Abstract
Understanding changes in the quality of life (QoL) and its risk factors can facilitate identify individuals who may benefit from transcatheter aortic valve replacement (TAVR). However, the relationships between frailty, mental health, cardiac function, and QoL in patients after TAVR have not been well-studied. From February 2022 to November 2023, 396 patients who underwent TAVR were selected as a convenience sample. A structural equation model was used to validate the hypothesized model. We employed descriptive statistics, Spearman correlation coefficients, independent-sample t-test, and one-way ANOVA analysis to determine direct correlations. Bootstrapping analysis was used to evaluate the indirect effects. In patients who underwent TAVR, QoL was negatively correlated with NYHA class and frailty phenotype. Specifically, frailty had a statistically direct impact on patients’ mental health (β = 0.237, 95% CI 0.068 to 0.365, p < 0.01) and QoL (β=−0.375, 95% CI −0.524 to 0.193, p < 0.01). Also, patients’ mental health (β = 0.159, 95% CI 0.031 to 0.30, p < 0.05) and cardiac function (β=−0.356, 95% CI −0.599 to −0.168, p < 0.01) showed significant direct effects on QoL. Meanwhile, patients’ mental health played a mediating role in the relationship between frailty and QoL (β = 0.038, 95% CI 0.006 to 0.072, p < 0.05) in patients after TAVR. Future initiatives to raise patients’ awareness of frailty before and after TAVR, especially by considering the possible impact of mental health other than just anxiety and depression, may improve the overall QoL after TAVR. More extensive prospective trials, including psychological interventions tailored to patients after TAVR, are required.
Similar content being viewed by others
Introduction
Transcatheter aortic valve replacement (TAVR) has emerged as an effective minimally invasive treatment option for patients suffering from severe aortic valve stenosis (AS) and aortic regurgitation (AR). These patients are deemed high-risk for surgical aortic valve replacement1. Nowadays, TAVR has experienced rapid advancement, driven by innovative technological breakthroughs and strong clinical evidence emerging across the world. Quality of life (QoL) is a crucial factor in predicting treatment effectiveness and has significant prognostic value, making it extremely important in medical decision-making2. Changes in QoL may better reflect patients’ experiences during disease progression and treatment-related complications. This, in turn, may lead to refinements and enhancements in treatment approaches and patient care3. Although the Placement of Aortic Transcatheter Valves (PARTNER) trial4 and another study5 have demonstrated an improvement in QoL for patients after TAVR, there remains a dearth of systematic and comprehensive research exploring the trajectory of QoL over time for those who have undergone TAVR.
Frailty is one of the most prevalent factors that influence the QoL of patients after TAVR. It not only has a major effect on the recovery ability of these older patients6,7 but also acts as a risk factor leading to poor outcomes. Such outcomes include longer hospital stays, disabilities, and even death after the TAVR procedure8,9,10. Significantly, frailty has been identified as an independent factor that can predict a deteriorating QoL. It was found that the risk of frail patients not having an improvement in their QoL one year after TAVR was two times higher than that of non-frail patients11,12. As a general concept, frailty is a clinical condition characterized by reduced capacities in multiple physiological systems, determining a state of increased vulnerability to negative psychological conditions like anxiety or depression and susceptibility to adverse health-related QoL13.
As reported from a worldwide study involving 40 countries, poorer cardiac function characterized by the New York Heart Association (NYHA) class had a strong correlation to poorer health-related QoL of heart failure patients14. Heart failure patients with complex life demands would lead to adverse psychosocial stressors not merely anxiety and depression15. Meanwhile, anxiety and depression are established predictors of adverse clinical outcomes in elderly cardiovascular patients with multiple comorbidities, significantly compromising their QoL16,17,18. Currently, less is known about how mental health is related to TAVR. This includes the prevalence of depression and anxiety during the TAVR perioperative period in real-world situations, as well as the outcomes after TAVR that are associated with the patient’s baseline mental health status19. Based on findings from other settings, it can be inferred that depression in TAVR patients is connected with a variety of functional declines, particularly manifesting as frailty, reduced mobility, and impaired QoL19. Surman et al. outlined specific prospective outcomes related to depression, frailty, and QoL in TAVR patients. Nonetheless, this finding did not go deeper into exploring the inherent relationships and mechanisms among these three factors20.
To fill these knowledge gaps, we aimed to investigate the relationships and figure out the interaction mechanisms between frailty, mental health, cardiac function, and QoL after TAVR procedures. Our conceptual framework (Fig. 1) posits three core hypotheses for patients who had TAVR. First of all, we assumed that frailty had a direct negative influence on mental health and QoL, while cardiac function had a direct positive influence on mental health and QoL for these patients. Secondly, we supposed that the mental health of patients after TAVR had a direct negative influence on their QoL. Thirdly, we hypothesized that frailty indirectly influenced the QoL of patients after TAVR through the mediating role of their mental health. Additionally, we also hypothesized that patients’ cardiac function indirectly influenced their QoL by the effects of mental health.
Methods
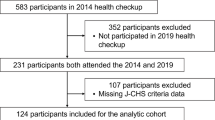
Study design, setting, and participants
This study was a cross-sectional descriptive study designed to evaluate the interconnections among frailty, cardiac function, mental health, and QoL. It took place at a public hospital in Sichuan Province, China.
