Abstract
The Pediatric Quality of Life Inventory™ (PedsQL™) family impact module is a widely used tool for assessing the health-related quality of life (HRQoL) of caregivers of children with chronic illnesses; however, it has not been available in Swahili. This study aimed to translate, culturally adapt, and validate the Swahili version of the PedsQL family impact module (FIM) among caregivers of children with heart disease in Tanzania. As a secondary aim, the study explored differences in caregiver HRQoL between those whose children had undergone surgery and those who had not, using the newly translated tool. A cross-sectional survey was conducted among 204 primary caregivers at a national cardiac referral centre. Standardised translation and adaptation procedures were followed. Psychometric evaluation included internal consistency reliability, construct validity through known-groups comparisons, and effect size estimation. The Swahili version demonstrated excellent internal consistency (Cronbach’s α = 0.99) and good construct validity. Socioeconomic status was the only consistent predictor of HRQoL in multivariable models. Caregivers in the operated group consistently reported higher HRQoL scores, highlighting the potential benefit of surgical intervention on family well-being. These findings strongly support the Swahili PedsQL FIM as a culturally appropriate and psychometrically sound tool. It offers promise for clinical care and future outcome evaluations in similar settings.
Similar content being viewed by others
Introduction
Children born with congenital heart disease (CHD) are increasingly surviving into adolescence and adulthood due to advances in diagnosis and treatment1,2. As survival rates improve, families become central to long-term care, often facing ongoing emotional, social, and economic stress3,4,5,6,7,8. Understanding the impact of chronic diseases such as CHD on families is critical to improving both clinical outcomes and caregiver well-being9.
The Pediatric Quality of Life Inventory™ (PedsQL™) family impact module (FIM) was developed to assess how chronic pediatric illness affects parents and family functioning10. It measures caregiver-reported outcomes across emotional, physical, social, and cognitive domains, including communication, worry, and daily activities. The FIM has been translated and validated in various languages, such as Spanish, Turkish, Persian, and Chinese, demonstrating strong psychometric performance in diverse populations. However, no Swahili version currently exists11,12,13,14.
Over 100 million people across East and Central Africa speak Swahili. Despite this, few validated caregiver-reported tools are available in Swahili. Instruments developed in English often fail to capture Swahili-speaking caregivers’ cultural and contextual realities, limiting their applicability. Without culturally adapted tools, understanding the psychosocial impact of chronic illness in these populations is challenging15.
International guidelines from the MAPI Research Trust and the ISPOR Task Force emphasise rigorous methodologies for translating and validating outcome measures. These include forward–backwards translation, expert panel review, cognitive debriefing, and psychometric testing to ensure linguistic and conceptual equivalence16,17. Applying these standards ensures the tool’s cultural relevance and reliability.
This study, therefore, aimed to translate, culturally adapt, and validate the Swahili version of the PedsQL™ family impact module for use among caregivers of children with heart disease in Tanzania. The primary objective was to assess its linguistic appropriateness and psychometric properties, including internal consistency and construct validity using the known-groups method. As a secondary, exploratory objective, we employed the newly translated tool to examine whether caregiver-reported health-related quality of life (HRQoL) differed between families of children who had undergone cardiac surgery and those who had not. This sub-analysis is particularly relevant in low- and middle-income countries (LMICS), where access to pediatric cardiac surgery remains limited. Many children remain unoperated due to systemic delays, financial barriers, or infrastructure constraints. In such contexts, caregivers often bear prolonged burdens with little psychosocial support. Validated tools like the Swahili FIM provide a framework for assessing caregiver needs, informing family-centred care, and guiding policies that support families navigating the long course of pediatric heart disease.
We hypothesised that family functioning and caregiver quality of life would be lower among families of children awaiting surgical correction, compared to those whose children had already received intervention.
Methods
Study design
The cross-sectional descriptive study was conducted between September and December 2022 and was approved by the Ethics Review Committee of Jakaya Kikwete Cardiac Institute (JKCI), Tanzania (Ref no: AB.123/307/01H/40). The study adhered to the ethical principles of the 1975 Declaration of Helsinki. Written informed consent was obtained from all participants. Consent to translate and use the PedsQL™ FIM was obtained from the MAPI Research Trust.
