustrate the average stress for three different mesh dimensions. The dimensions listed in the first row of both tables represent the optimal dimensions identified for the meshes. As shown in Tables 4 and 5, the average stress varies with changes in the orientation of the meshes. Although the meshes are square-shaped, rotating them by 45 degrees results in significantly different average stress values. Under these conditions, the skin exhibits a distinctly altered response. However, it remains unclear whether changing the mesh angles improves the skin’s reaction to tension.
A rectangle measuring 1 mm by 1 mm-effectively a square mesh with one side aligned along the x-axis-shows a higher average stress compared to the same mesh rotated by 45 degrees, which forms a rhombus with 1 mm sides. Furthermore, the tables demonstrate that smaller mesh sizes do not necessarily produce better results than larger ones. In some cases, larger mesh openings actually enhance the skin’s performance under uniaxial tension.
Conclusion
This study aimed to identify the optimal mesh shape for grafted skin and determine the best dimensions for this geometry. Our results demonstrate that a horizontal rectangular mesh provides the best performance, exhibiting the lowest maximum von Mises stress. This finding was achieved through comparative analysis of horizontal rectangular, vertical rectangular, vertical rhomboid, and horizontal rhomboid geometries using ABAQUS software.
The key findings of this study are:
-
The shape of the mesh significantly influences stress distribution during tension.
-
Rotating square meshes by 45° leads to a substantial change in average stress.
-
A rectangular mesh aligned with the x-axis experiences higher stress compared to the same mesh rotated 45°, which forms a rhombus.
-
Smaller mesh sizes do not necessarily produce better results.
A few limitations of this work should be acknowledged. First, only isotropic graft models were studied, and the effects of skin anisotropy were not investigated. Second, the graft models were not tested under very high strains, and their fracture properties were not characterized. Third, all experiments were conducted at a constant strain rate. To improve the accuracy of future studies, we recommend increasing the population size in the genetic algorithm. Additionally, expanding the number of experimental tests to better characterize both healthy and damaged skin properties, as well as exploring additional mesh geometries and analyzing them through software, could further refine the optimization process and enhance results. The findings of this research will be invaluable for surgeons aiming to improve the success of burn surgeries.
Data availability
Data will be made available on request from the corresponding author.
References
Choe, C. et al. Human skin in vivo has a higher skin barrier function than Porcine skin ex vivo—comprehensive Raman microscopic study of the stratum corneum. J. Biophotonics. 11 (6), e201700355 (2018).
Joodaki, H. & Panzer, M. B. Skin mechanical properties and modeling: A review. Proc. Inst. Mech. Eng. Part H: J. Eng. Med. 232 (4), 323–343. (2018).
Wilkinson, P. & Millington, R. Skin (Digitally Printed Version ed) (Cambridge University Press, 2009).
Eylert, G. et al. Skin regeneration is accelerated by a lower dose of multipotent mesenchymal stromal/stem cells—a paradigm change. Stem Cell Res. Ther. 12 (1), 1–11 (2021).
Perez-Valle, A., Amo, C. D. & Andia, I. Overview of current advances in extrusion Bioprinting for skin applications. Int. J. Mol. Sci. 21 (18), 6679 (2020).
Vandeput, J. et al. A review of skin meshers. Burns 21 (5), 364–370 (1995).
Johnson, T. M., Ratner, D. & Nelson, B. R. Soft tissue reconstruction with skin grafting. J. Am. Acad. Dermatol. 27 (2), 151–165 (1992).
Al Shlash, S. O. et al. Demographic characteristics and outcome of burn patients requiring skin grafts: a tertiary hospital experience. Int. J. Burns Trauma. 6 (2), 30 (2016).
Narayan, N., Shivaiah, R. & Kumar, K. M. A novel technique of collagen application over meshed split thickness graft for wound coverage. Int. J. Surg. Med. 7 (4), 54–54 (2021).
Skouge, J. W. Techniques for split-thickness skin grafting. Dermatol. Surg. 13 (8), 841–850 (1987).
Arnljots, B. & Svedman, P. Irrigation treatment in split-thickness skin grafting of intractable leg ulcers. Scand. J. Plast. Reconstr. Surg. 19 (2), 211–213 (1985).
Horan, T. C. & Emori, T. G. Definitions of key terms used in the NNIS system. Am. J. Infect. Control. 25 (2), 112–116 (1997).
Kohlhauser, M. et al. Historical evolution of skin grafting—a journey through time. Medicina 57 (4), 348 (2021).