A total of 396 patients who had undergone TAVR were selected as convenience samples in this study from February 2022 to November 2023. Patients were eligible for inclusion if (1) they were elderly with severe calcified stenosis of the aortic valve; (2) they had symptoms like palpitation, exertional dyspnea, angina, chest pain, heart failure, syncope, a history of presyncope, or presyncope during exercise testing; (3) they were asymptomatic severe AS with a left ventricular ejection fraction (LVEF) < 55% (in the absence of left ventricular systolic dysfunction caused by other incentives); (4) they were AS patients<70 years old who were at high risk of surgical procedures or have other risk factors, such as those who have had chest radiotherapy, suffer from liver failure, have severe diffuse aortic calcification, or are extremely frail21. Patients with mental diseases who were unable to communicate were excluded from the study.
Measurement instruments and variables
Exogenous variable: frailty
Frailty was measured using the Frailty Phenotype (FP), the initial and most widely used assessment scale for providing an operational definition of physical frailty. This scale consists of 5 items, with at least three of the five criteria required to diagnose frailty: gait speed over 5 m, grip strength, weight loss, self-reported exhaustion, and inactivity22. If a patient meets only one or two of these criteria, they are classified as pre-frailty, while meeting none is categorized as non-frailty. Frailty is diagnosed when three or more criteria are met.
Endogenous variable: quality of life
The short-form health survey 12 (SF-12) is a shortened version of the SF-36 Health Survey from the United States. It provides a more concise alternative to assess the QoL23. The SF-12 is scored on a 0-100 scale containing 12 items that contribute to two components: the physical component summary (PCS-12) and the mental component summary (MCS-12). Raw scores from each item response have to be linearly transformed to a 0-100 scale to calculate PCS-12 and MCS-12 scores24.
Endogenous variable: mental health
Mental health was measured utilizing the Hospital Anxiety and Depression Scale (HADS), which is a commonly employed brief screening instrument in hospital settings to detect emotional disorders25,26. It comprises 14 items, of which seven items are used to assess the anxiety dimension (HADS-A), and the remaining seven are applied to assess the depression dimension (HADS-D). Each item is rated on a 4-point Likert scale ranging from 0 to 3. A raw score exceeding 8 suggests a mild disorder, while a score surpassing 10 indicates a moderate disorder.
Endogenous variable: heart functional status
The patients’ cardiac functional status was evaluated using the NYHA class27 and brain natriuretic peptide (BNP) levels28. The NYHA class is widely used in clinical practice to assess the degree of heart failure. It comprises four classifications ranging from class I, indicating no physical limitations during activity, to class IV, indicating symptoms present even when the patient is at rest. BNP and the aminoterminal part of its pro-hormone (NT-pro-BNP) are cardiac hormones mainly secreted by ventricular cardiomyocytes. They have the property of vasodilation and can help reduce preload and afterload. The levels of these hormones are correlated with myocardial wall stress and the severity of AS29.
Data collection and ethical considerations
Our study adhered to the Declaration of Helsinki guidelines30. Approval was granted by the Ethics Committee of the West China Hospital (2022 Review No. 909). We obtained the informed consent of every participant before the study initiation. On the second day after the TAVR operation, once the study’s purpose had been thoroughly explained, eligible participants independently completed the baseline demographic survey and self-report questionnaires (SF-12, FP, and HADS scale). They did this without any interruption or guidance. The NYHA class and the NT-pro-BNP values were extracted from the electronic medical records before the operation. Out of 423 potential patients, 396 consented to take part in the study, yielding a response rate of 93.6%.
Statistical analysis and model testing
We employed IBM SPSS Statistics (version 24.0; made by IBM, Chicago, IL, USA) and Amos (version 20.0; made by IBM, Chicago, Illinois, USA) to perform the statistical analysis. A p-value < 0.05 was regarded as statistically significant. Continuous variables were presented as mean ± standard deviation or were described in the median and interquartile range (IQR), while categorical variables were expressed as frequency and the percentage distribution within each group. We conducted a Spearman correlation analysis to examine the relationships between all the variables. Additionally, independent-sample t-test and one-way ANOVA were conducted to explore the differences in the main variables of interest among different sociodemographic groups.
A structural equation model (SEM) was utilized to validate the hypothesized model and yielded the path coefficients of the factors. The goodness-of-fit index of SEM and their acceptable threshold levels were reported to evaluate the appropriateness of the hypothesized model31. The χ2/degrees of freedom ratio (df) < 3.0, the goodness-of-fit index (GFI) > 0.9, the adjusted goodness-of-fit index (AGFI) > 0.9, the root mean square error of approximation (RMSEA) < 0.08, the nonstandard fit index (NFI) > 0.9, the relative fit index (RFI) > 0.9, the incremental fit index (IFI) > 0.9, the Tucker-Lewis index (TLI) > 0.9, and the comparative fit index (CFI) > 0.9 indicate a well-fitting structural model32,33,34,35. In addition, we adopted bootstrapping analysis with a sample size of 2000 to estimate indirect pathways36.