Study setting
The study was conducted at JKCI in Dar es Salaam, the national cardiac referral centre serving over 60 million Tanzanians and individuals from neighbouring countries. The pediatric outpatient clinic operates five days a week and sees approximately 30 children daily.
Recruitment of study participants
Primary caregivers were eligible if they had a child aged 2–18 years with a confirmed diagnosis of CHD, either awaiting or having undergone curative or palliative surgery more than 6 months prior. Caregivers of children with syndromes, significant comorbidities, or cognitive impairments were excluded. Parents of children under the age of 2 years were also excluded to enhance the specificity of the burden analysis. Participants were recruited while waiting for medical care and interviewed in private rooms by trained research assistants who spoke native Swahili, under the supervision of the first authors. Informed consent was obtained from all legal guardians of the recruited children with CHD prior to enrollment.
Sample size and data collection
A total of 204 caregivers were enrolled: 100 had children who underwent surgery, while 104 did not. The sample size was calculated to detect a 5-point difference in HRQoL scores with 80% power and a 5% significance level, requiring at least 92 per group. Face-to-face interviews lasting 15–20 min were conducted to eliminate literacy bias.
PedsQL family impact module
The PedsQL™ family impact module (FIM) Version 2.0 is a 36-item parent-proxy instrument designed to assess the impact of chronic pediatric illness on caregiver and family functioning. It comprises eight subscales: physical functioning (6 items), emotional functioning (5 items), social functioning (4 items), cognitive functioning (3 items), communication (3 items), worry (5 items), daily activities (3 items), and family relationships (7 items). Two summary scores are derived from the tool. The Parent Health-Related Quality of Life (HRQoL) Summary Score is based on 26 items drawn from the first six subscales (physical, emotional, social, cognitive, communication, and worry), while the Family Functioning Summary Score includes 10 items from the daily activities and family relationships subscales. Responses are recorded on a 5-point Likert scale ranging from 0 (“never a problem”) to 4 (“almost always a problem”), which are reverse-scored and linearly transformed to a 0–100 scale. Higher scores indicate better functioning and a lower perceived impact. A total score is computed when more than 50% of items are completed, in accordance with the instrument’s standard scoring protocol10.
Clinical and sociodemographic variables
Sociodemographic and clinical data included caregiver age, gender, education, child age, diagnosis, surgical history, and residence. Disease complexity was classified according to the Bethesda system18, and heart failure severity was assessed using the Ross classification19. Socioeconomic status was measured using an adapted WAMI index suited to the Tanzanian context (Supplementary File 4).
Statistical analysis
Data were collected using REDCap and analyzed with SPSS version 28. Descriptive statistics summarised participant characteristics. Internal consistency was assessed using Cronbach’s alpha, with a threshold of ≥ 0.70 accepted for group-level comparisons20. Construct validity was established through the known-groups method. This method compares scale scores across groups expected to differ in the measured construct—in this instance, caregiver-reported HRQL. Surgical status (operated vs. unoperated) served as the known grouping variable, based on the expectation that caregivers of children who underwent surgery would report higher HRQL. Group differences were assessed using independent two-sided t-tests, with a 5-point difference in mean scores deemed clinically meaningful. Effect sizes were calculated using Cohen’s d and interpreted as small [0.2], medium [0.5], or large [0.8]21. Predictors of caregiver HRQL were evaluated using generalized linear models (GLM) with backwards elimination. Variables included in the initial model were socioeconomic status (SES), child age, gender, operative status, and age at surgery. Model assumptions were checked and satisfied prior to final analysis.