Yuan, J. et al. Computational models for the determination of depth-dependent mechanical properties of skin with a soft, flexible measurement device. Proc. Royal Soc. A: Math. Phys. Eng. Sci. 472 (2194), p20160225 (2016).
Singh, G., Gupta, V. & Chanda, A. Artificial skin with varying biomechanical properties. Mater. Today Proc. 62, 3162–3166 (2022).
Oh, S. J. A systematic review of the scalp donor site for split-thickness skin grafting. Archives Plast. Surg. 47 (06), 528–534 (2020).
Bogdanov, S. B. et al. Total full-thickness skin grafting for treating patients with extensive facial burn injury: A 10-year experience. Burns 47 (6), 1389–1398 (2021).
Adams, D. C. & Ramsey, M. L. Grafts in dermatologic surgery: review and update on full-and split‐thickness skin grafts, free cartilage grafts, and composite grafts. Dermatol. Surg. 31, 1055–1067 (2005).
Herndon, D. N. Principles and Practice of Burn Surgery (CRC, 2004).
Singh, M. et al. Evolution of skin grafting for treatment of burns: reverdin pinch grafting to Tanner mesh grafting and beyond. Burns 43 (6), 1149–1154 (2017).
Hauben, D. J., Baruchin, A. & Mahler, D. On the history of the free skin graft. Ann. Plast. Surg. 9 (3), 242–246 (1982).
Davis, J. S. The story of plastic surgery. Ann. Surg. 113 (5), 641–656 (1941).
Lyons, J. L. & Kagan, R. J. The true meshing ratio of skin graft meshers. J. Burn Care Res. 35 (3), 257–260 (2014).
Pripotnev, S. & Papp, A. Split thickness skin graft meshing ratio indications and common practices. Burns 43 (8), 1775–1781 (2017).
Gupta, V. & Chanda, A. Biomechanics of skin grafts: effect of pattern size, spacing and orientation. Eng. Res. Express. 4 (1), 015006 (2022).
Gupta, V., Singh, G. & Chanda, A. High expansion auxetic skin graft simulants for severe burn injury mitigation. Eur. Burn J. 4 (1), 108–120 (2023).
Gupta, V., Singla, R. & Chanda, A. Development and characterization of novel anisotropic skin graft simulants. Dermato 3 (2), 114–130 (2023).
Rassoli, A. et al. Quantification and comparison of the nonlinear mechanical properties of transcutaneous and human aortic valve leaflets: experimental and numerical studies. Mech. Mater. 188, 104872 (2024).
Rassoli, A. et al. Comparison of tensile properties of xenopericardium from three animal species and finite element analysis for bioprosthetic heart valve tissue. Artif. Organs. 44 (3), 278–287 (2020).
Holzapfel, G. A. et al. Large strain analysis of soft biological membranes: formulation and finite element analysis. Comput. Methods Appl. Mech. Eng. 132 (1–2), 45–61 (1996).
Holzapfel, G. A., Gasser, T. C. & Ogden, R. W. A new constitutive framework for arterial wall mechanics and a comparative study of material models. J. Elast. Phys. Sci. Solids. 61, 1–48 (2000).
Huston, R. & Josephs, H. Practical Stress Analysis in Engineering Design (CRC, 2008).
Lubliner, J. Plasticity Theory (Courier Corporation, 2008).
Rivlin, R. S. Some applications of elasticity theory to rubber engineering, in Collected Papers of RS Rivlin: Volume I and II. Springer. 9–16. (1997).
Ogden, R. W. & Holzapfel, G. A. Mechanics of Biological Tissue (Springer, 2006).
Acknowledgements
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
M.K: Writing – original draft, Software, Resources, Methodology, Validation. A.R: Writing – review & editing, Supervision, Conceptualization. A.K: Writing – review & editing, Supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Research ethics and patient consent
The human skin samples used in this study were obtained from the Razi Hospital in Rasht, Iran. Informed consent was obtained from the families of the patients prior to sample collection. The research team was granted authorization to use these samples by the National Institute of Medical Research Development of Iran, under approval letter number IR.NIMAD.REC.1401.030. All methods were carried out in strict accordance with relevant guidelines and regulations, including those outlined in the Declaration of Helsinki. Additionally, all experimental protocols were reviewed and approved by the Ethics Committee of the National Institute of Medical Research Development (NIMAD) of Iran.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Khayami, M., Rassoli, A. & Feizkhah, A. Optimal geometrical selection of skin mesh: experimental analysis and numerical optimization. Sci Rep 15, 21263 (2025). https://doi.org/10.1038/s41598-025-04829-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04829-0