Results
Demographic characteristics
In our study, most respondents were male (60.1%) and resided in urban areas (65.4%). The mean age of all the patients, male patients, and female patients was 72.03 (SD 7.06), 72.59 (SD 7.33), and 71.19 (SD 6.55) years, respectively. The majority of patients who did not report experiencing a history of syncope (90.2%) were in a partnered relationship (88.4%) and exhibited abnormal NT-pro-BNP levels (90.9%). More than half of the patients (52.8%) had a normal BMI. Among all the patients with cardiovascular disease, only 32.8% had more than five comorbidities. Concerning the NYHA class, a large proportion of the patients (55.8%) were grouped into level II or lower, while the rest were at level III or higher. Nearly half of the patients (48.2%) were classified as having a pre-frailty phenotype. Table 1 shows the demographic profile of the participants.
The profiles for all the variables of interest
Specifically, the means and standard deviations for total SF-12, PCS-12, MCS-12, HADS-A, and HADS-D were 50.29 (SD 20.035), 33.32 (SD 23.931), 67.14 (SD 22.764), 4.51 (SD 2.469), 4.19 (SD 2.497), respectively. Details are presented in (Table 2). The median value of NT-pro-BNP was 1962.5 (interquartile range [IQR] 567 to 4859.75). The mean scores of HADS-A and HADS-D indicated that there were no significant levels of anxiety and depression in the patients. There were statistically significant differences in the scores of total SF-12, PCS-12, and MCS-12 when grouped by NYHA class and frailty phenotype. Regarding HADS-A and HADS-D, they had statistically significant differences when considering factors like frailty phenotype, age groups, and history of syncope.
Relationships among frailty, QoL, mental health, and cardiac function
The Spearman correlation analysis revealed statistically significant positive correlations between the NYHA class and the NT-pro-BNP value (r = 0.172, P < 0.01), the NYHA class and frailty (r = 0.225, P < 0.01), and between the NT-pro-BNP value and frailty (r = 0.110, P < 0.05). Additionally, positive correlations were observed between the NYHA class and the HADS-D scores (r = 0.106, P < 0.05), and between frailty and both the HADS-A scores (r = 0.221, P < 0.01) and HADS-D (r = 0.191, P < 0.01). In contrast, all the scores of the total SF-12, the PCS-12, and the MCS-12 were negatively correlated with the NYHA class and frailty. This implies that patients with poorer heart function, as indicated by a higher NYHA class, and those with a frailty phenotype generally had a lower QoL. These results are presented in (Table 2).
Testing of the hypothesized model
In summary, the fit index (χ2[114] = 452.55, p < 0.01, NFI = 0.989, RFI = 0.973, IFI = 1.005, TLI = 1.011, CFI = 1.00, RMSEA < 0.01) of the examined model yielded a good fit to our data. As illustrated in Fig. 2, among all the eight path coefficients within the structural model under examination, all but two were statistically significant. The exceptions were the path coefficient directly linking cardiac function to mental health and the indirect path coefficient from cardiac function to QoL.
Standardized coefficients of the structural equation model. **P < 0.05; HADS-D the hospital anxiety and depression scale-depression dimension, HADS-A the hospital anxiety and depression scale-anxiety dimension, NYHA the New York heart association class, BNP brain natriuretic peptide, NT-pro-BNP the aminoterminal part of BNP’s pro-hormone, SF-12 the short-form health survey 12, PCS-12 the physical component summary of SF-12, MCS-12 the mental component summary of SF-12.
To be specific, frailty had a statistically direct effect on patients’ mental health (β = 0.237, 95% CI 0.068 to 0.365, p < 0.01) and QoL (β=-0.375, 95% CI -0.524 to 0.193, p < 0.01). Similarly, both patients’ mental health (β = 0.159, 95% CI 0.031 to 0.30, p < 0.05) and cardiac function (β=-0.356, 95% CI -0.599 to -0.168, p < 0.01) showed significant direct effects on QoL. When we modeled patients’ mental health as a mediator, the results of the bootstrapping analysis indicated that it significantly mediated the relationship between frailty and QoL (β = 0.038, 95% CI 0.006 to 0.072, p < 0.05). Conversely, it did not impact the relationship between cardiac function and QoL (β = 0.009, 95% CI -0.019 to 0.064, p > 0.05). Table 3 illustrates the standardized total, direct, and indirect effects of the structural equation model we examined.
Discussion
Given the increasing number of TAVR procedures being performed worldwide and the expanding availability of this treatment option, gaining insights into patients’ experiences and post-procedure outcomes is of great importance. To the best of our knowledge, our study is the first to examine the relationships between frailty, mental health, cardiac function, and QoL in patients with TAVR. We found that the relationship between frailty and QoL was mediated by the effect on patients’ mental health.