Results
Translation and cross-cultural adaptation
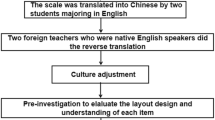
The translation process adhered to the guidelines of the MAPI Research Trust10. Two independent bilingual Swahili speakers with healthcare backgrounds translated English into Swahili. Their translations, T1 and T2, were reconciled into a single draft, which was then back-translated by a third individual, T3. A fourth translator, fluent in English and without prior exposure to the tool, conducted a back-translation to the original tool. A fifth reviewer compared the back-translated and original English versions to assess semantic and conceptual equivalence. An expert evaluated both semantic and conceptual equivalence. A preliminary version was pilot-tested with ten caregivers during cognitive debriefing interviews, who confirmed clarity, cultural appropriateness, and ease of understanding. No major revisions were required. These steps established face and content validity.
Sociodemographic characteristics of study participants
A total of 204 primary caregivers of children with CHD completed the Swahili PedsQL™ family impact module (FIM). Table 1 summarizes participant characteristics. The majority were mothers (74.0%), with an average of 9.5 ± 3.6 years of schooling, and most resided in Dar es Salaam (53.9%). The mean socioeconomic status (SES) score was 0.68 ± 0.17. The operated and unoperated groups were comparable across most variables, except for SES (higher in the operated group, p = 0.015) and child age (older in the operated group, p < 0.001).
Internal consistency reliability
The Swahili PedsQL™ FIM demonstrated high internal consistency reliability. Cronbach’s alpha for the total impact score was 0.99, parent HRQoL 0.91, and family functioning 0.81—exceeding acceptable thresholds for group comparison. Some individual subscales (e.g., communication: α = 0.36; emotional functioning: α = 0.67) fell below 0.70. However, all item-total correlations exceeded 0.30, and no items were identified as redundant. Therefore, no items were removed from the final version (Table 2).
Construct validity: known-groups analysis
Table 2 displays the results of construct validity using the known-groups method by comparing mean scores on the Swahili PedsQL™ family impact module between caregivers of children who underwent cardiac surgery and those whose children did not. The mean total impact score was 91.5 (SD = 10.4) for the operated group and 84.8 (SD = 11.9) for the unoperated group (mean difference = 6.7, p < 0.001; Cohen’s d = 0.60). The parent HRQoL summary score was 89.8 (SD = 11.8) for the operated group and 80.8 (SD = 14.3) for the unoperated group (mean difference = 9.1, p < 0.001; d = 0.69). Subscale effect sizes varied from 0.08 (communication) to 0.71 (emotional functioning). Differences in family functioning summary scores were 4.1 points (p = 0.066; d = 0.26). The subscales for daily activities and family relationships showed mean differences of 3.9 and 4.2 points, respectively.
Predictors of caregiver health-related quality of life
Multivariable analysis (Table 3) identified higher SES and having a child who had undergone surgery as significant predictors of better caregiver HRQoL (both p < 0.001). No significant associations were found for disease complexity, number of lesions, medication use, or parental education level.
Finalization of Swahili FIM
Based on findings from cognitive debriefing, internal consistency testing, and construct validity analysis, the Swahili version of the PedsQL™ FIM was finalized without item modification. It is now a culturally appropriate and psychometrically sound tool for assessing family impact in Swahili-speaking populations.
Discussion
This study aimed to translate, culturally adapt, and validate the Swahili version of the PedsQL™ family impact module (FIM) for caregivers of children with congenital heart disease (CHD) in Tanzania. Following internationally recognized guidelines—including forward–backwards translation, expert panel review, and cognitive debriefing—the tool was adapted to the local context. Caregivers confirmed that the translated version was clear, culturally relevant, and reflected their caregiving experiences, thereby establishing both content and face validity.
In terms of reliability, the Swahili PedsQL™ FIM demonstrated strong internal consistency, with Cronbach’s alpha values exceeding 0.80 for total and summary scores. However, several subscales—including physical functioning, cognitive functioning, communication, worry, and daily activities—had alpha values falling below the 0.70 threshold. Importantly, all item-total correlations were above 0.30, supporting the choice to retain all items. These findings align with validation studies conducted in Brazil and the United States, where similar subscale-level limitations and ceiling effects were observed19,22,23. As emphasized by the tool’s original developers, subscales are primarily intended for descriptive use, while total and summary scores provide the most robust psychometric interpretation. Although refinements such as larger sample sizes or item modifications may improve subscale reliability in future studies, structural changes were not pursued in our context. Our aim was to establish linguistic and psychometric equivalence with the original tool rather than alter its composition.
With respect to construct validity, caregivers of children who had undergone cardiac surgery reported higher overall scores on the Swahili PedsQL™ FIM compared to those whose children had not undergone surgery. The most pronounced differences were observed in emotional functioning and parent HRQoL summary scores, both of which demonstrated moderate to large effect sizes. Smaller differences were seen in family functioning domains such as daily activities and family relationships, while the communication subscale showed minimal variation between the two groups. These results are broadly consistent with previous studies using the English version of the PedsQL™ FIM, which also found that the tool could distinguish between caregiver groups based on clinical or treatment status. For instance, Varni et al.10 reported that caregivers of children undergoing active cancer treatment reported lower HRQoL than those in post-treatment phases22. Similarly, the Brazilian validation study found meaningful score differences based on illness severity19. These parallels suggest that the Swahili version performs comparably in differentiating family impact across clinically relevant subgroups.
These findings were further examined in relation to specific subscale performance and contextual interpretation. In our context, the modest differences observed in family functioning subscales—despite differences in surgical status—may reflect the enduring nature of caregiving in CHD, where families continue to experience disruptions to daily life even after surgical intervention23,24. Additionally, the limited variation in the communication domain may suggest that caregivers’ unmet needs in understanding and discussing their child’s condition persist regardless of treatment history25. These patterns highlight the potential utility of the FIM for identifying caregiver burden that remains even after medical intervention. Although our study focused on construct validity using the known-groups method, this is a well-established approach for initial validation of translated instruments. Future research may build on this by assessing additional psychometric properties, such as test–retest reliability to establish stability over time, and factor analysis to confirm whether the theoretical structure of the tool holds in the Swahili-speaking context26,27,28.
The translation process was not without challenges. Certain terms—particularly those describing emotional states or abstract concepts like “cognitive strain”—did not have direct Swahili equivalents. Achieving clarity while preserving meaning required careful language adaptation and expert consultation. While no changes were made to the structure or content of the translated items during cognitive debriefing, some caregivers, especially those with limited formal education, needed further clarification during interviewer-administered sessions. This underscores the importance of using trained interviewers and flexible administration formats in low-literacy settings to ensure accurate comprehension and consistent data quality.
The findings of this study also provide insight into the practical applicability of the Swahili PedsQL™ FIM in local healthcare settings. Caregivers generally found the tool to be acceptable and culturally appropriate during cognitive debriefing. However, several contextual factors may affect its routine use. First, while comprehensive, the tool’s length may pose challenges in high-volume outpatient clinics where time is limited. Although interviewer administration helped address literacy barriers in this study, implementing it in everyday practice would require trained personnel and dedicated time, which may not always be feasible in overstretched healthcare systems.
Second, while the tool captures multiple domains of family functioning, some constructs, such as worry or communication, may carry different connotations in Tanzanian cultural contexts than in Western settings where the tool was originally developed. For example, emotional expression and family decision-making are often shaped by extended family structures, religious beliefs, and community norms, which may influence how caregivers respond to certain items. Although no major issues were reported during debriefing, future use of the tool in diverse regions within East Africa may reveal areas where cultural tailoring could further enhance its sensitivity and relevance29.
Despite these limitations, the Swahili PedsQL™ FIM fills an important gap by providing a standardized, family-centred outcome measure in a language spoken by over 100 million people across the region. Its use could support more holistic assessments in pediatric cardiac care by helping providers identify psychosocial burdens that may otherwise go unaddressed. To maximize its utility, integration into clinic workflows, digital platforms, or community-based follow-up programs should be explored in future implementation studies.