In our study, male patients outnumbered female patients. Most of the patients were older than 65 years, which is consistent with the findings from a nationwide study in the United States37. Our findings revealed that among females, the group with lower SF-12 scores and PCS-12 scores tended to be more common compared to males. This suggests that tailored interventions based on gender differences might be necessary38. There were significant between-group differences in the HADS-A and HADS-D scores among patients of different ages. This highlights the complex biological process of aging, which may make individuals more prone to depression or anxiety disorders39. Furthermore, robust evidence indicates that the occurrence of syncope, angina, or other symptoms, along with increased blood levels of BNP/NT-pro-BNP, can predict the rapid progression of AS process29,40,41. Although only a small proportion of our participants had experienced syncope, most of them reported abnormal NT-pro-BNP levels. It is well-established that unpredictable and sudden syncope episodes could trigger anxiety and depression42. However, caution is warranted when interpreting the differences in the HADS-A, HADS-D, and MCS-12 scores between the two groups due to the sample size disparity. Conflicting findings have been reported regarding the association between elevated BNP/NT-proBNP levels and adverse outcomes after TAVR, with some studies supporting the association while others do not43,44,45. It has been speculated that low BNP/NT-proBNP levels in patients with AS may indicate an underdeveloped compensatory mechanism, which is a substrate for poor outcomes after TAVR46. Previous research has developed biomarker interventions to improve clinical and QoL outcomes substantially47. Nevertheless, we did not find any statistically significant differences between groups based on NT-pro-BNP levels regarding outcomes related to anxiety, depression, and QoL. Maybe NT-pro-BNP by itself is not the only biomarker influencing the QoL of patients with valvular diseases. Furthermore, while NT-pro-BNP serves as an objective indicator partially reflecting patients’ cardiac function, it may not necessarily have a direct relationship with subjective indicators of individual mental health status.
Compared to the previous two studies involving high surgical-risk AS patients48,49, our participants demonstrated distinct clinical characteristics, including younger age and better NYHA levels. Our findings revealed higher QoL scores, PCS-12 scores, and MCS-12 scores than those reported in these two studies. Correspondingly, other findings also indicated significant differences in QoL across different NYHA class levels50. This discrepancy may reflect an enhancing patient-reported health status that is typically associated with younger age and a lower risk of heart failure51. Heart failure patients with lower NYHA class not only had less debilitating physical symptoms but also reported less anxiety and depression, resulting in a better QoL52.
The mean scores for anxiety and depression after TAVR observed in this study were lower than in the previous study17. Maybe there exists a certain number of undisclosed cases of anxiety or depression among TAVR patients. This could stem from the self-reported attributes of the data and unmeasured cultural disparities53. Besides, as seen from Table 1, most of the patients in our study have partners. Moreover, due to the relatively high cost of the TAVR surgery, the patients who underwent the TAVR procedure had a relatively high family income, and the overall family support is good, which reduces the likelihood of anxiety and depression. Additionally, most of the patients had less than 5 comorbidities (67.2%). There were few patients with severe symptoms such as syncope (9.8%) and a relatively small proportion of frail patients (20.7%). Therefore, the degree of anxiety and depression caused by disease symptoms among our participants is relatively low.
Our results also showed that only a small portion (20.7%) of our participants experienced frailty. Inconsistent with similar research findings, we observed a relatively lower proportion of frail participants8,9. This could be partially attributed to the younger mean age of our study cohort. On the other hand, this finding may be attributed to the high proportion of participants with normal or elevated BMI (90.4%) in our study cohort, which is associated with higher bone mineral density and hormonal osteo-protective effects that can help weight-bearing and mobilization54. Therefore, the impact would lead to a lower risk of frailty development.
Exhaustion symptoms are one of the major frailty phenotypes in patients with valvular disease and are commonly observed in heart failure that is objectively assessed by NYHA class and BNP/NT-pro-BNP levels55,56,57. It is identical that we found frailty was positively associated with significantly increased NT-pro-BNP levels and as well a higher NYHA class. BNP/NT-proBNP, secreted by the myocardium in response to increased mechanical wall stress, the exceptionally high levels (> 10000ng/L) and low levels (< 800ng/L) have been confirmed a strong correlation with poor functional improvement after the TAVR procedure assessing by NYHA class44. When we examined the association of QoL, mental health, and the frailty phenotype, we documented significant negative interactions between the frailty phenotype and the SF-12 scores, PCS-12 scores, and MCS-12 scores. In addition, positive interactions between the frailty phenotype and the HADS-A and the HADS-D scores were noted. Frail patients with diminished physiological reserve are impaired in physical activity, endurance, mobility, strength, and other aspects. Therefore, frailty is an independent predictor of QoL for patients undergoing TAVR11. However, a TAVR procedure that only treats anatomic abnormalities might not be sufficient to continuously improve overall QoL for patients whose frailty dynamically fluctuates among different states22,58,59. Some indicators of frailty, like exhaustion, have an effect on individuals’ emotions. Strong bidirectional correlations between frailty, anxiety, and depression have recently been proven in elderly individuals with heart failure60. Effective prevention and treatment of anxiety and depression may hold promising prospects for improving frailty by increasing physical and social activities61.
The SEM findings from our study further the understanding of mental health status, particularly anxiety and depression, as a potential mediator in the relationship between frailty and QoL for patients following TAVR. Boureau et al.62 indicated that the baseline depression level in patients may not, at the very least, necessarily correlate with a worsening of their QoL six months after TAVR. Conversely, other studies have shown a correlation between depression and QoL both before and after the TAVR procedure63. We also observed not unanimous results in this study. There was no significant correlation between the HADS-A scores or HADS-D scores and the SF-12 scores, the PCS-12 scores, or the MCS-12 scores in the correlation analysis. However, using SEM, we found a direct correlation between mental health status and QoL. It is not surprising, given that the proportion of participants with anxiety (14.2%) or depression (11.1%) was relatively low, and the incidence of post-TAVR complications that impair their QoL was also low. SEM can delve deeper into the underlying relationships among variables compared to the Spearman correlation analysis, and it can also uncover some mediating effects. Besides, the uncertain reliability of self-reported scales is one of the reasons contributing to the inconsistent results. There are studies have reported that the prevalence of anxiety and depression symptoms based on scales was roughly three times higher than other diagnostic means64.
According to the Frailty Phenotype criteria, it may seem natural that frail individuals’ physical component QoL would be worse than those classified as robust. The mental QoL was also much worse among frail patients than among robust individuals. It can be speculated that frailty, even if mainly defined in physical terms, can substantially impact the mental components of the QoL65. This insight may provide a mechanism suggesting that incorporating interventions involving both physical and psychological factors could potentially improve QoL for patients undergoing TAVR.
There are several limitations in this study. Firstly, the cross-sectional study design we adopted restricted our possibility to interpret trends and trajectories longitudinally about the factors of interest. Therefore, it warrants further longitudinal research to explore the dynamics concerning QoL, frailty, anxiety, and depression among perioperative TAVR patients. Secondly, the chosen measurements for assessing QoL, frailty, anxiety, and depression are not the sole choices available. We were forced to make a selection, and our SEM lacked external validation, which downgraded the comparability and generalizability of the results. Finally, although the concept of frailty is increasingly being used, its translation from research to clinical practice remains a challenge in the coming years.
In summary, this is the first study that adds theoretical insights into patients’ QoL and its determinants, including patients’ cardiac function, frailty phenotype, and mental health status. In the future, it would be beneficial to launch campaigns to raise awareness of frailty among patients and conduct targeted interventions before and after TAVR. Therefore, specificity and standardization of frailty measurements are essential for its generalization66. Additionally, efforts should take into account the potential effects of mental health on the overall QoL of patients after TAVR, requiring beyond just anxiety and depression. Our results could also serve as an impetus for further research and the conduct of more extensive prospective trials, including additional psychological interventions targeting patients following TAVR67.
Data availability
The data are not publicly available due to privacy or ethical restriction. The data that support the findings of this study are available on reasonable request from the corresponding author.
Abbreviations
- QoL:
-
Quality of life
- TAVR:
-
Transcatheter aortic valve replacement
- AS:
-
Aortic valve stenosis
- AR:
-
Aortic regurgitation
- FP:
-
Frailty phenotype
- SF-12:
-
The short-form health survey 12
- PCS-12:
-
Physical component summary 12
- MCS-12:
-
Mental component summary 12
- HADS:
-
Hospital anxiety and depression scale
- HADS-A:
-
Anxiety dimension of hospital anxiety and depression scale
- HADS-D:
-
Depression dimension of hospital anxiety and depression scale
- NYHA:
-
New York heart association class
- BNP:
-
Brain natriuretic peptide
- NT-pro-BNP:
-
Pro-hormone of brain natriuretic peptide
- IQR:
-
Interquartile range
- SEM:
-
Structural equation model
- GFI:
-
Goodness-of-fit index
- AGFI:
-
Adjusted goodness-of-fit index
- RMSEA:
-
Root mean square error of approximation
- NFI:
-
Nonstandard fit index
- RFI:
-
Relative fit index
- IFI:
-
Incremental fit index
- TLI:
-
Tucker-Lewis index
- CFI:
-
Comparative fit index
- CI:
-
Confidence interval
- LVEF:
-
Left ventricular ejection fraction
References
Eleid, M. F. & Holmes, D. R. Jr Transcatheter aortic valve replacement: state of the art and future directions. Annu. Rev. Med. 68, 15–28. https://doi.org/10.1146/annurev-med-101615-020427 (2017).
Haraldstad, K. et al. A systematic review of quality of life research in medicine and health sciences. Qual. Life Res. 28 (10), 2641–2650. https://doi.org/10.1007/s11136-019-02214-9 (2019).
Kim, C. A. et al. Functional status and quality of life after transcatheter aortic valve replacement: a systematic review. Ann. Intern. Med. 160 (4), 243–254. https://doi.org/10.7326/M13-1316 (2014).
Reynolds, M. R. et al. Health-related quality of life after transcatheter or surgical aortic valve replacement in high-risk patients with severe aortic stenosis: results from the PARTNER (Placement of aortic transcatheter Valve) trial (Cohort A). J. Am. Coll. Cardiol. 60 (6), 548–558. https://doi.org/10.1016/j.jacc.2012.03.075 (2012).
Hoogma, D. F. et al. Postoperative delirium and quality of life after transcatheter and surgical aortic valve replacement: A prospective observational study. J. Thorac. Cardiovasc. Surg. 166 (1), 156–166e6. https://doi.org/10.1016/j.jtcvs.2021.11.023 (2023).
Kim, D. H., Kim, C. A., Placide, S., Lipsitz, L. A. & Marcantonio, E. R. Preoperative frailty assessment and outcomes at 6 months or later in older adults undergoing cardiac surgical procedures: A systematic review. Ann. Intern. Med. 165 (9), 650–660. https://doi.org/10.7326/M16-0652 (2016).
Talbot-Hamon, C. & Afilalo, J. Transcatheter aortic valve replacement in the care of older persons with aortic stenosis. J. Am. Geriatr. Soc. 65 (4), 693–698. https://doi.org/10.1111/jgs.14776 (2017).