Looking ahead, the next steps include obtaining licenses for clinical and research use of the Swahili PedsQL™ FIM and disseminating it through academic and healthcare networks. Future research should assess the responsiveness of the Swahili PedsQL™ FIM to clinical changes, especially through longitudinal studies that follow surgical or psychosocial interventions. Additional validation in other chronic pediatric conditions would help determine its broader applicability. Subscales with lower reliability, such as communication, may benefit from item refinement or expansion. Implementation studies are also needed to explore how the tool can be feasibly integrated into routine care, potentially through digital formats or shorter versions. These steps will help ensure the tool’s continued relevance in both clinical and research contexts across Swahili-speaking populations.
Data availability
Data from this study will be made available upon request to corresponding Author Naizihijwa Majani.
References
Hoffman, J. I. & Kaplan, S. The incidence of congenital heart disease. J. Am. Coll. Cardiol. 39(12), 1890–1900 (2002).
Gregory, M. R. B., Prouhet, P. M., Russell, C. L. & Pfannenstiel, B. R. Quality of life for parents of children with congenital heart defect: A systematic review. J. Cardiovasc. Nurs. 33, 363–371 (2018).
Jackson, A. C., Frydenberg, E., Liang, R. P., Higgins, R. O. & Murphy, B. M. Familial impact and coping with child heart disease: A systematic review. Pediatr. Cardiol. 36, 695–712 (2015).
Wray, J. et al. Psychosocial functioning of parents of children with heart disease—Describing the landscape. Eur. J. Pediatr. 177, 1811–1821 (2018).
Sood, E. et al. Parent mental health and family functioning following diagnosis of CHD: A research agenda and recommendations from the Cardiac Neurodevelopmental Outcome Collaborative. Cardiol. Young 31, 900–914 (2021).
Wei, H., Roscigno, C. I., Hanson, C. C. & Swanson, K. M. Families of children with congenital heart disease: A literature review. Heart Lung 44, 494–511 (2015).
Bratt, E.-L. & Moons, P. Forty years of quality-of-life research in congenital heart disease: Temporal trends in conceptual and methodological rigor. Int. J. Cardiol. 195(C), 1–6 (2015).
Silbert, A. R., Newburger, J. W. & Fyler, D. C. Marital stability and congenital heart disease. Pediatrics 69(6), 747–750 (1982).
Tesson, S. et al. Psychological interventions for people affected by childhood-onset heart disease: A systematic review. Health Psychol. 38, 151–161 (2019).
Varni, J. W., Sherman, S. A., Burwinkle, T. M., Dickinson, P. E. & Dixon, P. The PedsQL™ family impact module: preliminary reliability and validity. Health Qual. Life Outcomes 2, 1–6 (2004).
Ortega, J., Vázquez, N., Caro, I. A. & Assalone, F. Psychometric properties of the Spanish version of the pediatric quality of life inventory family impact module (pedsql FIM). An. Pediatr. (Engl. Ed.) 98(1), 48–57 (2023).
Memik, N. C., Agaoglu, B., Coskun, A., Uneri, O. S. & Karakaya, I. The validity and reliability of the Turkish pediatric quality of life inventory for children 13–18 years old. Turk Psikiyatr Dergisi 18(4), 353 (2007).
Amiri, P. et al. Validity and reliability of the Iranian version of the pediatric quality of life inventory™ 4.0 (PedsQL™) generic core scales in children. Health Qual. Life Outcomes 10, 1–9 (2012).
Chen, R., Hao, Y., Feng, L., Zhang, Y. & Huang, Z. The Chinese version of the pediatric quality of life inventory™ (PedsQL™) family impact module: Cross-cultural adaptation and psychometric evaluation. Health Qual. Life Outcomes 9, 1–10 (2011).
Haywood, K. et al. Patient and public engagement in health-related quality of life and patient-reported outcomes research: What is important and why should we care? Findings from the first ISOQOL patient engagement symposium. Qual. Life Res. 24, 1069–1076 (2015).
Giroudet, C. et al. When should translations of clinical outcome assessments (COAS) be considered obsolete? Recommendations from MAPI’S translations life expectancy working group. Value Health 19(7), A391 (2016).