Afilalo, J. et al. Frailty in older adults undergoing aortic valve replacement: the FRAILTY-AVR study. J. Am. Coll. Cardiol. 70 (6), 689–700. https://doi.org/10.1016/j.jacc.2017.06.024 (2017).
Strange, J. E. et al. Frailty and recurrent hospitalization after transcatheter aortic valve replacement. J. Am. Heart Assoc. 12 (8), e029264. https://doi.org/10.1161/JAHA.122.029264 (2023).
Abugroun, A., Daoud, H., Hallak, O., Abdel-Rahman, M. E. & Klein, L. W. Frailty predicts adverse outcomes in older patients undergoing transcatheter aortic valve replacement (TAVR): from the National inpatient sample. Cardiovasc. Revascula. 34, 56–60. https://doi.org/10.1016/j.carrev.2021.02.004 (2022).
Goudzwaard, J. A. et al. Impact of frailty on health-related quality of life 1 year after transcatheter aortic valve implantation. Age Ageing. 49 (6), 989–994. https://doi.org/10.1093/ageing/afaa071 (2020).
Biermann, J. et al. The impact of transcatheter aortic valve implantation on quality of life: results from the German transcatheter aortic valve interventions registry. Clin. Res. Cardiol. 104 (10), 877–886. https://doi.org/10.1007/s00392-015-0857-9 (2015).
Dent, E. et al. Physical frailty: ICFSR international clinical practice guidelines for identification and management. J. Nutr. Health Aging. 23, 771–787. https://doi.org/10.1007/s12603-019-1273-z (2019).
Johansson, I. et al. Factors associated with health-related quality of life in heart failure in 23 000 patients from 40 countries: results of the G-CHF research programme. Eur. J. Heart Fail. 24 (9), 1478–1490. https://doi.org/10.1002/ejhf.2535 (2022).
Pihl, E., Jacobsson, A., Fridlund, B., Strömberg, A. & Mårtensson, J. Depression and health-related quality of life in elderly patients suffering from heart failure and their spouses: a comparative study. Eur. J. Heart Fail. 7 (4), 583–589. https://doi.org/10.1016/j.ejheart.2004.07.016 (2005).
Sun, J. et al. Comparison of the levels of depression and anxiety in elderly aortic stenosis patients treated with surgical or transcatheter aortic valve replacement. J. Cardiothorac. Surg. 17 (1), 141. https://doi.org/10.1186/s13019-022-01888-6 (2022).
Bäz, L. et al. Depression and anxiety in elderly patients with severe symptomatic aortic stenosis persistently improves after transcatheter aortic valve replacement (TAVR). Int. J. Cardiol. 309, 48–54. https://doi.org/10.1016/j.ijcard.2020.03.021 (2020).
Williams, J. B. et al. Preoperative anxiety as a predictor of mortality and major morbidity in patients aged > 70 years undergoing cardiac surgery. Am. J. Cardiol. 111 (1), 137–142. https://doi.org/10.1016/j.amjcard.2012.08.060 (2013).
Suen, W. L., Bhasin, S., Betti, V., Bruckel, J. T. & Oldham, M. A. Mental health and transcatheter aortic valve replacement: A scoping systematic review. Gen. Hosp. Psychiat. 86, 10–23. https://doi.org/10.1016/j.genhosppsych.2023.11.009 (2024).
Surman, T. L. et al. Quality of life and frailty outcomes following surgical and transcatheter aortic valve replacement. J. Cardiothorac. Surg. 17 (1), 113. https://doi.org/10.1186/s13019-022-01876-w (2022).
Daxin, Z., Zhiwen, P., Yongjian, W. & Guangyuan, S. Chinese expert consensus on transcatheter aortic valve replacement (2020 update). Chin. J. Interventional Cardiol. 28 (06), 301–309. https://doi.org/10.3969/j.issn.1004-8812.2020.06.001 (2020).
Fried, L. P. et al. Frailty in older adults: evidence for a phenotype. The journals of gerontology. J. Gerontol. A-Biol. 56 (3), M146–M156. https://doi.org/10.1093/gerona/56.3.m146 (2001).
Ware, J., Jr Kosinski, M. & Keller, S. D. A 12-Item Short-Form health survey: construction of scales and preliminary tests of reliability and validity. Med. Care. 34 (3), 220–233. https://doi.org/10.1097/00005650-199603000-00003 (1996).
Ware, J. E., Keller, S. D. & Kosinski, M. SF-12: How To Score the SF-12 Physical and Mental Health Summary Scales (Health Institute, New England Medical Center, 1995).
Bjelland, I., Dahl, A. A., Haug, T. T. & Neckelmann, D. The validity of the hospital anxiety and depression scale: an updated literature review. J. Psychosom. Res. 52 (2), 69–77. https://doi.org/10.1016/s0022-3999(01)00296-3 (2002).
Zigmond, A. S. & Snaith, R. P. The hospital anxiety and depression scale. Acta Psychiat Scand. 67 (6), 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x (1983).
Yancy, C. W. et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American college of cardiology foundation/american heart association task force on practice guidelines. J. Am. Coll. Cardiol. 62 (16), e147–e239. https://doi.org/10.1161/CIR.0b013e31829e8776 (2013).