Wild, D. et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: Report of the ISPOR task force for translation and cultural adaptation. Value Health 8(2), 94–104. https://doi.org/10.1111/j.1524-4733.2005.04054.x (2005).
Bredy, C. et al. New York Heart Association (NYHA) classification in adults with congenital heart disease: Relation to objective measures of exercise and outcome. Eur. Heart J. Qual. Care Clin. Outcomes 4(1), 51–58 (2018).
Scarpelli, A. C. et al. The pediatric quality of life inventory™ (PedsQL™) family impact module: Reliability and validity of the Brazilian version. Health Qual. Life Outcomes 6, 35 (2008).
Novick, M. & Lewis, G. Coefficient alpha and the reliability of composite measurements. Psychometrika 32, 1–13 (1967).
Cohen, J. Statistical Power Analysis for the Behavioural Sciences (Academic Press, 2013).
McHorney, C. A., Ware, J. E., Lu, J. F. R. & Sherbourne, C. D. The MOS 36-item short-form health survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med. Care 32, 40–66 (1994).
Mano, K. E., Khan, K. A., Ladwig, R. J. & Weisman, S. J. The impact of pediatric chronic pain on parents’ health-related quality of life and family functioning: Reliability and validity of the PedsQL 4.0 family impact module. J. Pediatr. Psychol. 36, 517–527 (2011).
Goldbeck, L. The impact of newly diagnosed chronic paediatric conditions on parental quality of life. Qual. Life Res. 15(7), 1121–1131 (2006).
DeMaso, D. R. et al. The impact of maternal perceptions and medical severity on the adjustment of children with congenital heart disease. J. Pediatr. Psychol. 16(2), 137–149 (1991).
Streiner, D. L., Norman, G. R. & Cairney, J. Health Measurement Scales: A Practical Guide to Their Development and Use (Oxford University Press, 2024).
Beaton, D. E., Bombardier, C., Guillemin, F. & Ferraz, M. B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 25(24), 3186–3191 (2000).
Terwee, C. B. et al. Quality criteria were proposed for the measurement properties of health status questionnaires. J. Clin. Epidemiol. 60(1), 34–42 (2007).
Acquadro, C., Conway, K., Hareendran, A., Aaronson, N., European Regulatory Issues and Quality of Life Assessment (ERIQA) Group. Literature review of methods to translate health-related quality of life questionnaires for use in multinational clinical trials. Value Health 11(3), 509–521 (2008).
Acknowledgements
This study received partial funding from the Jo Kolk Study Foundation, Scholten-Cordes Fonds, van Wijck-Stam-Casperson, and the Hendrik Muller Fonds; we acknowledge them. The authors would also like to thank the Pediatric Cardiology, Surgery, and Critical Care Department of JKCI for their continuous care of children with heart disease. We thank Peter Zuithoff from the Julius Centre for Health Sciences and Primary Care for his assistance with statistics. We also thank the JKCI perfusionists, especially Sophia Mlonga, for their help in retrieving postoperative data. We acknowledge and appreciate the contributions of Rachel Leonce and Naftaly Godfrey to the data collection.
Author information
Authors and Affiliations
Contributions
NM and JK contributed equally to this paper. NM is a PhD candidate who developed the research topic, participated in the study design and data collection, and rewrote the initial draft of the manuscript. JK was involved in the study design, collected and analysed data, and drafted the initial manuscript. ZK and NL carried out the data collection. JH offered essential insights into QOL research and provided critical feedback on the results. DN, SM, SK, GS, and VM engaged in a critical review, discussion, and feedback on the manuscript draft. PK, DG, MS, PC, and MJ provided significant input on the manuscript drafts and offered mentorship on the data analyses. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Majani, N.G., Koster, J.R., Nkya, D. et al. Translation and validation of the Swahili pediatric quality of life family impact module for caregivers of children with congenital heart disease. Sci Rep 15, 20935 (2025). https://doi.org/10.1038/s41598-025-04838-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04838-z