Chang, P. et al. BNP protects against diabetic cardiomyopathy by promoting Opa1-mediated mitochondrial fusion via activating the PKG-STAT3 pathway. Redox Biol. 62, 102702. https://doi.org/10.1016/j.redox.2023.102702 (2023).
Gerber, I. L. et al. Increased plasma natriuretic peptide levels reflect symptom onset in aortic stenosis. Circulation 107 (14), 1884–1890. https://doi.org/10.1161/01.CIR.0000060533.79248.0C (2003).
World Medical Association. World medical association declaration of helsinki: ethical principles for medical research involving human subjects. Jama-J Am. Med. Assoc. 310 (20), 2191–2194. https://doi.org/10.1001/jama.2013.281053 (2013).
Kline, R. B. Principles and Practice of Structural Equation Modeling (Guilford, 2023).
Hu, L. T. & Bentler, P. M. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ Model. 6 (1), 1–55. https://doi.org/10.1080/10705519909540118 (1999).
Bentler, P. M. Comparative fit indexes in structural models. Psychol. Bull. 107 (2), 238–246. https://doi.org/10.1037/0033-2909.107.2.238 (1990).
Tabachnick, B. G., Fidell, L. S. & Ullman, J. B. Using Multivariate Statistics (Vol 6 pp. 497–516 (pearson, 2013).
Bollen, K. A. & Long, J. S. (eds) Testing Structural Equation Models Vol. 154 (Sage, 1993).
Preacher, K. J. & Hayes, A. F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods. 40 (3), 879–891. https://doi.org/10.3758/brm.40.3.879 (2008).
Young, M. N. et al. Geographic and demographic variability in transcatheter aortic valve replacement dispersion in the united States. J. Am. Heart Assoc. 10 (12), e019588. https://doi.org/10.1161/JAHA.120.019588 (2021).
Băjenaru, L., Balog, A., Dobre, C., Drăghici, R. & Prada, G. I. Latent profile analysis for quality of life in older patients. Bmc Geriatr. 22 (1), 848. https://doi.org/10.1186/s12877-022-03518-1 (2022).
Gao, X. et al. Accelerated biological aging and risk of depression and anxiety: evidence from 424,299 UK biobank participants. Nat. Commun. 14 (1), 2277. https://doi.org/10.1038/s41467-023-38013-7 (2023).
Ross, J. J. & Braunwald, E. Aortic stenosis. Circulation 38 (1s5), V–61. https://doi.org/10.1161/01.CIR.38.1S5.V-61 (1968).
Schwarz, F. et al. The effect of aortic valve replacement on survival. Circulation 66 (5), 1105–1110. https://doi.org/10.1161/01.CIR.66.5.1105 (1982).
Gümbel, D. C. et al. Association between Syncope and the 6-Month incidence of ischemic stroke, arrhythmia, brain tumor, epilepsy, and anxiety disorder. Healthc. (Basel). 11 (13), 1913. https://doi.org/10.3390/healthcare11131913 (2023).
O’Sullivan, C. J. et al. Impact of B-type natriuretic peptide on short-term clinical outcomes following transcatheter aortic valve implantation. EuroIntervention 10 (10), e1–e8. https://doi.org/10.4244/EIJV10I10A200 (2015).
Allen, C. J. et al. Baseline NT-proBNP accurately predicts symptom response to transcatheter aortic valve implantation. J. Am. Heart Assoc. 9 (23), e017574. https://doi.org/10.1161/JAHA.120.017574 (2020).
Abramowitz, Y. et al. Impact of preprocedural B-Type natriuretic peptide levels on the outcomes after transcatheter aortic valve implantation. Am. J. Cardiol. 116 (12), 1904–1909. https://doi.org/10.1016/j.amjcard.2015.09.031 (2015).
Chen, S. et al. Low and elevated B-type natriuretic peptide levels are associated with increased mortality in patients with preserved ejection fraction undergoing transcatheter aortic valve replacement: an analysis of the PARTNER II trial and registry. Eur. Heart J. 41 (8), 958–969. https://doi.org/10.1093/eurheartj/ehz892 (2020).
Mark, D. B. et al. Economic and Quality-of-Life outcomes of natriuretic Peptide-Guided therapy for heart failure. J. Am. Coll. Cardiol. 72 (21), 2551–2562. https://doi.org/10.1016/j.jacc.2018.08.2184 (2018).
Fairbairn, T. A. et al. Serial change in health-related quality of life over 1 year after transcatheter aortic valve implantation: predictors of health outcomes. J. Am. Coll. Cardiol. 59 (19), 1672–1680. https://doi.org/10.1016/j.jacc.2012.01.035 (2012).
Georgiadou, P. et al. Long-term quality of life improvement after transcatheter aortic valve implantation. Am. Heart J. 162 (2), 232–237. https://doi.org/10.1016/j.ahj.2011.06.004 (2011).
Adamo, M. et al. Comparison of early and Long-Term outcomes after transcatheter aortic valve implantation in patients with new York heart association functional class IV to those in class III and less. Am. J. Cardiol. 122 (10), 1718–1726. https://doi.org/10.1016/j.amjcard.2018.08.006 (2018).
Baron, S. J. et al. Health status after transcatheter versus surgical aortic valve replacement in Low-Risk patients with aortic stenosis. J. Am. Coll. Cardiol. 74 (23), 2833–2842. https://doi.org/10.1016/j.jacc.2019.09.007 (2019).
Majani, G. et al. Relationship between psychological profile and cardiological variables in chronic heart failure. The role of patient subjectivity. Eur. Heart J. 20 (21), 1579–1586. https://doi.org/10.1053/euhj.1999.1712 (1999).
Wang, J. H. et al. Factors associated with Chinese American and white cancer survivors’ physical and psychological functioning. Health Psychol. 38 (5), 455–465. https://doi.org/10.1037/hea0000666 (2019).
Huang, H. L. et al. Associations of body mass index and diabetes with hip fracture risk: a nationwide cohort study. BMC Public. Health. 18 (1), 1325. https://doi.org/10.1186/s12889-018-6230-y (2018).
Perez-Moreno, A. C. et al. Fatigue as a predictor of outcome in patients with heart failure: analysis of CORONA (Controlled Rosuvastatin multinational trial in heart Failure). Jacc-Heart Fail. 2 (2), 187–197. https://doi.org/10.1016/j.jchf.2014.01.001 (2014).
Metze, C. et al. Disentangling heart failure and physical frailty: prospective study of patients undergoing percutaneous mitral valve repair. JACC Heart Fail. 11 (8 Pt 1), 972–982. https://doi.org/10.1016/j.jchf.2023.04.011 (2023).
Tanaka, T. et al. Periprocedural changes in natriuretic peptide levels and clinical outcome after transcatheter mitral valve repair. Esc Heart Fail. 8 (6), 5237–5247. https://doi.org/10.1002/ehf2.13603 (2021).
Ferrucci, L. et al. Designing randomized, controlled trials aimed at preventing or delaying functional decline and disability in frail, older persons: a consensus report. J. Am. Geriatr. Soc. 52 (4), 625–634. https://doi.org/10.1111/j.1532-5415.2004.52174.x (2004).
Fried, L. P., Ferrucci, L., Darer, J., Williamson, J. D. & Anderson, G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J. Gerontol. Biol. Sci. Med. Sci. 59 (3), 255–263. https://doi.org/10.1093/gerona/59.3.m255 (2004).
Uchmanowicz, I. & Gobbens, R. J. The relationship between frailty, anxiety and depression, and health-related quality of life in elderly patients with heart failure. Clin. Interv Aging. 10, 1595–1600. https://doi.org/10.2147/CIA.S90077 (2015).
Gould, R. L., Coulson, M. C. & Howard, R. J. Efficacy of cognitive behavioral therapy for anxiety disorders in older people: a meta-analysis and meta-regression of randomized controlled trials. J. Am. Geriatr. Soc. 60 (2), 218–229. https://doi.org/10.1111/j.1532-5415.2011.03824.x (2012).
Boureau, A. S. et al. Predictors of Health-Related quality of life decline after transcatheter aortic valve replacement in older patients with severe aortic stenosis. J. Nutr. Health Aging. 21 (1), 105–111. https://doi.org/10.1007/s12603-016-0739-5 (2017).
Dalberto, M., Miot, S., Leclercq, F. & Blain, H. Frailty, depression and prognosis after transcatheter aortic valve replacement: a literature review. Geriatr. Psychol. Neuropsychiatr Vieil. https://doi.org/10.1684/pnv.2021.0966 (2021).
Edwards, K. S. et al. Impact of cognitive behavioral therapy on depression symptoms after transcatheter aortic valve replacement: A randomized controlled trial. Int. J. Cardiol. 321, 61–68. https://doi.org/10.1016/j.ijcard.2020.08.007 (2020).
Kojima, G., Iliffe, S., Jivraj, S. & Walters, K. Association between frailty and quality of life among community-dwelling older people: a systematic review and meta-analysis. J. Epidemiol. Commun. H 70 (7), 716–721. https://doi.org/10.1136/jech-2015-206717 (2016).
Hoogendijk, E. O. et al. Frailty: implications for clinical practice and public health. Lancet 394 (10206), 1365–1375. https://doi.org/10.1016/S0140-6736(19)31786-6 (2019).
Fehlmann, C. A. et al. Influence of preoperative frailty on quality of life after cardiac surgery: A systematic review and meta-analysis. J. Am. Geriatr. Soc. 71 (10), 3278–3286. https://doi.org/10.1111/jgs.18454 (2023).
Acknowledgements
The study was supported by the “Natural Science Foundation of Sichuan Province (Grant number 2022NSFSC0645),” and the “Natural Science Foundation of Sichuan Province (Grant number 2023YFQ0099).” These funds are essential for covering research expenses.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. YB, ZLC, and JYW conceived and designed the study; JYW, JC and XMY performed data collection; MC and XMY curated the data and supervised the study; JYW and SYT were responsible for software usage and performed the analysis process; JYW and JC drafted the manuscript; YW, LHZ, SYT, YJ and MC reviewed and edited the manuscript; All authors had reviewed and approved the final version of the manuscript. They had full access to all the data of this study. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, J., Cui, J., Yang, X. et al. The effects of frailty, mental health, and cardiac function on quality of life in patients undergoing transcatheter aortic valve replacement. Sci Rep 15, 22440 (2025). https://doi.org/10.1038/s41598-025-04859-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04859-8